Abstract
Few researchers have attempted to examine the mechanisms through which HIV-related stigma in the community is processed and experienced at an individual level by people living with HIV. We examined how the effects of perceived HIV stigma in the community on health outcomes for people living with HIV are mediated by internalized stigma and anticipated stigma. Participants (N = 203) from an HIV clinic completed self-report measures and their clinical data were obtained from medical records. Results suggested that the association between perceived community stigma and affective, cognitive, and mental health outcomes (self-esteem, depressive symptoms, avoidance coping, self-blame) are mediated by internalized stigma. Furthermore, a serial mediation model suggested that perceived community stigma leads to internalized stigma, which leads to anticipated community stigma, which in turn leads to lower medication adherence. The associations between perceived community stigma and interpersonal outcomes (social support, trust in physicians) were mediated by internalized stigma and anticipated stigma, again in a serial fashion (perceived community stigma leads to internalized stigma, which leads to anticipated stigma, which in turn leads to interpersonal outcomes). These results suggest that perceived HIV-related stigma in the community may cause people living with HIV to internalize stigma and anticipate stigmatizing experiences, resulting in adverse health and psychosocial outcomes—information that can be used to shape interventions.
Keywords: HIV, Stigma, Internalized stigma, Perceived community stigma, Anticipated stigma, Mechanisms, Mediation
Introduction
Stigma refers to the process by which a group of individuals is labeled as socially undesirable and these individuals are devalued due to attributes or behaviors that are societally deemed as “deeply discrediting” [1]. Stigma is a damaging social phenomenon. In the case of people living with HIV (PLWH), stigma has negative effects on health outcomes, including non-optimal medication adherence, lower visit adherence, higher depression, and overall lower quality of life [2–9]. Even though an abundance of research has documented the injurious effects of stigma, few researchers have attempted to classify specific mechanisms and examine the pathways through which social stigma related to HIV is processed and experienced by PLWH at an individual level, consequently affecting their health outcomes.
HIV-related stigma causes PLWH to lose social value and standing due to their HIV positive status [1, 10, 11]. Because stigma is a fundamentally social occurrence, requiring an “us” as compared to a “them”—thereby being interpersonal in nature—stigma is created and perpetuated by social structure and interpersonal processes [12]. Furthermore, prior research suggests that social stigma affects emotions, cognitions, and behavior of PLWH [2–9]. This confluence begs the question: How does an interpersonal process affect intrapersonal outcomes at an individual level?
Herein lies the value of defining mechanisms of stigma. Interpersonal processes can lead PLWH to internalize and anticipate stigma, which subsequently results in negative individual level health consequences, ranging from depression to poor medication and visit adherence [2–9]. Yet, there is a scarcity of research on mechanisms and processes by which social stigma in the society is processed, internalized, and affects cognitions, emotions, behaviors, and health outcomes of individual PLWH [10].
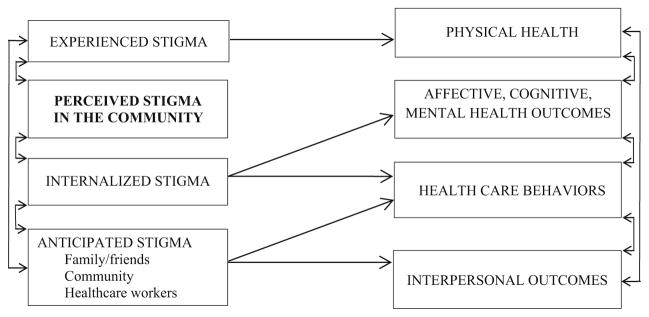
Earnshaw and Chaudoir’s Health Stigma Framework (HSF) [13, 14] provides an excellent heuristic model upon which to expand. The HSF suggests three HIV-related stigma mechanisms through which PLWH experience and respond to social stigma. These mechanisms then affect health outcomes. The three stigma mechanisms included in the HSF are (a) enacted stigma, (b) anticipated stigma, and (c) internalized stigma. Enacted stigma refers to actual past experiences of discrimination, devaluation, and prejudice by others due to one’s HIV-positive status. Anticipated stigma represents expectation of repercussions in the future; these are beliefs by PLWH that others will treat them negatively due to their HIV status. Internalized stigma is the acceptance of negative societal characterizations, labels, and perceptions about PLWH, and applying them to the self. Internalized stigma is often associated with self-deprecating emotions and cognitions such as shame, self-blame, embarrassment, and low self-worth [10, 15–17].
The value of distinguishing stigma mechanisms and processes is immense for researchers and public health practitioners alike; interventions which are designed to mitigate the effects of specific mechanisms tied to specific health behaviors and outcomes are more likely to be effective [11]. According to the HSF, each mechanism affects theoretically relevant outcomes relating to well-being and health (see Fig. 1 for a modified version of the model originally proposed by Earnshaw and Chaudoir). Experienced stigma is hypothesized to predict physical health (although not hypothesized within the original HSF, it is possible that experienced stigma also affects health behaviors); internalized stigma is hypothesized to predict affective, cognitive, and mental health outcomes as well as health care behaviors, and anticipated stigma is hypothesized to predict health care behaviors and interpersonal outcomes.
Fig. 1.
The health stigma framework (HSF) originally proposed by Earnshaw, modified by adding perceived community stigma as an additional stigma mechanism
Building upon the important contribution of the HSF, we propose the addition of a mechanism to the HSF: perceived stigma in the community (see Fig. 1). Perceived stigma in the community refers to a person’s perceptions of the severity of stigmatizing attitudes that exist in the community [11]. We hypothesized that perceived HIV stigma in the community, combined with PLWH’s knowledge of being HIV positive, has important implications. Following the theoretical formulation by Berger and colleagues [11], (also see [18]) we hypothesized that perceived stigma in the community has negative effects on self-concept and thus on affective, cognitive, and mental health outcomes for PLWH. Furthermore, we hypothesized that these effects would be mediated by internalized stigma (i.e., occur to the extent that perceived stigma in the community leads to internalized stigma; see Fig. 2).
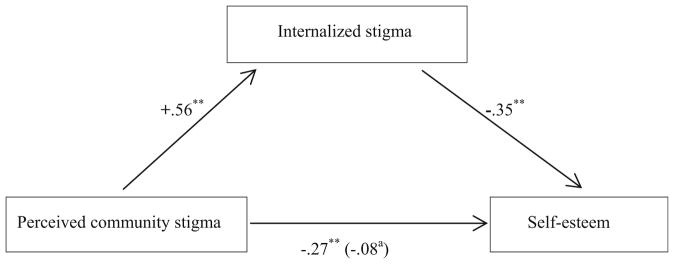
Fig. 2.
Internalized stigma mediates the effect of perceived community stigma on self-esteem. Path coefficients are unstandardized (B). Sex, race, age, socio-economic status, and time on ART are also controlled. aWhen internalized stigma is in the model. *p < 0.05; ** p < 0.01
The affective, cognitive, and mental health outcomes we examined in the current study were self-esteem, depressive symptoms, avoidance coping, and blame coping. Research suggests that these are important constructs in understanding the health of PLWH. According to the cognitive theory of depression, perceived low self-worth is a key cause of depression [19, 20]. Therefore, HIV-related stigma, especially internalized stigma, is expected to be positively associated with depressive symptoms and self-blame in PLWH, since internalized HIV stigma reflects how PLWH take in negative cognitions and feelings about HIV and carry these feelings (e.g. self-deprecation, feeling “dirty,” shame, guilt, self-blame) daily into intrapersonal reflection and interpersonal interactions [15–17]. Indeed, studies have found an association between internalized HIV-related stigma and depressive symptoms [5, 21]. One such study examined individuals with cancer and PLWH and found that the impact of illness on self-esteem is primarily due to differences in the experience of stigma, while other studies suggest that the coping mechanisms that individuals use to deal with stigma may have a direct effect on psychological and physiological outcomes [22–24]. What is particularly pertinent is that internalized stigma is intrapersonal in nature; thus, it occurs within the individual and can vary widely [25]. Like Earnshaw et al. [14], we expected internalized stigma (and associated negative cognitions and emotions about the self) to predict affective, cognitive, and mental health outcomes as well as health care behaviors.
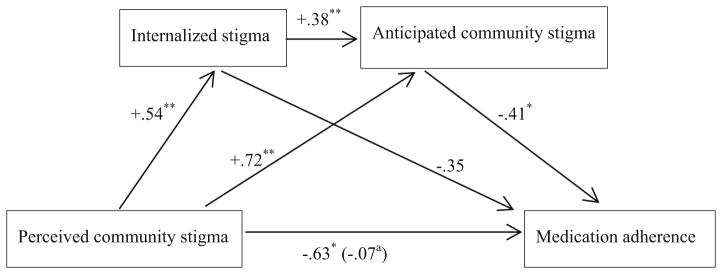
We hypothesized that perceived community stigma would also predict affective, cognitive, and mental health outcomes as well as health care behaviors, and that these effects of perceived community stigma would be mediated by internalized HIV-related stigma (see Fig. 2). We also hypothesized that anticipated stigma would predict health-care behaviors (e.g., medication adherence); thus, we hypothesized a serial mediation model in the effect of perceived community stigma on health-care behaviors (Fig. 3). Serial mediation examines a chain of effects that include more than one mediator [26]. Our model posits that perceived community stigma leads to internalized stigma, which in turn leads to anticipated stigma, which in turn leads to sub-optimal medication adherence.
Fig. 3.
Internalized stigma and anticipated community stigma mediate the effect of perceived community stigma on medication adherence (serial mediation). Path coefficients are unstandardized (B). Sex, race, age, socio-economic status, and time on ART are also controlled. aWhen internalized stigma and anticipated community stigma are in the model. *p < 0.05; **p <0.01
Anticipated stigma should also affect one’s interactions with others—and therefore interpersonal outcomes (e.g., social support, physician trust; see Fig. 1). PLWH who anticipate stigma may withdraw from social relationships in an attempt to minimize potential discrimination, which would lead to social isolation and reduced opportunities for social support [11, 12]. PLWH who anticipate stigma in the healthcare setting may have lower trust in health care providers, since the defining characteristic of trusting a person is having positive expectations regarding that person’s behavior and attitude toward the self [27]. Conversely, it is also possible that lack of trust leads to anticipating stigmatizing attitudes.
To add greater granularity to the proposed model, we make distinctions in the source of anticipated stigma: anticipated stigma from family and friends, anticipated stigma from the community, and anticipated stigma from health-care workers. Splitting anticipated stigma into these three separate sources allows for more fine-tuned empirical testing of the effect of stigma anticipated from each source on outcomes related to that source of anticipated stigma. For example, anticipated stigma from family and friends and from the community may be associated with lack of social support from these sources, while stigma anticipated from health-care workers may particularly affect behaviors and attitudes of PLWH in the health care setting (e.g., clinic visit adherence and trust in one’s medical provider, although it is of course possible that other stigma mechanisms may also be associated with health care behaviors), and stigma anticipated from the community may be associated with adherence to medication.
Thus, by examining how specific stigma mechanisms affect outcomes through theoretically hypothesized pathways, we aim to specify and deepen current knowledge of the deleterious effects of HIV-related stigma. Using these findings, researchers, clinicians, and public health practitioners may be able to obtain a more nuanced understanding of stigma-related behaviors and biases, and therefore be able to predict and mitigate different negative health outcomes for PLWH.
Methods
Participants and Procedures
Participants were 203 patients from the HIV clinic at the University of Alabama at Birmingham (UAB), who participated in a larger study on psychosocial factors related to HIV outcomes. Participants were on antiretroviral therapy (ART) and current non-substance users. The sample consisted of 74 women and 129 men (73 White, 130 Black) with a mean age of 44.8 (SD = 11.1). Participants were invited to research visits separate from their clinic visits, and completed study measures using computers. Participants self-reported their socio-economic status using a five-point scale (lower, lower middle, middle, upper middle, and upper). Data on depressive symptoms and duration of ART were extracted from clinic records. The study was approved by the Institutional Review Board of the university and all procedures were carried out with the adequate understanding and written consent of the participants.
HIV-Related Stigma Measures
Since no existing stigma measure includes all stigma mechanisms in which we are interested, we used two different measures. We used two subscales of the revised HIV Stigma Scale [28] that showed good internal consistency in the current study: perceived stigma in the community (concern with public attitudes), six items, α = 0.84 and internalized stigma (negative self-image), seven items, α = 0.85. Anticipated stigma from three different sources (friends and family, neighbors and others in the community, and health-care workers) was assessed using three items for each source adapted from the measure created by Earnshaw et al. [14]. (α = 0.90, α = 0.94, and α = 0.83, respectively for the friends and family, neighbors and others in the community, and health-care workers scales).
Affective, Cognitive, and Mental Health Factors
Global self-esteem was assessed using the Rosenberg self-esteem scale [29] (ten items, α = 0.81 in the current study). Depressive symptom data were extracted from clinic records on the nine-item depression scale of the Patient Health Questionnaire (PHQ-9 [30]; α = 0.87 in the current study). The total score was used as a measure of depressive symptom severity. Two coping subscales from the Ways of Coping [31] were used to assess coping by avoidance (ten items, α = 0.76 in the current study) and coping by blaming (three items, α = 0.81 in the current study).
Medication Adherence
ART adherence was assessed with the single question developed by Lu et al. [32]: “In the past 4 weeks, how was your ability to take all of your anti-HIV medications that were prescribed by your doctor?” (reported in a recent manuscript [9]). Response options ranged from very poor to excellent. According to previous literature, this measure is as good as or better than other self-report adherence measures [33]. Because 71 % of participants indicated excellent adherence, responses were dichotomized (excellent versus all other response options). While self-report measures may over-estimate adherence, research has consistently demonstrated the predictive value of self-reported non-adherence (i.e., non-optimal adherence) [34].
Interpersonal Factors
Social support was assessed with the short form [35] of the interpersonal support evaluation list (ISEL), which includes 16 items (α = 0.88 in the current sample). Trust in one’s physician was assessed with the ten-item Wake Forest Physician Trust Scale [36], which had good internal consistency (α = 0.82) in the current study.
Statistical Analyses
In order to test hypothesized mediational models (for example, the model depicted in Fig. 2, where internalized stigma mediates the effect of perceived community stigma on self-esteem), we calculated bias-corrected 95 % confidence intervals (CIs) for the indirect effect (in this example, the effect of perceived community stigma on self-esteem through the pathway of internalized stigma) using bootstrapping with the Process procedure [26]. A significant indirect effect is revealed when the CI does not include the value zero, which suggests statistical mediation. Serial mediation examines a chain of effects that include more than one mediator (see Fig. 3 for an example) [26]. Serial mediation hypotheses were also tested by examining the indirect effects using the Process procedure. In addition to calculating indirect effects, Process also calculates the unstandardized path coefficients for all paths in the model. In all of the analyses, we entered the following covariates as control variables: sex, race, age, socio-economic status, and time on ART.
Results
Affective, Cognitive, and Mental Health Factors
The associations that perceived community stigma showed with the outcome variables are presented in Table 1. As seen in Table 1 and in Fig. 2, perceived community stigma was significantly and negatively associated with self-esteem (the path with B = −0.27 in Fig. 2, the total effect when internalized stigma is not in the model). Furthermore, perceived community stigma was significantly associated with internalized stigma (the path with B = 0.56), and internalized stigma in turn was associated with self-esteem (the path with B = −0.35). Importantly, the indirect effect of perceived community stigma through internalized stigma (the product of the path coefficients. 56 and −0.35 in Fig. 2) was significant [B = −0.20, SE = 0.03, 95 % CI (−0.27, −0.14)], suggesting that internalized stigma mediates the effect of perceived community stigma on self-esteem. The path between perceived community stigma and self-esteem dropped to a non-significant value (B = −0.08) when internalized stigma was in the model (the direct effect of perceived community stigma when the indirect effect is accounted for).
Table 1.
The associations between perceived community stigma and outcomes
| Outcome | B | β | AOR | P |
|---|---|---|---|---|
| Self-esteem | −0.27 | −0.37 | 0.00 | |
| Depressive symptoms | 1.84 | 0.24 | 0.00 | |
| Avoidance coping | 0.58 | 0.48 | 0.00 | |
| Blame coping | 0.47 | 0.29 | 0.00 | |
| Medication adherence | −0.63 | 0.54 | 0.04 | |
| Social support | −0.28 | −0.31 | 0.00 | |
| Physician trust | −0.16 | −0.17 | 0.02 |
Covariates sex, race, age, socio-economic status, and time on ART were also entered in all analyses
AOR adjusted odds ratio. AOR is reported for logistic regression analysis and β is reported for multiple linear regression analyses
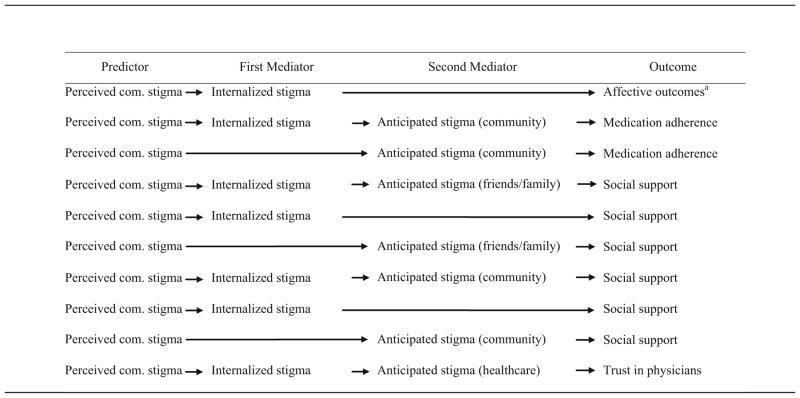
Similarly, analyses using the other three affective/cognitive/mental health factors as dependent variables yielded a significant mediation of the effect of perceived community stigma by internalized stigma. Indirect effects on depressive symptoms, avoidance coping, and blame coping, respectively, were as follows: [B = 0.72, SE = 0.35, 95 % CI (0.08, 1.53); B = 0.25, SE = 0.05, 95 % CI (0.14, 0.35); and B = 0.46, SE = 0.08, 95 % CI (0.30, 0.63)]. Table 2 presents all mediators of the effects of perceived community stigma that were significant in the current analyses.
Table 2.
Significant mediators of the effect of perceived community stigma in the present study
The affective, cognitive, and mental health outcomes included self-esteem, depressive symptoms, avoidance coping, and blame coping
Medication Adherence
We tested the mediational model in Fig. 3. Perceived community stigma was significantly and negatively associated with medication adherence (the path with B = −0.63, the total effect when internalized stigma and anticipated community stigma are not in the model). The serial mediation which suggests that perceived community stigma leads to internalized stigma, which leads to anticipated community stigma, which in turn leads to lower adherence yielded a significant overall indirect effect [coefficient = −0.084, CI (−0.244, −0.005)]. Figure 3 also shows coefficients for all paths in the model. The indirect effect of perceived community stigma through anticipated community stigma was also significant [the product of the path coefficients +0.72 and −0.41: coefficient = −0.295, CI (−0.664, −0.009)]. However, the indirect effect of perceived community stigma through internalized stigma was not significant [the product of the path coefficients +0.54 and −0.35: coefficient = −0.187, CI (−0.564, 0.179)]. When anticipated stigma from friends and family or anticipated stigma in the healthcare setting was used as the last mediator in the model (instead of anticipated stigma from the community) the serial mediation was not significant.
Interpersonal Factors
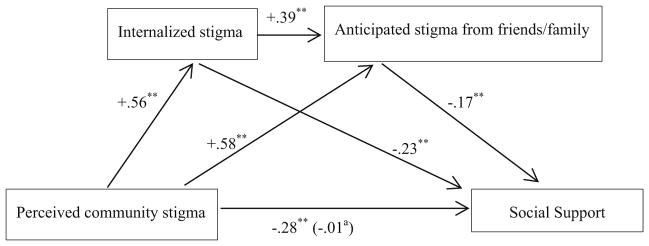
First, we tested the mediational model in Fig. 4. The serial mediation (indirect) effect of perceived community stigma on social support through internalized stigma and stigma anticipated from friends and family was significant [coefficient = −0.04, SE = 0.02, CI (−0.08, −0.01)]. The indirect effect of perceived community stigma on social support through internalized stigma was also significant [coefficient = −0.13, SE = 0.04, CI (−0.21, −0.07)]. The indirect effect of perceived community stigma on social support through stigma anticipated from friends and family was also significant [coefficient = −0.10, SE = 0.04, CI (−0.19, −0.05)].
Fig. 4.
Internalized stigma and anticipated stigma from friends and family mediate the effect of perceived community stigma on social support (serial mediation). Path coefficients are unstandardized (B). Sex, race, age, socio-economic status, and time on ART are also controlled. aWhen internalized stigma and anticipated stigma from friends and family are in the model. *p < 0.05; **p < 0.01
When we used stigma anticipated from the community instead of stigma anticipated from friends and family as the last mediator, results were similar. The indirect effect of perceived community stigma on social support through internalized stigma and stigma anticipated from the community was significant [not shown in the figure; coefficient = −0.03, SE = 0.02, CI (−0.07, −0.01)]. The indirect effect of perceived community stigma on social support through internalized stigma was also significant [coefficient = −0.26, SE = 0.04, CI (−0.36, −0.19)]. The indirect effect of perceived community stigma on social support through stigma anticipated from the community was also significant [coefficient = −0.10, SE = 0.03, CI (−0.17, −0.05)].
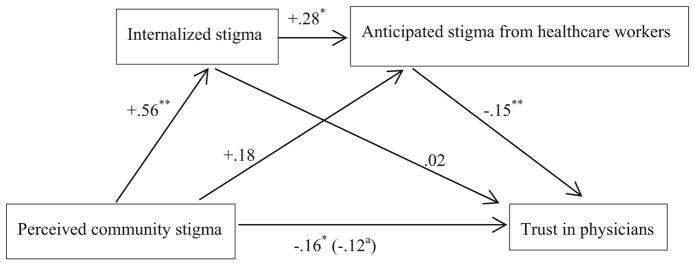
We then examined trust in physicians as the outcome. We tested the serial mediational model in Fig. 5 (perceived community stigma predicts internalized stigma, which predicts stigma anticipated from health-care workers, which in turn is associated with lower trust in physicians), which yielded a significant indirect effect for serial mediation [coefficient = −0.02, SE = 0.01, CI (−0.06, −0.01)]. The other indirect effects in the model were not significant: For the effect of perceived community stigma on trust in physicians through internalized stigma [coefficient = 0.01, SE = 0.04, CI (−0.07, 0.08)]; and for the effect of perceived community stigma on social support through stigma anticipated from health-care workers [coefficient = −0.03, SE = 0.03, CI (−0.08, 0.01)].
Fig. 5.
Internalized stigma and anticipated stigma from healthcare workers mediate the effect of perceived community stigma on trust in physicians (serial mediation). Path coefficients are unstandardized (B). Sex, race, age, socio-economic status, and time on ART are also controlled. When internalized stigma and anticipated stigma from healthcare workers are in the model. *p < 0.05; **p < 0.01
Discussion
The goals of this study were to test an expanded model of the HSF, including perceived community stigma, and to investigate meditational pathways for the effects of this dimension of HIV-related stigma. Perceived community stigma was associated with all of our affective, cognitive, and mental health factors, and these associations were all mediated by internalized stigma. For medication adherence, the serial mediation model suggested that perceived community stigma leads to internalized stigma, which leads to stigma anticipated from the community, which in turn was associated with lower medication adherence. The association between perceived community stigma and interpersonal outcomes (social support and physician trust) were also mediated by internalized stigma and anticipated stigma in a serial fashion. Another important finding in our study is that specifying the person or group from which HIV-related stigma is anticipated (i.e., the source) may aid in understanding outcomes associated with those persons or groups.
Thus, our model not only expands the HSF by adding perceived community stigma, it also includes mediating pathways elucidating how specific stigma mechanisms mediate the effects of perceived community stigma. To our knowledge, examining how some stigma mechanisms mediate the effects of other stigma mechanisms is a new approach in HIV research (see an example with an undergraduate student sample with other chronic diseases [25]), and is important in understanding the subtle ways that social/interpersonal stigma affects interpersonal as well as intrapersonal outcomes.
This study had some limitations. Some of our analyses utilized self-report measures, which may involve reporting biases. Furthermore, our study was cross-sectional, which precludes causal inferences, even though our models are supported by theory and previous research. It will be important going forward to use longitudinal designs to examine the effects of HIV-related stigma prospectively. Additionally, participants were recruited from a single HIV clinic at a research university that provides comprehensive social work and clinical services, which may limit the generalizability of the present findings. Finally, in this exploratory study we tested multiple mediational models with a moderate sample size; it will be important for future studies to examine these hypotheses in larger samples. There may be individual differences that moderate the association between perceived community stigma and internalized stigma and future research can also examine these individual differences.
In spite of these limitations, the present results point to how stigma mechanisms may affect psychological and physical health of PLWH in different ways. It is also noteworthy that when one considers the total effect of the entire spectrum of stigma mechanisms addressed in the literature, stigma seems to have a considerable overall effect on multiple outcomes [12]. The findings of this study have theoretical as well as practical implications. Researchers interested in the mechanisms and processes of stigma may want to explore the impact of perceived community stigma on health outcomes, in addition to the mechanisms defined in the HIV Stigma Framework (experienced stigma, anticipated stigma, and internalized stigma). When predicting certain outcomes, it may also be useful to specify the source of anticipated stigma.
Future studies should further examine and refine psychosocial mechanisms in the effects of HIV stigma mechanisms on health outcomes. For example, what are mediating psychosocial factors in the frequently found association between internalized stigma or anticipated stigma and medication adherence? Only a few studies have examined psychological constructs (e.g., depression, attachment styles, interpersonal worries) as mediating mechanisms in the association between internalized stigma and adherence [5, 9, 37, 38], and revealing relevant mediating constructs is important for gaining a deeper and more nuanced understanding of the effects of HIV-related stigma in the lives of PLWH.
A deeper understanding of how different stigma mechanisms affect outcomes, and the mediating pathways involved, is also important in designing interventions aimed at reducing the effects of HIV-related stigma. Based on the present findings, researchers may consider different intervention strategies (e.g., targeting stigma in the community, blocking the perceived community stigma—internalization of stigma pathway, and/or targeting internalized stigma—anticipated stigma pathway). Based on previous research suggesting that depression and other psycho-social factors may mediate the effects of stigma on outcomes, another intervention strategy may be to treat depression and address other mediating psychosocial factors. Programs with adequate resources may even target all of these mechanisms in a comprehensive intervention strategy to maximize the probability of success in reducing the effects of HIV-related stigma on the well-being of PLWH.
Acknowledgments
We would like to thank Maria Lechtreck, C. Blake Helms, Christy Thai, and all the research assistants for their help in data collection.
Funding This research was supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, an NIH funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. Dr. Fazeli is supported by 1K99 AG048762-01 from NIA (P. Fazeli, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest Bulent Turan, Henna Budhwani, Pariya L. Fazeli, Wesley R. Browning, James L. Raper, Michael J. Mugavero, and Janet M. Turan, declares that they has no conflict of interest.
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Goffman E. Stigma; notes on the management of spoiled identity. Englewood Cliffs: Prentice-Hall; 1963. [Google Scholar]
- 2.Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;5(10):473–82. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sweeney S, Vanable P. The association of HIV-related stigma to HIV medication adherence: a systematic review and synthesis of the literature. AIDS Behav. 2016;20:29–50. doi: 10.1007/s10461-015-1164-1. [DOI] [PubMed] [Google Scholar]
- 5.Turan B, Smith W, Cohen MH, Wilson TE, Adimora AA, Merenstein D, Adedimeji A, Wentz EL, Foster AG, Metsch L, Tien PC, Weiser SD, Turan JM. Mechanisms for the negative effects of internalized HIV-related stigma on ART adherence in women: the roles of social isolation and depression. JAIDS. 2016;72(2):198–205. doi: 10.1097/QAI.0000000000000948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turan B, Fazeli P, Raper JL, Mugavero MJ, Johnson MO. Social support and moment-to-moment changes in treatment self-efficacy in men living with HIV: psychosocial moderators and clinical outcomes. Health Psychol. doi: 10.1037/hea0000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turan B, Stringer KL, Onono M, et al. Linkage to HIV care, postpartum depression, and HIV-related stigma in newly diagnosed pregnant women living with HIV in Kenya: a longitudinal observational study. BMC Pregnancy Childbirth. 2014;14(1):400. doi: 10.1186/s12884-014-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turan J, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17(7):2528–39. doi: 10.1007/s10461-013-0446-8. [DOI] [PubMed] [Google Scholar]
- 9.Helms CB, Turan JM, Atkins G, et al. Interpersonal mechanisms contributing to the association between HIV-related internalized stigma and medication adherence. AIDS Behav. 2016 doi: 10.1007/s10461-016-1320-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalichman SC. The Harms of Internalized AIDS Stigma: a Comment on Tsai et al. Ann Behav Med. 2013;46(3):256–7. doi: 10.1007/s12160-013-9529-z. [DOI] [PubMed] [Google Scholar]
- 11.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 12.Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528–9. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- 13.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–95. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Person B, Bartholomew LK, Gyapong M, Addiss DG, van den Borne B. Health-related stigma among women with lymphatic filariasis from the Dominican Republic and Ghana. Soc Sci Med. 2009;68(1):30–8. doi: 10.1016/j.socscimed.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 16.Kilinc S, Campbell C. “It shouldn’t be something that’s evil, it should be talked about”: a phenomenological approach to epilepsy and stigma. Seizure. 2009;18(10):665–71. doi: 10.1016/j.seizure.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Mak WW, Cheung RY, Law RW, Woo J, Li PC, Chung RW. Examining attribution model of self-stigma on social support and psychological well-being among people with HIV+/AIDS. Soc Sci Med. 2007;64(8):1549–59. doi: 10.1016/j.socscimed.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 18.Cox WT, Abramson LY, Devine PG, Hollon SD. Stereotypes, prejudice, and depression the integrated perspective. Perspect Psychol Sci. 2012;7(5):427–49. doi: 10.1177/1745691612455204. [DOI] [PubMed] [Google Scholar]
- 19.Beck AT, Alford BA. Depression: causes and treatment. Philadelphia: University of Pennsylvania Press; 2009. [Google Scholar]
- 20.Rieger S, Gollner R, Trautwein U, Roberts BW. Low self-esteem prospectively predicts depression in the transition to young adulthood: a replication of Orth, Robins, and Roberts (2008) J Pers Soc Psychol. 2015;110(1):e16. doi: 10.1037/pspp0000037. [DOI] [PubMed] [Google Scholar]
- 21.Tsai AC, Bangsberg DR, Frongillo EA, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74(12):2012–9. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Major B, Quinton WJ, McCoy SK. Antecedents and consequences of attributions to discrimination: theoretical and empirical advances. Adv Exp Soc Psychol. 2002;34:251–330. [Google Scholar]
- 23.Wrubel J, Stumbo S, Johnson MO. Antiretroviral medication support practices among partners of men who have sex with men: a qualitative study. AIDS Patient Care STDS. 2008;22(11):851–8. doi: 10.1089/apc.2008.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmitz MF, Crystal S. Social relations, coping, and psychological distress among persons with HIV/AIDS. J Appl Soc Psychol. 2000;30(4):665–85. [Google Scholar]
- 25.Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17(2):157–68. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- 27.Holmes JG. Interpersonal expectations as the building blocks of social cognition: an interdependence theory perspective. Pers Relatsh. 2002;9(1):1–26. [Google Scholar]
- 28.Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- 29.Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 30.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150. doi: 10.1037//0022-3514.48.1.150. [DOI] [PubMed] [Google Scholar]
- 32.Lu M, Safren SA, Skolnik PR, et al. Optimal recall period and response task for self-reported HIV medication adherence. AIDS Behav. 2008;12(1):86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 33.Feldman B, Fredericksen R, Crane P, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–18. doi: 10.1007/s10461-012-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817–33. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Payne TJ, Andrew M, Butler KR, Wyatt SB, Dubbert PM, Mosley TH. Psychometric evaluation of the interpersonal support evaluation list–short form in the ARIC study cohort. SAGE Open. 2012;2(3):2158244012461923. [Google Scholar]
- 36.Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 37.Rao D, Feldman BJ, Fredericksen RJ, et al. A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS Behav. 2012;16(3):711–6. doi: 10.1007/s10461-011-9915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mitzel LD, Vanable PA, Brown JL, Bostwick RA, Sweeney SM, Carey MP. Depressive symptoms mediate the effect of HIV-related stigmatization on medication adherence among HIV-infected men who have sex with men. AIDS Behav. 2015;19(8):1454–9. doi: 10.1007/s10461-015-1038-6. [DOI] [PubMed] [Google Scholar]