Summary:
Reconstruction of ptotic or large breasts is challenging due to skin redundancy after skin-sparing mastectomy. Skin reduction can be performed with a long horizontal ellipse, but this often flattens the breast and leaves conspicuous scars medially on the chest. Wise pattern skin reduction is an effective technique for shaping, but excision of skin within the Wise pattern can lead to high rates of skin necrosis and implant exposure or infection. This study describes a technique where the Wise pattern skin is preserved, but deepithelialized, allowing apparent reduction of the skin with preservation of the subdermal plexus. This study reviews data for case series of 26 breasts in 15 patients who have undergone this technique with simultaneous prosthetic reconstruction using an expander.
Reconstruction of ptotic or large breasts is challenging due to skin redundancy after skin-sparing mastectomy. Excess skin can lead to wrinkling of the skin or implant, poor breast shape, and high risk of seroma. Skin reduction can be performed with a long horizontal ellipse, but this often flattens the breast and leaves conspicuous scars medially on the chest. The Wise pattern was initially described for breast reduction and mastopexy by Wise in 1956. The pattern allows removal of skin in both vertical and horizontal dimensions allowing for lifting and coning of the breast into a less ptotic shape. The Wise pattern has been used for skin reduction in skin-sparing mastectomy in the past.1 However, the skin necrosis rate in his study was 27%, which can be associated with high rates of infection and implant exposure.
This article presents a technique where all of the skin within the Wise pattern markings is deepithelialized during skin-sparing mastectomy to preserve the underlying subdermal plexus. To our knowledge, this technique has not been described in literature in the past.
METHODS
A prospective database of patients undergoing this procedure was kept starting in 2010 when this procedure was first performed in our practice until the present time. Retrospective review of the patient records was then performed to obtain data regarding chemotherapy, radiation, tobacco use, body mass index, expander fill volume, follow-up interval, and complications.
Surgical Technique
The patient is marked while standing for a traditional Wise pattern skin reduction, as if the patient was having a standard breast reduction procedure (Fig. 1). The skin-sparing mastectomy is performed via either a circumareolar incision or a vertical oval incision located within the Wise pattern skin markings.
Fig. 1.
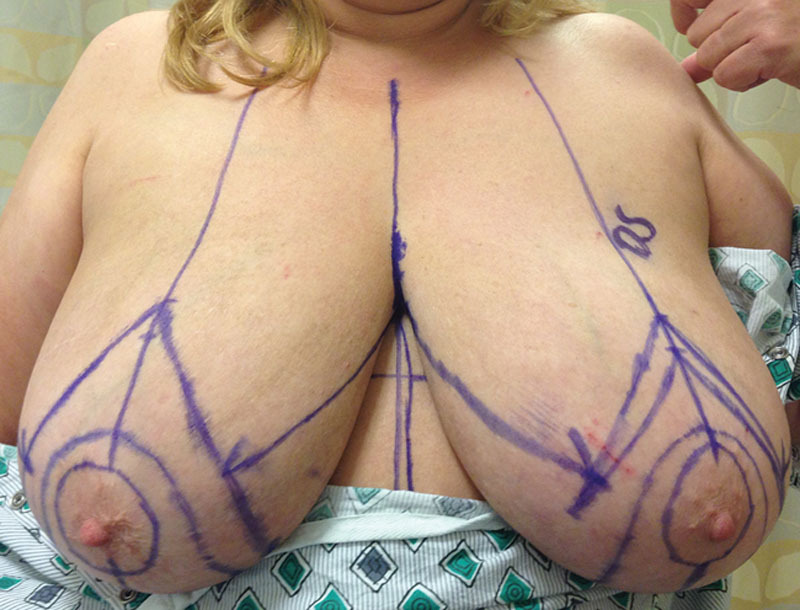
Preoperative view of a patient with grade III breast ptosis. Wise pattern markings have been drawn, as they would be for a standard breast reduction.
After the skin-sparing mastectomy has been completed, expander reconstruction is performed in a subpectoral pocket with a sling of acellular dermal matrix or mesh along the inferior lateral aspect of the pocket as described by other authors.2, 3 Our general preference is to use an 8 cm × 20 cm sheet of AlloDerm of a thickness of less than 1.5 mm for each breast, but sometimes other products were used in these patients including FlexHD and SERI Surgical Scaffold. The expander is filled to full capacity under the pectoralis major muscle–acellular dermal matrix pocket. The expander is filled to full capacity to allow for accurate assessment of the skin redundancy.
The skin is tailor tacked with staples along the Wise pattern skin markings placed before surgery (Fig. 2). Often the markings represent a slight overestimation of the skin redundancy so adjustments are made as necessary. Markings are made along the staple lines and the staples are removed. The skin within the new Wise pattern markings is deepithelialized (Fig. 3). Sometimes the mastectomy flaps need to be thinned under the area of deepithelialization to avoid excess bulk along the inframammary fold during closure.
Fig. 2.

Same patient as in Figure 1. Bilateral skin-sparing mastectomies were performed through circumareolar incisions. Expanders were placed under the pectoralis major and acellular dermal graft. The expanders were filled to full capacity. The right breast skin has been tailor tacked with staples along the Wise pattern skin markings to assess for skin redundancy.
Fig. 3.

Same patient as in Figure 1. The staples have been removed and the skin within the Wise pattern markings has been deepithelialized bilaterally. The acelluar dermal allograft and a small portion of the pectoralis major muscle can be seen through the circular mastectomy incisions.
A single drain is placed in each breast between the mastectomy skin flaps and the pectoralis major muscle–acellular dermal matrix layer. The circumareolar or oval mastectomy skin defect is closed primarily in a vertical line. Sometimes this vertical closure is tacked down to the underlying dermal allograft or muscle to suspend it. This can prevent ptosis and bunching of the excess skin inferiorly along the inframammary fold. The Wise pattern skin closure is performed along the vertical and horizontal lines (Fig. 4). At the end of the procedure, the expander is accessed to remove some of the volume to take any tension off of the mastectomy skin.
Fig. 4.

Postoperative view of the same patient after the expanders have been replaced with implants, but before nipple reconstruction.
RESULTS
Fifteen patients (26 breasts) were included in this study. This included 11 bilateral patients and 4 unilateral patients. The average age was 51 with a range of 36 to 65. The average body mass index was 27 with a range of 21 to 37. Average follow-up time was 38 months with a range of 7 to 82. Seven patients had postmastectomy radiation. Six patients had neoadjuvant chemotherapy and 4 patients had postmastectomy chemotherapy. Three patients were active tobacco users (defined as smoking within 1 month before surgery), 2 bilateral, and 1 unilateral. Initial expander fill volume averaged 77% of expander capacity and ranged from 61% to 100%. All reconstructions were two-stage expander/implant reconstructions.
Complications included skin necrosis that required surgical revision (23%), seroma requiring aspiration (8%), expander removal (8%), and cellulitis that resolved with intravenous antibiotics (4%). The most common complication was skin necrosis, which occurred in 6 breasts (23%), 3 of which were in patients that were active tobacco users. All 6 breasts with skin necrosis were treated with operative excision of the necrotic area within 2 weeks after the mastectomy procedure. One of these breasts developed an infection requiring removal of the expander. This patient had unilateral reconstruction. She was an active smoker with a body mass index of 27 who developed skin necrosis followed by infection with Serratia marcesens.
The second most common complication was seroma occurring in 2 breasts (8%) after removal of the drains. The seromas were treated with ultrasound-guided drain placement in 1 breast and ultrasound-guided aspiration without drain placement in 1 breast. The breast that had a drain placed developed late pseudomonas infection while on chemotherapy, leading to removal of the expander. This patient had bilateral reconstruction and she was not a smoker. Her body mass index was 37.
DISCUSSION
Our series of 26 reconstructions of ptotic breasts using a Wise pattern deepithelialization technique showed a skin necrosis rate of 23% (6 breasts in 4 patients). This included 3 breasts (2 patients) that were active tobacco users. Our prosthesis removal rate was 8% (2 breasts in 2 patients). One patient was an active smoker who developed an infection. The other had an elevated body mass index of 37 who developed a seroma followed by an infection. Although these factors likely contributed to their complications, it is difficult to assess the significance due to the small size of this study.
Other techniques to reconstruct the ptotic breast include the use of standard Wise pattern skin excision,1 Wise pattern skin excision with autograft sling of deepithelialized dermis over the lower pole,4–7 Wise pattern skin excision with dermal autograft and acellular dermis,8 circumvertical skin deepithelialization,9, 10 and staged Wise pattern skin excision.11 These studies report complication rates varying from 0% to 27%, but details regarding body mass index and tobacco use were often not included.
Footnotes
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
REFERENCES
- 1.Carlson GW, Bostwick J, 3rd, Styblo TM, et al. Skin-sparing mastectomy. Oncologic and reconstructive considerations. Ann Surg. 1997;225:570–575. doi: 10.1097/00000658-199705000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Breuing KH, Colwell AS. Inferolateral AlloDerm hammock for implant coverage in breast reconstruction. Ann Plast Surg. 2007;59:250–255. doi: 10.1097/SAP.0b013e31802f8426. [DOI] [PubMed] [Google Scholar]
- 3.Zienowicz RJ, Karacaoglu E. Implant-based breast reconstruction with allograft. Plast Reconstr Surg. 2007;120:373–381. doi: 10.1097/01.prs.0000267340.31742.1. [DOI] [PubMed] [Google Scholar]
- 4.Bostwick J. Total mastectomy with breast skin and volume reduction using an inverted ‘T’ incision. In: Bostwick J, editor. In Plastic and Reconstructive Breast Surgery. St Louis: Quality Medical Publisher Inc; 1990. pp. 1048–1054. [Google Scholar]
- 5.Prathap P, Harland RN. Wise pattern mastectomy with immediate breast reconstruction. Breast. 2004;13:502–505. doi: 10.1016/j.breast.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Nava MB, Cortinovis U, Ottolenghi J, et al. Skin-reducing mastectomy. Plast Reconstr Surg. 2006;118:603–610. doi: 10.1097/01.prs.0000233024.08392.14. discussion 611. [DOI] [PubMed] [Google Scholar]
- 7.Nair A, Jaleel S, Abbott N, et al. Skin-reducing mastectomy with immediate implant reconstruction as an indispensable tool in the provision of oncoplastic breast services. Ann Surg Oncol. 2010;17:2480–2485. doi: 10.1245/s10434-010-1058-4. [DOI] [PubMed] [Google Scholar]
- 8.Derderian CA, Karp NS, Choi M. Wise-pattern breast reconstruction: modification using AlloDerm and a vascularized dermal-subcutaneous pedicle. Ann Plast Surg. 2009;62:528–532. doi: 10.1097/SAP.0b013e3181a0cfee. [DOI] [PubMed] [Google Scholar]
- 9.Bayram Y, Kulahci Y, Irgil C, et al. Skin-reducing subcutaneous mastectomy using a dermal barrier flap and immediate breast reconstruction with an implant: a new surgical design for reconstruction of early-stage breast cancer. Aesthetic Plast Surg. 2010;34:71–77. doi: 10.1007/s00266-009-9452-7. [DOI] [PubMed] [Google Scholar]
- 10.Ibrahim AE, Atiyeh BS, Dibo SA, et al. De-epithelialized dermal barrier for a safe immediate prosthetic breast reconstruction post circumvertical skin sparing/reducing mastectomy (SSM/SRM). Eur J Plast Surg. 2012;35:787–793. [Google Scholar]
- 11.Liu TS, Crisera CA, Festekjian JH, et al. Staged wise-pattern skin excision for reconstruction of the large and ptotic breast. Plast Reconstr Surg. 2010;126:1831–1839. doi: 10.1097/PRS.0b013e3181f5278f. [DOI] [PubMed] [Google Scholar]


