Abstract
Purpose
Data on weight history may enhance the predictive validity of epidemiological models of the health risks of obesity but collecting such data is often not feasible. In this study, we investigate the validity of a summary measure of weight history.
Methods
We evaluated the quality of reporting of maximum weight in a sample of adults ages 50-84 using data from the Health and Retirement Study. Recalled max body mass index (BMI, measured in kg/m2) based on recalled weight in 2004 was compared to calculated max BMI based on self-reported weight collected biennially between 1992 and 2004. Logistic regression was used to assess similarity between the measures in predicting prevalent conditions.
Results
The correlation coefficient between recalled and calculated max weight in the overall sample was 0.95. Recalled max BMI value was within 3 BMI units of the calculated value 91.4% of the time. The proportion of individuals obese I (BMI 30.0-34.9), obese II (35.0-39.9) and obese III (40.0 and above) were 28.8%, 12.7% and 6.6% using recalled values compared to 27.1%, 10.5% and 4.9% using calculated values. In multivariate analyses, the two BMI measures similarly predicted disease prevalence across a number of chronic conditions.
Conclusions
Recalled max BMI was strongly correlated with max BMI calculated over the twelve year period prior to recall, suggesting that this measure can serve as a reliable summary measure of recent weight status.
Keywords: Overweight, obesity, body mass index, weight histories, maximum weight, aging and lifecourse, mortality, epidemiology, validation, Health and Retirement Study
Introduction
The global age-standardized prevalence of obesity more than tripled in men and doubled in women over the last four decades, reaching 10.8% in men and 14.9% in women in 2014.[1] Despite the emergence of obesity as a major global health challenge, the impact of obesity on mortality remains poorly understood. A limitation of prior studies is that in most cases weight status was assessed at a single point in time [2–12], thus ignoring the effects of weight dynamics earlier in the life course. Using a one-time measure of BMI is also complicated by the fact that in some individuals, low BMI may reflect a pre-existing illness, which can create spurious associations between BMI and health outcomes.[13,14]
More sophisticated methods of risk assessment drawing on repeat measures of adiposity over multiple years have been explored in several recent studies.[15–17] However, longitudinal datasets required to implement analyses of this nature are not widely available and expensive to collect. Furthermore, most existing datasets only capture experience over a portion of the life course, often beginning in mid- to late-adulthood. Given these challenges, a validated summary measure of weight history that could be elicited in a single survey wave could potentially provide an appealing and practical alternative.
One such summary measure that was recently proposed is maximum BMI, which combines data on recalled maximum weight over the life course with information on height assessed at the time of survey.[18] As a measure of weight history, maximum BMI has several important features that distinguish it from other measures of weight history, such as weight at an earlier age or point in time. First, by enabling a distinction between non-obese individuals who were always non-obese versus those that were formerly obese and lost weight, this indicator provides an effective means of addressing confounding by illness in analyses of obesity and mortality.[19] Second, unlike other measures that use a fixed reference point, such as weight 10 years prior to survey or weight at a particular earlier age, maximum BMI can account for differences across individuals in the period over which illness-associated weight loss occurs. This is likely to be important given evidence of substantial heterogeneity by age and cause of death in trajectories of illness-associated weight loss prior to death.[20]
In this study, we use data from a high-quality nationally representative data set—the Health and Retirement Study [21]—to explore the validity of this measure for use in epidemiological studies. Because the HRS contains weight histories collected during longitudinal follow-up and the recalled maximum weight question, the database provides a unique opportunity to validate maximum BMI and assess the effects of measurement error in these data on the estimated health consequences of obesity in the US population. As a study of older adults, it also enables us to focus the validation on the critical age range in which obesity-related morbidities are common.
Material and Methods
We used data from the Health and Retirement Study (HRS), a nationally representative longitudinal study of US adults ages 50 and above who were surveyed biennially beginning in 1992. HRS participants considered eligible for the present study included respondents who consented to complete interviews from 1992 to 2004, either in person or indirectly by telephone, mail or online survey. Data for Waves 1-7 (1992-2004) of the original HRS cohort, born between 1931 and 1941, were obtained from the RAND HRS Data file (Version O). These data were supplemented with additional information of recalled maximum weight and age at maximum weight from the HRS 2004 core file.
To perform the validation, we defined two measures of max BMI using 2004 as the baseline year for analyses. The first measure (calculated max BMI) used the maximum value of self-reported current weight between 1992 and 2004 combined with self-reported height in 2004. The second measure (recalled max BMI) combined recalled max weight in 2004 with self-reported height in 2004. Information on recalled max weight in 2004 was based on a question in the HRS in that year which asked “Up to the present time, what is the most you have ever weighed?” In responding to this question, female respondents were instructed to exclude weight during pregnancy from consideration. Self-reported height was based on the response to a question in 1994 which asked “About how tall are you without shoes?” The height value was carried forward in subsequent waves as it was not asked again after 1994.
We adopted several inclusion/exclusion criteria for the validation procedure. First, we eliminated respondents missing data on recalled maximum weight or current height in 2004 and individuals who had any weight measurements missing between 1992 and 2004. We also restricted the sample to individuals between the ages of 50-84 at baseline, resulting in the exclusion of 63 individuals below the age of 50 and 13 individuals 85 years of age or above, as well as individuals with extreme values of recalled maximum weight (less than 118 or greater than 320 lbs., corresponding to the 1st and 99th percentile values) (n=143). Individuals whose reported age at maximum was more than twelve years prior to baseline age (n=1,790) or more than one year after baseline age (n=22) were also eliminated since histories were only observed over the twelve-year period spanning 1992 and 2004. To accomplish the latter restriction, we used information from a follow-up to the max weight question which asked “how old were you then?” Finally, individuals whose BMI category placed them in the underweight category on either measure were excluded (n=3). After imposing these exclusions, the final analytic dataset consisted of 5,108 observations.
To examine the validity of recalled max weight, we first calculated its correlation with calculated max weight by gender and age as well as combinations of these two characteristics. For examining age differences in recalled max weight, we divided the sample into the age groups 50-63, 64-68 and 69-84 based on the 33.3rd and 66.6th percentile values of the age distribution. Next, we compared mean values of recalled max BMI by gender and age to mean values obtained using calculated max BMI. To explore the quality of reporting within categories of BMI, we constructed categorical measures for both max BMI variables using the standard WHO definitions of normal weight (18.5-24.9), overweight (25.0-29.9), obese I (30.0-34.9), obese II (35.0-39.9) and obese III (≥40.0). We used these variables to compare the gender specific prevalence of each weight status and to examine the joint distribution of subjects by recalled and calculated max BMI category. We examined concordance across the two measures by calculating the ratio of the percentage of individuals in a particular weight class based on both measures to the percentage in that weight category based on calculated max BMI.
In addition to assessing concordance in BMI distributions between recalled and calculated max BMI, we investigated differences in patterns of obesity-related disease prevalence by BMI category across the two measures. We compared both crude prevalence values and measures of association derived from multivariate logistic regression models adjusted for age and gender in which maximum BMI was specified as a continuous variable. For these comparisons, we used data on provider diagnosed hypertension, diabetes, heart disease, stroke and arthritis from the 2004 wave of HRS.
Finally, in a supplementary analysis, we compared socio-demographic characteristics and lifestyle behaviors of respondents whose max weight was attained less than or equal to 12 years vs. more than 12 years prior to baseline. For these two groups of respondents, we also calculated mean values of recalled max BMI by age and gender. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) and were adjusted for unequal probabilities of selection and non-response using sample weights. The complex survey design of the HRS was accounted for by incorporating cluster and stratification variables.
Results
The final sample of 2,982 women and 2,126 men was 88% White or Caucasian, 9% Black and 3% other. A majority (74%) was married, and more than three fourths had a high school education or some college and above. 40% of the participants claimed that they never smoked, while 13% were current smokers at the time of baseline survey. Half of respondents reported that they consumed alcohol. An average of 4 times weekly vigorous physical activity and 3 times of light or moderate weekly exercises were reported (Table 1). Compared to female respondents, males were more likely to be married, alcohol consumers and former smokers (Appendix Table 1).
Table 1.
Baseline socio-demographic and behavioral characteristics of the study population
| Variables | % (SD) or Mean (SE) |
|---|---|
| Socio-demographics | |
| Female | 57.8% (0.6) |
| Age, Mean (SD) | 66.6 (0.1) |
| Ethnicity | |
| White/Caucasian | 87.9% (0.8) |
| Black/African American | 9.2% (0.6) |
| Other | 2.8% (0.4) |
| Married | 74.0% (0.9) |
| Levels of Education | |
| LT High School | 19.1% (0.9) |
| GED | 5.3% (0.4) |
| High School Graduate | 34.7% (0.9) |
| Some College | 20.7% (0.8) |
| College and above | 20.2% (1.0) |
| Lifestyle Behaviors | |
| Smoking | |
| Never Smoker | 39.9% (0.9) |
| Former Smoker | 47.5% (0.8) |
| Current Smoker | 12.6% (0.6) |
| Alcohol (Yes) | 50.8% (1.2) |
| Physical Exercises | |
| Frequency of light physical activities / week | 2.5 (0.02) |
| Frequency of moderate physical activities / week | 2.8 (0.03) |
| Frequency of vigorous physical activities / week | 4.0 (0.02) |
Alcohol status was defined based on the question “Do you ever drink any alcoholic beverages such as beer, wine, or liquour?
Appendix Table 1.
Association between max weight categories and the prevalence of various conditions, comparing calculated to recalled scales
| Variables | Hypertension OR (95%CI) |
Diabetes OR (95%CI) |
Heart Disease OR (95%CI) |
Stroke OR (95%CI) |
Arthritis OR (95%CI) |
|---|---|---|---|---|---|
| Calculated | |||||
| Normal Weight | Reference | Reference | Reference | Reference | Reference |
| Overweight | 1.77 (1.47, 2.14) | 3.77 (2.51, 5.68) | 1.20 (0.93, 1.55) | 1.30 (0.81, 2.09) | 1.56 (1.32, 1.84) |
| Obese I | 3.18 (2.57, 3.94) | 9.38 (6.69, 13.15) | 1.65 (1.26, 2.15) | 1.44 (0.85, 2.45) | 2.16 (1.74, 2.69) |
| Obese II | 3.66 (2.95, 4.54) | 13.70 (8.61, 21.82) | 1.81 (1.30, 2.51) | 1.74 (1.00, 3.02) | 2.49 (1.91, 3.23) |
| Obese III | 6.24 (4.33, 8.97) | 34.13 (21.08, 55.27) | 2.75 (1.94, 3.90) | 3.33 (1.80, 6.16) | 5.25 (3.85, 7.15) |
| Recalled | |||||
| Normal Weight | Reference | Reference | Reference | Reference | Reference |
| Overweight | 1.82 (1.49, 2.24) | 2.86 (1.93, 4.24) | 1.32 (1.02, 1.71) | 1.40 (0.80, 2.44) | 1.61 (1.31, 1.97) |
| Obese I | 3.18 (2.53, 4.00) | 6.52 (4.42, 9.62) | 1.61 (1.25, 2.08) | 1.61 (0.90, 2.90) | 2.00 (1.66, 2.42) |
| Obese II | 4.17 (3.35, 5.20) | 11.68 (7.50, 18.18) | 2.05 (1.49, 2.82) | 2.03 (1.18, 3.49) | 2.92 (2.32, 3.68) |
| Obese III | 5.73 (4.33, 7.58) | 25.86 (16.82, 39.77) | 2.80 (2.00, 3.93) | 3.23 (1.81, 5.78) | 4.30 (3.30, 5.58) |
Multivariate logistic regression model adjusted for gender and baseline age (age in 2004).
The overall correlation between recalled and calculated max weight was 0.948 and was slightly higher in women compared to men (r=0.949 vs. 0.944). Table 2 compares mean values recalled and calculated max BMI by gender and age. Across all gender/age categories, mean values were higher when recalled data were used. Among females the mean values for recalled and calculated max BMI were 30.8 vs. 30.1 for individuals ages 50-63, 30.6 vs. 29.9 for those ages 64-68 and 30.3 vs. 29.8 for those ages 69-84. A similar pattern was observed in males, with the difference in mean BMI being slightly greater in younger as compared to older individuals.
Table 2.
Comparison of mean recalled and calculated maximum BMI by gender and age
| Female | Male | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| N | Recalled BMI Mean (SE) |
Calculated BMI Mean (SE) |
N | Recalled BMI Mean (SE) |
Calculated BMI Mean (SE) |
|
| All* | 2982 | 30.6 (0.12) | 29.9 (0.11) | 2126 | 30.6 (0.10) | 29.9 (0.09) |
| 50-63 | 995 | 30.8 (0.25) | 30.1 (0.23) | 347 | 31.1 (0.26) | 30.2 (0.25) |
| 64-68 | 1101 | 30.6 (0.18) | 29.9 (0.17) | 853 | 30.9 (0.17) | 30.2 (0.17) |
| 69-84 | 886 | 30.3 (0.20) | 29.8 (0.19) | 926 | 30.1 (0.19) | 29.5 (0.18) |
The age categories were defined based on the 33.3rd and 66.7th percentile values of the distribution of ages in the sample.
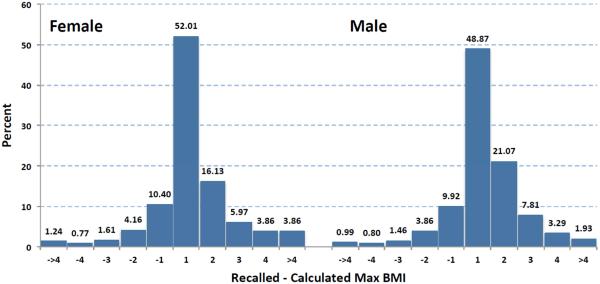
Figure 1 presents gender-specific histograms of the difference between recalled and calculated max BMI. In males, recalled max values were within 1 BMI unit of the calculated values 59% of the time, within 2 BMI units 85% of the time and within 3 units 94% of the time. Discrepancy between recalled and calculated values were similar in females with the difference falling within 1 unit of BMI 62% of the time, 2 units 83% of the time and 3 units 90% of the time.
Figure 1.
Difference between recalled and calculated max BMI by gender
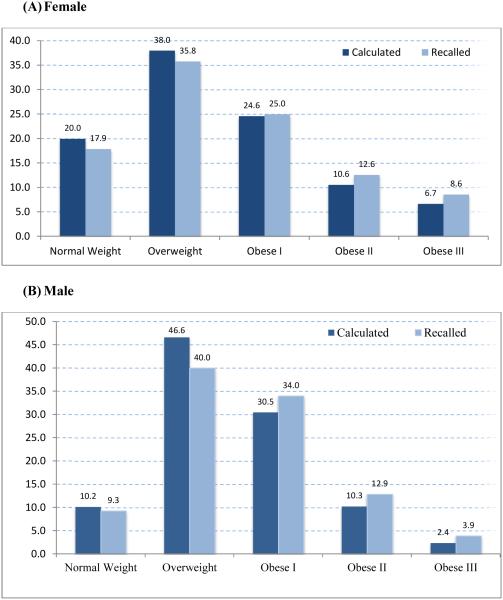
In addition to exploring the two measures on a continuous basis, we constructed categorical measures of recalled and calculated max BMI to investigate differences in prevalence values across the standard categories of BMI. Figure 2 presents the comparison by gender for the prevalence of normal weight, overweight, obese I, obese II and obese III. Among females, the distribution of recalled max BMI was 17.9% normal weight, 35.8% overweight, 25.0% obese I, 12.6% obese II and 8.6% obese III. Using calculated values the corresponding values were 20.0%, 38.0%, 24.6%, 10.6% and 6.7%. In males, the corresponding distributions for recalled and calculated values were 9.3% vs. 10.2%, 40.0% vs. 46.6%, 34.0% vs. 30.5%, 12.9% vs. 10.3% and 3.9% vs. 2.4%. The absolute difference in prevalence values between the two measures was greatest in the overweight category in both sexes. In both sexes, the prevalence of normal and overweight were underestimated using recalled max BMI, whereas the prevalence of obese I, II, III were overestimated.
Figure 2.
Comparison of the prevalence of normal weight, overweight and obesity for recalled vs. calculated maximum BMI by gender
Table 3 shows the joint distribution between recalled and calculated max BMI categories. Adding up the values along the diagonal of the matrix shows that recalled max BMI agreed with the calculated value for 79% of individuals. Concordance was highest for individuals with a calculated max BMI in the obese III range (91%). In the remaining categories the percentage of those in a given category of recalled BMI that were in the same category of calculated BMI was between 70-80%. The sum of values in the upper and lower diagonals of the matrix showed that recalled values were higher than calculated values for 17.1% of individuals and lower than calculated values in 4.1% of cases. Among individuals who were not in their calculated BMI category, most were displaced by one BMI category. Patterns were similar when the joint distributions were examined separately by age. The proportion of cases in which recalled max BMI agreed with the calculated value was 77.1%, 79.2% and 79.8% at ages 50-63, 64-68 and 69-84, respectively (Appendix Table 2).
Table 3.
Joint distribution of subjects by recalled and calculated prevalence of weight status
| Calculated Class |
Recalled Class | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Normal (%) |
Over (%) |
Obese I (%) |
Obese II (%) |
Obese III (%) |
Total (%) |
|
| Normal | 12.72 | 3.16 | 0.0 | 0.0 | 0.0 | 15.88 |
| Over | 1.49 | 33.00 | 7.03 | 0.07 | 0.01 | 41.61 |
| Obese I | 0.06 | 1.34 | 20.88 | 4.69 | 0.13 | 27.10 |
| Obese II | 0.01 | 0.02 | 0.77 | 7.72 | 1.98 | 10.50 |
| Obese III | 0.0 | 0.06 | 0.12 | 0.24 | 4.50 | 4.92 |
| Total | 14.28 | 37.58 | 28.80 | 12.72 | 6.63 | 100 |
Appendix Table 2.
Joint distribution of subjects by recalled and calculated prevalence of weight status by age levels
| (A) Age 50-63 |
| Calculated Class |
Recalled Class | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Normal (%) |
Over (%) |
Obese I (%) |
Obese II (%) |
Obese III (%) |
Total (%) |
|
| Normal | 13.6 | 3.0 | 0.0 | 0.0 | 0.0 | 16.6 |
| Over | 1.5 | 31.1 | 6.6 | 0.3 | 0.05 | 39.5 |
| Obese I | 0.0 | 1.4 | 19.4 | 5.5 | 0.2 | 26.4 |
| Obese II | 0.0 | 0.0 | 0.4 | 7.7 | 3.3 | 11.4 |
| Obese III | 0.0 | 0.2 | 0.2 | 0.5 | 5.3 | 6.1 |
| Total | 15.1 | 35.6 | 26.5 | 14.0 | 8.8 | 100 |
| (B) Age 64-68 |
| Calculated Class |
Recalled Class | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Normal (%) |
Over (%) |
Obese I (%) |
Obese II (%) |
Obese III (%) |
Total (%) |
|
| Normal | 13.0 | 3.2 | 0.0 | 0.0 | 0.0 | 16.3 |
| Over | 1.4 | 30.8 | 6.8 | 0.0 | 0.0 | 39.0 |
| Obese I | 0.03 | 1.3 | 22.0 | 5.0 | 0.2 | 28.6 |
| Obese II | 0.02 | 0.0 | 1.0 | 8.3 | 1.7 | 11.0 |
| Obese III | 0.0 | 0.0 | 0.0 | 0.1 | 5.1 | 5.2 |
| Total | 14.4 | 35.3 | 29.8 | 13.4 | 7.0 | 100 |
| (C) Age 69-84 |
| Calculated Class |
Recalled Class | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Normal (%) |
Over (%) |
Obese I (%) |
Obese II (%) |
Obese III (%) |
Total (%) |
|
| Normal | 11.7 | 3.2 | 0.0 | 0.0 | 0.0 | 14.9 |
| Over | 1.6 | 36.8 | 7.6 | 0.0 | 0.0 | 45.9 |
| Obese I | 0.1 | 1.4 | 20.8 | 3.8 | 0.0 | 26.1 |
| Obese II | 0.0 | 0.1 | 0.9 | 7.1 | 1.3 | 9.3 |
| Obese III | 0.0 | 0.02 | 0.2 | 0.2 | 3.4 | 3.8 |
| Total | 13.5 | 41.4 | 29.4 | 11.0 | 4.6 | 100 |
We also investigated the association between recalled and calculated max BMI categories and prevalent conditions, including provider-diagnosed hypertension, diabetes, heart disease, stroke and arthritis. Table 4 shows the prevalence of each condition by BMI category and Table 5 shows results from multivariate logistic regression models relating each prevalent condition to calculated and recalled max BMI. Across all the conditions examined, strong gradients in disease prevalence were observed across categories of BMI whether recalled or calculated values were used. For hypertension, prevalence values for normal weight, overweight and obese I-III were 37.8%, 51.9%, 65.5%, 68.3%, 78.2% based on calculated BMI and 36.0%, 50.7%, 63.8%, 69.3% and 75.0% using recalled values. For diabetes the corresponding values for calculated and recalled max BMI were 3.4% vs. 4.0%, 12.4% vs. 11.2%, 25.5% vs. 22.3%, 32.6% vs. 32.6% and 52.2% vs. 49.2%. The extent of agreement was similar for other conditions. With respect to patterns in the discrepancy in prevalent conditions between recalled and calculated values by BMI category, the most consistent difference emerged in the obese III category, where the calculated values were slightly higher than the recalled values across all the disease states. Table 5 based on continuous measures of exposure and Appendix Table 1 based on categorical measures of exposure show similar patterns as Table 4, with strong and consistent increases in the covariate-adjusted odds of having a prevalent condition with increases in max BMI, regardless of the measure used.
Table 4.
Weighted prevalence by weight categories from calculated and recalled information
| Prevalence | Recalled Weight Categories | Calculated Weight Categories | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Normal weight | Overweight | Obese I | Obese II | Obese III | Normal weight | Overweight | Obese I | Obese II | Obese III | |
| Hypertension | 36.0% | 50.7% | 63.8% | 69.3% | 75.0% | 37.8% | 51.9% | 65.5% | 68.3% | 78.2% |
| Diabetes | 4.0% | 11.2% | 22.3% | 32.6% | 49.3% | 3.4% | 12.4% | 25.5% | 32.6% | 52.3% |
| Heart Disease | 16.3% | 22.3% | 25.9% | 28.9% | 32.2% | 17.3% | 22.2% | 27.3% | 28.0% | 33.5% |
| Stroke | 3.6% | 5.3% | 6.0% | 7.0% | 9.8% | 4.0% | 5.5% | 5.8% | 6.7% | 11.2% |
| Arthritis | 51.4% | 61.0% | 65.0% | 72.9% | 80.5% | 52.4% | 60.9% | 67.7% | 70.7% | 84.5% |
Table 5.
Association between max BMI and the prevalence of various conditions, comparing calculated to recalled values
| Variables | Hypertension OR (95% CI) |
Diabetes OR (95% CI) |
Heart Disease OR (95% CI) |
Stroke OR (95% CI) |
Arthritis OR (95% CI) |
|---|---|---|---|---|---|
| Calculated Max BMI |
1.098 (1.085, 1.111) |
1.159 (1.139, 1.181) |
1.049 (1.034, 1.063) |
1.051 (1.025, 1.079) |
1.078 (1.066, 1.090) |
| Recalled Max BMI |
1.093 (1.081, 1.105) |
1.150 (1.131, 1.169) |
1.049 (1.036, 1.061) |
1.049 (1.023, 1.076) |
1.073 (1.062, 1.084) |
Multivariate logistic regression model adjusted for gender and baseline age (age in 2004).
To better understand the subpopulation that reported attaining their max BMI earlier in life, we compared recalled max BMI, socio-demographic characteristics and lifestyle behaviors of respondents whose max weight was attained less than or equal to 12 years vs. more than 12 years prior to baseline. The results are displayed in Appendix Table 3. Compared to those with recent recalled maximum BMI, respondents who attained their max BMI earlier in life were slightly older on average and were more likely to be male and current smokers. Members of this subpopulation also had somewhat lower recalled maximum BMI compared to those who attained their max BMI within 12 years of baseline.
Appendix Table 3.
Sample characteristics by years elapsed since maximum weight was attained by gender
| Variables | Elapsed Year > 12 (26%) (N=1790) | Elapsed Year ≤ 12 (74%) (N=5108) | ||
|---|---|---|---|---|
|
|
|
|||
| Female % (SD) or Mean (SE) |
Male % (SD) or Mean (SE) |
Female % (SD) or Mean (SE) |
Male % (SD) or Mean (SE) |
|
| Recalled Max BMI | 29.2 (0.2) | 29.2 (0.2) | 30.6 (0.1) | 30.6 (0.1) |
| Socio-demographics | ||||
| Age, Mean (SD) | 66.1 (0.2) | 68.9 (0.2) | 65.5 (0.1) | 68.1 (0.1) |
| Ethnicity | ||||
| White/Caucasian | 86.3% (1.2) | 91.0% (1.0) | 86.8% (0.9) | 89.6% (0.8) |
| Black/African American | 10.7% (1.0) | 7.0% (0.9) | 10.5% (0.7) | 7.5% (0.7) |
| Other | 3.0% (0.5) | 2.0% (0.5) | 2.8% (0.4) | 3.0% (0.4) |
| Married | 60.1% (1.8) | 82.3% (1.1) | 65.8% (1.1) | 85.2% (0.8) |
| Levels of Education | ||||
| LT High School | 22.7% (1.8) | 20.6% (1.5) | 18.5% (1.1) | 19.9% (1.1) |
| GED | 3.4% (0.6) | 5.7% (0.9) | 4.9% (0.6) | 5.8% (0.6) |
| High School Graduate | 36.7% (1.9) | 27.7% (1.5) | 38.0% (1.1) | 30.3% (1.1) |
| Some College | 20.7% (1.3) | 18.6% (1.3) | 21.8% (0.9) | 19.1% (1.1) |
| College and above | 16.6% (1.8) | 27.5% (1.8) | 16.8% (0.9) | 24.9% (1.4) |
| Lifestyle Behaviors | ||||
| Smoking | ||||
| Never Smoker | 42.1% (2.0) | 27.7% (1.8) | 48.2% (1.0) | 28.4% (1.1) |
| Former Smoker | 35.0% (1.8) | 56.8% (1.6) | 39.1% (0.9) | 59.1% (1.0) |
| Current Smoker | 22.9% (1.9) | 15.6% (1.3) | 12.7% (0.6) | 12.5% (0.9) |
| Alcohol (Yes) | 43.5% (2.1) | 58.4% (2.0) | 46.9% (1.4) | 56.0% (1.3) |
| Physical Exercises | ||||
| Frequency of light physical activities / week |
2.4 (0.03) | 2.8 (0.1) | 2.4 (0.02) | 2.8 (0.03) |
| Frequency of moderate physical activities / week |
2.9 (0.1) | 2.7 (0.04) | 2.9 (0.03) | 2.8 (0.04) |
| Frequency of vigorous physical activities / week |
4.1 (0.1) | 3.8 (0.1) | 4.1 (0.02) | 3.8 (0.04) |
Discussion
Life course data on adiposity may significantly enrich the quality of epidemiological models of the health consequences of obesity, yet most studies continue to rely on weight status recorded at a single instance in time.[2–12] A major challenge to adopting a life course approach is that few datasets include the long-term repeat measures of adiposity that would be necessary to carry out such studies and those that do exist often do not begin early enough in the life of the cohort to capture all the relevant history. In the absence of these data, alternative measures are needed that capture key features of weight history but are at the same time simple and inexpensive to collect.
One such measure that was recently proposed is maximum BMI, constructed using data on recalled maximum weight.[18] Maximum BMI has several important features that make it particularly suitable for use in studying the association between obesity and mortality. First, maximum BMI enables identification of a low-risk subset of the population whose weight never exceeded the normal weight category, thus providing an effective means of addressing confounding by illness. Second, it provides a more flexible manner of identifying pre-illness weight status than metrics that rely on weight recalled at a specific age or point in time, such as weight at age 25 or weight 10 years prior to the survey. This is a valuable given prior findings in the literature that illness-associated weight-loss trajectories vary substantially by age and cause of death.[20] Although maximum BMI has shown promise in several recent studies[18,19], it has not previously been validated.
In this study, we took advantage of a nationally representative longitudinal dataset to perform such a validation. We compared maximum BMI based on recalled maximum weight in 2004 to an alternative measure of maximum BMI calculated using data on self-reported weight collected biennially between 1992 and 2004. We found that the overall correlation coefficient between the two measures was 0.948 and that respondents’ recalled max BMI value was within 3 BMI units of the calculated value 91.4% of the time. When categorical versions of the two measures were compared, recalled max BMI category concurred with the calculated category in 79% of instances. The percent overweight or obese was 85.7% based on recalled values and 84.1% using calculated max BMI. Based on comparisons of categorical BMI, the quality of reporting was slightly higher in women than men and higher in older as compared to younger adults.
To the best of our knowledge, this is the first study to investigate the validity of recalled max weight. However, several prior studies have compared data on recalled and measured past weight.[22,23] In one such study based on data from the National Health and Nutrition Examination Survey 1 Epidemiologic Follow-up Study, the correlation coefficient between measured weight in 1971-1975 and recalled 1971-1975 body weight reported in 1982-1984 was 0.73 for men and 0.74 for women.[22] A study of Japanese men ages 34-61 that compared measured to recalled weight at age 25 reported a correlation coefficient of 0.85.[23] In the current study, we found a correlation coefficient of 0.948—a value similar to that found in comparisons of self-reported and measured current BMI.[24,25]
This study had several limitations. First, the gold standard we used to assess the quality of recalled max weight was based on respondents’ self-reported weight during longitudinal follow-up. Although these data were not subject to recall bias, they may still been affected by errors of self-reporting. Prior studies have found strong correlations between self-reported and measured current weight [24,25], however, indicating that although not a perfect proxy, self-reported values provides a reasonable approximation to measured values. Second, members of the sample may have been more aware of their maximum weight status than members of the population at large as a result of their participation in the study, leading us to overestimate the quality of recalled maximum weight. Third, weight was only reported in two-year intervals during follow-up and as such we cannot rule out the possibility that some respondents’ max weight was attained between survey waves and thus not observed. This possibility is supported by the fact that for over a third of respondents, self-reported age at max weight was different from the calculated value by a single year (data not shown). Both self-reporting bias in current BMI over follow-up and the lack of granularity in the weight histories may have led us to underestimate calculated max BMI and thus overestimate the discrepancy between the two max BMI measures. This possibility is consistent with our findings, which showed that in the large majority of cases where the two measures were different, the recalled value was higher than the calculated value. The fact that recalled max was rarely lower than the calculated value is reassuring and suggests that recalled max weight is not systematically underreported in these data, which may be expected a priori given the well-documented underreporting of self-reported current BMI.
An additional limitation of our study was that the validation was limited to those who reported attaining their max weight within the twelve years prior to baseline due to the fact that longitudinal data for constructing calculated max BMI were not available beyond this interval. In a supplementary analysis comparing sample characteristics by time since max BMI, we found that respondents whose reported max weight occurred more than 12 years before baseline were similar with respect to race/ethnicity, marital status and educational attainment, but slightly older and more likely to be male and current smokers than those whose max weight occurred within 12 years of baseline. Studies on recall error generally find quality of recall deteriorates with its length, thus this restriction may have led us to overestimate the quality of the data.21 A direction for future research is to perform additional validations in datasets with more extensive weight histories than those available here in order to that the quality of data on max weight can be examined over the entire life course.
Integrating weight history into studies on the health consequences of obesity is challenging due to the fact few datasets collect longitudinal data on weight over the life course. In this study, we evaluated the validity of a summary measure of weight history—maximum BMI—for use in epidemiological studies. We found that recalled max BMI was strongly correlated with max BMI calculated using longitudinal data over a twelve year period prior to recall, suggesting that this measure can serve as a reliable summary measure of recent weight history for use in research on the health consequences of obesity.
Acknowledgements
The authors would like to thank Samuel Preston and Lucia Tiererova for their helpful comments and suggestions
Source of Funding: This project was supported by Grant Number R03SH000037 from the National Center for Health Statistics and by Grant Number R01AG040212 from the National Institute on Aging.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors declare that they have no conflicts of interest.
References
- [1].NCD Risk Factor Collaboration Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19· 2 million participants. Lancet. 2016;387:1377–96. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, Macinnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363:2211–9. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Boggs DA, Rosenberg L, Cozier YC, Wise L, Coogan PF, Ruiz-Narvaez E a, et al. General and abdominal obesity and risk of death among black women. N Engl J Med. 2011;365:901–8. doi: 10.1056/NEJMoa1104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess Deaths Associated with Underweight, Overweight, and Obesity. JAMA. 2005;293:1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- [5].Flegal KM, Graubard BI, Williamson DF, Gail MH. Cause Specific Excess Deaths Associated With Underweight, Overweight, and Obesity. JAMA. 2007;298 doi: 10.1001/jama.298.17.2028. [DOI] [PubMed] [Google Scholar]
- [6].Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA. 2013;309:71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355:779. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- [8].Park Y, Wang S, Kitahara CM, Moore SC, De Gonzalez AB, Bernstein L, et al. Body mass index and risk of death in Asian Americans. Am J Public Health. 2014;104:520–5. doi: 10.2105/AJPH.2013.301573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–96. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Yi S-W, Ohrr H, Shin S-A, Yi J-J. Sex-age-specific association of body mass index with all-cause mortality among 12.8 million Korean adults: a prospective cohort study. Int J Epidemiol. 2015:1–10. doi: 10.1093/ije/dyv138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156. doi: 10.1136/bmj.i2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].The Global BMI Mortality Collaboration Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;6736:1–11. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hu F. Obesity and Mortality. In: Hu FB, editor. Obes. Epidemiol. Oxford University Press; New York: 2008. pp. 216–33. [Google Scholar]
- [14].Lawlor DA, Hart CL, Hole DJ, Smith GD. Reverse causality and confounding and the associations of overweight and obesity with mortality. Obesity. 2006;14 doi: 10.1038/oby.2006.269. [DOI] [PubMed] [Google Scholar]
- [15].Zajacova A, Ailshire J. Body Mass Trajectories and Mortality Among Older Adults: A Joint Growth Mixture-Discrete-Time Survival Analysis. Gerontologist. 2013:1–11. doi: 10.1093/geront/gns164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Zajacova A, Huzurbazar S, Greenwood M, Nguyen H. Long-Term BMI Trajectories and Health in Older Adults: Hierarchical Clustering of Functional Curves. J Aging Health. 2015:1–19. doi: 10.1177/0898264315584329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zheng H, Tumin D, Qian Z. Obesity and mortality risk: New findings from body mass index trajectories. Am J Epidemiol. 2013;178:1591–9. doi: 10.1093/aje/kwt179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Stokes A. Using maximum weight to redefine body mass index categories in studies of the mortality risks of obesity. Popul Health Metr. 2014;12:6. doi: 10.1186/1478-7954-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Stokes, Preston SH. Revealing the burden of obesity using weight histories. Proc Natl Acad Sci. 2016 doi: 10.1073/pnas.1515472113. 201515472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Alley DE, Metter EJ, Griswold ME, Harris TB, Simonsick EM, Longo DL, et al. Changes in weight at the end of life: Characterizing weight loss by time to death in a cohort study of older men. Am J Epidemiol. 2010;172:558–65. doi: 10.1093/aje/kwq168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Juster TF, Suzman R. An Overview of the Health and Retirement Study. J Hum Resour. 1995;30:S7–56. [Google Scholar]
- [22].Perry G, Byers T, Mokdad A, Serdula M. The validity of self-reports of past body weights by US adults. Epidemiology. 1995;6:61–6. doi: 10.1097/00001648-199501000-00012. [DOI] [PubMed] [Google Scholar]
- [23].Tamakoshi K, Yatsuya H, Kondo T, Hirano T, Hori Y, Yoshida T, et al. The accuracy of long-term recall of past body weight in Japanese adult men. Int J Obes Relat Metab Disord. 2003;27:247–52. doi: 10.1038/sj.ijo.802195. [DOI] [PubMed] [Google Scholar]
- [24].McAdams M, Van Dam RM, Hu FB. Comparison of self-reported and measured BMI as correlates of disease markers in US adults. Obesity (Silver Spring) 2007;15:188–96. doi: 10.1038/oby.2007.504. [DOI] [PubMed] [Google Scholar]
- [25].Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002;5:561–5. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]