Monitoring pathogen emergence provides insight into how pathogens adapt in the human population. Secreted virulence factors, important contributors to infections, may differ in a manner dependent on the strain and host. Temporal changes of Staphylococcus aureus toxigenic potential, for example, in encoding toxic shock syndrome toxin 1 (TSST-1), contributed to an epidemic of TSS with significant health impact. This study monitored changes in atopic dermatitis (AD) S. aureus isolates and demonstrated both temporal and host infection differences according to host race based on secreted superantigen potential. The current temporal increase in enterotoxin gene cluster superantigen prevalence and lack of the gene encoding TSST-1 in AAs predict differences in infection types and presentations.
KEYWORDS: atopic dermatitis, clonal groups, phenotype, race, Staphylococcus aureus, superantigens
ABSTRACT
Atopic dermatitis (AD) is an inflammatory skin condition strongly associated with Staphylococcus aureus colonization and infection. S. aureus strains shift in populations in ~10-year intervals depending on virulence factors. Shifts in S. aureus virulence factors may in part explain the racial differences observed in the levels of prevalence and severity of AD. AD S. aureus isolates collected from 2011 to 2014 (103 isolates) and in 2008 (100 isolates) were examined for the prevalence of genes encoding superantigens (SAgs). The strains from 2011 to 2014 were obtained from AD patients as a part of the National Institute of Allergy and Infectious Diseases (NIAID) Atopic Dermatitis Research Network (ADRN). The prevalence of SAg genes was investigated temporally and racially. The enterotoxin gene cluster (EGC) was more prevalent in the 2011–2014 AD isolates than in the 2008 AD isolates. The prevalences of virulence factor genes were similar in European American (EA) and Mexican American (MA) patients but differed in 6 of 22 SAg genes between EA and African American (AA) or MA and AA isolates; notably, AA isolates lacked tstH, the gene encoding toxic shock syndrome toxin 1 (TSST-1). The presence of tstH and sel-p (enterotoxin-like P) was associated with decreased clinical severity and increased blood eosinophils, respectively. The EGC is becoming more prevalent, consistent with the previously observed 10 years of cycling of S. aureus strains. Race-specific S. aureus selection may account for differences in virulence factor profiles. The lack of TSST-1-positive (TSST-1+) AD S. aureus in AA is consistent with the lack of AAs acquiring TSST-1-associated menstrual toxic shock syndrome (TSS).
IMPORTANCE Monitoring pathogen emergence provides insight into how pathogens adapt in the human population. Secreted virulence factors, important contributors to infections, may differ in a manner dependent on the strain and host. Temporal changes of Staphylococcus aureus toxigenic potential, for example, in encoding toxic shock syndrome toxin 1 (TSST-1), contributed to an epidemic of TSS with significant health impact. This study monitored changes in atopic dermatitis (AD) S. aureus isolates and demonstrated both temporal and host infection differences according to host race based on secreted superantigen potential. The current temporal increase in enterotoxin gene cluster superantigen prevalence and lack of the gene encoding TSST-1 in AAs predict differences in infection types and presentations.
INTRODUCTION
Atopic dermatitis (AD) is the most common chronic inflammatory skin disease in the general population. AD is often a T helper 2 (Th2)-mediated disease, accompanied by increased serum total IgE production, circulating interleukin-4 (IL-4)/IL-13-expressing T cells, and eosinophilia (1–3). It is often associated with skin infections caused by herpes simplex virus and Staphylococcus aureus (4).
S. aureus is capable of producing a myriad of virulence factors, allowing it to be a multidimensional pathogen. Sortase and covalently attached surface adhesin molecules confer colonization properties, cytolysins cause acute, localized keratinocyte toxicity and inflammation, and superantigens (SAgs) act locally and systemically to dysregulate the host immune response, thereby interfering with immunity (5).
Classically, SAgs function by cross-linking the variable part of the β-chain of the T-cell receptor (Vβ-TCR) and α and/or β chains of the major histocompatibility complex II (MHC II) molecules, leading to potent proinflammatory responses, sometimes termed cytokine storms (6). The nomenclature for staphylococcal SAgs indicates their primary disease associations. Staphylococcal enterotoxins (SEs) A to E and G cause emesis in humans and nonhuman primates. Toxic shock syndrome toxin 1 (TSST-1), differing in its primary amino acid sequence from other SAgs, is the cause of all cases of menstrual TSS (mTSS) and 50% of nonmenstrual cases. The remaining repertoire of SAgs related to SEs either lacks emetic activity or has not been tested, and thus they are labeled staphylococcal enterotoxin-like (SEl) molecules. The enterotoxin gene cluster (EGC) is composed of 6 superantigen genes, seg, sel-i, sel-m, sel-n, sel-o, and sel-u, that are increasingly recognized as important to staphylococcal disease (3), despite previously being considered a cluster or “nursery” of SAg genes of unknown function or potentially giving rise to new toxins through recombination (7).
Recently, SAgs have been shown to interact with and elicit proinflammatory responses from epithelial cells (8). This interaction leads to a local immunological response that can be followed by the systemic symptoms of TSS, through a mechanism known as outside-in signaling. Support for the idea of SAg roles in AD comes from a recent study characterizing the SAg profile of S. aureus isolated from AD patients who were resistant to steroid treatment, the most common anti-inflammatory therapy in AD, as well as from those who were not (9). Significant differences were seen in the numbers and types of SAgs encoded by the isolates infecting steroid-resistant patients compared to those encoded by isolates infecting steroid-sensitive patients, indicating that different S. aureus isolates were preferentially infecting those differing host environments.
As of 2003, the overall prevalence of AD in children was over 10% (10). Further investigation of host race depicts a significant difference in prevalence between African American (AA) and European American (EA) children, 15.9% and 9.7%, respectively (10). Multiple studies have attempted to correlate prevalences of AD as well as differences in disease severity with host race by examining differences in stratum corneum ceramide composition, transepithelial water loss (TEWL) (11), pH (12), filaggrin mutations (13), and nasal carriage of S. aureus. No one of these factors alone was responsible for variable AD presentation in AA versus EA patients, suggesting that other factors may be responsible for the observed differences. Interestingly, racial differences in immune activation have recently been identified in AD patients (14).
S. aureus can be found in 40 to 100% of AD lesions and at levels as high as 107 CFU/cm2 (15). Antibiotic use leads to reduction of lesions, demonstrating that S. aureus infection functions critically in disease progression and persistence (16). Many known host factors in AD vary by host race, and yet no studies to date have classified S. aureus strains infecting patients of different racial backgrounds.
Through the identification of the SAg profile of lesional AD isolates, we aimed to discern differences in S. aureus strains between the 2008 (9) and 2011–2014 time periods, as well as to differentiate the strains that infect EA, AA, and Mexican American (MA) AD patients.
RESULTS
Enterotoxin gene cluster (EGC) genes were carried more frequently in the 2011–2014 lesional AD isolates than in the 2008 AD isolates.
S. aureus was isolated from lesions of 103 AD patients from 2011 to 2014. Age, sex, eczema area and severity index (EASI) score, total serum IgE level, and eosinophil count for AD patients providing isolates from 2011 to 2014 are summarized by host race in Table 1. Of the 103 AD patients, 50 were EA, 27 AA, and 26 MA. Other than being from AD patients from diverse geographic locations in the United States, no additional demographics were available for the 100 patients who provided isolates in 2008. However, the diversity in SAg gene profiles in those isolates supports the evaluation that the strains tested were not from a clonal outbreak of AD.
TABLE 1 .
Demographic characteristics of patients with sample collection from 2011 to 2014a
| Parameter | Values |
||
|---|---|---|---|
| African Americans (n = 27) | European Americans (n = 50) | Mexican Americans (n = 26) | |
| Age (yrs) | 20 (8, 26) | 13 (9, 37) | 12 (6, 19) |
| Sex | |||
| Female | 17 (63) | 24 (48) | 11 (42) |
| Male | 10 (37) | 26 (52) | 15 (58) |
| Total serum IgE (kU/liter) | 946 (253, 2,358) | 1,175 (261, 5,457) | 955 (188, 2,721) |
| EASI score | 13 (8, 22) | 20 (7, 29) | 20 (8, 29) |
| Eosinophil count (cell count/mm3) | 422 (231, 625) | 445 (147, 706) | 420 (219, 690) |
All statistics are median (25th quartile, 75th quartile), except the sex data, which represent the number (percent) of patients.
For the 2011–2014 isolates, SAg genes associated with the EGC (sel-i, seg, sel-m, sel-n, and sel-o) were the most frequently represented SAg genes, with >50% of the isolates carrying one or more of the EGC genes (Table 2). sel-u is also carried by the EGC, but this SAg gene was not evaluated in the 2008 study and thus is not reported in the comparison in Table 2. However, among the 2011–2014 isolates (n = 46) that had all five of the other EGC genes, 100% also contained sel-u.
TABLE 2 .
Comparison of SAg prevalence levels over time
| SAg gene | No. (%) of strains positive for indicated gene |
P valuea | |
|---|---|---|---|
| 2008 AD (n = 100) | 2011–2014 AD (n = 103) | ||
| sea | 41 (41) | 7 (6.8) | <0.0001 |
| seb | 35 (35) | 6 (5.8) | <0.0001 |
| sec | 25 (25) | 11 (11) | 0.009 |
| sed | 39 (39) | 16 (16) | 0.0002 |
| see | 39 (39) | 0 (0) | <0.0001 |
| seg | 55 (55) | 70 (68) | 0.06 |
| sel-h | 43 (43) | 2 (1.9) | <0.0001 |
| sel-i | 48 (48) | 59 (57) | 0.20 |
| sel-j | 69 (69) | 13 (13) | <0.0001 |
| sel-k | 49 (49) | 16 (16) | <0.0001 |
| sel-l | 29 (29) | 5 (4.9) | <0.0001 |
| sel-m | 64 (64) | 59 (57) | 0.39 |
| sel-n | 51 (51) | 71 (69) | 0.009 |
| sel-o | 37 (37) | 55 (53) | 0.02 |
| sel-q | 40 (40) | 12 (12) | <0.0001 |
| tstH | 38 (38) | 10 (9.7) | <0.0001 |
P values are based on comparisons of the prevalence levels of each SAg between the 2008 AD cohort and the 2011-to-2014 AD cohort.
A comparison of the representation of 16 SAg genes in 103 AD isolates from 2011 to 2014 to those in 100 AD isolates previously studied in 2008 (9) revealed a significant shift in the prevalence of selected SAg genes. Notably, SAg genes associated with the EGC (sel-n and sel-o) were significantly (P < 0.05) more prevalent in isolates from 2011 to 2014 than in those from 2008. In contrast, a significant (P < 0.05) reduction in the prevalences of tstH (the gene for TSST-1), sel-q, sed, sel-j, and sea was observed in the 2011–2014 isolates compared to the 2008 isolates (Table 2).
SAg profiles of 2011–2014 AD isolates describe three genotypic groups.
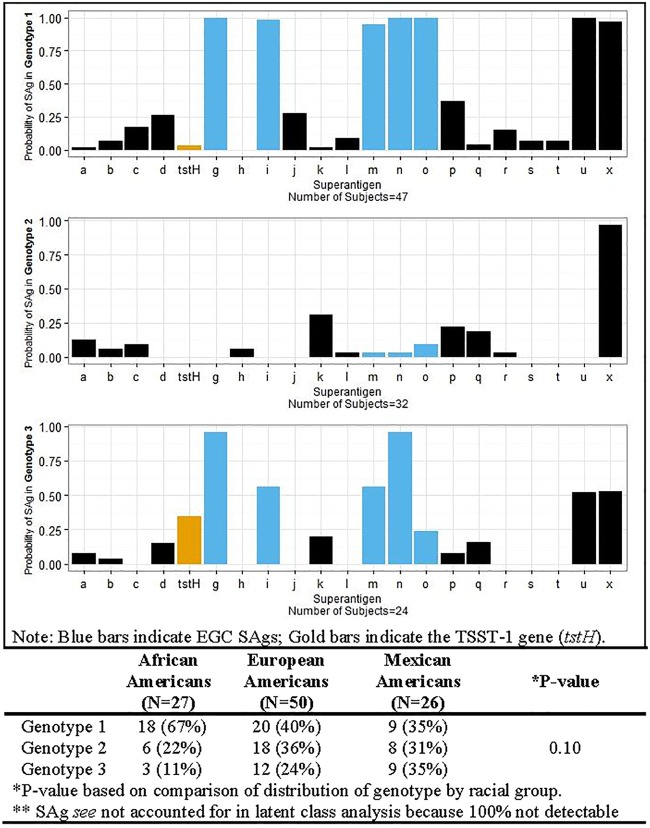
S. aureus strains are commonly clonal grouped by overall chromosome arrangement, using, for example, pulsed-field gel electrophoresis. Alternatively, through the use of a latent class analysis, patients from 2011 to 2014 with similar SAg profiles were grouped into three major genotypes using 22 SAgs (Fig. 1). The basis for this analysis is that such studies allow groupings based on the virulence factors present versus chromosomal DNA patterns that may or may not reflect virulence trait differences. Genotype 1 included patients with strains that carried the EGC SAgs (seg, sel-i, sel-m, sel-n, sel-o, and sel-u) and sel-x ≥97% of the time. Genotype 1 also had a higher probability of carrying sel-p (enterotoxin-like P) (37%), sel-j (28%), sed (26%), sec (17%), sel-r (15%), sel-l (9%), sel-s (7%), and sel-t (7%) than the other two genotypes. Similarly to genotype 1, genotype 2 had a high probability of carrying sel-x (≥97%). Genotype 2 appears to be largely defined by only containing sel-x, suggesting that this group contains high numbers of USA300s (17) based on SAg profiles. Genotype 2 also had a ≥13% probability of carrying sel-k, sel-p, sel-q, and sea (Fig. 1). Genotype 3 had the highest (35%) probability of carrying tstH and had a ≥50% probability of encoding the majority of EGC SAgs and carrying sel-x (Fig. 1).
FIG 1 .
Probability of superantigen for a given S. aureus genotype. The table component of the figure displays the probability of each S. aureus genotype within each racial group.
SAg genotypes suggest differences as a function of host race.
Examination of the association between racial groups and S. aureus SAg profiles demonstrated that among AA isolates, 67% were in genotype 1, whereas EA and MA isolates were relatively evenly distributed across all three genotype groups (Fig. 1). Among AA isolates, 89% were in genotypes 1 and 2, which were those most notably lacking tstH. A comparison of the distributions of genotypes by race indicated no significant statistical differences, however.
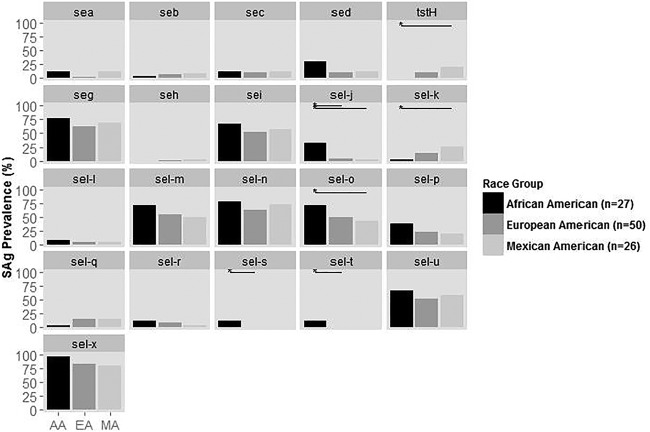
Pairwise comparison of individual SAg genes by host race indicates some SAg differences.
Using the isolates collected from 2011 to 2014, a comparison of the prevalences of each SAg gene among racial groups demonstrates some significant differences (Fig. 2). There were no significant differences in the prevalences of any of the 21 SAg genes between EA and MA isolates (Fig. 2). Significant differences in the prevalences of 3 of 21 and 4 of 21 SAg genes were observed between EA and AA isolates and MA and AA isolates, respectively. MA isolates had significantly higher prevalences of tstH and sel-k and significantly lower prevalences of sel-o compared to AA isolates. EA and MA isolates lacked sel-s and sel-t, with AA isolates being the only strains containing these genes. AA isolates also more frequently carried sel-j and genes comprising the EGC than EA and MA isolates.
FIG 2 .
Prevalence of superantigen (SAg) genes in S. aureus isolates from 2011 to 2014 within each racial group. Horizontal lines indicate comparisons that are statistically significant at the 0.05 level.
EASI scores and eosinophil counts show an association with tstH and sel-p, respectively, but not host race.
There was no significant difference in EASI scores, total serum IgE levels, or eosinophil counts among the racial groups (data not shown). On the SAg gene level, isolates carrying tstH had a lower EASI score than isolates lacking the gene (mean difference, −9.3; 95% confidence interval [CI], −18.5, −0.2; P = 0.05) (Table 3, EASI score data). Isolates containing sel-p had significantly higher eosinophil counts than isolates lacking this gene (GMR, 1.6; 95% CI, 0.03, 2.4; P = 0.04) (Table 3, eosinophil count data).
TABLE 3 .
Adjusted mean differences in disease severity or geometric mean ratio in biomarkers (total serum IgE and eosinophils) between isolates with the given SAg gene and isolates without the given SAg genea
| SAg | EASI score |
Total serum IgE (kU/liter) |
Eosinophil count (cells/mm3) |
|||
|---|---|---|---|---|---|---|
| Mean difference (95% CI) | P value | GMR (95% CI) | P value | GMR (95% CI) | P value | |
| sea | −5.3 (−16.2, 5.7) | 0.34 | 0.85 (0.18, 4.0) | 0.83 | 0.70 (0.33, 1.5) | 0.35 |
| seb | 6.4 (−5.5, 18.2) | 0.29 | 0.57 (0.11, 3.0) | 0.50 | 0.94 (0.42, 2.1) | 0.89 |
| sec | 1.3 (−7.7, 10.3) | 0.77 | 0.46 (0.13, 1.6) | 0.22 | 0.90 (0.49, 1.7) | 0.73 |
| sed | 1.7 (−6.0, 9.3) | 0.67 | 2.3 (0.81, 6.8) | 0.12 | 0.95 (0.56, 1.6) | 0.84 |
| tstH | −9.3 (−18.5, −0.2) | 0.05* | 0.74 (0.2, 2.8) | 0.66 | 0.67 (0.36, 1.3) | 0.21 |
| seg | 0.21 (−5.8, 6.3) | 0.95 | 0.98 (0.42, 2.3) | 0.97 | 0.76 (0.50, 1.1) | 0.17 |
| sel-h | −10.5 (−30.4, 5.3) | 0.30 | 2.9 (0.18, 48.0) | 0.45 | 1.2 (0.29, 4.4) | 0.87 |
| sel-i | 1.5 (−4.2, 7.2) | 0.60 | 0.88 (0.39, 2.0) | 0.75 | 0.78 (0.53, 1.1) | 0.19 |
| sel-j | 6.5 (−1.8, 14.8) | 0.12 | 2.8 (0.84, 9.4) | 0.09 | 1.2 (0.62, 2.0) | 0.71 |
| sel-k | −2.6 (−10.5, 5.3) | 0.51 | 1.7 (0.58, 5.3) | 0.32 | 1.5 (0.86, 2.5) | 0.15 |
| sel-l | −4.6 (−17.5, 8.2) | 0.48 | 0.87 (0.14, 5.3) | 0.88 | 0.71 (0.30, 1.7) | 0.44 |
| sel-m | 2.6 (−3.0, 8.3) | 0.36 | 1.2 (0.56, 2.8) | 0.59 | 1.1 (0.72, 1.6) | 0.75 |
| sel-n | 1.5 (−4.6, 7.6) | 0.63 | 1.3 (0.56, 3.1) | 0.54 | 0.87 (0.58, 1.3) | 0.51 |
| sel-o | 3.4 (−2.1, 9.0) | 0.22 | 1.6 (0.73, 3.5) | 0.24 | 1.1 (0.72, 1.6) | 0.75 |
| sel-p | 1.2 (−5.2, 7.6) | 0.71 | 2.3 (0.93, 5.5) | 0.07 | 1.6 (1.03, 2.4) | 0.04* |
| sel-q | −0.60 (−9.5, 8.3) | 0.89 | 1.4 (0.39, 4.7) | 0.62 | 1.5 (0.82, 2.7) | 0.18 |
| sel-r | 7.2 (−3.1, 17.5) | 0.17 | 2.6 (0.62, 11.2) | 0.19 | 1.79 (0.87, 3.5) | 0.12 |
| sel-s | 10.9 (−5.7, 27.5) | 0.19 | 1.7 (0.1, 30.0) | 0.70 | 0.32 (0.08, 1.3) | 0.10 |
| sel-t | 10.9 (−5.7, 27.5) | 0.19 | 1.7 (0.1, 30.0) | 0.70 | 0.32 (0.08, 1.3) | 0.10 |
| sel-u | 1.3 (−4.3, 7.0) | 0.64 | 0.94 (0.42, 2.1) | 0.89 | 0.77 (0.52, 1.1) | 0.17 |
| sel-x | 5.7 (−2.3, 13.7) | 0.16 | 2.1 (0.7, 6.4) | 0.20 | 1.3 (0.76, 2.3) | 0.33 |
All models adjusted for age at enrollment and sex. Statistically significant values are bolded and denoted with an asterisk (*). EASI, eczema area and severity index; GMR, geometric mean ratio.
S. aureus from menstrual TSS isolates encoded TSST-1, but none of these were obtained from AA patients.
AA AD isolates of S. aureus lacked the tstH gene (Fig. 2). The Schlievert laboratory identified TSST-1 in 1981 (18) and has collected menstrual TSS isolates continually since then. Retrospective investigation of >6,000 menstrual TSS isolates revealed that no TSS isolate was from an AA patient.
DISCUSSION
Treatment of the chronic inflammatory skin disease AD is costly; upward of a billion dollars per year in health care costs goes into managing symptoms associated with the disease. Further complexity in treatment stems from the fact that patients from different racial backgrounds respond differently to treatments (19). These differences are not associated with previously identified host barrier defects such as stratum corneum ceramide composition, TEWL, skin pH, or S. aureus nasal carriage (13, 20–23).
This study was undertaken to examine a possible temporal shift in SAg profiles over the past 3 to 6 years and to classify S. aureus isolates from AD patients from different racial backgrounds on the basis of virulence factor profile. The myriad of virulence factors encoded by S. aureus give it the ability to evade host immune elimination and additionally provide niche selection for colonization and infection. For example, patients who develop menstrual TSS do not develop immunity to their infecting S. aureus strain due to lack of protective response in the presence of TSST-1, and they remain susceptible to lifelong recurrences (24).
Analyses of AD isolates from 2011 to 2014 have shown a significantly higher prevalence of genes encoding EGC SAgs and a significantly lower prevalence of tstH, sel-q, and sea than analyses of AD isolates from 2008. We expected a shift in SAg profile over this time period, and our results engender particular concern with the emergence of the EGC. The EGC is a cluster of 6 SAgs and is intact in 2011–2014 isolates; this cluster was occasionally present in 2008, but in many strains collected in 2008 the cluster was broken up such that few strains carried all 6 EGC members. Results presented in this study suggest that in-depth patient information is important in analyzing the toxigenic potential of S. aureus isolates and that a lack of such information limits the utility of results obtained in comparing two pools of isolates. However, our data suggest that the toxigenic potential of strains changes over time and that such changes warrant further study. For example, important shifts in clonal groups have been correlated with the emergence of mTSS.
This shift to greater numbers of encoded EGC SAgs predicts that those SAgs should be more prevalent in disease isolates today. This is clearly the case for AD patients. However, significantly more S. aureus isolates from infective endocarditis, pneumonia, and bloodstream infections are also carrying the intact EGC. We have shown that SAgs contribute to development of AD and that SAgs are required for infective endocarditis, pneumonia, and bloodstream infections due to S. aureus (25–27). Furthermore, we have recently shown in a sensitive rabbit model (28) that EGC SAgs contribute to both pneumonia and infective endocarditis (3). It is noteworthy that the majority of infective endocarditis strains encode the EGC and that S. aureus has simultaneously become the leading cause of native valve infective endocarditis (29).
It is possible that the increased prevalence of the EGC results from development of immunity against a once-prevalent toxin, i.e., TSST-1. This would confer a positive selection of strains lacking this toxin, allowing them to become more prevalent. It is known that different S. aureus strains cycle through the human population in roughly 10-year intervals, and the changes seen in SAg genes may be a reflection of the cycling. For example, the 80/81 clonal group of S. aureus emerged in hospitals in about 1950, peaking to cause 85% of hospital infections in 1955 and disappearing by 1960. This clonal group was replaced in 1960 by the 52/52-A clonal group, which peaked in hospitals in 1965 and disappeared by 1970. Finally, this clonal group was replaced by clonal group USA200 (also known as 29/52), which produces TSST-1. The last-named clonal group also accounted for the emergence of TSST-1 in 1972 and for that seen in association with high-absorbency tampons in 1975 (30). Today, the incidence of menstrual TSS, which is caused by TSST-1 at a rate of nearly 100%, is lower than it was in the early 1980s, when the USA200 strain was emerging (31, 32).
Further analyses of the 2011–2014 isolates of AD showed that the isolates can be divided into three genotype groups, depending on their SAg profiles. We believe that these genotype groupings provide an emergent, important tool for epidemiological analysis of S. aureus associated with diseases. To date, the majority of clonal groupings of S. aureus have depended on chromosomal DNA analyses, for example, pulsed-field gel electrophoresis. This new genotype method studies the actual virulence factors required for human diseases. Genotype group 1 was characterized by carrying the EGC and SEl-X. Genotype group 3 has the highest probability of encoding TSST-1, among other SAgs. It is expected that genotype group 1 will continue to emerge epidemiologically and to be associated with a myriad of significant human diseases due to the presence of the EGC. Genotype group 3 strains would be expected to cause menstrual and nonmenstrual TSS due to the presence of the TSST-1 gene and should be associated with infective endocarditis, as has been seen, due to the presence in many strains of the EGC.
Examining genotype grouping based on host race revealed that ~90% of AA isolates were in genotype groups 1 and 2, which lacked the gene for TSST-1. The three genotype groups were relatively evenly distributed across MA and EA isolates. A trend in the prevalence among genotype groups based on host race may suggest that SAgs confer colonization or infection benefits that are dependent in part on host race. In contrast, host factors are likely to exert selective pressures against S. aureus producing TSST-1. Our observations of the lack of TSST-1-producing S. aureus strains in AAs merit further investigation, particularly of genetic differences among the host races that could explain these findings.
The total EASI scores are not significantly different across AAs, EAs, and MAs. However, patients colonized with strains containing tstH had a significant decrease in EASI score compared to patients colonized with isolates lacking this gene. Results from patients colonized with strains containing sel-p were significantly associated with increased eosinophil counts compared to those from patients colonized with isolates lacking this gene. Other SAg results approached statistical significance in correlation to increased EASI, IgE, or eosinophil counts. These data collectively suggest that the capacity of an infecting S. aureus strain to produce certain SAgs may contribute to disease severity (Table 3).
In sum, this study was the first of its kind to analyze the complete S. aureus SAg profile of AD patients across time and by racial background. Our data indicate that the EGC continues to emerge as the dominant SAg group, associated with many kinds of S. aureus infections, including AD. Our data presented here also suggest the S. aureus strains infecting AAs, EAs, and MAs have significant differences (Fig. 2). This may lead to differences in the prevalence and severity of diseases. The development of the SAg genotype method for clonal grouping is in its infancy, but we have already shown epidemiologically that the method can be used to analyze SAg distribution and associations. We expect its use to increase significantly, as it is increasingly recognized that SAgs contribute importantly to all or nearly all S. aureus infections.
MATERIALS AND METHODS
2011–2014 patient enrollment and data collection.
Patients (n = 103) with AD were enrolled at six centers across the United States as part of the Atopic Dermatitis Research Network (ADRN) Registry study (ClinicalTrials.gov NCT01494142). Patients were administered a standardized set of questionnaires and underwent a physical examination (performed by a qualified medical professional) as well as blood and skin swab collection. The questionnaires, exam, and samples were used to evaluate their overall medical history and disease status. AD severity was assessed using the standardized eczema area and severity index (EASI) grading score, a sensitive clinical measure of the presentation and spread of inflamed skin at a single point in time. A higher EASI score (score range 0 to 72) equates to more-severe and extensive skin involvement. A complete blood count (CBC) with differential was performed on blood samples at Quest Diagnostics Laboratory. Total serum IgE (kU/liter) was measured by ImmunoCAP tests (Thermo Fisher Scientific) at the Johns Hopkins Asthma and Allergy Center (JHAAC). Patients were asked to self-identify their race and ethnicity from a list of 2010 United States Census categories. Patient age was calculated from self-reported date of birth to the date of study enrollment.
Bacterial strains and PCR identification of SAgs.
Bacterial strains from 2011 to 2014 (n = 103) were isolated from swabs of lesional AD skin and were grown overnight in 25-ml Todd Hewitt broth cultures at 37°C and 200 revolutions/min. DNA samples from all 103 isolates from 2011 to 2014 were prepared using a Qiagen DNeasy blood and tissue kit. PCRs were carried out with Taq polymerase (Qiagen) along with known positive controls for all 22 known SAgs by using primers previously utilized (33). Positive DNA controls for PCR screening were obtained from laboratory strains maintained in a lyophilized state in the laboratory.
The data from a prior AD study published in 2008 were used for comparison to more recent isolates. Those prior isolates were lesional isolates from a general population of AD patients obtained in 2002 from diverse geographic locations. Since the prior 2008 AD study (9), six new SAgs have been described which were not assessed in the 2008 study. Therefore, analyses examining SAg profiles over time include only the 16 SAgs which were analyzed in common.
The S. aureus strains used in this study are maintained by and available as low-passage-number stocks through the NIH-funded Atopic Dermatitis Research Network (ADRN). The ADRN steering committee receives requests and approves release of samples to researchers, with authors Patrick M. Schlievert and Gloria David as contact individuals.
Statistical methods.
Within each racial group, age data, total serum IgE levels, EASI scores, and eosinophil counts were summarized by medians and quartiles and sex was summarized using frequencies and percentages. Fisher’s exact tests were used to compare the prevalences of all SAgs between the 2011–2014 cohort and the 2008 cohort. A latent class analysis, performed via the poLCA package in R, was used to cluster isolates into SAg classes (or genotypes). The number of potential classes, ranging from 2 to 5, was examined using 500 iterations performed in each algorithm run. For each set of classes, the distribution of the model fit, measured by the Bayesian information criterion, was examined across each run. Three classes showed the least variability and best model fit across all runs. The prevalences of all SAgs were compared between racial groups using an unadjusted logistic regression model. Exact logistic regression was used to account for a low SAg prevalence of tstH, sel-q, sel-s, and sel-t. Multivariable generalized linear models adjusting for age and sex were used to compare individual outcomes of EASI scores, total serum IgE levels, and eosinophil counts between racial groups or between isolates with or without each SAg. No adjustments were made for multiple comparisons. All analyses were conducted using R software (version 3 to 2.2).
ACKNOWLEDGMENTS
This research was supported by the Atopic Dermatitis Research Network (ADRN) through U19 AI117673, UM2AI117870, HHSN272201000020C, and HHSN272201000017C, from NIAID, as well as by the NIH/National Center for Advancing Translational Sciences, Colorado Clinical and Translational Institute, grant UL1 TR001082, and the Edelstein Family Chair for Pediatric Allergy-Immunology at National Jewish Health.
REFERENCES
- 1.Suárez-Fariñas M, Ungar B, Correa da Rosa JC, Ewald DA, Rozenblit M, Gonzalez J, Xu H, Zheng XZ, Peng XY, Estrada YD, Dillon SR, Krueger JG, Guttman-Yassky E. 2015. RNA sequencing atopic dermatitis transcriptome profiling provides insights into novel disease mechanisms with potential therapeutic implications. J Allergy Clin Immunol 135:1218–1227. doi: 10.1016/j.jaci.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Leung DYM, Guttman-Yassky E. 2014. Deciphering the complexities of atopic dermatitis: shifting paradigms in treatment approaches. J Allergy Clin Immunol 134:769–779. doi: 10.1016/j.jaci.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stach CS, Vu BG, Merriman JA, Herrera A, Cahill MP, Schlievert PM, Salgado-Pabón W. 2016. Novel tissue level effects of the Staphylococcus aureus enterotoxin gene cluster are essential for infective endocarditis. PLoS One 11:e0154762. doi: 10.1371/journal.pone.0154762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gao L, Bin L, Rafaels NM, Huang L, Potee J, Ruczinski I, Beaty TH, Paller AS, Schneider LC, Gallo R, Hanifin JM, Beck LA, Geha RS, Mathias RA, Barnes KC, Leung DY. 2015. Targeted deep sequencing identifies rare loss-of-function variants in IFNGR1 for risk of atopic dermatitis complicated by eczema herpeticum. J Allergy Clin Immunol 136:1591–1600. doi: 10.1016/j.jaci.2015.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spaulding AR, Salgado-Pabón W, Kohler PL, Horswill AR, Leung DY, Schlievert PM. 2013. Staphylococcal and streptococcal superantigen exotoxins. Clin Microbiol Rev 26:422–447. doi: 10.1128/CMR.00104-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marrack P, Kappler J. 1990. The staphylococcal enterotoxins and their relatives. Science 248:705–711. doi: 10.1126/science.2185544. [DOI] [PubMed] [Google Scholar]
- 7.Jarraud S, Peyrat MA, Lim A, Tristan A, Bes M, Mougel C, Etienne J, Vandenesch F, Bonneville M, Lina G. 2001. egc, a highly prevalent operon of enterotoxin gene, forms a putative nursery of superantigens in Staphylococcus aureus. J Immunol 166:669–677. doi: 10.4049/jimmunol.166.1.669. [DOI] [PubMed] [Google Scholar]
- 8.Peterson ML, Ault K, Kremer MJ, Klingelhutz AJ, Davis CC, Squier CA, Schlievert PM. 2005. Innate immune system is activated by stimulation of vaginal epithelial cells with Staphylococcus aureus and toxic shock syndrome toxin 1. Infect Immun 73:2164–2174. doi: 10.1128/IAI.73.4.2164-2174.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schlievert PM, Case LC, Strandberg KL, Abrams BB, Leung DY. 2008. Superantigen profile of Staphylococcus aureus isolates from patients with steroid-resistant atopic dermatitis. Clin Infect Dis 46:1562–1567. doi: 10.1086/586746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaw TE, Currie GP, Koudelka CW, Simpson EL. 2011. Eczema prevalence in the United States: data from the 2003 National Survey of Children’s Health. J Invest Dermatol 131:67–73. doi: 10.1038/jid.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta J, Grube E, Ericksen MB, Stevenson MD, Lucky AW, Sheth AP, Assa’ad AH, Khurana Hershey GK. 2008. Intrinsically defective skin barrier function in children with atopic dermatitis correlates with disease severity. J Allergy Clin Immunol 121:725–730.e2. doi: 10.1016/j.jaci.2007.12.1161. [DOI] [PubMed] [Google Scholar]
- 12.Bandier J, Johansen JD, Petersen LJ, Carlsen BC. 2014. Skin pH, atopic dermatitis, and filaggrin mutations. Dermatitis 25:127–129. doi: 10.1097/DER.0000000000000045. [DOI] [PubMed] [Google Scholar]
- 13.Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, Lee SP, Goudie DR, Sandilands A, Campbell LE, Smith FJ, O’Regan GM, Watson RM, Cecil JE, Bale SJ, Compton JG, DiGiovanna JJ, Fleckman P, Lewis-Jones S, Arseculeratne G, Sergeant A, Munro CS, El Houate B, McElreavey K, Halkjaer LB, Bisgaard H, Mukhopadhyay S, McLean WH. 2006. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet 38:441–446. doi: 10.1038/ng1767. [DOI] [PubMed] [Google Scholar]
- 14.Noda S, Suárez-Fariñas M, Ungar B, Kim SJ, de Guzman Strong C, Xu H, Peng X, Estrada YD, Nakajima S, Honda T, Shin JU, Lee H, Krueger JG, Lee KH, Kabashima K, Guttman-Yassky E. 2015. The Asian atopic dermatitis phenotype combines features of atopic dermatitis and psoriasis with increased TH17 polarization. J Allergy Clin Immunol 136:1254–1264. doi: 10.1016/j.jaci.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 15.Leyden JJ, Marples RR, Kligman AM. 1974. Staphylococcus aureus in the lesions of atopic dermatitis. Br J Dermatol 90:525–530. doi: 10.1111/j.1365-2133.1974.tb06447.x. [DOI] [PubMed] [Google Scholar]
- 16.Breuer K, HAussler S, Kapp A, Werfel T. 2002. Staphylococcus aureus: colonizing features and influence of an antibacterial treatment in adults with atopic dermatitis. Br J Dermatol 147:55–61. doi: 10.1046/j.1365-2133.2002.04872.x. [DOI] [PubMed] [Google Scholar]
- 17.King JM, Kulhankova K, Stach CS, Vu BG, Salgado-Pabon W. 2016. Phenotypes and virulence among Staphylococcus aureus USA100, USA200, USA300, USA400, and USA600 clonal lineages. mSphere 1:e00071-16. doi: 10.1128/mSphere.00071-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schlievert PM, Shands KN, Dan BB, Schmid GP, Nishimura RD. 1981. Identification and characterization of an exotoxin from Staphylococcus aureus associated with toxic-shock syndrome. J Infect Dis 143:509–516. doi: 10.1093/infdis/143.4.509. [DOI] [PubMed] [Google Scholar]
- 19.Vachiramon V, Tey HL, Thompson AE, Yosipovitch G. 2012. Atopic dermatitis in African American children: addressing unmet needs of a common disease. Pediatr Dermatol 29:395–402. doi: 10.1111/j.1525-1470.2012.01740.x. [DOI] [PubMed] [Google Scholar]
- 20.Berardesca E, Maibach HI. 1988. Racial differences in sodium lauryl sulphate induced cutaneous irritation: black and white. Contact Dermatitis 18:65–70. doi: 10.1111/j.1600-0536.1988.tb02741.x. [DOI] [PubMed] [Google Scholar]
- 21.Jungersted JM, Høgh JK, Hellgren LI, Jemec GB, Agner T. 2010. Ethnicity and stratum corneum ceramides. Br J Dermatol 163:1169–1173. doi: 10.1111/j.1365-2133.2010.10080.x. [DOI] [PubMed] [Google Scholar]
- 22.Rippke F, Schreiner V, Doering T, Maibach HI. 2004. Stratum corneum pH in atopic dermatitis: impact on skin barrier function and colonization with Staphylococcus aureus. Am J Clin Dermatol 5:217–223. doi: 10.2165/00128071-200405040-00002. [DOI] [PubMed] [Google Scholar]
- 23.Kuehnert MJ, Kruszon-Moran D, Hill HA, McQuillan G, McAllister SK, Fosheim G, McDougal LK, Chaitram J, Jensen B, Fridkin SK, Killgore G, Tenover FC. 2006. Prevalence of Staphylococcus aureus nasal colonization in the United States, 2001–2002. J Infect Dis 193:172–179. doi: 10.1086/499632. [DOI] [PubMed] [Google Scholar]
- 24.Osterholm MT, Davis JP, Gibson RW, Mandel JS, Wintermeyer LA, Helms CM, Forfang JC, Rondeau J, Vergeront JM. 1982. Tri-state toxic-state syndrome study. I. Epidemiologic findings. J Infect Dis 145:431–440. doi: 10.1093/infdis/145.4.431. [DOI] [PubMed] [Google Scholar]
- 25.Salgado-Pabón W, Breshears L, Spaulding AR, Merriman JA, Stach CS, Horswill AR, Peterson ML, Schlievert PM. 2013. Superantigens are critical for Staphylococcus aureus infective endocarditis, sepsis, and acute kidney injury. mBio 4:e00494-13. doi: 10.1128/mBio.00494-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pragman AA, Yarwood JM, Tripp TJ, Schlievert PM. 2004. Characterization of virulence factor regulation by SrrAB, a two-component system in Staphylococcus aureus. J Bacteriol 186:2430–2438. doi: 10.1128/JB.186.8.2430-2438.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spaulding AR, Salgado-Pabón W, Merriman JA, Stach CS, Ji Y, Gillman AN, Peterson ML, Schlievert PM. 2014. Vaccination against Staphylococcus aureus pneumonia. J Infect Dis 209:1955–1962. doi: 10.1093/infdis/jit823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salgado-Pabón W, Schlievert PM. 2014. Models matter: the search for an effective Staphylococcus aureus vaccine. Nat Rev Microbiol 12:585–591. doi: 10.1038/nrmicro3308. [DOI] [PubMed] [Google Scholar]
- 29.Nienaber JJ, Sharma Kuinkel BK, Clarke-Pearson M, Lamlertthon S, Park L, Rude TH, Barriere S, Woods CW, Chu VH, Marín M, Bukovski S, Garcia P, Corey GR, Korman T, Doco-Lecompte T, Murdoch DR, Reller LB, Fowler VG Jr, International Collaboration on Endocarditis-Microbiology Investigators . 2011. Methicillin-susceptible Staphylococcus aureus endocarditis isolates are associated with clonal complex 30 genotype and a distinct repertoire of enterotoxins and adhesins. J Infect Dis 204:704–713. doi: 10.1093/infdis/jir389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Altemeier WA, Lewis SA, Bjornson HS, Staneck JL, Schlievert PM. 1983. Staphylococcus in toxic shock syndrome and other surgical infections. Development of new bacteriophages. Arch Surg 118:281–284. doi: 10.1001/archsurg.1983.01390030013002. [DOI] [PubMed] [Google Scholar]
- 31.DeVries AS, Lesher L, Schlievert PM, Rogers T, Villaume LG, Danila R, Lynfield R. 2011. Staphylococcal toxic shock syndrome 2000–2006: epidemiology, clinical features, and molecular characteristics. PLoS One 6:e22997. doi: 10.1371/journal.pone.0022997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schlievert PM, Tripp TJ, Peterson ML. 2004. Reemergence of staphylococcal toxic shock syndrome in Minneapolis-St. Paul, Minnesota, during the 2000–2003 surveillance period. J Clin Microbiol 42:2875–2876. doi: 10.1128/JCM.42.6.2875-2876.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vu BG, Stach CS, Salgado-Pabón W, Diekema DJ, Gardner SE, Schlievert PM. 2014. Superantigens of Staphylococcus aureus from patients with diabetic foot ulcers. J Infect Dis 210:1920–1927. doi: 10.1093/infdis/jiu350. [DOI] [PMC free article] [PubMed] [Google Scholar]