Abstract
BACKGROUND:
Healthcare professionals are expected to have knowledge of current basic and advanced cardiac life support (BLS/ACLS) guidelines to revive unresponsive patients.
METHODS:
A cross-sectional study was conducted to evaluate the current practices and knowledge of BLS/ACLS principles among healthcare professionals of North-Kerala using pretested self-administered structured questionnaire. Answers were validated in accordance with American Heart Association’s BLS/ACLS teaching manual and the results were analysed.
RESULTS:
Among 461 healthcare professionals, 141 (30.6%) were practicing physicians, 268 (58.1%) were nurses and 52 (11.3%) supporting staff. The maximum achievable score was 20 (BLS 15/ACLS 5). The mean score amongst all healthcare professionals was 8.9±4.7. The mean score among physicians, nurses and support staff were 8.6±3.4, 9±3.6 and 9±3.3 respectively. The majority of healthcare professionals scored ≤50% (237, 51.4%); 204 (44.3%) scored 51%–80% and 20 (4.34%) scored >80%. Mean scores decreased with age, male sex and across occupation. Nurses who underwent BLS/ACLS training previously had significantly higher mean scores (10.2±3.4) than untrained (8.2±3.6, P=0.001). Physicians with <5 years experience (P=0.002) and nurses in the private sector (P=0.003) had significantly higher scores. One hundred and sixty three (35.3%) healthcare professionals knew the correct airway opening manoeuvres like head tilt, chin lift and jaw thrust. Only 54 (11.7%) respondents were aware that atropine is not used in ACLS for cardiac arrest resuscitation and 79 (17.1%) correctly opted ventricular fibrillation and pulseless ventricular tachycardia as shockable rhythms. The majority of healthcare professionals (356, 77.2%) suggested that BLS/ACLS be included in academic curriculum.
CONCLUSION:
Inadequate knowledge of BLS/ACLS principles amongst healthcare professionals, especially physicians, illuminate lacunae in existing training systems and merit urgent redressal.
KEY WORDS: Basic life support, Advanced cardiac life support, Healthcare professionals, Awareness, Cardiopulmonary resuscitation
INTRODUCTION
The American Heart Association (AHA) frames and periodically updates Cardiopulmonary Resuscitation (CPR) and Emergency Cardiac Care (ECC) guidelines on how to provide basic and advanced cardiac life support (BLS/ACLS) to resuscitate valuable lives.[1] CPR is a simple and effective procedure if the skill required is maintained by frequent training.[2] Healthcare professionals are expected to have current knowledge of BLS/ACLS guidelines to revive unresponsive and cardiac arrest patients. Unlike in Western countries, there are no strict licensing protocols in India and other developing countries that mandate physicians, nurses and paramedics to be trained in current BLS/ACLS guidelines.
Kerala is a state in India with 100 percent literacy rate and an exemplary healthcare model with health indices approaching international standards.[3] Hence, public expectations from healthcare professionals in emergency care are also high. Studies of BLS/ACLS knowledge among physicians and nurses who are in the forefront of medical care are lacking in India, particularly from Kerala. Previous studies were mostly done among interns, homeopaths, medical, nursing and dental students, who are often not directly responsible for emergency patient care.[4–6] Hence, the current study assessed BLS/ACLS knowledge amongst a broad sample of Keralite healthcare professionals who are directly involved in emergency care. The objective was to evaluate their current knowledge of BLS/ACLS guidelines and to suggest remedial measures to tackle any deficiencies.
METHODS
Study subjects
This cross-sectional study was conducted among healthcare professionals including practicing physicians, nurses and support staff in public and private hospitals and clinics of North-Kerala. Practicing physicians included doctors with basic medical degree, specialisations or sub-specialisations and were either running their own clinics or were attached to hospitals. Registered nurses were either degree/diploma holders in general nursing and midwifery. Support staff included nursing assistants (auxiliary nursing midwifery diploma holders) and paramedics.
Inclusion criteria
All private and government hospitals with Intensive Care Units and Emergency services were identified and listed. Among the listed hospitals, 7 private and 7 government hospitals were randomly selected. Physicians, nurses and support staff from these hospitals were recruited by means of pamphlets and announcements and those who volunteered were included in the study. Physicians working in clinics were listed and randomly selected. All those who consented to respond were included in the study. Respondents were free to opt out from the study anytime.
Exclusion criteria
We excluded interns, medical, dental, nursing and paramedical students from participating. Furthermore, non-practicing physicians and indigenous medical practitioners were also excluded.
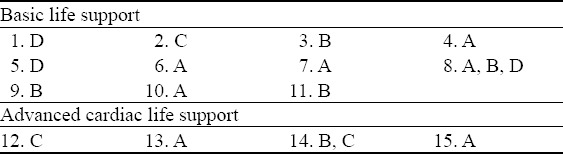
Study tool
A self-administered structured questionnaire with demographic characteristics, academic profile and multiple choice questions (Table 1) on BLS/ACLS was the study tool. Questions were prepared by the investigators based on AHA 2010 guidelines (prevailing at the time of study) with a maximum score of 20 (15 for BLS/5 for ACLS) and was pilot pretested among Emergency Department staff at our hospital. Answers to BLS/ACLS related questions (Table 2) were validated in accordance with AHA’s teaching manual.[1] Participant opinion regarding the inclusion of BLS/ACLS in academic healthcare curriculum and the preferred mode of training was also sought.
Table 1.
BLS/ACLS questionnaire
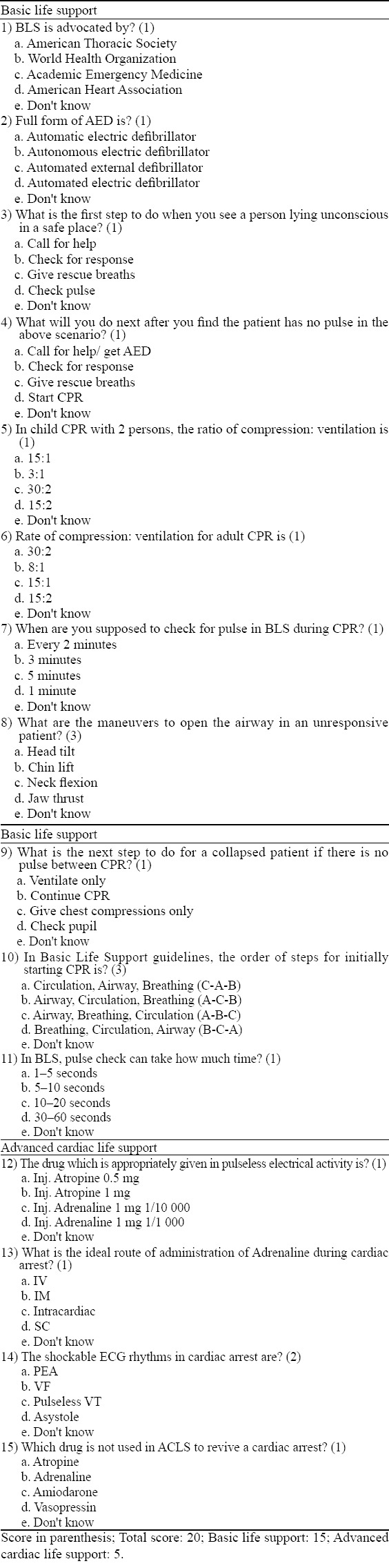
Table 2.
Answers to questions
Ethical approval
The study received approval from the Institutional Research and Ethics Committee and was conducted from October to December 2014.
Data collection
Data was collected from study participants by the authors in person from hospitals and their respective workplaces after prior written informed consent was obtained. Data that would reveal the identity of participants in any manner were not collected. To minimize any bias in answering the questionnaire, a 10-minute response time period was maintained during which discussions among participants were not permitted. Clear instructions as to certain questions requiring multiple answers were also provided.
Statistical analysis
Data collected was entered in MS Excel Spread sheet and, analysed using EPI INFO 7.0. Appropriate statistical methods including ANOVA, Student t-test and multivariate logistic regression analysis were applied. Accounting for Bonferonni correction, a P value <0.005 was considered statistically significant.
RESULTS
Out of a total 462 respondents, one was excluded from further analysis due to missing data. The basic characteristics of study participants were summarised in Table 3.
Table 3.
Study participant characteristics in BLS/ACLS study
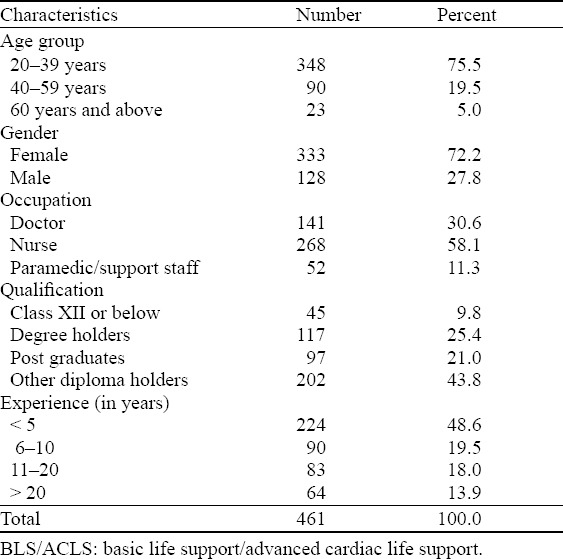
The mean score among respondents was 8.9±4.7 out of 20. The mean score among physicians was the least (8.6±3.4). Nurses and support staff had relatively higher mean scores, with (9±3.6), (9±3.3) respectively. Mean scores in general were noted to decrease with age (P=0.03), male sex (P=0.007) and occupation being doctor (P=0.009).
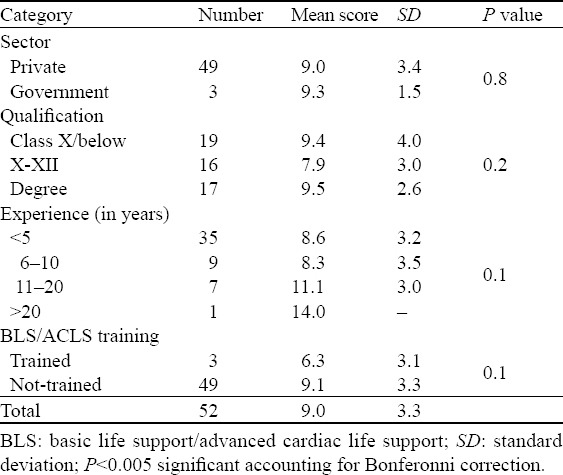
Among the 461 study participants, 178 (38.6%) reported as having attended both BLS and ACLS workshops. Those who underwent BLS/ACLS training previously had significantly higher mean scores compared to the 283 untrained persons (9.5±3.4 vs. 8.5±3.5, P=0.002). Nurses who underwent BLS/ACLS training achieved significantly higher scores than untrained nurses (10.2±3.4 vs. 8.2±3.6, P=0.001). Physicians with less than five years of experience (P=0.002) and nurses of private sector (P=0.003) had significantly better scores (Tables 4, 5). Prior BLS/ACLS training did not improve the mean score among physicians (8.5±3.2 vs. 8.6±3.6, P=0.82) among support staff where, in fact, the score trended lower with BLS/ACLS training (9.1±3.3 vs. 6.3±3.1, P=0.10) as shown in Tables 4 and 6 respectively.
Table 4.
Scoring patterns across categories among physicians in BLS/ACLS study
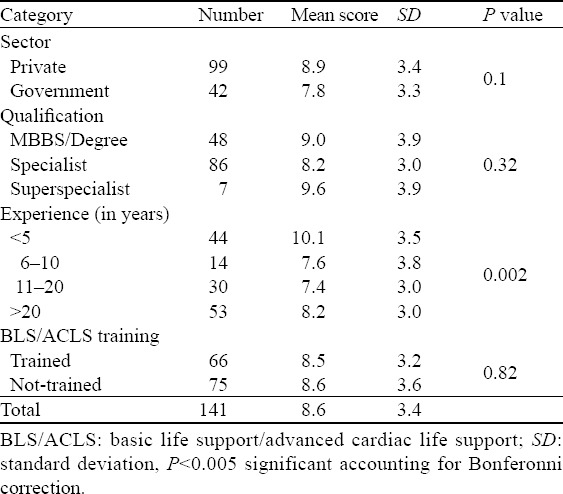
Table 5.
Scoring patterns across categories among nurses in BLS/ACLS study
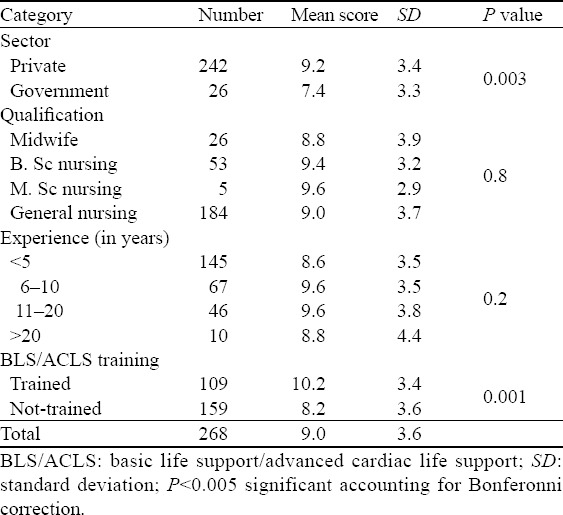
Table 6.
Scoring patterns across categories among support staff in BLS/ACLS study
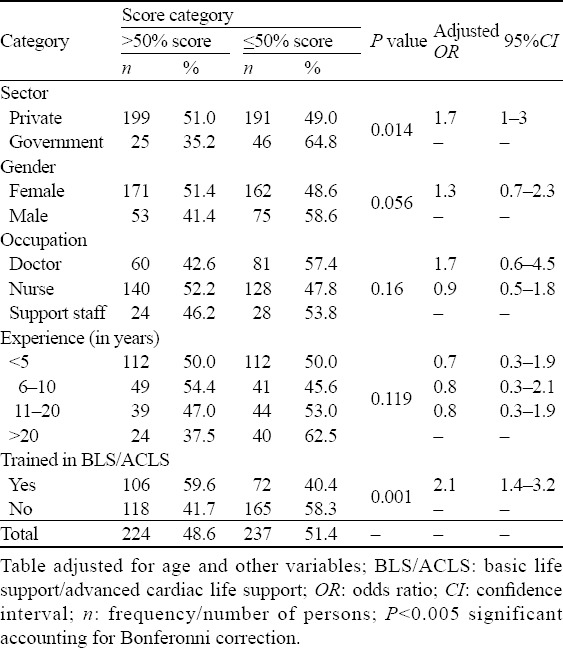
The majority of respondents scored ≤50% (237, 51.4%); 204 (44.3%) scored 51%–80% and 20 (4.3%) scored >80%, differences existing between occupational groups of healthcare professionals (P=0.009). On comparing groups with a cut-off mark of 50%, it was observed after logistic regression analysis that prior BLS/ACLS training (P=0.001) and private sector employment (P=0.014) were independent predictors of higher scores. Table 7.
Table 7.
Multivariate logistic regression analysis of variables across score categories
Knowledge assessment
Two hundred and forty seven (53.6%) respondents knew that BLS and ACLS were propounded by the AHA. The correct meaning of an automated external defibrillator (AED) was known to 249 (54%) respondents. Two hundred and thirty three (50.5%) respondents knew the correct order of BLS resuscitation as Circulation–Airway-Breathing (C-A-B). Two hundred and forty five (53.1%) respondents correctly answered that they would first check for response on finding a cardiac arrest patient in a safe scene. More than half the respondents (256, 55.5%) were aware that the compression: ventilation ratio in adult CPR was 30:2 but only 183 (39.7%) knew that it was 15:2 in child CPR with two rescuers. As many as 187 (40.6%) respondents correctly knew that pulse checks should be carried out every two minutes and 175 (38%) persons knew that pulse checks should not take more than 5–10 seconds. About two-thirds (306, 66.4%) responded that CPR is to be continued if there was no pulse amidst resuscitation. One hundred and sixty three (35.3%) respondents knew all three airway opening manoeuvres including head tilt, chin lift and jaw thrust. Two-third of therespondents (308, 66.8%) opted for head tilt, 366 (79.39%) for chin lift and 237 (51.41 %) opted for jaw thrust without knowing that all the three were airway opening manoeuvres.
Whereas 212 (46%) were aware of the correct dose and route of adrenaline administration in the setting of cardiac arrest, 59 (12.8%) wrongly marked the route as intramuscular. About 25.4% (117) wrongly considered atropine as the drug of choice in cardiac arrest and only 54 (11.7%) respondents were aware that atropine was not used in ACLS resuscitation for reviving cardiac arrest. Seventy nine (17.1%) respondents correctly identified both ventricular fibrillation and pulseless ventricular tachycardia as shockable rhythms. Nearly one-third (155, 33.6%) responded to only ventricular fibrillation and 133 (28.9%) recorded only pulseless ventricular tachycardia as shockable rhythms.
As many as 356 (77.2%) respondents suggested that BLS/ACLS should be included as mandatory teaching in the academic curriculum for all healthcare professionals. A majority (408, 88.5%) agreed on the need for frequent training of healthcare professionals on BLS/ACLS principles to keep themselves updated. The most preferred mode was a three-day workshop than conferences/lectures.
DISCUSSION
The primary outcome measure in this study was knowledge of BLS/ACLS guidelines among healthcare professionals in North-Kerala who were involved in emergency patient care. Our study found a low level of knowledge in BLS/ACLS, with a mean score of 44.5%. Though, different measures of BLS/ACLS guidelines were used in similar studies, the mean score of respondents in the current study was comparable to 41.6% in a previous South-Indian study by Aroor et al[5] and marginally higher compared to 36.05% in a study of Indian dentists by Baduni et al.[6] The mean score was comparable to a Nepalese study by Roshana et al[7] (44%). A greater than 50% score was achieved by 48.6% of the participants in our study, compared to <25% in the South African study by Raghavan et al[8] and South-Indian study by Chandrasekharan et al[4] (15.18%). Participants of this study also had better scores compared to a recent study on knowledge of BLS/ACLS among medical students and interns in New Delhi, India by Sinha et al.[9] It should be noted that only 4.3% of the participants in our study surpassed the >80% standard set by AHA.
A progressive decline in scores with male sex, and significantly so among physicians with more experience are of concern, as the archetypal Indian patient population generally tends to look up to the ‘aged, male doctor’ in emergencies. Whereas Bjornsson et al[10] concluded that physician’s experience did not improve cardiac arrest outcome, the current study noted a decline in the knowledge levels of physicians with experience. A decrease in the knowledge base of senior doctors in comparison to junior doctors was reported by Zamir et al[11] from Rawalpindi, Pakistan. However, the latter study had interns and medical/dental students as the majority participants. A study by Lima et al[12] noted, the level of knowledge in BLS and ACLS among nurses to be inversely proportional to the time elapsed since the completion of their undergraduate or technical course. Our results were in line with this; however the same appears true among all healthcare workers, especially physicians.
Physicians were less knowledgeable than nurses and support staff in BLS/ACLS guidelines as reflected by their lower scores in this study. Lack of strict professional accreditation policies in India and limited enthusiasm to refresh BLS/ACLS skills among subset of physicians over time could be contributory factors. In this study, BLS and ACLS training were seen to only marginally enhance the mean scores by 8.1%, as against a two-thirds improvement (68.4%) of knowledge and skill of CPR following BLS training as reported by Chaudhari et al.[13] This may be due to the inconsistent time lag between BLS/ACLS training received by participants and this study, whereas most other studies compared knowledge gain by virtue of a pre-training and an immediate post-training questionnaire. BLS/ACLS training was however seen to have significant impact only among nursing population in this study. This may be attributable to the fact that nurses who are keen to migrate to other countries for professional satiety are compelled to update their knowledge of BLS/ACLS guidelines. Though not statistically significant, the mean scores were unexpectedly low after training in BLS/ACLS among support staff. This may be due to lack of formal professional education and lack of frequent patient exposure or regular practice of BLS/ACLS and is a plausible research area worth further exploration. A majority of healthcare professionals (77.2%) in our study recommended that BLS/ACLS training should to be part of professional healthcare curriculum, Sinha et al[9] study where 96% of medical students and interns stressed the same.
The fact that this study was conducted among healthcare professionals from Kerala, a state renowned for 100% literacy and exemplary healthcare model that is comparable with international standards, and yet reveals a low knowledge of BLS/ACLS principles among its healthcare workers is alarming. Despite BLS and ACLS being emphasized in the Indian context for more than a decade now, the standards of knowledge of physicians in this regard are still low and are a matter of concern. This needs to be rectified and we believe, the apex health authorities must develop accreditation policies to maintain standards of primary resuscitation and emergency care among healthcare professionals. Our study adds to available Indian evidence about life support practices which were mostly studies done on interns and students. As only actively practicing registered physicians and nursing staff were part of this study, our findings reflect the pulse of current emergency healthcare in this part of the world.
Limitations
Since this was a questionnaire-based study, assessment of skill and presence of mind in putting into action the participants’ theoretical knowledge of BLS/ACLS could not be assessed in detail. Moreover, the questionnaire used in this study differed from those used in other studies making exact comparisons difficult. It is a documented fact that the skills of CPR are difficult to teach and once learnt difficult to retain.[14,15] The time elapsed since training in BLS/ACLS grouped as two years or more was a pitfall in the current study and hence, a detailed analysis of drain in the skills with respect to time was not possible.
Future research is needed to ponder the insufficient improvement in knowledge among health professionals, particularly physicians even after formal BLS/ACLS training. Practical assessment of the delivery of emergency services like BLS/ACLS should also be considered. The reason why emergency care and critical illness research is still in the archaic phase in developing countries like India is obviously the lack of awareness of clinicians and healthcare professionals in this field, as pointed out earlier. This study would add to epidemiological data to help improve patient care and health policy making across the globe in the field of emergency services in relation to developing countries.
In conclusion, despite the emphasis for over a decade, a low level of knowledge on BLS and ACLS among healthcare workers, particularly the Keralite physicians in in this study, is a matter of concern. A strict accreditation/licensing programme and periodic revision of life saving practices is the need of the hour. Inadequate improvement in knowledge levels even after BLS/ACLS training also points to an urgent need for innovative educational programs with an impetus for novel life support skills training in healthcare curriculum. This would help improve clinical practices, motivate better emergency care and foster research among future health professionals in this field in addition to bettering resuscitation skills-training.
ACKNOWLEDGEMENTS
Dr. Suresh G, HOD and Professor, Emergency Medicine, ACME, Pariyaram, Kannur, Kerala for his valuable support in general for this project. Dr. P.V. Aboobacker, Senior Resident, Emergency Medicine, ACME, Pariyaram, Kannur, Kerala for helping us reach out to more number of healthcare professionals in North-Malabar region. We would like to thank Matthew Douma, Nurse educator, Alberta Health Services, Canada and Dr. K.K. Suresh Kumar, Associate Professor of Medicine, Temple University, USA for their help in revising the manuscript.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Research and Ethics Committee.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Nambiar M proposed the study. Nambiar M and Nedungalaparambil NM drafted the manuscript. All authors read and approved the final version of the paper.
REFERENCES
- 1.Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, et al. Part 1: executive summary 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 suppl 3):S640–56. doi: 10.1161/CIRCULATIONAHA.110.970889. [DOI] [PubMed] [Google Scholar]
- 2.Berden HJ, Bierens JJ, Willems FF, Hendrick JM, Pijls NH, Knape JT. Resuscitation skills of lay public after recent training. Ann Emerg Med. 1994;23:1003–1008. doi: 10.1016/s0196-0644(94)70094-x. [DOI] [PubMed] [Google Scholar]
- 3.Sen A. Health in development. Bull World Health Organ. 1999;77:619–623. [PMC free article] [PubMed] [Google Scholar]
- 4.Chandrasekaran S, Kumar S, Bhat SA, Saravanakumar Shabbir PM, Chandrasekaran V. Awareness of basic life support among medical, dental, nursing students and doctors. Indian J Anaesth. 2010;54:121–126. doi: 10.4103/0019-5049.63650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aroor AR, Saya RP, Attar NR, Saya GK, Ravinanthanan M. Awareness about basic life support and emergency medical services and its associated factors among students in a tertiary care hospital in South India. J Emerg Trauma Shock. 2014;7:166. doi: 10.4103/0974-2700.136857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baduni N, Prakash P, Srivastava D, Sanwal MK, Singh BP. Awareness of basic life support among dental practitioners. Natl J Maxillofac Surg. 2014;5:19. doi: 10.4103/0975-5950.140159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roshana S, Batajoo KH, Piryani RM, Sharma MW. Basic life support: knowledge and attitude of medical/paramedical professionals. World J Emerg Med. 2012;3:141. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ragavan S, Schneider H, Kloeck WG. Basic resuscitation—knowledge and skills of full-time medical practitioners at public hospitals in northern province. S Afr Med J. 2000;90:504. [PubMed] [Google Scholar]
- 9.Sinha A, Mayank M. Basic life support and advanced cardiac life support: knowledge of medical students in New Delhi. Journal of Young Medical Researchers. 2015;1:25–30. [Google Scholar]
- 10.Bjornsson HM, Marelsson S, Magnusson V, Sigurdsson G, Thorgeirsson G. Physician experience in addition to ACLS training does not significantly affect the outcome of prehospital cardiac arrest. Eur J Emerg Med. 2011;18:64. doi: 10.1097/MEJ.0b013e32833c6642. [DOI] [PubMed] [Google Scholar]
- 11.Zamir Q, Nadeem A, Rizvi AH. Awareness of cardiopulmonary resuscitation in medical-students and physicians in Rawalpindi-Islamabad, Pakistan. J Pak Med Assoc. 2012;62:1361–1364. [PubMed] [Google Scholar]
- 12.Lima SG, Macedo LA, Vidal ML, Sá MP. Permanent Education in BLS and ACLS: impact on the knowledge of nursing professionals. Arq Bras Cardiol. 2009;93:582. doi: 10.1590/s0066-782x2009001200012. [DOI] [PubMed] [Google Scholar]
- 13.Chaudhary A, Parikh H, Dave V. Current scenario: knowledge of basic life support in medical college. National Journal of Medical Research. 2011;1:80–82. [Google Scholar]
- 14.Christenson J, Nafziger S, Compton S, Vijayaraghavan K, Slater B, Ledingham R, et al. The effect of time on CPR and automated external defibrillator skills in the Public Access Defibrillation Trial. Resuscitation. 2007;74:52–62. doi: 10.1016/j.resuscitation.2006.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sternbach GL. The retention of cardiopulmonary resuscitation skills. J Emerg Med. 1984;2:33. doi: 10.1016/0736-4679(84)90046-5. [DOI] [PubMed] [Google Scholar]


