Abstract
Background:
Lichen sclerosus (LS) is an inflammatory dermatosis with autoimmune pathogenesis. Although relatively common, its true incidence is unknown and likely underestimated. LS is usually anogenital, but in around 10% of patients, it can present as extragenital lesions. Continuous administration of topical corticosteroids is the mainstay of medical treatment. Other treatments are available but are only occasionally prescribed along with or instead of topical steroids. Injection of platelet-rich plasma (PRP) into affected areas has been reported to result in the regeneration of normal skin. In this study, we aimed to evaluate the safety, symptom resolution, and objective improvement in patients with autoimmune condition like genital LS after treatment with PRP.
Methods:
Over a 2-year period at FBW Gynaecology Plus, we had a total of 28 patients with confirmed LS on biopsy, unresponsive to topical steroid treatment. After acquiring informed consent, patients’ own blood was centrifuged on site and injected under local anesthesia to the external genitalia.
Results:
Almost all of our patients showed clinical improvement in the size of their lesions, and in 8 cases, lesions totally disappeared after treatment with PRP. Symptoms disappeared in 15 of the 28 patients after treatment, with no need for further steroid therapy in 23 patients. Thirteen women experienced partial symptom relief.
Conclusions:
Based on our limited findings, we hypothesize that PRP presents a potential alternative to topical steroids for treatment of vulvovaginal autoimmune conditions such as LS. A larger pilot and/or randomized controlled trial study is required to evaluate this finding further.
Lichen sclerosus (LS) is a chronic autoimmune inflammatory dermatosis characterized by a lymphocytic response that has a predilection for the genital skin in both sexes and an association with several other autoimmune diseases.1 Women are 6 to 10 times more often affected than men.2 LS may involve complications of erosions, atrophy, and scarring as a result of inflammation and altered fibroblast function, leading to fibrosis of the upper dermis. There can also be purpura, hyperpigmentation, fissures, and edema.3 LS mainly affects the anogenital area of the skin, in more than a 5:1 ratio when compared with extragenital skin.4
LS is relatively common although the true incidence is unknown and possibly underestimated, in part, due to the distribution of patients among different clinical specialities and to the fact that it can be asymptomatic.1 The etiology of LS is uncertain although there is evidence for linkages between autoimmune mechanisms and the pathogenesis of LS.5
LS is a scarring process and may cause loss of the labia minora, sealing of the clitoral hood, and burying of the clitoris. In women, vulvar LS can present with progressive pruritus, dyspareunia, dysuria, or genital bleeding.4 These symptoms may also occur in postmenopausal women due to the lack of estrogen in the vaginal area. LS has a considerable impact on affected patients physically, emotionally, and psychologically, affecting their quality of life through pain and embarrassment and having a significant impact on their sexual lives, which can affect their intimate relationships.
Severe introital stenosis (ie, narrowing of the vaginal opening) occurs rarely.1 LS can also be associated with squamous cell carcinoma (SCC); there is a 4% lifetime risk of developing SCC among LS sufferers.6 Histopathological examination of vulval SCC cases shows that over 60% have a background of LS.7 In the presence of typical clinical features, confirmation with colposcopy and exclusion of conditions such as vulvar intraepithelial neoplasia, a biopsy is not always necessary for the diagnosis of LS.8 However, histological examination is recommended given the presentation of atypical features and mandatory if the disease fails to respond to treatment and second-line therapy is to be used.1
There is no current cure for LS nor is there a comprehensive treatment to cover all patients. Much of the management of LS is aimed at controlling symptoms, such as pruritus in extragenital LS. Current guidelines aim at treating patients with ultrapotent topical corticosteroids, which are symptomatically effective in 90% of women and show variable objective improvement.9 Corticosteroids require continuous administration and present complications.10 Furthermore, for the 40% to 57% of postmenopausal women experiencing symptoms resulting from atrophic vaginitis11 due to menopausal estrogen deficiency and natural aging of the vagina, corticosteroids can worsen the atrophy.12 As most patients with LS are of postmenopausal age,13 corticosteroids are a problematic treatment option.
In Australia, the guidelines for treatment of LS are for betamethasone dipropionate ointment (0.05%) to be used twice daily for 1 month, then daily for 2 months, and gradually reduced as needed (ideally 1–2 times per week14). This high-maintenance treatment regime can lead to relapse by patients who are not compliant or who find it to be a difficult regime to uphold. A study by Renaud-Vilmer et al15 investigated remission and recurrence rates of 85 patients with 0.05% clobetasol proprionate ointment and found that 72% of women under age 50 showed complete remission, 23% of women between 50 and 70 years old had complete remission, and no women over 70 years old had complete remission. These results highlight the impact of age on the success of topical corticosteroids as treatment for LS.15
A variety of other treatment options are available, including calcipotriol, retinoids, systemic steroids, tacrolimus, and pimecrolimus. Photodynamic therapy has also been reported to be beneficial.16 Surgical treatments involve vulvectomy, cryosurgery, and laser ablation.1 These procedures pose the risk of scarring to damaged tissues and present high recurrence rates.17 Less invasive techniques are therefore of interest.
In recent years, many scientists have shown the existence of cells in the adult body that are capable of repairing and regenerating damaged tissue. By extracting and processing blood through a sophisticated extraction system, it is possible to produce platelet-rich plasma (PRP), a type of plasma that contains several major growth factors, nutrients, minerals, and monocytes with the potential to assist in wound healing.
PRP has been used clinically for tissue regeneration, reconstructive and plastic operations, and surgery, including wound hemostasis, wound sealing, augmentation of bone grafts periodontics, and treatment of tendonitis.18–20 In addition, PRP has promoted tendon healing in acute tendon injury and repair models. Increased epithelialization has been demonstrated in both acute traumatic wounds and chronic diabetic wounds through the use of PRP.20 PRP injection with or without needling has been described as a new and promising modality for the treatment of atrophic acne scars.21 Activated platelets release growth factors that contribute to cell migration, proliferation, differentiation, angiogenesis, removal of tissue debris, and regeneration of appropriate type of tissue.22 PRP has a high safety level and can be obtained relatively noninvasively through a venous blood draw where the blood is then mechanically centrifuged to extract a concentrate of PRP, which allows repeated administration.17,23
One study investigated a new regenerative approach based on grafting of adipose-derived stem cells and injection of PRP that removed symptoms and reduced atrophy and sclerosus in 15 female patients with a histologic diagnosis of LS who were unresponsive to topical steroid therapy.17 However, the need for all patients to undergo liposuction to isolate the adipose-derived stem cells means that the process still requires day surgery, thereby having a significant impact on the health system and patients’ lifestyles. The aim of this study was to investigate the efficacy of injecting PRP alone as a treatment for LS, so that the need for surgery may be eliminated or rendered as minimally invasive as possible for patients who do not respond to topical steroid treatment.17
The potential adoption of PRP for autoimmune skin conditions such as LS has been discussed in the literature.5,17 However, it still remains unclear whether PRP is a sufficiently effective treatment to replace topical steroids. The aim of this article is to present a new regenerative approach that removes symptoms and reduces atrophy and sclerosus in patients diagnosed with LS. This method is based on injection of PRP.17
PATIENTS AND METHODS
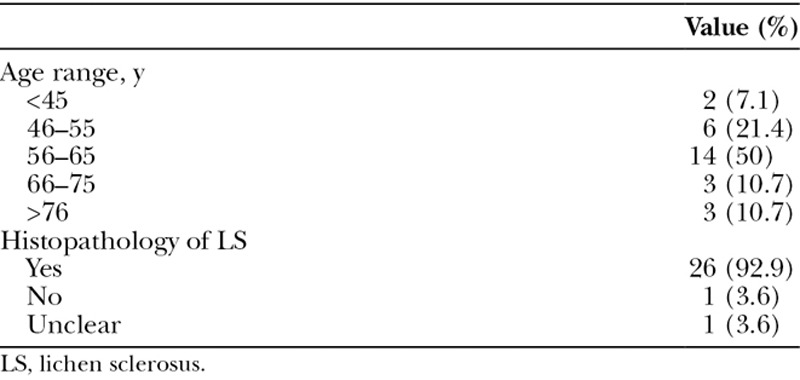
Patients were 28 women aged 22 to 88 years (M = 60) who attended FBW Gynaecology Plus from 2013 to 2016 (Table 1). Twenty-six of the 28 patients had confirmed LS on biopsy, with histopathological data indicating possible LS for 1 patient and no LS for one other patient. However, colposcopic examination suggested the presence of LS in all patients. Symptoms were unresponsive to topical steroid treatment in all cases. Those patients who had been using steroids for management of LS symptoms discontinued their use throughout the duration of the study.
Table 1.
Baseline Patient Characteristics
After providing written informed consent, patients’ own blood (10 mL) was centrifuged (Regens Lab, New York, N.Y.) on site and injected under local anesthesia (lignocaine, 23%; tetracaine, 7%) to any affected areas of the external genitalia, including the labia majora, labia minora, clitoris, and clitoral hood. The injection was carried out using a 27-gauge needle in a fanning motion to break the scar and fibrotic tissue and retrograde injection of PRP in the tissue. Patients received 3 PRP treatments 4 to 6 weeks apart and again at 12 months. Patients were verbally interviewed about their symptoms (eg, soreness, discomfort, and dyspareunia) after each treatment session, and lesions were evaluated at each session by colposcopy. Patients with vulval intraepithelial neoplasia (n = 2) were excluded from the study. Posttreatment pain scores were measured after each treatment using a verbal scale from 0 to 10. Patients were asked to complete the Australian Pelvic Floor Questionnaire 24 at baseline and at 2 to 3 months after the final PRP treatment, with higher scores indicating greater frequency of symptoms on each variable. The questionnaire was used to assess symptoms of urinary incontinence, general bladder function, prolapse, and sexual function.
Statistical Analyses
Changes in lesion size, symptoms, and need for topical steroid use were compared from pre- to posttreatment using the Wilcoxon signed-rank test. Statistical analyses were performed using SPSS Statistics version 21.0 (IBM, Chicago, Ill.), and values of P less than 0.05 were considered to be statistically significant.
RESULTS
Nearly all patients exhibited clinical improvement in the size of their lesions (Table 2), and in 8 of the 28 patients (28.6%), lesions disappeared completely after treatment with PRP. A Wilcoxon signed-rank test indicated that there was a statistically significant decrease in the number of patients with lesions after PRP treatment (Z = −4.562; P < 0.001).
Table 2.
Presence of Lesions and Symptoms after Platelet-rich Plasma Treatment
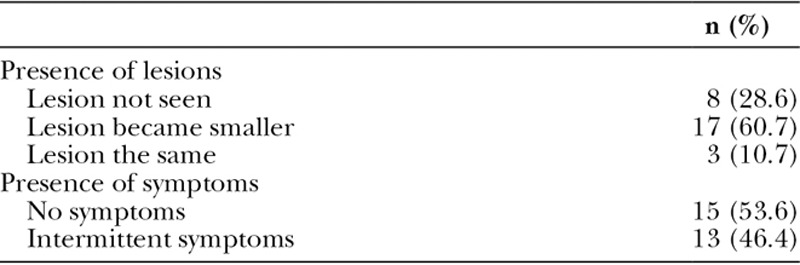
Pretreatment symptoms included severe itch (requiring steroid treatment), soreness, discomfort, and/or dyspareunia. As shown in Table 2, more than half the sample had become free of symptoms after the final PRP treatment at 12 months or more. A Wilcoxon signed-rank test showed a statistically significant decrease in the presence of symptoms after treatment (Z = −4.768; P < 0.001).
After the final treatment (at 12 months or more), 82.1% of patients (n = 23) no longer needed to use steroids; the remaining 17.9% (n = 5) continued to use them intermittently. A Wilcoxon signed-rank test showed a statistically significant decrease in steroid use after treatment with PRP (Z = −4.963; P <.001).
Although there was a generally declining trend for responses to items on the Australian Pelvic Floor Questionnaire from pre- to posttreatment, none of the changes were statistically significant, likely due to the very small sample size for pelvic floor disorders.
Patients reported minimal to moderate pain. During the 24 hours after the procedure, 26 patients (92.9%) reported pain scores of 2 to 3; the remaining patients reported scores of 5 and 7, respectively. There were 0 cases of infection, bleeding, hematoma, or other adverse outcomes.
DISCUSSION
In this study, we found that the majority of patients with LS reported significant improvement in their symptoms, with no need for further steroid therapy after PRP treatment.
Furthermore, the majority of patients’ lesions disappeared or became smaller after treatment. Based on these limited findings, we hypothesize that PRP can be used as a possible alternative to topical corticosteroids for the treatment of LS or at least in cases where steroids have ceased to work. The PRP procedure is minimally invasive and safe and can be performed in an office setting under local anesthesia. Our findings lend support to those of Casabona et al17 by demonstrating that PRP injection may be an effective treatment for LS, without the need for further surgery and associated risks.
The study possessed several limitations. First, our sample size was limited, and a subsequent pilot study or randomized controlled trial (RCT) with a larger sample size is required to further evaluate the efficacy of PRP. Second, the vast majority of patients were postmenopausal, making it difficult to generalize the current findings to women of reproductive age. However, it should be considered that LS occurs most frequently in postmenopausal women.25 Finally, it is conceivable that the observed improvements in LS symptoms after PRP treatment were partially or wholly due to the tissue needling involved in the PRP injection process rather than to a simple effect of the PRP in and of itself. Subjecting tissues to microtrauma can instigate the tissue repair cascade, and in the present circumstances, this cannot be ruled out as a therapeutic mechanism. For this reason, we intend to conduct a double-blind RCT in which one group is randomized to a saline injection, with a second group randomized to PRP treatment.
CONCLUSIONS
Growth factors released by platelets, monocytes, and nutrients have an important role in phagocytosis of fibrotic tissue, inflammation reduction, angiogenesis stimulation, and collagen III synthesis. The injection of PRP can therefore be considered effective therapy for LS.
It remains unclear whether needling with saline can result in the same outcome as PRP due to the breakdown of sclerotic tissue, allowing the local stem cells and monocytes to improve tissue healing. There is a need for further RCTs to compare outcomes between these 2 treatment methods and to elucidate the precise mechanism whereby PRP treatment seems to benefit patients with skin conditions like LS.
ACKNOWLEDGMENTS
We thank Katherine Bell for her assistance in proofreading the article.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Neill SM, Lewis FM, Tatnall FM, et al. British Association of Dermatologists. British Association of Dermatologists’ guidelines for the management of lichen sclerosus 2010. Br J Dermatol. 2010;163:672–682. doi: 10.1111/j.1365-2133.2010.09997.x. [DOI] [PubMed] [Google Scholar]
- 2.Newman N, Dolphin NN, Newman GR. Signs and symptoms of genital lichen sclerosus in women seeking autologous adipose derived stem cell treatment. Med J Obstet Gynecol. 2015;3:1067–1072. [Google Scholar]
- 3.Ball SB, Wojnarowska F. Vulvar dermatoses: lichen sclerosus, lichen planus, and vulval dermatitis/lichen simplex chronicus. Semin Cutan Med Surg. 1998;17:182–188. doi: 10.1016/s1085-5629(98)80012-6. [DOI] [PubMed] [Google Scholar]
- 4.Meffert J Lichen sclerosus et atrophicus [Internet] Medscape. Accessed May 21, 2016. Available at: http://emedicine.medscape.com/article/1123316-overview.
- 5.Boero V, Brambilla M, Sipio E, et al. Vulvar lichen sclerosus: a new regenerative approach through fat grafting. Gynecol Oncol. 2015;139:471–475. doi: 10.1016/j.ygyno.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Wallace HJ. Lichen sclerosus et atrophicus. Trans St Johns Hosp Dermatol Soc. 1971;57:9–30. [PubMed] [Google Scholar]
- 7.Neill SM, Tatnall FM, Cox NH British Association of Dermatologists. Guidelines for the management of lichen sclerosus. Br J Dermatol. 2002;147:640–649. doi: 10.1046/j.1365-2133.2002.05012.x. [DOI] [PubMed] [Google Scholar]
- 8.Royal College of Obstetricians and Gynaecologists. The Management of Vulval Skin Disorders. London: Royal College of Obstetricians and Gynaecologists; 2011. [Google Scholar]
- 9.Sinha P, Sorinola O, Luesley DM. Lichen sclerosus of the vulva. Long-term steroid maintenance therapy. J Reprod Med. 1999;44:621–624. [PubMed] [Google Scholar]
- 10.Liu D, Ahmet A, Ward L, et al. A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol. 2013;9:30. doi: 10.1186/1710-1492-9-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palacios S. Managing urogenital atrophy. Maturitas. 2009;63:315–318. doi: 10.1016/j.maturitas.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 12.Fischer G. Treatment of vaginitis and vulvitis. Aust Prescr. 2001;24:59–61. [Google Scholar]
- 13.Moyal-Barracco M, Wendling J. Vulvar dermatosis. Best Pract Res Clin Obstet Gynaecol. 2014;28:946–958. doi: 10.1016/j.bpobgyn.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Welsh BM, Berzins KN, Cook KA, et al. Management of common vulval conditions. Med J Aust. 2003;178:391–395. doi: 10.5694/j.1326-5377.2003.tb05257.x. [DOI] [PubMed] [Google Scholar]
- 15.Renaud-Vilmer C, Cavelier-Balloy B, Porcher R, et al. Vulvar lichen sclerosus: effect of long-term topical application of a potent steroid on the course of the disease. Arch Dermatol. 2004;140:709–712. doi: 10.1001/archderm.140.6.709. [DOI] [PubMed] [Google Scholar]
- 16.Olejek A, Kozak-Darmas I, Kellas-Sleczka S, et al. Effectiveness of photodynamic therapy in the treatment of lichen sclerosus: cell changes in immunohistochemistry. Neuro Endocrinol Lett. 2009;30:547–551. [PubMed] [Google Scholar]
- 17.Casabona F, Priano V, Vallerino V, et al. New surgical approach to lichen sclerosus of the vulva: the role of adipose-derived mesenchymal cells and platelet-rich plasma in tissue regeneration. Plast Reconstr Surg. 2010;126:210e–211e. doi: 10.1097/PRS.0b013e3181ea9386. [DOI] [PubMed] [Google Scholar]
- 18.Jeon YR, Kang EH, Yang CE, et al. The effect of platelet-rich plasma on composite graft survival. Plast Reconstr Surg. 2014;134:239–246. doi: 10.1097/PRS.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 19.Salcido RS. Autologous platelet-rich plasma in chronic wounds. Adv Skin Wound Care. 2013;26:248. doi: 10.1097/01.ASW.0000430666.20897.c0. [DOI] [PubMed] [Google Scholar]
- 20.Harris NL, Huffer WE, von Stade E, et al. The effect of platelet-rich plasma on normal soft tissues in the rabbit. J Bone Joint Surg Am. 2012;94:786–793. doi: 10.2106/JBJS.J.00984. [DOI] [PubMed] [Google Scholar]
- 21.Nofal E, Helmy A, Nofal A, et al. Platelet-rich plasma versus CROSS technique with 100% trichloroacetic acid versus combined skin needling and platelet rich plasma in the treatment of atrophic acne scars: a comparative study. Dermatol Surg. 2014;40:864–873. doi: 10.1111/dsu.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 22.Dionyssiou D, Demiri E, Foroglou P, et al. The effectiveness of intralesional injection of platelet-rich plasma in accelerating the healing of chronic ulcers: an experimental and clinical study. Int Wound J. 2013;10:397–406. doi: 10.1111/j.1742-481X.2012.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeong KH, Shin MK, Kim NI. Refractory lipodermatosclerosis treated with intralesional platelet-rich plasma. J Am Acad Dermatol. 2011;65:e157–e158. doi: 10.1016/j.jaad.2011.06.040. [DOI] [PubMed] [Google Scholar]
- 24.K Baessler, SM O’Neill, CF Maher, D Battistutta. Australian pelvic floor questionnaire: a validated interviewer-administered pelvic floor questionnaire for routine clinic and research. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:149–158. doi: 10.1007/s00192-008-0742-4. [DOI] [PubMed] [Google Scholar]
- 25.O’Connell TX, Nathan LS, Satmary WA, et al. Non-neoplastic epithelial disorders of the vulva. Am Fam Physician. 2008;77:321–326. [PubMed] [Google Scholar]


