Abstract
The aim of this study, carried out before the beginning of human papillomavirus (HPV) vaccinations as a National Immunization Program (NIP) in Korea in 2016, is to assess the ranges of perceptions and personal experience and their influences on attitudes regarding HPV vaccinations of children, among mothers of adolescent (9–14 years of age) daughters in Korea. From November 2015 to February 2016, we distributed a written questionnaire to mothers who had daughters aged 9–14 years. The questionnaire consisted of several questions, related to knowledge of HPV, personal experiences of HPV vaccination, and attitudes toward HPV vaccinations of their adolescent daughters. Of the 260 questionnaires distributed, 140 participants returned answered ones. And although only 51% of participants were aware that cervical cancer is highly related with HPV infection, 70% said they were willing to vaccinate their daughters, showing that awareness does not coincide with intention to vaccinate. Among the participants showing negative attitudes, 50% were concerned about the vaccination side effects. The more the participants’ pre-knowledge about HPV infection, and about the relationship of HPV to cervical cancer, the more positive their attitudes (P = 0.002, P < 0.001). Our study showed that, as the level of education rose, the proportion of mothers with negative attitudes toward vaccinating their adolescent daughters rose as well. Thus, the provision of correct education by health care providers and accurate information through active advertising may play an important role in increasing the vaccination rate among adolescent girls in Korea.
Keywords: Human Papillomavirus, Mothers’ Attitude, Adolescent, Vaccination
Graphical Abstract
INTRODUCTION
It is estimated that cervical cancer accounted for 3,100 (2.2%) of all new cancers and 761 (2.6%) of all cancer deaths among Korean women in 2015 (1,2). Human papillomavirus (HPV) infection is the main cause of cervical cancer, and infection typically occurs through sexual behavior (3,4). In 2006, a 3-dose HPV vaccine was introduced for primary prevention of cervical cancer. This HPV vaccine has demonstrated nearly 100% efficacy when administered prior to HPV exposure. The Centers for Disease Control and Prevention (CDC) and their partners recommend HPV vaccinations for both girls and boys at ages 11 or 12, and encourage clinicians to strongly recommend HPV vaccination for preteens and teens. Today quadrivalent and bivalent clinically approved HPV vaccines are used worldwide, and in 2014 the World Health Organization (WHO) recommended 2-dose schedules for two types of HPV vaccines at ages 9–14. As of August 2014, 58 countries had introduced HPV vaccines in their National Immunization Programs (NIP) (5). HPV vaccine uptake and completion rates have been suboptimal in many countries. In 2013, 57% of American females aged 13–17 had received at least one dose of HPV vaccine, but only 38% had completed the HPV vaccine series as recommended (6). One reason for the low uptake and completion rates in the U.S. is a lack of knowledge about HPV and the HPV vaccine among mothers of children in the eligible age range (7,8,9). McRee and Reiter stated in particular that adolescents aged 11–14 years contribute less to the decision-making process concerning their vaccinations than do their parents, with the parents making the decisions on whether their children should be vaccinated (10,11,12,13,14,15,16,17). For the successful general implementation of HPV vaccines targeting populations of children and adolescents, the vaccines’ acceptability to mothers plays an important role.
The Korean government has planned introduction of 2-dose HPV vaccines to girls as a NIP in 2016. The aim of this study, carried out before the beginning of HPV vaccinations in the Korean NIP, was to assess the ranges of perceptions and personal experiences among mothers with adolescent daughters (9–14 years) in Korea before the NIP began, and their influences on attitudes regarding HPV vaccinations of children.
MATERIALS AND METHODS
Sample and setting
From November 2015 to February 2016, we distributed a written questionnaire to 260 mothers who had daughters aged 9–14 in one elementary school and two middle schools in Seoul, Korea. The questionnaire consisted of several questions related to knowledge of HPV, personal experiences regarding HPV vaccinations, and attitude toward HPV vaccinations of the participants’ adolescent daughters. Among the returned questionnaires we excluded the following cases: 1) if the mothers’ daughters were already vaccinated; 2) if there were obvious errors or questions left blank in the questionnaires. Ultimately, we included 140 mothers’ questionnaires in this study.
Instruments and data collection
After careful inspection of the related literature, a data collection form was created to contain questions concerning parents’ sociodemographic characteristics, including their ages, highest levels of education completed, employment statuses and the ages and genders of their children, as well as their opinions about HPV vaccination and attitudes toward vaccination of their daughters and the reasons for them.
Statistical analysis
Data analysis was conducted via SPSS (IBM Corp., Armonk, NY, USA). We used Fisher’s exact test, the χ2 test, and multiple logistic regression for statistical analysis, where a P value of less of 0.05 was considered to be statistically significant.
Ethics statement
This study was approved by the Institutional Review Board at Kangnam Sacred Heart Hospital of Hallym University (IRB File No. 2016-05-67), and conducted in accordance with the principles expressed in the Declaration of Helsinki. The board exempted informed consent due to retrospective study.
RESULTS
Sociodemographic characteristics and knowledge about HPV of mothers
Of the 140 mothers considered, 53 (38%) had final education levels of high school, 76 (54%) were university graduates, and 12 (8%) had graduate degrees. The optional occupation statuses were currently working, unemployed, and retired-accounted for by 77 (55%), 56 (40%), and 7 (5%) mothers respectively. Only two participants had histories of past HPV infections, while 17 (12%) had family histories of cervical cancer (Table 1). Concerning the degrees of mothers’ knowledge of HPV, and of the associations between HPV infection, vaccinations, and cervical cancer, 66 (47%) replied that they were aware of HPV infections, 67 (48%) that they already knew about HPV vaccinations, and 72 (51%) that they were aware of HPV being a direct cause of cervical cancer (Table 2).
Table 1. Sociodemographic characteristics of mothers (n = 140).
| Characteristics | No. of response (%) |
|---|---|
| Age, yr | |
| 30–39 | 67 (48) |
| 40–49 | 62 (44) |
| 50– | 12 (8) |
| Highest level of education achieved | |
| High school and below | 53 (38) |
| College or university | 76 (54) |
| Graduate school or higher | 12 (8) |
| Employment status | |
| Working | 77 (55) |
| Not working | 56 (40) |
| Retired | 7 (5) |
| Experience with genital warts | |
| Yes | 2 (2) |
| No | 137 (98) |
| Family history of cervical cancer | |
| Yes | 17 (12) |
| No | 123 (88) |
| Vaccination of mothers herself | |
| Yes | 26 (19) |
| No | 114 (81) |
Table 2. Mothers’ pre-knowledge about HPV and HPV vaccine (n = 140).
| Knowledge | No. of response (%) |
|---|---|
| Knowledge about HPV infection | |
| Yes | 66 (47) |
| No | 74 (53) |
| Knowledge about HPV vaccine | |
| Yes | 67 (48) |
| No | 73 (52) |
| Knowledge of HPV relationship to cervical cancer | |
| Yes | 72 (51) |
| No | 68 (49) |
HPV = human papillomavirus.
Mothers’ opinions about vaccinating their daughters and reasons
Regarding mothers’ will to vaccinate their adolescent daughters, 99 (70%) responded positively, with 49 mothers indicating strong wills and 50 mothers' considerable wills. The other 41 (30%) mothers responded negatively, with 15 of them strongly opposed and 26 having unfavorable opinions (Table 3). We also analyzed the reasons for these opinions. Among the 99 mothers who responded positively, the reasons included gaining protection against cervical cancer (83 responses, 84%), physicians’ recommendations (13, 13%), their daughters having reached the indicated age (2, 2%), and concerns about their daughters being high-risk subjects (1, 1%). Of the 41 mothers who answered negatively, the reasons included concerns about possible side effects (20, 49%), poor awareness regarding HPV (18, 44%), and consideration of their daughters as being in the low-risk population (3, 7%) (Table 4).
Table 3. Opinions of parents concerning vaccinations of their children.
| Willing to vaccinate daughters | No. of response (%) | |
|---|---|---|
| Yes | Strongly | 49 (35) |
| Slightly | 50 (35) | |
| No | Slightly | 26 (19) |
| Strongly | 15 (11) | |
Table 4. Reasons for parents’ willingness or unwillingness to vaccinate their daughters.
| Reasons | No. of response (%) |
|---|---|
| Reasons for willingness to vaccinate daughters (n = 99) | |
| Protection against cervical cancer | 83 (84) |
| Recommendation by physician | 13 (13) |
| Being in age group for vaccination | 2 (2) |
| Being in at-risk group | 1 (1) |
| Reasons for unwillingness to vaccinate daughters (n = 41) | |
| Possible side effects | 20 (49) |
| Low awareness of HPV | 18 (44) |
| Not being in at risk group | 3 (7) |
| Expense | 0 (0) |
HPV = human papillomavirus.
Factors influencing willingness for vaccination
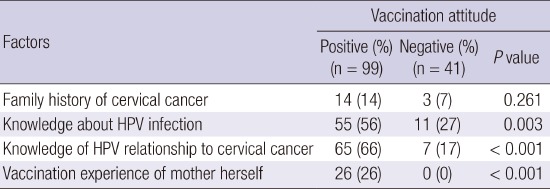
Among the participants with positive attitudes toward vaccinating their daughters, particularly high proportions were shown by those with family histories of cervical cancer (14/17, 82%) and who had already received vaccinations themselves (26/26, 100%). None of the participants with negative perceptions about the vaccine had been vaccinated themselves (0/41, 0%). All mothers who had experienced vaccinations themselves had positive rather than negative attitudes (P < 0.001). The higher the participants’ levels of education, the more negative their attitudes (P = 0.035). The more the participants had pre-knowledge about HPV infection, and about the relationship of HPV to cervical cancer, the more they showed positive attitudes (P = 0.002, P < 0.001). Knowledge regarding HPV infection and regarding its association with cervical cancer were also significantly greater in mothers with positive attitudes (P = 0.003 and P < 0.001, respectively) (Tables 5 and 6).
Table 5. Factors influencing attitudes toward vaccination.
| Factors | Vaccination attitude | ||
|---|---|---|---|
| Positive (%) (n = 99) |
Negative (%) (n = 41) |
Logistic test | |
| Age, yr | P = 0.046 | ||
| Thirties | 24 (24) | 4 (10) | 1.00 |
| Forties | 55 (56) | 22 (54) | 1.91 (0.80–4.54) |
| Over fifties | 20 (20) | 15 (36) | 2.29 (0.83–6.36) |
| Highest level of education achieved | P = 0.035 | ||
| High school and below | 44 (44) | 9 (22) | 1.00 |
| College or university | 49 (49) | 27 (66) | 2.53 (1.26–5.12) |
| Graduate school or higher | 6 (6) | 5 (12) | 3.68 (1.03–13.10) |
Table 6. Factors influencing attitudes toward vaccination.
| Factors | Vaccination attitude | ||
|---|---|---|---|
| Positive (%) (n = 99) |
Negative (%) (n = 41) |
P value | |
| Family history of cervical cancer | 14 (14) | 3 (7) | 0.261 |
| Knowledge about HPV infection | 55 (56) | 11 (27) | 0.003 |
| Knowledge of HPV relationship to cervical cancer | 65 (66) | 7 (17) | < 0.001 |
| Vaccination experience of mother herself | 26 (26) | 0 (0) | < 0.001 |
HPV = human papillomavirus.
DISCUSSION
Recent studies have demonstrated that, although parents support HPV vaccinations for their daughters, the rates of vaccination vary across populations with different sociocultural levels and knowledge of HPV (18,19,20). In one review, Seven et al. (18) in Turkey reported that only 26.9% of mothers knew about HPV infections, and only 24.5% about HPV vaccines. Ezenwa et al. (19) in Nigeria also reported the majority of respondents to have no awareness of HPV or HPV vaccines; only 27.9% of mothers had heard of HPV, and only 21% knew of relationship between cervical cancer and HPV. Yu et al. (20) in China also reported that a mere 19% of mothers had heard of HPV before the investigation, and that there was no significant difference in HPV awareness based on the mothers’ age group, education level or employment status. Considering these reviews, the knowledge of mothers in Korea concerning HPV is not low, although it was found to be below 60%. Knowledge about HPV infection, HPV vaccination, and cervical cancer also did not differ depending upon the mothers’ ages, final education levels or current occupational statuses.
Seven et al. (18) in Turkey reported that only 14.4% of the mothers surveyed wanted their daughters to be vaccinated. Ezenwa et al. (19) in Nigeria meanwhile reported that 30.3% of mothers were unworried about vaccinating their daughters against HPV. In contrast, in a study conducted in Indonesia, 96% of parents wished to vaccinate their daughters against HPV (21). In Denmark, where the HPV vaccine is included in the NIP, Mortensen (22) reported that 84% of parents with daughters aged 12–15 had had them vaccinated, and that 80% of the remaining parents wished to do so in due time. In our study, 70% of mothers said they would vaccinate her daughters with HPV vaccines, while 30% had concerns that made them hesitate about doing so (Table 4).
The most common reasons for mothers’ negative attitudes toward vaccinating their adolescent daughters differ across different countries. In Nigeria, for example, the most common reason (51.5%) was mothers not knowing where or how to access the vaccine (19), while in China it was mothers believing their daughter too young to be at risk of cervical cancer (31%) (20), and in Turkey it was low awareness concerning HPV (67.2%) (18). Our data showed the most common reasons for negative attitudes in Korea to be concerned about possible side effects (49%), followed by low awareness about HPV (44%).
Our data showed other factors influencing the willingness to have vaccinations to include age and level of education, where increased age and higher final education status were associated with hesitant attitudes. Also, mothers’ extensive knowledge regarding HPV infections, HPV vaccinations, and cervical cancer had positive influences. This may therefore imply that accurate knowledge of HPV and cervical cancer may be an important factor, regardless of the mother’s final education level. This is presumably a consequence of the particularly developed Internet and generalized access to enormous information in Korea. It might also be the reason for the lower will to vaccinate as the mother’s age increases, due to reduced exposure to the Internet and information. The study in Nigeria indicates that women with higher educational qualifications had higher awareness of HPV vaccines than those who were less educated, whereas other factors such as the mothers’ ages or religions did not influence their attitudes or degrees of knowledge (19). In the study in Turkey, although parents’ willingness to vaccinate their daughters increased if it was to be paid for by the Ministry of Health, very few parents who did not want to vaccinate their daughters cited expense as a reason. This result suggests that parents’ decisions are highly influenced by physicians’ recommendations, rather than by the cost of the vaccine (18).
This study is important in being the first evaluation of the opinions of mothers concerning vaccination of their adolescent daughters in Korea. Another of its strengths is that the questionnaire was distributed randomly in three different schools, rather than being performed within a hospital. The limitations of the study, meanwhile, are that 1) the total number of participants is not large; 2) we distributed the questionnaire in a well-developed city in Korea, and so it is hard for it to represent the general population, especially the population in rural districts; 3) there may be a potential response bias in the study, since the questionnaire was filled in by mothers themselves, who may tend to supply socially desirable responses; and 4) there may be a selection bias, in that there were only two mothers who had past histories of HPV infection in this study. Despite the above limitations, our study is the only one evaluating mothers’ opinions on vaccinating their daughters, and since cervical cancer vaccination was introduced as an NIP from June 2016, it may help in the development and reinforcement of the program to improve the vaccination rate.
In conclusion, our study found that the proportion of mothers with negative attitudes toward vaccinating their adolescent daughters rose with the level of their education. The most common reason for avoiding vaccinations was concern about their side effects, even though the WHO guidelines have stated that vaccines have been administered to millions of girls and women around the world without serious side effects. Meanwhile, correct knowledge regarding HPV and cervical cancer development was associated with positive attitudes, and mothers’ personal experiences of vaccination were significantly associated with intentions to vaccinate their daughters. Thus, the dissemination of proper education by health care providers, and accurate information through active advertising, might play an important role in increasing the vaccination rate of adolescent girls in Korea.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Research conception and design: Lee KN, Chang KH, Park ST. Data acquisition: Lee KN. Data analysis and interpretation: Chang KH, Cho SS, Park SH. Statistical analysis: Cho SS. Critical revision of the manuscript: Park ST. Approval of final manuscript: all authors.
References
- 1.Lee Y, Lim MC, Kim SI, Joo J, Lee DO, Park SY. Comparison of quality of life and sexuality between cervical cancer survivors and healthy women. Cancer Res Treat. 2016;48:1321–1329. doi: 10.4143/crt.2015.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Human papillomavirus vaccines: WHO position paper, October 2014. Wkly Epidemiol Rec. 2014;89:465–491. [PubMed] [Google Scholar]
- 3.Han KT, Kim SJ, Lee SY, Park EC. Cost-effectiveness analysis of HPV vaccination: comparing the general population with socially vulnerable individuals. Asian Pac J Cancer Prev. 2014;15:8503–8508. doi: 10.7314/apjcp.2014.15.19.8503. [DOI] [PubMed] [Google Scholar]
- 4.Kelly BJ, Leader AE, Mittermaier DJ, Hornik RC, Cappella JN. The HPV vaccine and the media: how has the topic been covered and what are the effects on knowledge about the virus and cervical cancer? Patient Educ Couns. 2009;77:308–313. doi: 10.1016/j.pec.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Evidence based recommendations on human papilloma virus (HPV) vaccines schedules: background paper for SAGE discussions [Internet] [cited 10 June 2016]. Available at http://www.who.int/immunization/sage/meetings/2014/april/1_HPV_Evidence_based_recommendationsWHO_with_Appendices2_3.pdf.
- 6.Elam-Evans LD, Yankey D, Jeyarajah J, Singleton JA, Curtis RC, MacNeil J, Hariri S, Immunization Services Division, National Center for Immunization and Respiratory Diseases Centers for Disease Control and Prevention (CDC). National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years--United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:625–633. [PMC free article] [PubMed] [Google Scholar]
- 7.Davis K, Dickman ED, Ferris D, Dias JK. Human papillomavirus vaccine acceptability among parents of 10- to 15-year-old adolescents. J Low Genit Tract Dis. 2004;8:188–194. doi: 10.1097/00128360-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. 2012;30:3546–3556. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 9.Laz TH, Rahman M, Berenson AB. An update on human papillomavirus vaccine uptake among 11-17 year old girls in the United States: National Health Interview Survey, 2010. Vaccine. 2012;30:3534–3540. doi: 10.1016/j.vaccine.2012.03.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahlström LA, Tran TN, Lundholm C, Young C, Sundström K, Sparén P. Attitudes to HPV vaccination among parents of children aged 12-15 years-a population-based survey in Sweden. Int J Cancer. 2010;126:500–507. doi: 10.1002/ijc.24712. [DOI] [PubMed] [Google Scholar]
- 11.Mullins TL, Griffioen AM, Glynn S, Zimet GD, Rosenthal SL, Fortenberry JD, Kahn JA. Human papillomavirus vaccine communication: perspectives of 11-12 year-old girls, mothers, and clinicians. Vaccine. 2013;31:4894–4901. doi: 10.1016/j.vaccine.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hertweck SP, LaJoie AS, Pinto MD, Flamini L, Lynch T, Logsdon MC. Health care decision making by mothers for their adolescent daughters regarding the quadrivalent HPV vaccine. J Pediatr Adolesc Gynecol. 2013;26:96–101. doi: 10.1016/j.jpag.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reiter PL, McRee AL. Correlates of receiving recommended adolescent vaccines among youth with special health care needs: findings from a statewide survey. Vaccine. 2016;34:3125–3131. doi: 10.1016/j.vaccine.2016.04.062. [DOI] [PubMed] [Google Scholar]
- 14.McRee AL, Gottlieb SL, Reiter PL, Dittus PJ, Tucker Halpern C, Brewer NT. Human papillomavirus vaccine discussions: an opportunity for mothers to talk with their daughters about sexual health. Sex Transm Dis. 2012;39:394–401. doi: 10.1097/OLQ.0b013e318248aaa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gilkey MB, Magnus BE, Reiter PL, McRee AL, Dempsey AF, Brewer NT. The vaccination confidence scale: a brief measure of parents’ vaccination beliefs. Vaccine. 2014;32:6259–6265. doi: 10.1016/j.vaccine.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilkey MB, Reiter PL, Magnus BE, McRee AL, Dempsey AF, Brewer NT. Validation of the vaccination confidence scale: a brief measure to identify parents at risk for refusing adolescent vaccines. Acad Pediatr. 2016;16:42–49. doi: 10.1016/j.acap.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah PD, McRee AL, Reiter PL, Brewer NT. What parents and adolescent boys want in school vaccination programs in the United States. J Adolesc Health. 2014;54:421–427. doi: 10.1016/j.jadohealth.2013.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seven M, Güvenç G, Şahin E, Akyüz A. Attitudes to HPV vaccination among parents of children aged 10 to 13 years. J Pediatr Adolesc Gynecol. 2015;28:382–386. doi: 10.1016/j.jpag.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Ezenwa BN, Balogun MR, Okafor IP. Mothers’ human papilloma virus knowledge and willingness to vaccinate their adolescent daughters in Lagos, Nigeria. Int J Womens Health. 2013;5:371–377. doi: 10.2147/IJWH.S44483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu Y, Xu M, Sun J, Li R, Li M, Wang J, Zhang D, Xu A. Human papillomavirus infection and vaccination: awareness and knowledge of HPV and acceptability of HPV vaccine among mothers of teenage daughters in Weihai, Shandong, China. PLoS One. 2016;11:e0146741. doi: 10.1371/journal.pone.0146741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaspers L, Budiningsih S, Wolterbeek R, Henderson FC, Peters AA. Parental acceptance of human papillomavirus (HPV) vaccination in Indonesia: a cross-sectional study. Vaccine. 2011;29:7785–7793. doi: 10.1016/j.vaccine.2011.07.107. [DOI] [PubMed] [Google Scholar]
- 22.Mortensen GL. Parental attitudes towards vaccinating sons with human papillomavirus vaccine. Dan Med Bull. 2010;57:A4230. [PubMed] [Google Scholar]


