Abstract
Inflammation is associated with the development and malignant progression of most cancers. As most of the cell types involved in cancer associated inflammation are genetically stable and thus are not subjected to rapid emergence of drug resistance, the targeting of inflammation represents an attractive strategy both for cancer prevention and cancer therapy. Tumor extrinsic inflammation is caused by many factors, including bacterial and viral infections, autoimmune diseases, obesity, tobacco smoking, asbestos exposure and excessive alcohol consumption, all of which increase cancer risk and stimulate malignant progression. By contrast, cancer-intrinsic or cancer-elicited inflammation can be triggered by cancer initiating mutations and can contribute to malignant progression through the recruitment and activation of inflammatory cells. Both extrinsic and intrinsic inflammation can result in immune suppression, thereby providing a preferred background for tumor development. In clinical trials, lifestyle modifications including healthy diet, exercise, alcohol and smoking cessation have proven effective in ameliorating inflammation and reducing the risk of cancer-related deaths. In addition, consumption of certain anti-inflammatory drugs, including aspirin, can significantly reduce cancer risk, suggesting that common non-steroidal anti-inflammatory drugs (NSAIDs) and more specific COX2 inhibitors can be used in cancer prevention. In addition to being examined for their preventative potential, both NSAIDs and more potent anti-inflammatory antibody-based drugs need to be tested for their ability to augment the efficacy of more conventional therapeutic approaches based on tumor resection, radiation and cytotoxic chemicals.
Keywords: Inflammation, Cancer, Prevention, Therapy
Chronic inflammation and invasive tumour growth: wounds that do not heal
A correlation between inflammation and cancer was identified in 1863, by Rudolf Ludwig Carl Virchow(1), who recognized the inflammatory process as one of the predisposing conditions for tumor development, described as an “Out of the ‘normal’ inflammatory hyperplasia”(2), frequently associated with alteration of the physiological healing process. In response to tissue injury, a multifactorial network of chemical signals, initiated and amplified upon recruitment and infiltration of leukocytes (neutrophils, monocytes and eosinophils) from the venous system to the sites of damage, initiates and maintains a host response designed to ‘heal’ the afflicted tissue. In addition to cell proliferation and tissue repair, inflammation is also responsible for clearing dead cells and other debris. This kind of physiological inflammatory response is self-limiting, and is terminated after the assaulting agent is removed or the repair is completed(3, 4). However, if inflammation is unregulated, it can become chronic, inducing malignant growth and tumor initiation in the surrounding tissue, due to the persistent production of growth factors as well as reactive oxygen and nitrogen species that interact with the DNA of the proliferating epithelium and result in permanent genomic alterations(5, 6). In addition to tumor initiation, inflammation plays a decisive role in tumor promotion, malignant conversion and metastatic dissemination. Many different inflammatory mediators can stimulate tumor development, including cytokines, chemokines, growth factors, free radicals, prostaglandins and proteolytic enzymes. These factors are produced by a variety of cells that populate the tumor microenvironment such as macrophages, neutrophils, lymphocytes, dendritic cells, natural killer cells, fibroblasts, adipocytes and endothelial cells and sometimes also by the cancer cells themselves. Some of these factors act directly on cancer cells, stimulating their proliferation and inhibiting their death while promoting the accumulation of oncogenic mutations, whereas other factors manifest their protumorigenic activity by acting on other components of the tumor microenvironment. While epidemiological studies indicate that at least 20% of all cancers begin as a direct consequence of chronic inflammatory disease (Table 1)(7, 8), inflammatory processes elicited by the tumor itself are likely to be involved in the majority of solid malignancies, as recently demonstrated for colorectal cancer(9, 10). Inflammation is the common mechanism of action for numerous cancer risk factors, including infection, obesity, tobacco smoking, alcohol consumption, exposure to microparticles, dysbiosis and chronic inflammatory diseases such as pancreatitis and colitis. Considering the extreme commonality of inflammatory changes in different cancer types, preventing or reversing inflammation is an important approach to cancer control.
Table 1.
Risk factor and inflammatory conditions correlated with cancer development, and estimated new case from Cancer Statistics, 2016 7.
| Cancer Type | Estimated new cases in 2016 | Risk factors correlated with inflammation |
|---|---|---|
| Pancreas | 53,070 | Cigarette smoking, chronic pancreatitis diabetes, obesity, Lynch syndrome |
| Lung & bronchus | 224,390 | Cigarette, cigar and pipe smoking, bronchitis. |
| Stomach | 26,370 | Helicobacter pylori (H. pylori) |
| Colon & rectum | 134,490 | obesity, physical inactivity, long-term smoking, alcohol consumption, chronic inflammatory bowel disease (e.g., ulcerative colitis or Crohn disease). |
| Esophagus | 16,910 | Reflux oesophagitis, Barret’s oesophagus |
| Lymphoma | 81,080 | Epstein-Barr virus, human immunodeficiency virus [HIV]. |
| Liver & intrahepatic bile duct | 39,230 | Hepatitis B virus (HBV) and/or hepatitis C virus (HCV), heavy alcohol consumption, obesity, diabetes, tobacco smoking, Cholangitis. |
| Melanoma of the skin | 76,380 | Skin inflammation. |
| Uterine cervix | 12,990 | human papillomavirus HPV |
| Uterine Corpus (Endometrium) | 60,050 | Obesity and abdominal fatness Lynch syndrome and diabetes. |
| Brest cancer | 246,660 | Obesity, long-term, heavy smoking, physical inactivity, and alcohol consumption. |
| Urinary Bladder | 76,960 | Smoking, Cystitis/Bladder Syndrome |
| Oral Cavity and Pharynx | 48,330 | Excessive alcohol consumption. HPV infection, tobacco use. |
| Kidney & renal pelvis | 62,700 | Obesity and tobacco smoking, chronic renal failure. |
| Leukemia | 60,140 | Obesity, Cigarette smoking, T-cell leukemia virus type I (HTLV-I) |
The major goal of cancer prevention that can be divided into primary, secondary and tertiary prevention is to reduce the risk of cancer occurrence or recurrence and disease complications after diagnosis(11). Avoiding exposure to known risk factors is an important means in primary prevention, since it has the potential to reduce the number of cancer deaths by 30%. In addition to screening procedures that detect pre-clinical pathological changes, other components of secondary prevention are chemoprevention and immunoprevention. The aim of immunoprevention is to control initiation or development of cancer by modulating the immune system, whereas chemoprevention entails the use of natural, synthetic, or biologic chemical agents to reverse, suppress, or prevent malignant progression to invasive cancer. Only a relatively small number of agents have been specifically approved for cancer chemoprevention, including the two anti-inflammatory drugs celecoxib and diclofenac, while for other medications, including aspirin and statins, commonly used to treat a variety of common, non-cancer-related medical situations, even if data are accumulating to support a significant negative association with cancer occurrence, at the current level of evidence their potential chemopreventive properties should be considered in high–risk situations or by using a personalized approach of maximizing individual benefits and minimizing the potential for adverse effects(12).
Preventable cancer risk factors
Obesity and cancer
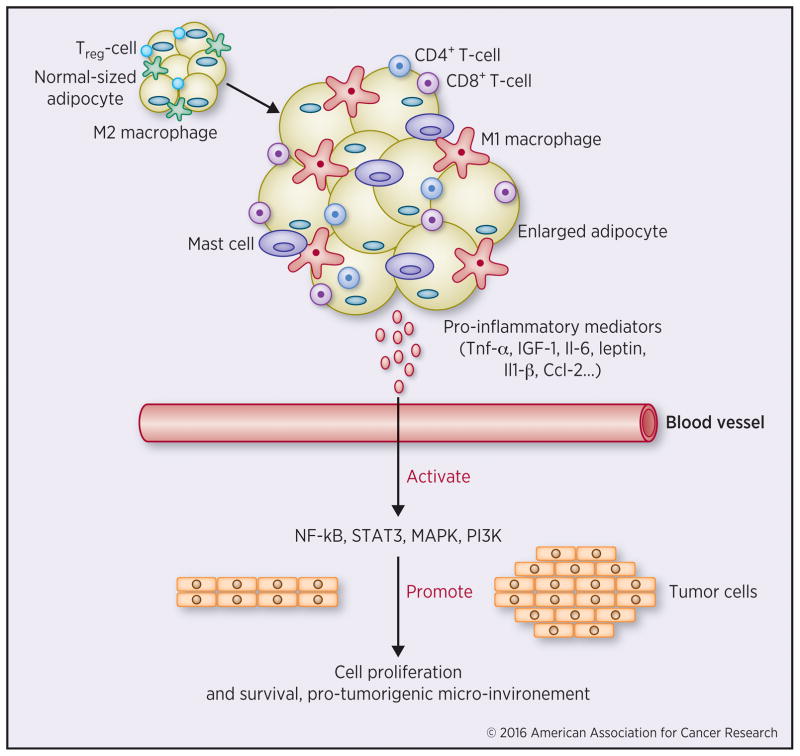
According to the World Health Organization’s 2014 report 39% adults worldwide are overweight and 13% are obese(13). Obese individuals are at a substantial elevated risk to develop cancer and at least 3.6% of all new cancer cases in adults over 30 years of age are obesity-related(14). There is a close relationship between obesity and inflammation, which led to the development of a new concept of “metaflammation” (15). Furthermore, the major mechanism through which obesity promotes cancer is inflammation related(16). A hallmark of obesity, adipocyte hypertrophy is characterized by changes in the abundance and type of mediators secreted by adipocytes. While lean adipocytes produce anti-inflammatory factors such as adiponectin, IL-4 and IL-10, adipocytes from obese individuals are a source of pro-inflammatory mediators including leptin, IL-1, IL-6 and TNF. These pro inflammatory adipokines initiate a cascade of changes that result in broader adipose tissue inflammation, characterized by proinflammatory macrophage infiltration, increased T cell proliferation, Th1 cell polarization and inhibition of Treg expansion (Figure 1). Furthermore, NK cells that produce IFNγ, mast cells and B cells accumulate in obese adipose tissue and impact subsequent systemic metabolic changes(17). In addition to systemic metabolic dysregulation, proinflammatory adipokines alter the tumor microenvironment and promote angiogenesis and cancer cell proliferation. For example, leptin and IL-6 secreted by obese adipocytes activate Janus kinases (JAK) and signal transducer and activator of transcription (STAT3) resulting in inhibition of apoptosis and increased VGEF secretion, which promotes tumor vascularization. STAT3 also stimulates cancer cell proliferation(18, 19). Metabolic dysfunction in obesity is also characterized by increased systemic concentrations of insulin and IGF-1, both of which stimulate cancer cell proliferation and enhance cancer growth(20). Furthermore, free fatty acids released from adipose tissue in obesity accumulate in the liver and lead to development of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatits (NASH), which increases the risk of hepatocellular carcinoma (HCC)(21). Weight loss in obese subjects reduces serum concentrations of inflammatory markers including C-reactive protein, IL-6, and TNF and decreases macrophage numbers in adipose tissue, liver and colon. Weight loss is also associated with reduced activity of tumor promoting transcription factors, including AP-1, STAT3 and NF-κB(18, 22–24). Bariatric surgery is commonly used for weight reduction in extremely obese individuals and was found to reduce cancer incidence and mortality(25). Therefore, weight loss represents an effective anti-inflammatory strategy proven to be effective for cancer prevention and control. Additional modulation of obesity-related inflammation is possible through the use of anti-inflammatory nutritional supplements such as omega-3 fatty acids, whose consumption ameliorates adipose tissue inflammation(26). By reducing the concentration of proinflammatory arachidonic acid (AA) metabolites, omega-3 fatty acids reduce the production of eicosanoids that can activate AP-1 and NF-κB signaling and promote angiogenesis(27). Recommendations made by the Joslin Diabetes Research Center at Harvard Medical School for the treatment of obesity stated that Omega-3 fatty acids should be taken twice a week using food sources such as fatty fish(28). Moreover, cholesterol-lowering and antidiabetic drugs, such as statins and metformin, respectively, that are often used in obese patients, have also shown beneficial effects in preventing some types of cancer(29).
Figure 1. Mechanisms linking obesity, inflammation and cancer.
In obesity, enlarged adipocytes secrete pro-inflammatory adipokines such as leptin, TNF-α, CCl-2 and IL-6 and localy induce an M1 macrophage phenotype. In addition to macrophages mast- and T-cells infiltrate adipose tissue in obesity and aggravate an inflammatory state. The adipose tissue-derived inflammatory mediators also exert their effects systemically and may activate inflammatory pathways such as NF-kB and STAT3 pathway in pre malignant and malignant cells and promote a microenvironment favorable for tumorigenesis.
In particular, metformin, commonly used as oral antihyperglycaemic drug and statins (3-hydroxy-3-methyl-glutaryl-coenzyme A (HMG-CoA) reductase inhibitors), was proposed to decrease the risk of hepatocellular carcinoma up to 50% and 60% respectively, modifying several steps of RAS/RAF/MEK/ERK, PI3K/AKT/mTOR and Wnt/β-catenin signaling(29).
Alcohol and cancer
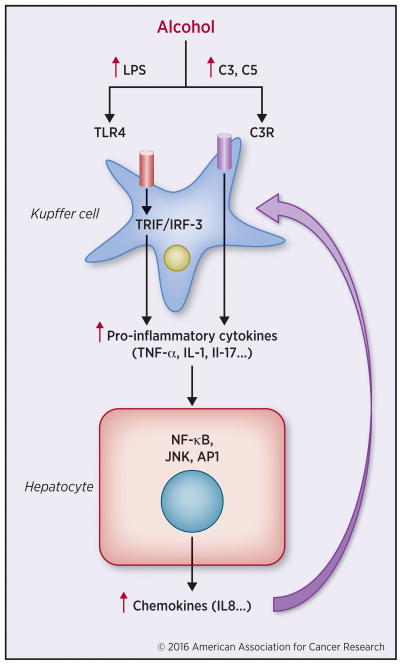
There is a strong association between alcohol consumption and increased risk of cancer especially head and neck, esophageal, breast, liver and pancreatic cancers(30–32). Much of the effort to date has focused on alcoholic liver disease (ALD), which accounts for 70% of alcohol related mortality(33). Alcohol intake leads to alcoholic steatohepatitis (ASH) (Figure 2), fibrosis and cirrhosis, eventually culminating in HCC(34). The mechanisms involved in the pathogenesis of ALD include endotoxin-induced liver damage, oxidative stress and inflammation(35). Several inflammatory cytokines including TNF, IL-1 and IL-6, all of which are tumor promoting(8), are elevated in ALD(36). All of these cytokines were found to promote HCC development and also contribute to the pathogenesis of pancreatic cancer(37). As shown in NASH-driven HCC(38), TNF antagonists may also inhibit the development of ASH-driven HCC(39), but in this case they can increase the risk of infection. A key mediator of ALD is lipopolysaccharide (LPS) released by Gram-negative bacilli in the gut and transported to the liver through the portal vein(40). LPS activates liver macrophages via TLR4 to produce tumor promoting cytokines, including TNF and IL-6 and activate hepatic stellate cells (HSC), which produce TGFβ, a potent immunosuppressive cytokine(41). By causing dysbiosis and destroying the gut permeability barrier, excessive alcohol consumption can also increase the risk of colorectal cancer(42, 43). Meta-analysis indicates that cessation of alcohol consumption decreases HCC risk by 6% to 7% a year(44). Excessive alcohol consumption is also a major etiological factor in chronic pancreatitis and pancreatic ductal adenocarcinoma (PDAC)(45, 46). Similar to its effects on liver cancer, alcohol-induced deterioration of the gut permeability barrier and LPS entry into the pancreas promote pancreatic inflammation and fibrosis(47), resulting in acinar-to ductal metaplasia, an initiating event in PDAC development. Therefore reducing alcohol consumption should significantly decrease the risk of some of the most aggressive cancers.
Figure 2. Inflammation in ALD.
Alcohol consumption increases gut permeability and facilitates translocation of bacteria-derived LPS from the gut to the liver. LPS activates TLR4-TRIF/IRF-3 pathway in Kupffer cells, which results in increased proinflammatory cytokine production subsequently leading to hepatocyte damage. Alcohol consumption also activates complement C3 and C5, which bind to the receptors on Kupffer cells and increase their TNF-α production, which leads to activation of NF-kB and other inflammatory pathways in hepatocytes and hepatocyte injury. In response to pro-inflammatory stimuli hepatocytes secrete chemokines to attract more inflammatory cells.
Tobacco smoking and cancer
Cigarette smoke induces the production and release of several inflammatory mediators(48–50) and activates signaling pathways involved in the regulation of inflammation, cell survival and cell proliferation(51). Importantly, tobacco smoke enhances Ras activity through activation of receptors for advanced glycation end-products (RAGE)(52). Elevated Ras activity, is a characteristic of several epithelial-derived cancers including lung and pancreatic cancers (53) and it induces downstream NF-κB activation and elevated expression of inflammatory cytokines and chemokines(52). In addition to NF-κB, ROS in tobacco smoke activate AP-1, which mediates IL-8 production, monocyte and macrophage activation and development of corticosteroid-resistant inflammation(54). Short term tobacco smoke exposure in mice, resulted in activation of IKKβ and JNK signaling and induction of inflammatory cytokines in myeloid cells and had a promoting effect on lung cancer development in mice(55). Importantly, IKKβ and JNK ablation reduced tobacco smoke-induced malignant cell proliferation and lung cancer promotion. Therefore, it is likely that anti-inflammatory intervention may slow down the development and progression of lung cancer. Anti-inflammatory therapy and smoking cessation could be useful in secondary prevention that attempts to address a disease at its earliest stage, such that prompt intervention may slow down disease progression or in a best case, stop it completely!
Microbiome, inflammation and cancer
Helicobacter pylori and hepatitis C virus are among the most-well described pathogens that promote cancer development (Table.1), both of which induce tumorigenesis through epithelial injury and inflammation(56). In addition to specific bacterial pathogens, global microbiota changes and imbalance can also promote tumor development(57). Activation of Toll like receptors (TLRs) by microbial products represents one of the strongest pro-inflammatory signals(58). Mice lacking TLR4, whose activation by LPS results in production of pro-inflammatory mediators, are protected against HCC, PDAC and inflammation-induced CRC development(57, 59, 60). TLR4, whose basal expression in the intestinal mucosa is low, is upregulated in patients with inflammatory bowel disease (IBD) that are at high risk of developing colitis-associated cancer (CAC)(60, 61). Therefore, TLR4 signaling blockade may be of value in prevention or treatment of several different inflammation-associated cancer types.
Localized loss of the intestinal epithelial barrier, resulting in increased translocation of commensal microbiota was found to activate an inflammatory IL-23/IL-17 cytokine cascade leading to accelerated colorectal tumorigenesis(9). Ablation of the NLRP6 inflammasome component resulted in dysbiosis and increased abundance of colitogenic bacteria that promote CRC development through a mechanism dependent on microbe-induced increase in CCL-5 secretion by epithelial cells, leading to subsequent infiltration of IL-6 producing immune cells and increased epithelial proliferation(62). However, the relationship between inflammation and the microbiota during tumorigenesis is not one-sided. For instance, IL-10-deficient mice that develop spontaneous colitis exhibit dysbiosis, which promotes development of CRC(63). Colitis may also exacerbate tumorigenesis by inducing the expansion of microorganisms with genotoxic capabilities(64). Such microorganisms are enriched in IBD patients as well as in CRC(64). Consumption of probiotics and prebiotics may exert some beneficial effects that can be used in cancer prevention(65). The World Health Organization (WHO) defines probiotics as “Live microorganisms that, when administered in adequate amounts, confer a health benefit on the host”(66). Prebiotics are “Selectively fermented ingredients that allow specific changes, both in the composition and/or activity in the gastrointestinal microflora that confers benefits upon host well-being and health” (67). Importantly, attenuated inflammation may be the major mechanism by which some pre- and probiotic organisms inhibit cancer development(68).
Exercise, inflammation and cancer prevention
Inflammatory disorders and cancer progression are characteristically associated with accumulation of distinctive genetic mutations, preceded by exposure to several risk factors, classified as non-modifiable (sex, age, presence of genetic mutations, ethnicity) and modifiable (specific behaviors, bad habits and lifestyle). For instance, exercise is beneficial both for cancer prevention and as supportive therapy for cancer patients that in addition to improving patients’ quality of life is capable of slowing down disease progression(69). The recruitment of lymphocytes to the blood stream after physical exertion was observed in 1893, by Schulte(69), and may account for reduction of risk of breast, colon, and prostate cancers(69, 70). During an acute bout of exercise, both epinephrine and norepinephrine drive NK cell mobilization, thereby enhancing anti-tumor immunity(71). Additionally muscle-derived factors, known as myokines, including IL-15, IL-7, and IL-6, can regulate NK cell proliferation, maturation, and activation(72).
Drugs, inflammation and cancer prevention
Nonsteroidal anti-inflammatory drugs
NSAIDs (including aspirin, ibuprofen, naproxen) use has been linked to reduced cancer risk(73). Acetylsalicylic acid (ASA), also known as aspirin, is one of the most widely used drugs in the world, particularly for prevention of cardiovascular diseases(74). Multiple clinical trials had demonstrated a link between long-term aspirin use and a reduction in the incidence and mortality for several cancer types with an overall effect of 20%–25%(73). The strongest beneficial effect has been found in esophageal adenocarcinoma, colorectal and stomach cancers and a smaller effect was observed in breast, lung and prostate cancers(73). No benefit was found for hematopoietic malignancies, pancreatic and endometrial cancer(73). Several possible mechanisms were suggested to explain the association between NSAID and aspirin use and cancer prevention including COX1/2 inhibition, immune response modulation, effect on the phosphatidylinositol-3-kinase (PI3K) signaling, inhibition of certain pro-inflammatory and pro-tumorigenic transcription factors, maintenance of cancer stem-cell homeostasis and decreased glycolytic rate in cancer cells(75). The mechanism of action of COX1/2 inhibition seems to be reduced production of inflammatory mediators such as prostaglandins and leukotrienes(76). Increased expression of COX2 and its major metabolite prostaglandin E2 (PGE2) has been observed in many different types of cancer in which they enhance angiogenesis, apoptosis resistance, tumor growth, and metastasis(77). PGE2 activates MAPK, PI3K-AKT and NF-κB signaling, and induces expression of several factors implied in tumorigenesis including VEGF, proto-oncogene Bcl-2, epidermal growth factor receptor (EGFR) and different matrix metalloproteinases (MMP-2 and MMP-9)(77). But NSAIDs may also act through different mechanisms including induction of apoptosis through cytochrome C release from mitochondria and subsequent activation of caspase-9 and -3, and/or interference with cell-cycle progression and inhibition of carcinogen activation and stimulation of immune surveillance(78). Recent studies show that epigenetic modifications may also be involved in the chemopreventive actions of ASA, leading to suppressed HDAC activity and increased H3K27 acetylation which results in reduced expression of iNOS, TNF and IL-6(74).
Nevertheless, long-term NSAID administration can result in side-effects including renal failure and gastrointestinal (GI) symptoms including: mucosal lesions, bleeding, peptic ulcer and intestinal inflammation which causes perforation and strictures in small and large intestines(79). Such adverse effects may actually increase cancer risk. Furthermore, NSAID intake increases the risk of deep vein thrombosis and its potentially life-threatening complications of pulmonary embolism, myocardial infarction and stroke(80). Several selective COX2 inhibitors that impair tumor growth and metastasis (celecoxib, rofecoxib, valdecoxib, apricoxib, etoricoxib, and lumiracoxib) were approved for marketing, but later withdrawn mostly due to increased risk of thromboembolic events. Celecoxib is the only selective COX-2 inhibitor that is still available in the US and Europe(81). Combining COX2 inhibitors with 5-LOX inhibitors can block synthesis of both prostaglandins and leukotrienes, resulting in reduced gastrointestinal toxicity(79). In this context, the herbal medicines including the natural hydro-alcoholic extract of Cordia myxa fruit is considerably effective in treatment of acute inflammation in rats, and the active ingredients of its seeds, such as alpha-amyrins, have anti-cancer and anti-inflammatory activities by inhibiting COX2 and 5-LOX(79).
Corticosteroids
Corticosteroids, most commonly used as anti-emetic drugs that prevent chemotherapy-induced nausea and vomiting, are the most effective anti-inflammatory drugs for many chronic inflammatory diseases and were shown to have anti–cancer activity(82). For example, pre-treatment with dexamethasone (DEX) increased effectiveness of chemotherapy in xenograft or syngeneic experimental tumor models of glioma, breast, lung and colon cancer(83). Dietary consumption of DEX has a chemopreventive effect in mice exposed to tobacco smoke, leading to decreased lung tumor incidence(84). Recent studies had shown that DEX in combination with carfilzomib and lenalidomide, significantly improved progression-free survival of patients with relapsed multiple myeloma(85), (ClinicalTrials.gov number, NCT01080391). In contrast high dose inhaled (ICS) and oral corticosteroid (OCS) treatment, used to reduce local and systemic inflammation in asthma and chronic obstructive pulmonary disease (COPD) patients, was found to increase the risk of squamous lung cell carcinoma in men(86).
Statins and metformin
Statins are a family of drugs that lower blood cholesterol concentration by blocking the 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, which results in impaired cholesterol synthesis and by enhancing cholesterol clearance from the circulation(87). In addition to its cholesterol-lowering effects statins also have anti-inflammatory properties(88), which makes them powerful agents in prevention of atherosclerosis and resulting life-threatening conditions, heart attack and stroke. Statins are able of reducing systemic pro-inflammatory cytokine and C reactive protein (CRP) levels and macrophage infiltration(89, 90). By exerting anti-inflammatory and other effects statins also reduce the risk of development of several cancer types including CRC, HCC and breast cancer(91–93). The proposed anti-tumoral mechanisms of statins are increased apoptosis due to downregulation of the RAF/MEK/ERK pathway, inhibition of degradation of cell cycle regulators p21 and p27, inhibition of c-Myc activation and inhibition of several key pro-inflammatory pathways including NF-κB and COX2(94). Metformin, a drug used for treatment of type 2 diabetes mellitus, was found to be associated with decreased incidence of a variety of cancer types including colon, breast, lung, prostate, ovarian, and pancreatic cancer(95). Its anti-neoplastic effect is mediated through activation of the AMPK pathway, which counteracts the pro-tumorigenic effect of hyperinsulinemia, the reduction of systemic glucose concentration, which counteracts Warburg effect and through its anti-inflammatory properties(96).
Targeting recruitment and polarization of tumor-associated macrophages (TAMs)
Macrophages, an essential component of the innate immune system in humans, can represent up to 50% of the tumor mass, which makes them an important part of the tumor stroma, where they are commonly referred to as tumor-associated macrophages (TAM). TAM can generally promote cancer cell proliferation, stimulate tumor angiogenesis and extracellular matrix breakdown, suppress anti-tumor immune responses and enhance tumor invasion and metastasis(97). Their recruitment into the tumor microenvironment from the blood stream, is primarily regulated by cytokines, chemokines, and growth factors that are derived from tumor and stromal cells. The tumor-derived C-C chemokine ligand 2 (CCL2), acting via its receptor C-C chemokine receptor 2 (CCR2), is a direct mediator of monocyte recruitment into primary tumors(98). TAM are classified as either classically activated M1 or alternatively activated M2 macrophages(99). The Th1 cytokine interferon-γ (IFN-γ) and LPS are the major inducers of the M1 phenotype, whereas Th2 cytokines, such as IL-4, IL-10 and IL-13, stimulate M2 polarization(100). During the course of tumor development the TAM phenotype is modulated by different factors in the tumor microenvironment and it changes from the M1 to the M2 phenotype, which is claimed to have stronger tumor promoting properties(101). M2 macrophages are associated with poor prognosis in many different cancer types and can promote cell cycle progression and angiogenesis while inhibiting apoptosis(102). However, the M1/M2 model is an oversimplified representation of the functional diversity of macrophages. In fact, M1 and M2 characteristics often coexist within the same cell and there is a broad variety of macrophage subtypes between the M1 and M2 poles(103). Furthermore, the most potent tumor promoting cytokines, such as IL-6, TNF, IL-1 and IL-23 are considered as M1 cytokines(104).
Due to their important role in linking inflammation and cancer, the targeting of TAM recruitment and differentiation, provides an opportunity for cancer prevention and treatment. Depletion of CCL2 with a neutralizing antibody prevents monocyte recruitment to the primary tumor site and reduces pulmonary metastasis of human breast cancer cells(105). A human anti-CCL2 antibody, CNTO 888, showed preliminary anti-tumor activity in patients while being well tolerated(106). Blockade of CCR2 with small-molecule antagonist showed anti-tumor activity in pancreatic cancer in animal studies(107) and this strategy is now being tested in clinical trials (ClinicalTrials.gov Identifier: NCT02732938). Trabectedin, a DNA-binding drug approved in Europe for the treatment of soft tissue sarcoma has been shown to selectively deplete mononuclear phagocytes in vivo, including TAM(106). Rapidly growing tumors often outgrow their blood supply, which results in formation of hypoxic areas with TAM accumulation(108). Binding of Semaphorin 3A to its receptor Neuropilin-1 (Nrp1) recruits TAM toward the hypoxic area where they adopt the M2 phenotype and release pro-angiogenic factors(106). Inhibition of Nrp1 reduced TAM migration and prevented their phenotypic switch to M2-like immunosuppressive cells with angiogenic activity making it an interesting target for anti-cancer therapy. Several therapies convert macrophages from an M2 to an M1 phenotype(109). Tasquinimod is a small-molecule compound that reduces the immune suppressive potential of the tumor microenvironment(110). A recent study demonstrated its ability to induce a shift of imunosuppresive M2 to pro-inflammatory M1 macrophages in colon and breast cancer models(111). Colony-stimulating factor 1 (CSF-1) and its receptor, CSF-1R, mediate migration, differentiation, and survival of macrophages(106). Treatment with anti-CSF-1R antibody resulted in TAM depletion in several tumor types in vitro and in vivo and a clinical benefit for patients with diffuse-type giant cell tumors(106). Importantly, CSF-1 triggers M2 phenotype in macrophages and treatment with anti-CSF-1R/GM-CSF antibodies resulted in their cell death(106). TAM express significant amounts of COX2 and the selective COX2 inhibitor celecoxib was shown to switch their phenotypic characteristics from M2- to M1-like, which was followed by a reduction in number of colon polyps in an animal study on colon cancer(112). Recent studies had shown that decreasing TAM survival, by the targeting folate receptor-β (FR-β), a marker for the M2-polarized phenotype, is another promising strategy against cancer, in an experimental glioma model(113).
Targeting pro-inflammatory pathways
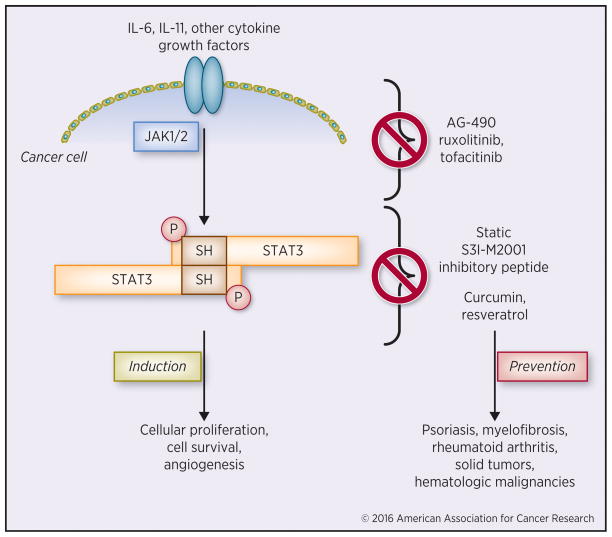
NF-κB and STAT3 are two critical transcription factors that are activated in many types of cancers(8, 114, 115). The STAT proteins family, which includes seven members, regulates multiple processes related to cellular proliferation, survival, and angiogenesis(116). Amongst the different STATs, the one most important for cancer is STAT3, whose activity is stimulated by IL-6, IL-11 and other members of their cytokine family, as well as different growth factors(117). In HCC and liver adenomas STAT3 activity is stimulated by various oncogenic mutations(118), but more often than not STAT3 is maintained in an activated state due to elevated production of IL-6 and other cytokines(117). STAT3 signaling also has important roles in tumor microenvironment where it promotes IL-23-mediated, pro-tumorigenic immune responses while inhibiting expression of anti-tumorigenic IL-12(119). Inhibition or ablation of STAT3 can mediate tumor regression(120). Therefore, inhibition of STAT3 provides a rational strategy to block carcinogenesis at an early stage and induce regression of established tumors.
There are three major approaches to inhibit STAT3 signaling: inhibition of tyrosine kinases, such as JAK1 and 2, that are responsible for STAT3 activation (AG- 490, ruxolitinib, etc.), STAT3 dimerization inhibitors that target its SH2 domain (Static, S3I-M2001, STAT3 inhibitory peptide, etc.) and non-specific compounds that indirectly inhibit STAT3, such as resveratrol and curcumin, which inhibit many other targets(116) (Figure 3). Among tyrosine kinase inhibitors some are rather specific for JAK2 family members, while others inhibit several different kinases that lead to STAT3 activation(116). JAK inhibitors have already been tested in several clinical trials mostly for hematological/oncological and inflammatory diseases and some of them such as Ruxolitinib and Tofacitinib have been approved for use in psoriasis, myelofibrosis and rheumatoid arthritis(121, 122). Currently, these drugs are being evaluated as neo-adjuvants in several types of cancer, including pediatric refractory or recurrent solid tumors, hematologic malignancies (HMs)(123), pancreatic adenocarcinoma, triple-negative breast cancer, urothelial cancer, multiple myeloma, acute myeloid leukemia, myelodysplastic syndrome lymphoma (ClinicalTrials.gov number, NCT02265510), endometrial cancer, gastric cancer, head and neck squamous cell carcinoma, melanoma, microsatellite unstable colorectal cancer, non-small cell lung cancer (ClinicalTrials.gov number, NCT02559492, NCT02646748) and estrogen-receptor positive Invasive Metastatic Breast Cancer (ClinicalTrials.gov number, NCT01594216). Despite their clinical approval and marketing in myelofibrosis and rheumatoid arthritis, JAK inhibitors exert rather serious side effects including anemia, thromobocytopenia, headaches, nausea and neurotoxicity(124). However, more selective inhibitors with fewer side effects are currently being developed. Yet, it is doubtful whether such agents will ever find use in cancer prevention.
Figure 3. Targeting STAT3 pro-inflammatory pathway.
Schematic representation of the major targetable events during STAT3 activation, and the corresponding compounds with cancer-preventive properties.
The NF-κB pathway is constitutively activated in many cancers, both in malignant cells and in components of the tumor microenviroment(115). NF-κB activation in malignant cells increases the expression of genes, whose products promote cell survival and proliferation, whereas NF-κB activation in components of the tumor stroma increases expression of inflammatory cytokines and growth factors(8, 115). NF-κB activation also promotes epithelial to mesenchymal transition (EMT) and tumor angiogenesis(125). Although NF-κB activation plays a major role in the induction of inflammation, long term and extensive inhibition of NF-κB can result in profound inflammation due to enhanced production of IL-1β upon activation of the NLRP3 inflammasome(126). This can result in severe neutrophilia(127), a serious condition that led to termination of any further clinical development. Nonetheless, the cancer prevention literature is full of reports using natural anti-inflammatory agents, including curcumin, resveratrol, ursolic acid, capsaicin, silibinin, silymarin, guggulsterone, and plumbagin, all of which are claimed to act as NF-κB inhibitors(128–132). Most likely, however, these are rather mild and non-specific NF-κB inhibitors, most of which affect multiple targets, including STAT3. Due to their rather mild effects, such agents, many of which are used as nutritional supplements, can be used in cancer prevention(133), but it is doubtful whether they will ever find use as anti-cancer drugs.
The major problem associated with NF-κB inhibition is enhanced activation of the NLRP3 inflammasome(126). The inflammasome is a multimeric complex consisting of the intracellular Nod-like receptors (NLRs) and the adaptor protein ASC that serves as a platform for activation of caspase 1(134). Inflammasomes have a crucial role in host defense against infection as well as various autoinflammatory conditions(135). Upon NLR oligomerization and subsequent interaction between the adaptor protein ASC and the CARD domain, caspase-1 mediated processing results in production of the proinflammatory cytokines IL-1β and IL-18 or a rapid inflammatory form of cell death called pyroptosis(126). NF-κB is the first signal that primes NLR and pro-IL-1β expression(136), but persistent NF-κB activation is also responsible for dysregulated NLRP3 inflammasome activation by inducing the mitophagic clearance of damaged mitochondria(126).
The role of NLR containing inflammasomes in mediating cancer initiation and progression by creating a pro-inflammatory microenvironment for inducing malignant transformation and suppression of local immunity caused by NK or T cells, open the way for novel strategy in cancer prevention. Between the 22 NLRs in the human and the 34 NLRs in the mouse genome, NLRP3 (NLR family, pyrin domain containing 3) is the best characterized. The NLRP3 inflammasome plays an important role in several inflammatory disorders including IBD(137), and its activation is negatively regulated by selective mitochondrial autophagy (mitophagy)(126), whose dysregulation promotes inflammatory diseases, including pancreatitis(138, 139) and may increase cancer risk(140). The natural diterpenoid Andrographolide (Andro), which was approved in China for the treatment of various inflammatory conditions, inhibit tumor growth in mice at a high dose (about 200 mg/kg), and attenuates colitis progression and prevents carcinogenesis by inhibiting NLRP3 activity and stimulating autophagy(135).
Cytokines as targets for cancer prevention and therapy
The complex of IL-6 and its nonsignaling receptor (IL-6R) binds glycoprotein 130 (gp130) that forms a dimer, which results in activation of the JAK/STAT pathway and induces expression of other inflammatory cytokines and suppresses apoptosis(141). During tumorigenesis IL-6 has served detrimental effects including stimulation of cell survival and proliferation, regulation of stem cell renewal and induction of angiogenesis. A humanized anti–IL-6 receptor monoclonal antibody Toclizumab is an FDA-approved immunosuppressive drug that blocks IL-6 signaling. It is used in the treatment of rheumatoid arthritis and systemic juvenile idiopathic arthritis(142). Chimeric monoclonal antibody Siltuximab that binds IL-6 showed good tolerance in cancer patients in a phase I clinical trial and is currently investigated for the treatment of several tumor types including prostate cancer and metastatic renal cell cancer(142). Long-term treatment with anti-IL-6-blocking antibody was associated with very few side effects in a mouse model of pancreatic cancer prevention(142). Thus, IL-6 emerges as a promising potential target for cancer prevention. The proinflammatory chemokine IL-8 and its receptors CXCR1 and CXCR2 were also linked to cancer and inflammation(142). Treatment with monoclonal antibodies, siRNA or small molecule inhibitors of IL-8 or CXCR1/2 reduced tumor growth in pre-clinical studies, which makes them attractive targets for cancer prevention and therapy. A combination therapy with a small molecule inhibitor of CXCR1/2 activation (reparixin) and paclitaxel in HER-2 negative breast cancer patients is a major clinical study currently conducted(142). Another proinflammatory cytokine with reported role in promoting tumorigenesis is IL-17A(143). TGF-β and IL-6 are needed for the differentiation and IL-23 for the maintenance of T helper 17 cells (Th17) that produce IL-17A. Antibodies against IL-17A (ixekizumab and secukinumab) and its receptor IL17AR (brodalumab) are in clinical trials for chronic inflammatory conditions and autoimmune diseases and an anti-IL23 antibody ustekinumab was FDA approved for the treatment of psoriatic arthritis(144). However, preventive application of such drugs should take in account reported antitumor effects of IL-17 in established tumors(144) as well as its role in autoimmunity.
Immunoprevention meets inflammation
Vaccines that protect against certain viral infection play important role in cancer prevention. For instance hepatitis B virus (HBV) is a major cause of HCC whose impact has been dramatically reduced in all countries due to massive vaccination efforts(145). The most effective way to prevent HBV infection and reduce HCC development is vaccination(146). The prophylactic vaccine that is currently in use is generated by recombinant DNA technology and contains HBsAg protein and adjuvants. For patients who have already been infected by HBV and developed chronic hepatitis, secondary prevention becomes more important. Currently antiviral drugs used in patients with chronic hepatitis B include the immunomodulator pegylated IFN-α and oral nucleos(t)ide analogues(147). IFNs activate various IRF family members that regulates transcription of numerous targets, including genes involved in control of viral mRNA translation or degradation(147). However, the mechanism of IFN-α-mediated cell protection against viral infection is not fully understood. In addition to HBV, hepatitis C virus (HCV) is another important cause of HCC, against which there is no preventive vaccine(148). However, the recent development of highly effective anti-HCV drugs will lead to major decrease in HCV-induced HCC(148). Human papilloma virus (HPV) is a major cause of cervical intraepithelial neoplasia that can progress to invasive cervical cancer(149). Recently we have witnessed the development of an effective HPV vaccine that if properly distributed amongst young adults, will lead to a major decrease in the impact of cervical and other urogenital cancers. In summary vaccination against cancer causing viruses is one of the most effective and economical ways to reduce the toll of several inflammation-related cancers.
Acknowledgments
Financial support: J.T. was supported by the Erwin Schroedinger Fellowship from the Austrian Science Fund (J3233) and Univ. Prof. Dr. 17 Matthias M. Müller Fellowship from the Austrian Association for Laboratory Medicine and Clinical Chemistry (ÖGLMKC) and the Austrian Program for Advanced Research and Technology of the Austrian Academy of Sciences. LA was supported by the International Cancer Research Fellowship (iCARE), AIRC (Associazione Italiana per la ricerca sul cancro) co-founded by the European Union. M.K. was supported by grants from the NIH grants (CA163798) and the Lustgarten Foundation (RFP-B-007) to M.K. who holds the Ben and Wanda Hildyard Chair for Mitochondrial and Metabolic Diseases and is an American Cancer Society Research Professor.
Footnotes
The authors declare no potential conflicts of interest.
References
- 1.Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357:539–545. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt A, Weber OF. In memoriam of Rudolf virchow: a historical retrospective including aspects of inflammation, infection and neoplasia. Contrib Microbiol. 2006;13:1–15. doi: 10.1159/000092961. [DOI] [PubMed] [Google Scholar]
- 3.Norling LV, Serhan CN. Profiling in resolving inflammatory exudates identifies novel anti-inflammatory and pro-resolving mediators and signals for termination. J Intern Med. 2010;268:15–24. doi: 10.1111/j.1365-2796.2010.02235.x. [DOI] [PubMed] [Google Scholar]
- 4.Karin M, Clevers H. Reparative inflammation takes charge of tissue regeneration. Nature. 2016;529:307–315. doi: 10.1038/nature17039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maeda H, Akaike T. Nitric oxide and oxygen radicals in infection, inflammation, and cancer. Biochemistry (Mosc) 1998;63:854–865. [PubMed] [Google Scholar]
- 6.Shaked H, Hofseth LJ, Chumanevich A, Chumanevich AA, Wang J, Wang Y, et al. Chronic epithelial NF-kappaB activation accelerates APC loss and intestinal tumor initiation through iNOS up-regulation. Proc Natl Acad Sci U S A. 2012;109:14007–14012. doi: 10.1073/pnas.1211509109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 8.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140:883–899. doi: 10.1016/j.cell.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grivennikov SI, Wang K, Mucida D, Stewart CA, Schnabl B, Jauch D, et al. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature. 2012;491:254–258. doi: 10.1038/nature11465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang K, Kim MK, Di Caro G, Wong J, Shalapour S, Wan J, et al. Interleukin-17 receptor a signaling in transformed enterocytes promotes early colorectal tumorigenesis. Immunity. 2014;41:1052–1063. doi: 10.1016/j.immuni.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spratt JS. The primary and secondary prevention of cancer. J Surg Oncol. 1981;18:219–230. doi: 10.1002/jso.2930180302. [DOI] [PubMed] [Google Scholar]
- 12.Gronich N, Rennert G. Beyond aspirin-cancer prevention with statins, metformin and bisphosphonates. Nat Rev Clin Oncol. 2013;10:625–642. doi: 10.1038/nrclinonc.2013.169. [DOI] [PubMed] [Google Scholar]
- 13.WorldHealthOrgan. Obesity and Overweight. Geneva: WHO Media Centre; 2015. http://who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
- 14.Arnold M, Pandeya N, Byrnes G, Renehan AG, Stevens GA, Ezzati M, et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol. 2015;16:36–46. doi: 10.1016/S1470-2045(14)71123-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 16.Font-Burgada J, Sun B, Karin M. Obesity and Cancer: The Oil that Feeds the Flame. Cell Metab. 2016;23:48–62. doi: 10.1016/j.cmet.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 17.McNelis JC, Olefsky JM. Macrophages, immunity, and metabolic disease. Immunity. 2014;41:36–48. doi: 10.1016/j.immuni.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Park EJ, Lee JH, Yu GY, He G, Ali SR, Holzer RG, et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell. 2010;140:197–208. doi: 10.1016/j.cell.2009.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.He G, Yu GY, Temkin V, Ogata H, Kuntzen C, Sakurai T, et al. Hepatocyte IKKbeta/NF-kappaB inhibits tumor promotion and progression by preventing oxidative stress-driven STAT3 activation. Cancer Cell. 2010;17:286–297. doi: 10.1016/j.ccr.2009.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollak M. Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer. 2008;8:915–928. doi: 10.1038/nrc2536. [DOI] [PubMed] [Google Scholar]
- 21.Kew MC. Obesity as a cause of hepatocellular carcinoma. Ann Hepatol. 2015;14:299–303. [PubMed] [Google Scholar]
- 22.Pendyala S, Neff LM, Suarez-Farinas M, Holt PR. Diet-induced weight loss reduces colorectal inflammation: implications for colorectal carcinogenesis. Am J Clin Nutr. 2011;93:234–242. doi: 10.3945/ajcn.110.002683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bai Y, Sun Q. Macrophage recruitment in obese adipose tissue. Obes Rev. 2015;16:127–136. doi: 10.1111/obr.12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Font-Burgada J, Beicheng S, Karin M. Obesity and Cancer: The Oil that Feeds the Flame. Cell Metab. 2016;23:48–62. doi: 10.1016/j.cmet.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 25.Sjostrom L, Gummesson A, Sjostrom CD, Narbro K, Peltonen M, Wedel H, et al. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol. 2009;10:653–662. doi: 10.1016/S1470-2045(09)70159-7. [DOI] [PubMed] [Google Scholar]
- 26.Todoric J, Loffler M, Huber J, Bilban M, Reimers M, Kadl A, et al. Adipose tissue inflammation induced by high-fat diet in obese diabetic mice is prevented by n-3 polyunsaturated fatty acids. Diabetologia. 2006;49:2109–2119. doi: 10.1007/s00125-006-0300-x. [DOI] [PubMed] [Google Scholar]
- 27.Sears DD, Miles PD, Chapman J, Ofrecio JM, Almazan F, Thapar D, et al. 12/15-lipoxygenase is required for the early onset of high fat diet-induced adipose tissue inflammation and insulin resistance in mice. PLoS One. 2009;4:e7250. doi: 10.1371/journal.pone.0007250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guidelines, JDRCD. https://www.joslin.org/docs/Nutrition_Guideline_Graded.pdf.
- 29.Ampuero J, Romero-Gomez M. Prevention of hepatocellular carcinoma by correction of metabolic abnormalities: Role of statins and metformin. World J Hepatol. 2015;7:1105–1111. doi: 10.4254/wjh.v7.i8.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hashibe M, Brennan P, Chuang SC, Boccia S, Castellsague X, Chen C, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev. 2009;18:541–550. doi: 10.1158/1055-9965.EPI-08-0347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grewal P, Viswanathen VA. Liver cancer and alcohol. Clin Liver Dis. 2012;16:839–850. doi: 10.1016/j.cld.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 32.Hamajima N, Hirose K, Tajima K, Rohan T, Calle EE, Heath CW, Jr, et al. Alcohol, tobacco and breast cancer--collaborative reanalysis of individual data from 53 epidemiological studies, including 58,515 women with breast cancer and 95,067 women without the disease. Br J Cancer. 2002;87:1234–1245. doi: 10.1038/sj.bjc.6600596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sheron N, Hawkey C, Gilmore I. Projections of alcohol deaths--a wake-up call. Lancet. 2011;377:1297–1299. doi: 10.1016/S0140-6736(11)60022-6. [DOI] [PubMed] [Google Scholar]
- 34.Crawford JM. Histologic findings in alcoholic liver disease. Clin Liver Dis. 2012;16:699–716. doi: 10.1016/j.cld.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 35.Bataller R, Gao B. Liver fibrosis in alcoholic liver disease. Semin Liver Dis. 2015;35:146–156. doi: 10.1055/s-0035-1550054. [DOI] [PubMed] [Google Scholar]
- 36.Khoruts A, Stahnke L, McClain CJ, Logan G, Allen JI. Circulating tumor necrosis factor, interleukin-1 and interleukin-6 concentrations in chronic alcoholic patients. Hepatology. 1991;13:267–276. [PubMed] [Google Scholar]
- 37.Li N, Grivennikov SI, Karin M. The unholy trinity: inflammation, cytokines, and STAT3 shape the cancer microenvironment. Cancer Cell. 2011;19:429–431. doi: 10.1016/j.ccr.2011.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakagawa H, Umemura A, Taniguchi K, Font-Burgada J, Dhar D, Ogata H, et al. ER stress cooperates with hypernutrition to trigger TNF-dependent spontaneous HCC development. Cancer Cell. 2014;26:331–343. doi: 10.1016/j.ccr.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.European Association for the Study of L. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146:1513–1524. doi: 10.1053/j.gastro.2014.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Watanabe A, Sohail MA, Gomes DA, Hashmi A, Nagata J, Sutterwala FS, et al. Inflammasome-mediated regulation of hepatic stellate cells. Am J Physiol Gastrointest Liver Physiol. 2009;296:G1248–1257. doi: 10.1152/ajpgi.90223.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Purohit V, Bode JC, Bode C, Brenner DA, Choudhry MA, Hamilton F, et al. Alcohol, intestinal bacterial growth, intestinal permeability to endotoxin, and medical consequences: summary of a symposium. Alcohol. 2008;42:349–361. doi: 10.1016/j.alcohol.2008.03.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsuruya A, Kuwahara A, Saito Y, Yamaguchi H, Tsubo T, Suga S, et al. Ecophysiological consequences of alcoholism on human gut microbiota: implications for ethanol-related pathogenesis of colon cancer. Sci Rep. 2016;6:27923. doi: 10.1038/srep27923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Heckley GA, Jarl J, Asamoah BO, UGG How the risk of liver cancer changes after alcohol cessation: a review and meta-analysis of the current literature. BMC Cancer. 2011;11:446. doi: 10.1186/1471-2407-11-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lang MB, Segersvard R, Grundsten M, Segerdahl M, Arnelo U, Permert J, et al. Management of alcohol use disorders in patients with chronic pancreatitis. JOP. 2012;13:654–659. doi: 10.6092/1590-8577/1037. [DOI] [PubMed] [Google Scholar]
- 46.Duell EJ. Epidemiology and potential mechanisms of tobacco smoking and heavy alcohol consumption in pancreatic cancer. Mol Carcinog. 2012;51:40–52. doi: 10.1002/mc.20786. [DOI] [PubMed] [Google Scholar]
- 47.Gu H, Fortunato F, Bergmann F, Buchler MW, Whitcomb DC, Werner J. Alcohol exacerbates LPS-induced fibrosis in subclinical acute pancreatitis. Am J Pathol. 2013;183:1508–1517. doi: 10.1016/j.ajpath.2013.07.023. [DOI] [PubMed] [Google Scholar]
- 48.Mio T, Romberger DJ, Thompson AB, Robbins RA, Heires A, Rennard SI. Cigarette smoke induces interleukin-8 release from human bronchial epithelial cells. Am J Respir Crit Care Med. 1997;155:1770–1776. doi: 10.1164/ajrccm.155.5.9154890. [DOI] [PubMed] [Google Scholar]
- 49.Kode A, Yang SR, Rahman I. Differential effects of cigarette smoke on oxidative stress and proinflammatory cytokine release in primary human airway epithelial cells and in a variety of transformed alveolar epithelial cells. Respir Res. 2006;7:132. doi: 10.1186/1465-9921-7-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pace E, Ferraro M, Siena L, Melis M, Montalbano AM, Johnson M, et al. Cigarette smoke increases Toll-like receptor 4 and modifies lipopolysaccharide-mediated responses in airway epithelial cells. Immunology. 2008;124:401–411. doi: 10.1111/j.1365-2567.2007.02788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee J, Taneja V, Vassallo R. Cigarette smoking and inflammation: cellular and molecular mechanisms. J Dent Res. 2012;91:142–149. doi: 10.1177/0022034511421200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reynolds PR, Kasteler SD, Schmitt RE, Hoidal JR. Receptor for advanced glycation end-products signals through Ras during tobacco smoke-induced pulmonary inflammation. Am J Respir Cell Mol Biol. 2011;45:411–418. doi: 10.1165/rcmb.2010-0231OC. [DOI] [PubMed] [Google Scholar]
- 53.Bos JL. ras oncogenes in human cancer: a review. Cancer Res. 1989;49:4682–4689. [PubMed] [Google Scholar]
- 54.Walters MJ, Paul-Clark MJ, McMaster SK, Ito K, Adcock IM, Mitchell JA. Cigarette smoke activates human monocytes by an oxidant-AP-1 signaling pathway: implications for steroid resistance. Mol Pharmacol. 2005;68:1343–1353. doi: 10.1124/mol.105.012591. [DOI] [PubMed] [Google Scholar]
- 55.Takahashi H, Ogata H, Nishigaki R, Broide DH, Karin M. Tobacco smoke promotes lung tumorigenesis by triggering IKKbeta- and JNK1-dependent inflammation. Cancer Cell. 2010;17:89–97. doi: 10.1016/j.ccr.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Peek RM, Jr, Blaser MJ. Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat Rev Cancer. 2002;2:28–37. doi: 10.1038/nrc703. [DOI] [PubMed] [Google Scholar]
- 57.Dapito DH, Mencin A, Gwak GY, Pradere JP, Jang MK, Mederacke I, et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4. Cancer Cell. 2012;21:504–516. doi: 10.1016/j.ccr.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moresco EM, LaVine D, Beutler B. Toll-like receptors. Curr Biol. 2011;21:R488–493. doi: 10.1016/j.cub.2011.05.039. [DOI] [PubMed] [Google Scholar]
- 59.Ochi A, Nguyen AH, Bedrosian AS, Mushlin HM, Zarbakhsh S, Barilla R, et al. MyD88 inhibition amplifies dendritic cell capacity to promote pancreatic carcinogenesis via Th2 cells. J Exp Med. 2012;209:1671–1687. doi: 10.1084/jem.20111706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fukata M, Chen A, Vamadevan AS, Cohen J, Breglio K, Krishnareddy S, et al. Toll-like receptor-4 promotes the development of colitis-associated colorectal tumors. Gastroenterology. 2007;133:1869–1881. doi: 10.1053/j.gastro.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Di Caro G, Marchesi F, Laghi L, Grizzi F. Immune cells: plastic players along colorectal cancer progression. J Cell Mol Med. 2013;17:1088–1095. doi: 10.1111/jcmm.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hu B, Elinav E, Huber S, Strowig T, Hao L, Hafemann A, et al. Microbiota-induced activation of epithelial IL-6 signaling links inflammasome-driven inflammation with transmissible cancer. Proc Natl Acad Sci U S A. 2013;110:9862–9867. doi: 10.1073/pnas.1307575110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Arthur JC, Perez-Chanona E, Muhlbauer M, Tomkovich S, Uronis JM, Fan TJ, et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 2012;338:120–123. doi: 10.1126/science.1224820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sears CL, Garrett WS. Microbes, microbiota, and colon cancer. Cell Host Microbe. 2014;15:317–328. doi: 10.1016/j.chom.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ambalam P, Raman M, Purama RK, Doble M. Probiotics, prebiotics and colorectal cancer prevention. Best Pract Res Clin Gastroenterol. 2016;30:119–131. doi: 10.1016/j.bpg.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 66.FAO/WHO. Report of a Joint FAO/WHO Expert Consultation on Evaluation of Health, and Nutritional Properties of Probiotics in Food Including Powder Milk with Live Lactic Acid Bacteria. Córdoba: Food and Agriculture Organization of the United Nations, World Health Organization; 2001. [Google Scholar]
- 67.Roberfroid M. Prebiotics: the concept revisited. J Nutr. 2007;137:830S–837S. doi: 10.1093/jn/137.3.830S. [DOI] [PubMed] [Google Scholar]
- 68.Kuo SM. The interplay between fiber and the intestinal microbiome in the inflammatory response. Adv Nutr. 2013;4:16–28. doi: 10.3945/an.112.003046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Idorn M, Hojman P. Exercise-Dependent Regulation of NK Cells in Cancer Protection. Trends Mol Med. 2016;22:565–577. doi: 10.1016/j.molmed.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 70.Friedenreich CM, Neilson HK, Farris MS, Courneya KS. Physical Activity and Cancer Outcomes: A Precision Medicine Approach. Clin Cancer Res. 2016 doi: 10.1158/1078-0432.CCR-16-0067. [DOI] [PubMed] [Google Scholar]
- 71.Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117:1175–1183. doi: 10.1172/JCI31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pedersen L, Idorn M, Olofsson GH, Lauenborg B, Nookaew I, Hansen RH, et al. Voluntary Running Suppresses Tumor Growth through Epinephrine- and IL-6-Dependent NK Cell Mobilization and Redistribution. Cell Metab. 2016;23:554–562. doi: 10.1016/j.cmet.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 73.Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW. Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet. 2011;377:31–41. doi: 10.1016/S0140-6736(10)62110-1. [DOI] [PubMed] [Google Scholar]
- 74.Guo Y, Liu Y, Zhang C, Su ZY, Li W, Huang MT, et al. The epigenetic effects of aspirin: the modification of histone H3 lysine 27 acetylation in the prevention of colon carcinogenesis in azoxymethane- and dextran sulfate sodium-treated CF-1 mice. Carcinogenesis. 2016;37:616–624. doi: 10.1093/carcin/bgw042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schror K. Pharmacology and cellular/molecular mechanisms of action of aspirin and non-aspirin NSAIDs in colorectal cancer. Best Pract Res Clin Gastroenterol. 2011;25:473–484. doi: 10.1016/j.bpg.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 76.Allaj V, Guo C, Nie D. Non-steroid anti-inflammatory drugs, prostaglandins, and cancer. Cell Biosci. 2013;3:8. doi: 10.1186/2045-3701-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ghosh N, Chaki R, Mandal V, Mandal SC. COX-2 as a target for cancer chemotherapy. Pharmacol Rep. 2010;62:233–244. doi: 10.1016/s1734-1140(10)70262-0. [DOI] [PubMed] [Google Scholar]
- 78.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ranjbar MM, Assadolahi V, Yazdani M, Nikaein D, Rashidieh B. Virtual Dual inhibition of COX-2/5-LOX enzymes based on binding properties of alpha-amyrins, the anti-inflammatory compound as a promising anti-cancer drug. EXCLI J. 2016;15:238–245. doi: 10.17179/excli2016-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011;8:e1001098. doi: 10.1371/journal.pmed.1001098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Grosch S, Maier TJ, Schiffmann S, Geisslinger G. Cyclooxygenase-2 (COX-2)-independent anticarcinogenic effects of selective COX-2 inhibitors. J Natl Cancer Inst. 2006;98:736–747. doi: 10.1093/jnci/djj206. [DOI] [PubMed] [Google Scholar]
- 82.Rayburn ER, Ezell SJ, Zhang R. Anti-Inflammatory Agents for Cancer Therapy. Mol Cell Pharmacol. 2009;1:29–43. doi: 10.4255/mcpharmacol.09.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang H, Li M, Rinehart JJ, Zhang R. Pretreatment with dexamethasone increases antitumor activity of carboplatin and gemcitabine in mice bearing human cancer xenografts: in vivo activity, pharmacokinetics, and clinical implications for cancer chemotherapy. Clin Cancer Res. 2004;10:1633–1644. doi: 10.1158/1078-0432.ccr-0829-3. [DOI] [PubMed] [Google Scholar]
- 84.Witschi H, Espiritu I, Ly M, Uyeminami D. The chemopreventive effects of orally administered dexamethasone in Strain A/J mice following cessation of smoke exposure. Inhal Toxicol. 2005;17:119–122. doi: 10.1080/08958370590899712. [DOI] [PubMed] [Google Scholar]
- 85.Stewart AK, Rajkumar SV, Dimopoulos MA, Masszi T, Spicka I, Oriol A, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372:142–152. doi: 10.1056/NEJMoa1411321. [DOI] [PubMed] [Google Scholar]
- 86.Jian ZH, Huang JY, Lin FC, Nfor ON, Jhang KM, Ku WY, et al. The use of corticosteroids in patients with COPD or asthma does not decrease lung squamous cell carcinoma. BMC Pulm Med. 2015;15:154. doi: 10.1186/s12890-015-0153-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Istvan ES, Deisenhofer J. Structural mechanism for statin inhibition of HMG-CoA reductase. Science. 2001;292:1160–1164. doi: 10.1126/science.1059344. [DOI] [PubMed] [Google Scholar]
- 88.Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005;4:977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 89.Massey RU. Reflections from the Dean’s office. Conn Med. 1976;40:212. [PubMed] [Google Scholar]
- 90.Schonbeck U, Libby P. Inflammation, immunity, and HMG-CoA reductase inhibitors: statins as antiinflammatory agents? Circulation. 2004;109:II18–26. doi: 10.1161/01.CIR.0000129505.34151.23. [DOI] [PubMed] [Google Scholar]
- 91.Tsan YT, Lee CH, Ho WC, Lin MH, Wang JD, Chen PC. Statins and the risk of hepatocellular carcinoma in patients with hepatitis C virus infection. J Clin Oncol. 2013;31:1514–1521. doi: 10.1200/JCO.2012.44.6831. [DOI] [PubMed] [Google Scholar]
- 92.Poynter JN, Gruber SB, Higgins PD, Almog R, Bonner JD, Rennert HS, et al. Statins and the risk of colorectal cancer. N Engl J Med. 2005;352:2184–2192. doi: 10.1056/NEJMoa043792. [DOI] [PubMed] [Google Scholar]
- 93.Bonovas S, Filioussi K, Tsavaris N, Sitaras NM. Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol. 2005;23:8606–8612. doi: 10.1200/JCO.2005.02.7045. [DOI] [PubMed] [Google Scholar]
- 94.Park JH, McMillan DC, Horgan PG, Roxburgh CS. The impact of anti-inflammatory agents on the outcome of patients with colorectal cancer. Cancer Treat Rev. 2014;40:68–77. doi: 10.1016/j.ctrv.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 95.Sehdev A, O’Neil BH. The Role of Aspirin, Vitamin D, Exercise, Diet, Statins, and Metformin in the Prevention and Treatment of Colorectal Cancer. Curr Treat Options Oncol. 2015;16:43. doi: 10.1007/s11864-015-0359-z. [DOI] [PubMed] [Google Scholar]
- 96.Bost F, Sahra IB, Le Marchand-Brustel Y, Tanti JF. Metformin and cancer therapy. Curr Opin Oncol. 2012;24:103–108. doi: 10.1097/CCO.0b013e32834d8155. [DOI] [PubMed] [Google Scholar]
- 97.Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Shi C, Pamer EG. Monocyte recruitment during infection and inflammation. Nat Rev Immunol. 2011;11:762–774. doi: 10.1038/nri3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Davies LC, Jenkins SJ, Allen JE, Taylor PR. Tissue-resident macrophages. Nat Immunol. 2013;14:986–995. doi: 10.1038/ni.2705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25:677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 101.Chanmee T, Ontong P, Konno K, Itano N. Tumor-associated macrophages as major players in the tumor microenvironment. Cancers (Basel) 2014;6:1670–1690. doi: 10.3390/cancers6031670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pollard JW. Tumour-educated macrophages promote tumour progression and metastasis. Nat Rev Cancer. 2004;4:71–78. doi: 10.1038/nrc1256. [DOI] [PubMed] [Google Scholar]
- 103.Karnevi E, Andersson R, Rosendahl AH. Tumour-educated macrophages display a mixed polarisation and enhance pancreatic cancer cell invasion. Immunol Cell Biol. 2014;92:543–552. doi: 10.1038/icb.2014.22. [DOI] [PubMed] [Google Scholar]
- 104.Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- 105.Qian BZ, Li J, Zhang H, Kitamura T, Zhang J, Campion LR, et al. CCL2 recruits inflammatory monocytes to facilitate breast-tumour metastasis. Nature. 2011;475:222–225. doi: 10.1038/nature10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mantovani A, Allavena P. The interaction of anticancer therapies with tumor-associated macrophages. J Exp Med. 2015;212:435–445. doi: 10.1084/jem.20150295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sanford DE, Belt BA, Panni RZ, Mayer A, Deshpande AD, Carpenter D, et al. Inflammatory monocyte mobilization decreases patient survival in pancreatic cancer: a role for targeting the CCL2/CCR2 axis. Clin Cancer Res. 2013;19:3404–3415. doi: 10.1158/1078-0432.CCR-13-0525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Murdoch C, Giannoudis A, Lewis CE. Mechanisms regulating the recruitment of macrophages into hypoxic areas of tumors and other ischemic tissues. Blood. 2004;104:2224–2234. doi: 10.1182/blood-2004-03-1109. [DOI] [PubMed] [Google Scholar]
- 109.Senovilla L, Aranda F, Galluzzi L, Kroemer G. Impact of myeloid cells on the efficacy of anticancer chemotherapy. Curr Opin Immunol. 2014;30:24–31. doi: 10.1016/j.coi.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 110.Shen L, Sundstedt A, Ciesielski M, Miles KM, Celander M, Adelaiye R, et al. Tasquinimod modulates suppressive myeloid cells and enhances cancer immunotherapies in murine models. Cancer Immunol Res. 2015;3:136–148. doi: 10.1158/2326-6066.CIR-14-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Olsson A, Nakhle J, Sundstedt A, Plas P, Bauchet AL, Pierron V, et al. Tasquinimod triggers an early change in the polarization of tumor associated macrophages in the tumor microenvironment. J Immunother Cancer. 2015;3:53. doi: 10.1186/s40425-015-0098-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Nakanishi Y, Nakatsuji M, Seno H, Ishizu S, Akitake-Kawano R, Kanda K, et al. COX-2 inhibition alters the phenotype of tumor-associated macrophages from M2 to M1 in ApcMin/+ mouse polyps. Carcinogenesis. 2011;32:1333–1339. doi: 10.1093/carcin/bgr128. [DOI] [PubMed] [Google Scholar]
- 113.Nagai T, Tanaka M, Tsuneyoshi Y, Xu B, Michie SA, Hasui K, et al. Targeting tumor-associated macrophages in an experimental glioma model with a recombinant immunotoxin to folate receptor beta. Cancer Immunol Immunother. 2009;58:1577–1586. doi: 10.1007/s00262-009-0667-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aggarwal BB, Sethi G, Ahn KS, Sandur SK, Pandey MK, Kunnumakkara AB, et al. Targeting signal-transducer-and-activator-of-transcription-3 for prevention and therapy of cancer: modern target but ancient solution. Ann N Y Acad Sci. 2006;1091:151–169. doi: 10.1196/annals.1378.063. [DOI] [PubMed] [Google Scholar]
- 115.Karin M. Nuclear factor-kappaB in cancer development and progression. Nature. 2006;441:431–436. doi: 10.1038/nature04870. [DOI] [PubMed] [Google Scholar]
- 116.Mankan AK, Greten FR. Inhibiting signal transducer and activator of transcription 3: rationality and rationale design of inhibitors. Expert Opin Investig Drugs. 2011;20:1263–1275. doi: 10.1517/13543784.2011.601739. [DOI] [PubMed] [Google Scholar]
- 117.Taniguchi K, Karin M. IL-6 and related cytokines as the critical lynchpins between inflammation and cancer. Semin Immunol. 2014;26:54–74. doi: 10.1016/j.smim.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 118.Pilati C, Amessou M, Bihl MP, Balabaud C, Nhieu JT, Paradis V, et al. Somatic mutations activating STAT3 in human inflammatory hepatocellular adenomas. J Exp Med. 2011;208:1359–1366. doi: 10.1084/jem.20110283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kortylewski M, Xin H, Kujawski M, Lee H, Liu Y, Harris T, et al. Regulation of the IL-23 and IL-12 balance by Stat3 signaling in the tumor microenvironment. Cancer Cell. 2009;15:114–123. doi: 10.1016/j.ccr.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fagard R, Metelev V, Souissi I, Baran-Marszak F. STAT3 inhibitors for cancer therapy: Have all roads been explored? JAKSTAT. 2013;2:e22882. doi: 10.4161/jkst.22882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mesa RA, Yasothan U, Kirkpatrick P. Ruxolitinib. Nat Rev Drug Discov. 2012;11:103–104. doi: 10.1038/nrd3652. [DOI] [PubMed] [Google Scholar]
- 122.Zerbini CA, Lomonte AB. Tofacitinib for the treatment of rheumatoid arthritis. Expert Rev Clin Immunol. 2012;8:319–331. doi: 10.1586/eci.12.19. [DOI] [PubMed] [Google Scholar]
- 123.Loh ML, Tasian SK, Rabin KR, Brown P, Magoon D, Reid JM, et al. A phase 1 dosing study of ruxolitinib in children with relapsed or refractory solid tumors, leukemias, or myeloproliferative neoplasms: A Children’s Oncology Group phase 1 consortium study (ADVL1011) Pediatr Blood Cancer. 2015;62:1717–1724. doi: 10.1002/pbc.25575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Plimack ER, Lorusso PM, McCoon P, Tang W, Krebs AD, Curt G, et al. AZD1480: a phase I study of a novel JAK2 inhibitor in solid tumors. Oncologist. 2013;18:819–820. doi: 10.1634/theoncologist.2013-0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Min C, Eddy SF, Sherr DH, Sonenshein GE. NF-kappaB and epithelial to mesenchymal transition of cancer. J Cell Biochem. 2008;104:733–744. doi: 10.1002/jcb.21695. [DOI] [PubMed] [Google Scholar]
- 126.Zhong Z, Umemura A, Sanchez-Lopez E, Liang S, Shalapour S, Wong J, et al. NF-kappaB Restricts Inflammasome Activation via Elimination of Damaged Mitochondria. Cell. 2016;164:896–910. doi: 10.1016/j.cell.2015.12.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hsu LC, Enzler T, Seita J, Timmer AM, Lee CY, Lai TY, et al. IL-1beta-driven neutrophilia preserves antibacterial defense in the absence of the kinase IKKbeta. Nat Immunol. 2011;12:144–150. doi: 10.1038/ni.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bhardwaj A, Sethi G, Vadhan-Raj S, Bueso-Ramos C, Takada Y, Gaur U, et al. Resveratrol inhibits proliferation, induces apoptosis, and overcomes chemoresistance through down-regulation of STAT3 and nuclear factor-kappaB-regulated antiapoptotic and cell survival gene products in human multiple myeloma cells. Blood. 2007;109:2293–2302. doi: 10.1182/blood-2006-02-003988. [DOI] [PubMed] [Google Scholar]
- 129.Shishodia S, Majumdar S, Banerjee S, Aggarwal BB. Ursolic acid inhibits nuclear factor-kappaB activation induced by carcinogenic agents through suppression of IkappaBalpha kinase and p65 phosphorylation: correlation with down-regulation of cyclooxygenase 2, matrix metalloproteinase 9, and cyclin D1. Cancer Res. 2003;63:4375–4383. [PubMed] [Google Scholar]
- 130.Singh S, Aggarwal BB. Activation of transcription factor NF-kappa B is suppressed by curcumin (diferuloylmethane) [corrected] J Biol Chem. 1995;270:24995–25000. doi: 10.1074/jbc.270.42.24995. [DOI] [PubMed] [Google Scholar]
- 131.Salamone F, Galvano F, Cappello F, Mangiameli A, Barbagallo I, Li Volti G. Silibinin modulates lipid homeostasis and inhibits nuclear factor kappa B activation in experimental nonalcoholic steatohepatitis. Transl Res. 2012;159:477–486. doi: 10.1016/j.trsl.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 132.Ahn DW, Seo JK, Lee SH, Hwang JH, Lee JK, Ryu JK, et al. Enhanced antitumor effect of combination therapy with gemcitabine and guggulsterone in pancreatic cancer. Pancreas. 2012;41:1048–1057. doi: 10.1097/MPA.0b013e318249d62e. [DOI] [PubMed] [Google Scholar]
- 133.Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009;15:425–430. doi: 10.1158/1078-0432.CCR-08-0149. [DOI] [PubMed] [Google Scholar]
- 134.Broz P, Dixit VM. Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16:407–420. doi: 10.1038/nri.2016.58. [DOI] [PubMed] [Google Scholar]
- 135.Guo W, Sun Y, Liu W, Wu X, Guo L, Cai P, et al. Small molecule-driven mitophagy-mediated NLRP3 inflammasome inhibition is responsible for the prevention of colitis-associated cancer. Autophagy. 2014;10:972–985. doi: 10.4161/auto.28374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Qiao Y, Wang P, Qi J, Zhang L, Gao C. TLR-induced NF-kappaB activation regulates NLRP3 expression in murine macrophages. FEBS Lett. 2012;586:1022–1026. doi: 10.1016/j.febslet.2012.02.045. [DOI] [PubMed] [Google Scholar]
- 137.Nunes T, de Souza HS. Inflammasome in intestinal inflammation and cancer. Mediators Inflamm. 2013;2013:654963. doi: 10.1155/2013/654963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Antonucci L, Fagman JB, Kim JY, Todoric J, Gukovsky I, Mackey M, et al. Basal autophagy maintains pancreatic acinar cell homeostasis and protein synthesis and prevents ER stress. Proc Natl Acad Sci U S A. 2015;112:E6166–6174. doi: 10.1073/pnas.1519384112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Li N, Wu X, Holzer RG, Lee JH, Todoric J, Park EJ, et al. Loss of acinar cell IKKalpha triggers spontaneous pancreatitis in mice. J Clin Invest. 2013;123:2231–2243. doi: 10.1172/JCI64498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Aghajan M, Li N, Karin M. Obesity, autophagy and the pathogenesis of liver and pancreatic cancers. J Gastroenterol Hepatol. 2012;27(Suppl 2):10–14. doi: 10.1111/j.1440-1746.2011.07008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem J. 2003;374:1–20. doi: 10.1042/BJ20030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015;12:584–596. doi: 10.1038/nrclinonc.2015.105. [DOI] [PubMed] [Google Scholar]
- 143.Wang K, Karin M. The IL-23 to IL-17 cascade inflammation-related cancers. Clin Exp Rheumatol. 2015;33:S87–90. [PubMed] [Google Scholar]
- 144.Teng MW, Bowman EP, McElwee JJ, Smyth MJ, Casanova JL, Cooper AM, et al. IL-12 and IL-23 cytokines: from discovery to targeted therapies for immune-mediated inflammatory diseases. Nat Med. 2015;21:719–729. doi: 10.1038/nm.3895. [DOI] [PubMed] [Google Scholar]
- 145.Bertoletti A, Gehring AJ. Immune therapeutic strategies in chronic hepatitis B virus infection: virus or inflammation control? PLoS Pathog. 2013;9:e1003784. doi: 10.1371/journal.ppat.1003784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chang MH, Chen CJ, Lai MS, Hsu HM, Wu TC, Kong MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med. 1997;336:1855–1859. doi: 10.1056/NEJM199706263362602. [DOI] [PubMed] [Google Scholar]
- 147.Koumbi L. Current and future antiviral drug therapies of hepatitis B chronic infection. World J Hepatol. 2015;7:1030–1040. doi: 10.4254/wjh.v7.i8.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61:S58–68. doi: 10.1016/j.jhep.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 149.Trottier H, Franco EL. The epidemiology of genital human papillomavirus infection. Vaccine. 2006;24(Suppl 1):S1–15. doi: 10.1016/j.vaccine.2005.09.054. [DOI] [PubMed] [Google Scholar]