Abstract
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging tick-borne disease characterized by fever, thrombocytopenia and diarrhea. SFTS was firstly reported in Korea in 2013 but its seroprevalence in the country has yet to be investigated. Here, we investigate the seroprevalence of SFTS in a Korean population. A cross-sectional study was conducted on patients who had their sera tested for various reasons at a tertiary university hospital on particular days in May 2015. This study was conducted in a tertiary hospital in southeastern Korea. Total antibodies including immunoglobulin G (IgG) and immunoglobulin M (IgM), specific to SFTS virus (SFTSV) in serum samples were detected by a double-antigen sandwich enzyme-linked immunosorbent assay (ELISA). A total of 1,069 serum samples were tested. Median age was 59 years (range 12–96 years), and 51.5% were male. Overall, 22 patients (2.1%) were tested positive for anti-SFTSV antibodies. The SFTS seroprevalence increased significantly with age (P = 0.034). The seropositive rate of rural area was higher than that of urban area (7.7% vs. 1.9%, P = 0.040). Seropositive rates were not significantly different among underlying diseases. None of the antibody-positive patients showed typical symptoms or laboratory findings of SFTS at the time of sample collection. Results of real-time reverse transcription polymerase chain reaction (RT-PCR) were negative for all the seropositive patients. Our study shows 2.1% SFTS seroprevalence among the patients visiting a tertiary hospital in Korea. Seroprevalence is higher in older and rural population.
Keywords: Bunyaviridae Infections; Zoonosis; Seroepidemiologic Studies; Communicable Diseases, Emerging
Graphical Abstract
INTRODUCTION
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging tick-borne disease caused by a novel bunyavirus known as SFTS virus (SFTSV), which was first reported in China in 2011 (1). The major clinical manifestations are fever, myalgia, and diarrhea; common laboratory findings are thrombocytopenia and leukopenia. The case-fatality rate has been reported to be 6%–30% (1,2). The first case of SFTS in Korea was reported in 2013; since then, cases of SFTS have been reported throughout Korea and the number has increased annually (3,4). As of July 4, 2016, a total of 192 cases of SFTS have been reported in South Korea according to the Disease Web Statistics System of the Korea Centers for Disease Control and Prevention (KCDC, http://is.cdc.go.kr/). The case-fatality rate of SFTS in 2014 and 2015 was reported as 47.2% and 29.1%, respectively (5).
The SFTSV Seropositivity rate in China is 0.3%–9.2%, depending on the population group and region investigated (6,7,8,9,10,11,12,13,14,15,16). However, no study has addressed the seroprevalence of SFTSV in Korea.
Here, we investigated the seroprevalence of SFTS in a Korean population, the factors influencing seropositive rates of SFTS.
MATERIALS AND METHODS
Study population, samples, and regions
A cross-sectional study was conducted on patients at a hospital on two separate days in May 2015. The patients visited outpatient clinics or were admitted for a various reason, such as elective surgery, regular check-up for diabetes, and cancer. We selected the study subjects randomly from among those patients whose leftover sera were stored. Aliquots were prepared, stored at −80°C until testing. The study hospital is a university-affiliated and tertiary hospital in Busan Metropolitan City (Busan), located in southeast Korea (35°10′N 129°04′E). Busan is the second-largest city in Korea and has a population of 3.6 million, with –0.006% of which are involved in farming, according to the Census of Agriculture, Forestry and Fisheries of the Republic of Korea (http://www.kosis.kr). Most of the city consists of an urban area, together with hills, rivers, and sea.
Demographic characteristics including age, gender, and residence address were collected by chart review. To identify differences in seroprevalence between urban and rural areas, we defined urban areas as an address in a metropolitan city or city according to the classification of the Local Autonomy Act, Statutes of the Republic of Korea. Underlying diseases of the subjects were reviewed. If the patient had received chemotherapy or immunosuppressive therapy, we reviewed whether the patient received such agents within 3 months from acquisition of serum sample for enzyme-linked immunosorbent assay (ELISA).
Serologic analysis
Serologic analysis was performed by double-antigen sandwich ELISA to detect total antibodies (including immunoglobulin G [IgG] and immunoglobulin M [IgM]) in serum samples, as described previously (17). The sensitivity and specificity of double-antigen sandwich ELISA were evaluated in a previous study, showing 100% and 99.57%, respectively (17). For the ELISA, the recombinant nucleocapsid protein (rNP) of the first Korean SFTSV strain (GenBank accession no. KF358693) was adsorbed to the solid phase and horseradish peroxidase-conjugated rNP was added after application of serum. Each serum sample was tested in duplicate, and the positive and negative controls were tested in quadruplicate. The optical density (OD) at 450 nm was measured after adding tetramethylbenzidine (Thermo Scientific, Waltham, MA, USA) and a stop solution. The results are expressed as the percentage of the positive (PP) control serum, determined using the following formula:
(OD of test serum/mean OD of positive-control serum) × 100
The cutoff value was set as the mean value plus 3 standard deviations, as derived from the PP values of the negative-control serum.
Serum samples positive by SFTSV ELISA were tested for the presence of SFTSV RNA. Viral RNA was extracted from the serum samples using a QIAamp MinElute Virus Spin Kit (Qiagen, Hilden, Germany). Viral RNA was amplified by one-step real-time reverse transcription polymerase chain reaction (RT-PCR) using primers specific to each of the large, medium, and small segments of SFTSV, and PCR was performed using a SensiFAST Probe Lo-ROX Kit (Bioline, London, UK).
Annual incidences of SFTS
To calculate regional annual incidences, annual numbers of cases of SFTS from the Disease Web Statistics System, KCDC (http://is.cdc.go.kr/) and population statistics based on resident registration (http://www.kosis.kr) were used.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics, version 21.0 (IBM Corp., Armonk, NY, USA) and MedCalc, version 15.6 (MedCalc Software, Ostend, Belgium). Categorical variables were compared between the seropositive and seronegative groups by Pearson’s χ2 test and Cochran-Armitage trend test. A two-sided P value < 0.05 was considered to indicate statistical significance.
Ethics statement
The study protocol was approved by the Institutional Review Board of Pusan National University Hospital (No. E-2015087). Informed consent was exempted by the board.
RESULTS
A total of 1,069 serum samples was randomly selected and subjected to ELISA for SFTSV. The median age of the patients was 59 years (range 12 days–96 years), and 51.5% were male. The most common residence of the patients was Busan (838/1,069), followed by Gyeongnam Province (191/1,069) and Ulsan Metropolitan City (23/1,069).
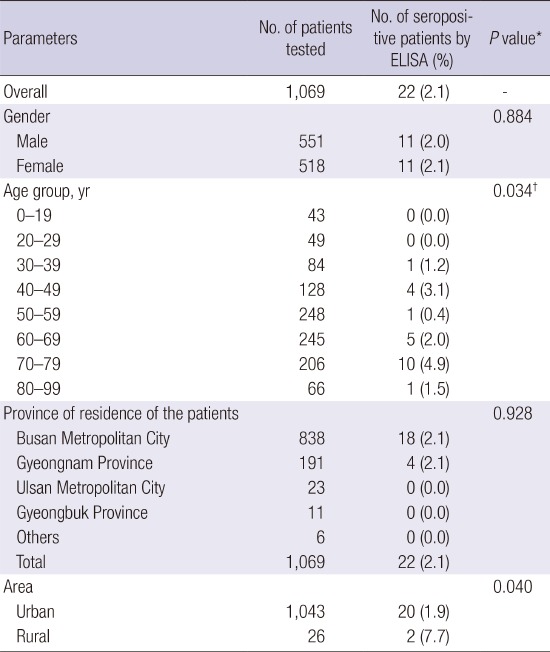
Overall, 22 patients (2.1%) were positive for anti-SFTSV antibodies (Table 1). No significant difference in seropositivity according to gender was detected. Patients aged 70–79 years had the highest seropositivity rate. SFTSV seroprevalence increased significantly with age (P = 0.034). All seropositive patients were from Busan (2.1%, 18/838) and Gyeongnam Province (2.1%, 4/191). According to the classification of urban vs. rural, the seropositivity rate was higher in patients from rural areas than in those from urban areas (7.7% vs. 1.9%, P=0.040).
Table 1. Seroprevalence of SFTS according to demographic characteristics in patients who visited a tertiary hospital located in southeastern Korea, 2015.
| Parameters | No. of patients tested | No. of seropositive patients by ELISA (%) | P value* |
|---|---|---|---|
| Overall | 1,069 | 22 (2.1) | - |
| Gender | 0.884 | ||
| Male | 551 | 11 (2.0) | |
| Female | 518 | 11 (2.1) | |
| Age group, yr | 0.034† | ||
| 0–19 | 43 | 0 (0.0) | |
| 20–29 | 49 | 0 (0.0) | |
| 30–39 | 84 | 1 (1.2) | |
| 40–49 | 128 | 4 (3.1) | |
| 50–59 | 248 | 1 (0.4) | |
| 60–69 | 245 | 5 (2.0) | |
| 70–79 | 206 | 10 (4.9) | |
| 80–99 | 66 | 1 (1.5) | |
| Province of residence of the patients | 0.928 | ||
| Busan Metropolitan City | 838 | 18 (2.1) | |
| Gyeongnam Province | 191 | 4 (2.1) | |
| Ulsan Metropolitan City | 23 | 0 (0.0) | |
| Gyeongbuk Province | 11 | 0 (0.0) | |
| Others | 6 | 0 (0.0) | |
| Total | 1,069 | 22 (2.1) | |
| Area | 0.040 | ||
| Urban | 1,043 | 20 (1.9) | |
| Rural | 26 | 2 (7.7) |
SFTS = severe fever with thrombocytopenia syndrome, ELISA = enzyme-linked immunosorbent assay.
*Categorical variables were compared between the seropositive and seronegative groups by Pearson’s χ2 test. A two-sided P value < 0.05 was considered to indicate statistical significance; †Age-related trend in seropositivity rate was evaluated using the Cochran-Armitage trend test.
Seropositive rates were not significantly different among underlying diseases (Table 2). Non-malignant disease without immunosuppressive therapy, including liver, renal, endocrine diseases and others, and health checkup comprised more than two thirds of the underlying diseases. None of the antibody-positive patients showed typical symptoms or laboratory findings of SFTS or other infectious diseases during the study period. The real-time RT-PCR SFTSV results of all seropositive patients were negative.
Table 2. Seroprevalence of SFTS according to underlying diseases in patients who visited a tertiary hospital located in southeastern Korea, 2015.
| Underlying diseases* | No. of patients tested | No. of seropositive patients by ELISA (%) |
|---|---|---|
| Non-malignant disease | ||
| without immunosuppressive therapy | 670 | 10 (1.5) |
| with immunosuppressive therapy† | 34 | 0 (0.0) |
| Malignant disease | ||
| without chemotherapy or immunosuppressive therapy | 219 | 6 (2.7) |
| with chemotherapy or immunosuppressive therapy‡ | 74 | 4 (5.4) |
| HIV infection | 12 | 0 (0.0) |
| Health checkup | 55 | 2 (3.6) |
| Information not available | 5 | 0 (0.0) |
SFTS = severe fever with thrombocytopenia syndrome, ELISA = enzyme-linked immunosorbent assay, HIV = human immunodeficiency virus.
*Seropositive rates were not significantly different among underlying diseases (P = 0.283); †Includes patients who have received immunosuppressive therapy within recent 3 months from acquisition of serum sample for ELISA; ‡Includes patients who have received chemotherapy or immunosuppressive therapy within recent 3 months from acquisition of serum sample for ELISA.
DISCUSSION
We determined the seropositive rate of SFTS in southeastern Korea. This is the first seroprevalence study of a large population in the country. According to the urban vs. rural classification, the seropositivity rate was higher in patients from rural than from urban areas (7.7% vs. 1.9%, P = 0.040), which is in agreement with a previous study in China (7.52% vs. 4.26%) (14). SFTS seroprevalence increased significantly with age (P = 0.034), which is consistent with previous studies in China (9,14). This can be due to the possibility that elderly subjects have had more opportunities to be exposed to SFTSV throughout their lifetime. However, this age-cumulative effect may not entirely explicate the higher seroprevalence in the elderly. In a previous study, SFTSV-IgG disappeared at around 44 months post infection (18). This finding can also suggest that contact with ticks increases with age and is consistent with the higher mean age in rural than in urban areas (69.3 vs. 56.1, P < 0.001). There were no significant differences in seropositive rates of SFTS among underlying diseases. Therefore, seropositive rates may not be affected by immunosuppression.
In a previous study from Xinyang, China, the seroprevalence of low-annual-incidence areas (0.17/1,000,000) was 6.12%, whereas that in high-annual-incidence areas (22.52/1,000,000) was 8.36% (14). In this study, the seroprevalence in Busan and Gyeongnam Province was 2.1% and 2.1%, respectively. The annual-incidence was 0.00–0.28 and 1.49–2.97/1,000,000 during the 2-year period between 2013 and 2015. The annual incidence rate might have not associated with the seroprevalence. The ecological and environmental differences between Xinyang and Busan may explain the different seropositivity rates. In addition, the average temperatures between April and November, the months when SFTS is prevalent, is higher in Xinyang than in Busan. Specifically, the average low and high temperatures between April and November are 7.8°C–23.4°C and 13.6°C–25.9°C in Busan and 5.9°C–23.9°C and 15.4°C–31.6°C in Xinyang (19,20). Higher temperatures result in the faster development, shorter life cycle, and increased activity of ticks (21). In Busan, only a small percentage (–0.006%) of the population is involved in farming, such that few people are at risk of SFTS. During 2013–2015, only 1 case was reported in Busan, where the seropositive rate was 2.1%. Therefore, subclinical cases or cases misdiagnosed as other well-known infectious diseases, such as scrub typhus, cannot be ruled out.
There were limitations in this study. The study hospital is located in the downtown area and most of its patients reside in the surrounding urban area. Because the tested samples were randomly selected from the leftover samples of patients, information regarding tick exposure, occupation, outdoor activities, and prior symptoms and signs of SFTS could not be collected from the study population.
In conclusion, the SFTSV seroprevalence of a large population in southeastern area of Korea was 2.1%. However, because this study was based on a tertiary hospital, the seropositivity rate may differ from that of the general population. Further study is needed to identify risk factors for exposure, and nationwide surveillance of SFTSV seroprevalence should be conducted in Korea.
Footnotes
Funding: This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant number NRF-2014R1A1A4A01009748).
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study design: Kim KH, Ko MK, Yi J. Enzyme-linked immunosorbent assay (ELISA): Kim KH, Ko MK, Yi J. Collection of samples: Kim KH, Ko MK, Kim N, Kim HH, Yi J. Writing manuscript: Kim KH, Yi J. Analysis and interpretation of data: Kim KH, Ko MK, Yi J. Revision and final approval of manuscript: all authors.
References
- 1.Yu XJ, Liang MF, Zhang SY, Liu Y, Li JD, Sun YL, Zhang L, Zhang QF, Popov VL, Li C, et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N Engl J Med. 2011;364:1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu Q, He B, Huang SY, Wei F, Zhu XQ. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect Dis. 2014;14:763–772. doi: 10.1016/S1473-3099(14)70718-2. [DOI] [PubMed] [Google Scholar]
- 3.Kim KH, Yi J, Kim G, Choi SJ, Jun KI, Kim NH, Choe PG, Kim NJ, Lee JK, Oh MD. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerg Infect Dis. 2013;19:1892–1894. doi: 10.3201/eid1911.130792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korean Centers for Disease Control and Prevention. Prevention of severe fever with thrombocytopenia syndrome [Internet] [accessed on 6 June 2016]. Available at http://www.cdc.go.kr/CDC/notice/CdcKrIntro0201.jsp?menuIds=HOME001-MNU0005-MNU0011&fid=21&q_type=&q_value=&cid=20790&pageNum=1.
- 5.Shin J, Kwon D, Youn SK, Park JH. Characteristics and factors associated with death among patients hospitalized for severe fever with thrombocytopenia syndrome, South Korea, 2013. Emerg Infect Dis. 2015;21:1704–1710. doi: 10.3201/eid2110.141928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao L, Zhai S, Wen H, Cui F, Chi Y, Wang L, Xue F, Wang Q, Wang Z, Zhang S, et al. Severe fever with thrombocytopenia syndrome virus, Shandong Province, China. Emerg Infect Dis. 2012;18:963–965. doi: 10.3201/eid1806.111345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui F, Cao HX, Wang L, Zhang SF, Ding SJ, Yu XJ, Yu H. Clinical and epidemiological study on severe fever with thrombocytopenia syndrome in Yiyuan County, Shandong Province, China. Am J Trop Med Hyg. 2013;88:510–512. doi: 10.4269/ajtmh.11-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ding S, Niu G, Xu X, Li J, Zhang X, Yin H, Zhang N, Jiang X, Wang S, Liang M, et al. Age is a critical risk factor for severe fever with thrombocytopenia syndrome. PLoS One. 2014;9:e111736. doi: 10.1371/journal.pone.0111736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Z, Hu J, Bao C, Li P, Qi X, Qin Y, Wang S, Tan Z, Zhu Y, Tang F, et al. Seroprevalence of antibodies against SFTS virus infection in farmers and animals, Jiangsu, China. J Clin Virol. 2014;60:185–189. doi: 10.1016/j.jcv.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 10.Liang S, Bao C, Zhou M, Hu J, Tang F, Guo X, Jiao Y, Zhang W, Luo P, Li L, et al. Seroprevalence and risk factors for severe fever with thrombocytopenia syndrome virus infection in Jiangsu Province, China, 2011. Am J Trop Med Hyg. 2014;90:256–259. doi: 10.4269/ajtmh.13-0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun JM, Zhang YJ, Gong ZY, Zhang L, Lv HK, Lin JF, Chai CL, Ling F, Liu SL, Gu SP, et al. Seroprevalence of severe fever with thrombocytopenia syndrome virus in southeastern China and analysis of risk factors. Epidemiol Infect. 2015;143:851–856. doi: 10.1017/S0950268814001319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang L, Sun J, Yan J, Lv H, Chai C, Sun Y, Shao B, Jiang J, Chen Z, Kortekaas J, et al. Antibodies against severe fever with thrombocytopenia syndrome virus in healthy persons, China, 2013. Emerg Infect Dis. 2014;20:1355–1357. doi: 10.3201/eid2008.131796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L, Ye L, Ojcius DM, Lou X, Wang C. feng C, Sun Y, Wang Z, Li S, Zhang Y. Characterization of severe fever with thrombocytopenia syndrome in rural regions of Zhejiang, China. PLoS One. 2014;9:e111127. doi: 10.1371/journal.pone.0111127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu C, Guo C, Yang Z, Wang L, Hu J, Qin S, Cui N, Peng W, Liu K, Liu W, et al. The severe fever with thrombocytopenia syndrome bunyavirus (SFTSV) antibody in a highly endemic region from 2011 to 2013: a comparative serological study. Am J Trop Med Hyg. 2015;92:479–481. doi: 10.4269/ajtmh.14-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wei J, Li S, Dong JH, Tian H, Chowell G, Tian HY, Lv W, Han ZQ, Xu B, Yu PB, et al. The first human infection with severe fever with thrombocytopenia syndrome virus in Shaanxi Province, China. Int J Infect Dis. 2015;35:37–39. doi: 10.1016/j.ijid.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 16.Zeng P, Ma L, Gao Z, Wang J, Liu J, Huang X, Yang Q, Cao R, Wen X, Zhu L, et al. A study of seroprevalence and rates of asymptomatic viremia of severe fever with thrombocytopenia syndrome virus among Chinese blood donors. Transfusion. 2015;55:965–971. doi: 10.1111/trf.12953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jiao Y, Zeng X, Guo X, Qi X, Zhang X, Shi Z, Zhou M, Bao C, Zhang W, Xu Y, et al. Preparation and evaluation of recombinant severe fever with thrombocytopenia syndrome virus nucleocapsid protein for detection of total antibodies in human and animal sera by double-antigen sandwich enzyme-linked immunosorbent assay. J Clin Microbiol. 2012;50:372–377. doi: 10.1128/JCM.01319-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lu QB, Cui N, Hu JG, Chen WW, Xu W, Li H, Zhang XA, Ly H, Liu W, Cao WC. Characterization of immunological responses in patients with severe fever with thrombocytopenia syndrome: a cohort study in China. Vaccine. 2015;33:1250–1255. doi: 10.1016/j.vaccine.2015.01.051. [DOI] [PubMed] [Google Scholar]
- 19.Korea Meteorological Administration. Monthly Normals of Busan, 1981–2010. Seoul: Korea Meteorological Administration; 2011. [Google Scholar]
- 20.China Meteorological Administration. Average Temperatures of Xinyang, Henan, China. Beijing: China Meteorological Administration; [Google Scholar]
- 21.Ogden NH, Lindsay LR. Effects of climate and climate change on vectors and vector-borne diseases: ticks are different. Trends Parasitol. 2016;32:646–656. doi: 10.1016/j.pt.2016.04.015. [DOI] [PubMed] [Google Scholar]


