Abstract
Cardio-vascular diseases are the leading cause of morbidity and mortality. Ischemia is a state of oxygen deprivation in tissues, whereas reperfusion is restoration of blood flow in ischemic tissues. Myocardial damage of tissue during reperfusion after ischemic insult is known as myocardial ischemia–reperfusion (I/R) injury. It induces damage to cardiac muscle via increasing expression of oxygen, sodium and calcium ions which are responsible in the activation of proteases and cell death. Heart renin angiotensin system (RAS) plays an important role in the myocardial ischemia and reperfusion injury. Angiotensin (1–7) is responsible for vasodilation and angiotensin II for vasoconstriction. Here-in we reviewed how myocardial I/R injury sets in by up-regulation of angiotensin II that leads to increased infarct size, which can be reduced by the use of ACE inhibitors, ACE2 activators and angiotensin II antagonist.
Keywords: Myocardial ischemia–reperfusion injury, Ischemia preconditioning, ACE inhibitor, ACE2 activator, Angiotensin II antagonist
1. Introduction
Cardiovascular disease (CVD) or blood vessel disease, is the leading cause of death worldwide.1 Ischaemic heart disease (IHD) causes damage to heart muscle via deposition of cholesterol plaques on the wall of coronary arteries and reducing the availability of nutrients like glucose.2, 3 Ischemia is defined as an insufficient supply of the nutrient and oxygen to the cardiac muscle. During ischemia, the level of glutathione, phosphocreatine and ATP are reduced while hypoxanthine level gets elevated. Altered ion distribution, i.e. increase in intracellular Ca2+/Na2+, cellular swelling, cytoskeleton disorganization and acidosis of cells occur.4 During reperfusion injury, blood flow supply returns to the cardiac muscle that causes release and activation of intracellular Ca2+ channel, formation of cellular edema and damage to lipid membrane.5, 6
The renin–angiotensin system (RAS) which is composed of renin, angiotensin converting enzyme (ACE), angiotensin I and angiotensin II, is localized in different areas of heart such as atria, conduction system, valves, coronary vessels, ventricles, fibroblasts and myocytes.7, 8 ACE 2 system is found in venous endothelial cells, arterial smooth muscle cells, cardiac myocytes, myofibroblasts, thoracic aorta, carotid arteries and veins.9, 10, 11 Myocardial angiotensin receptors were discovered in 1980s. These receptors are the supporter of local renin angiotensin system and intracardiac renin angiotensin system. They play a very crucial role in cardioprotection. Major effector peptide in renin angiotensin system is angiotensin II (vasoconstrictor), whose excess production increase the blood pressure and leads to the damage of various organs like brain, kidney and blood vessels.12 Angiotensin II antagonist and angiotensin converting enzyme inhibitors (captopril and enalapril) have cardioprotective effect by reducing the blood pressure and infarct size.13, 14
Cardiac angiotensinogen are glycoprotein of α2-globulin class, synthesized in the cardiac muscle. Gene expression of angiotensinogen has been found in the mice and rats. Lower concentration of angiotensinogen is found in the ventricles as compared to heart atria. It has been reported that cardiac angiotensinogen mRNA level in rat and mice liver is approximately 5% and 1%. Glucocorticoid hormone treatment increases the production of hepatic angiotensinogen in the rat heart. Dzau in 1987 observed that dietary sodium raises the level of mRNA angiotensinogen in rat tissue, which could be suppressed after ACE inhibitor treatment.15, 16, 17
Cardiac renin is a proteolytic enzyme which was discovered in 1898, by Robert Tigerstedt in Sweden. It has been documented that there is an increased gene expression of renin in both mice and rat heart. An estimated 2% mRNA level is found in rat kidney and the submaxillary gland of mice.18, 19, 20
Cardiac angiotensins are hormonal peptides, formed by the proteolytic reaction of angiotensinogen and renin. Angiotensins are of two types, angiotensin I and angiotensin II. Angiotensin I have no biological role on heart renin angiotensin system. They are precursor of angiotensin II and angiotensin III.21, 22 Angiotensin II is an effector hormone which plays a major role in heart renin angiotensin system. It leads to hypertension by increasing vasoconstriction and retention of fluid and sodium in the body.23 Angiotensin II is also responsible for stimulation of inflammatory mediators such as NAD(P)H oxidase, phospholipase A2 and JAK/STAT pathway. De Leeuw in 1999 reported that angiotensin converting enzymes treatment decreases angiotensin II level.24, 25
Cardiac ACE are metallopeptides which are commonly distributed on epithelial and endothelial cells surface. ACE inhibitors have been reported to exhibit protective effect on cardiovascular disease.26 They are involved in the treatment for hypertension, myocardial infarction and congestive heart failure (CHF) as they inhibit angiotensin II formation.27 Angiotensin converting enzyme 2 is an exopeptidase with zinc membrane which help in the conversion of angiotensin I and angiotensin II to angiotensin 1–9 and angiotensin 1–7. Angiotensin 1–7 is a vasodilator that further converts into angiotensin 1–5 via ACE.28, 29, 30
2. Myocardial ischemia/reperfusion injury
Myocardial ischemia/reperfusion injury was first discovered by Jennings et al. in 1960. It develops when coronary blood supply to myocardium is reduced. Restoration of blood flow to ischemic heart is necessary for maintaining heart physiology.31, 32 The non-lethal episodes of ischemia and reperfusion prior to global myocardial ischemic insult have proved to reduce myocardial injury, which is termed as preconditioning. Reperfusion can elicit a cascade of adverse events that paradoxically causes injury of tissue.33 During reperfusion after ischemic stress, hypoxanthine is oxidized by xanthine oxidase which produces reactive oxygen species (ROS).34 Ischemia followed by reperfusion is a stronger cause of apoptosis than sustained ischemic insult. Ischemia due to an anaerobic metabolism causes catabolism of adenine nucleotide and leads to depletion of adenosine triphosphate (ATP).35 At the time of reperfusion, xanthine oxidase metabolizes the hypoxanthine to xanthine and forms uric acid that leads to the formation of huge amount of reactive oxygen species, i.e. superoxide anion (O2−), hydrogen peroxide (H2O2) and hydrogen radical (OH−).36 Myocardial IR injury usually causes inflammation on the cardiac muscle and leads to hypoxia. This phenomena damages tissues by activating leukocytes, cytokines, reactive oxygen species and frequently develops during heart transplantation, infarction and sepsis.37, 38
3. Purpose of inflammatory cascade in myocardial ischemia/reperfusion (I–R) injury
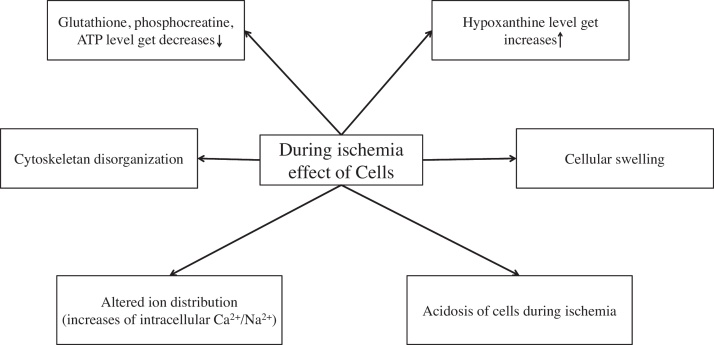
Ischemia is defined as an insufficient supply of the nutrient and oxygen to the cardiac muscle. During ischemia, the level of glutathione, phosphocreatine and adenosine triphosphate (ATP) are reduced and hypoxanthine level gets elevated. Altered ion distribution, i.e. increase in intracellular Ca2+/Na2+, cellular swelling, cytoskeleton disorganization and acidosis of cells occur39 (Fig. 1).
Fig. 1.
Cellular myocardial ischemia injury.
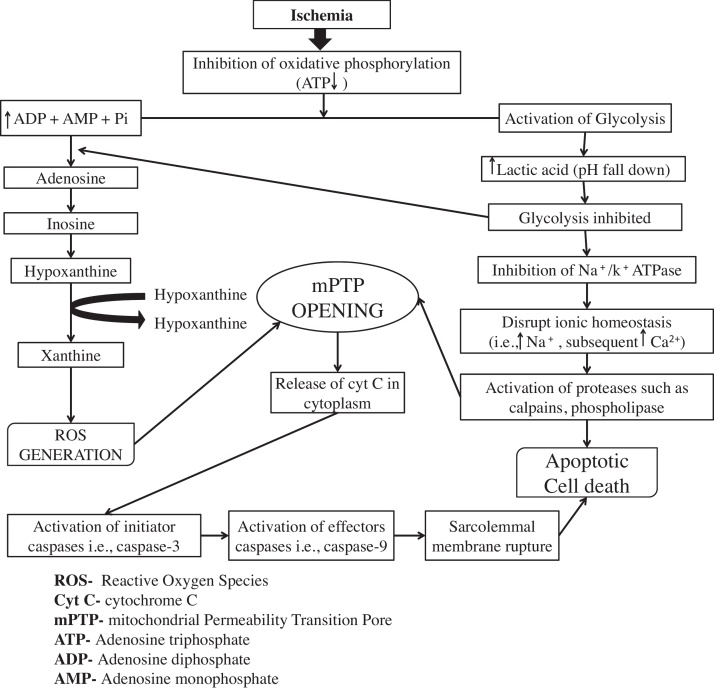
Myocardial ischemia injury leads to the inhibition of oxidative phosphorylation that decreases the level of adenosine diphosphate (ADP) and elevates adenosine monophosphate (AMP). AMP further forms adenosine that gets converted into inosine and hypoxanthine.40, 41 Further hypoxanthine forms xanthine via xanthine dehydrogenase and accounts for the activation of ROS.34 Inhibition of Na+/K+ ATPase and formation of ionic homeostasis (increases of Na+ and Ca+ ions) activates protease, i.e. calpains and phospholipases which are responsible for direct apoptosis cell death.42, 41 It also release cytokine C in the cytoplasm then activates effectors caspases and ruptures sarcolemmal membrane43 (Fig. 2).
Fig. 2.
Myocardial ischemia injuries.
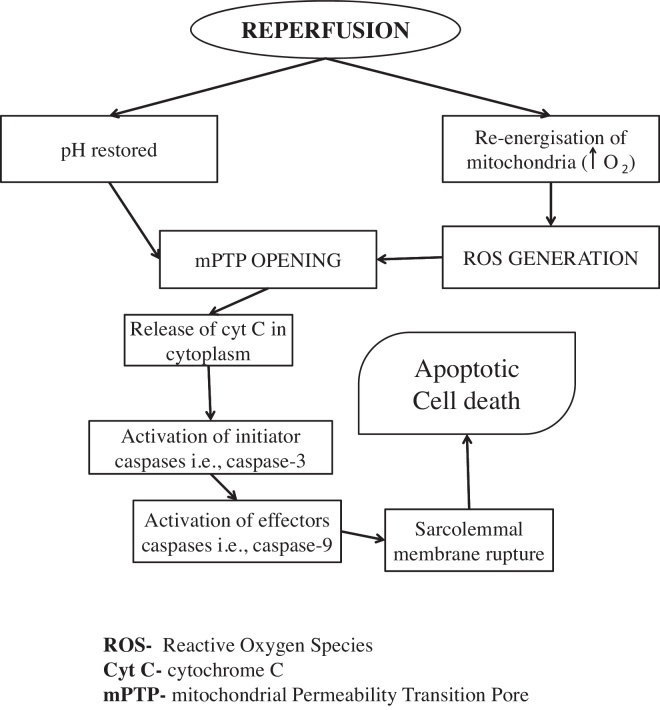
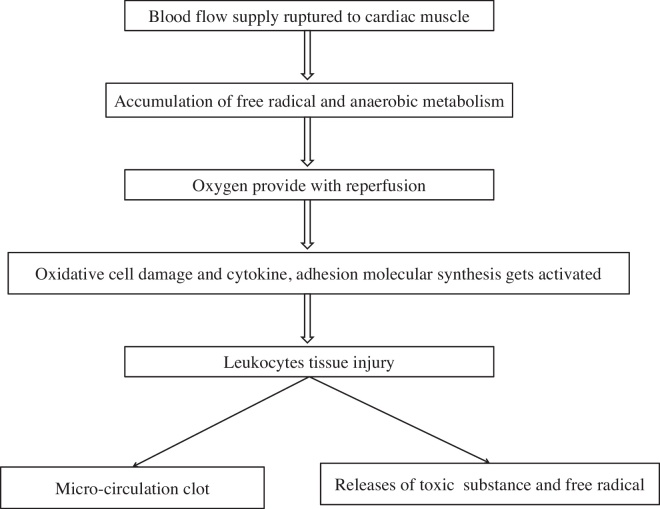
During reperfusion injury, re-energization of mitochondria generate reactive oxygen species.44, 45 It is documented that cell membrane damage during reperfusion is caused due to peroxidation of lipid and oxidizing agents such as peroxynitrite and hydroxyl radical.44, 46 Both reactive oxygen species and restored pH are responsible for the opening of mPTP during reperfusion injury. Activation of mPTP accelerates the release of cyt C and caspases to the ruptured sarcolemmal membrane that further leads to apoptosis cell death47 (Fig. 3). During reperfusion followed after ischemia, blood supply results in anaerobic metabolism, cardiac muscles rupture, cytokines damage, micro-circulation clots and accumulation of free radical in myocardium48 (Fig. 4).
Fig. 3.
Myocardial reperfusion injury.
Fig. 4.
Purpose of inflammatory cascade in myocardial ischemia/reperfusion (I–R) injury.
4. Role of heart RAS in I/R injury and ischemic preconditioning (IPC)
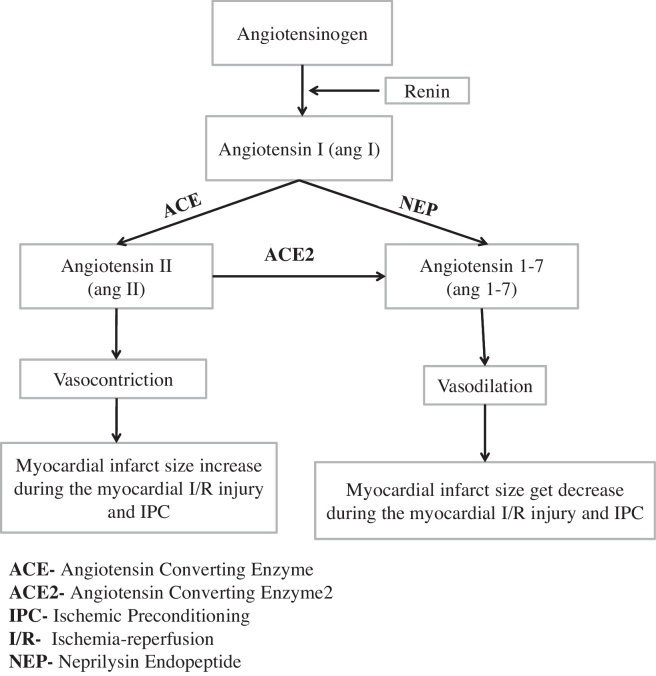
Renin angiotensin system plays an important role in myocardial ischemic and reperfusion injury (I/R). Cardiac RAS system consist of angiotensinogen, Ang I, Ang II, ACE, ACE 2, angiotensin 1–7, angiotensin 1–9 and angiotensin 1–5. Angiotensin I (vasodilator) convert into angiotensin II (Ang II) via angiotensin converting enzyme (ACE). Moreover, angiotensin I and angiotensin II (vasoconstrictor) also convert into angiotensin 1–7 by neprilysin endopeptide (NEP).12, 49 I/R injury get upregulated by induction of vasoconstrictors that leads to increased myocardial infarct size.50 Charan et al. in 2016 reported that atrial natriuretic peptide (ANP) restores the attenuated cardioprotective effect of IPC in diabetic rat heart51, 52 (Fig. 5).
Fig. 5.
Role of heart renin angiotensin system in I/R injury and IPC.
Singh et al., in 1999 investigated the cardioprotective role of angiotensin (Ang II) in ischemia preconditioning. Angiotensin II has been shown to reduce LDH, CKMB and infarct size. Nunez et al. reported that angiotensin-II induced preconditioning (APC) along with ischemic preconditioning (IPC) exhibited cardioprotection by affecting mitochondrial respiration and cardiac functions.53, 54
Loot et al., in 2002 reported that angiotensin (1–7) attenuates the development of heart failure after myocardial infarction in rat. Trask et al., in 2007 observed that angiotensin (1–7) regulates cardiac functions, blood pressure, cardiac hypertrophy, heart failure and growth of cells. Angiotensin (1–7) has anti-proliferative action on the vascular smooth muscles, cardiac muscles cells and improves endothelial functions by releasing bradykinin and nitric oxide.55, 56
5. Cardiac RAS and the role of ACE inhibitor/ACE 2 activator and angiotensin II antagonist
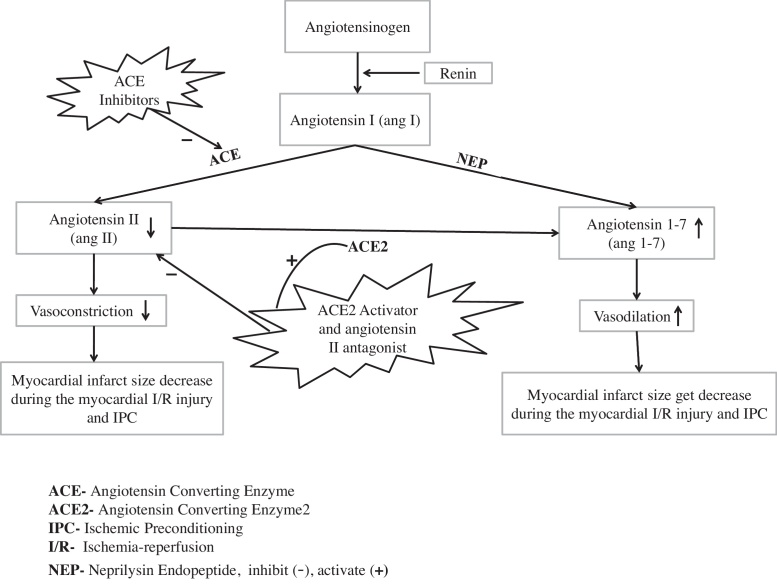
ACE inhibitors are vasodilators, used for the treatment of hypertension, CHF and myocardial infarction. ACE inhibitors have shown protective effect in 50% of patients with hypertension, and have proved to reduce morbidity and mortality rates.57 They inhibit angiotensin converting enzyme, which are responsible for the formation of angiotensin II (a vasoconstrictor) and decrease the myocardial infarct size. ACE inhibitor have shown to attenuate myocardial (I/R) injury by reducing the level of angiotensin II and increasing the level of angiotensin 1–7 (a vasodilator). They have promising approach to restore the cardioprotective effect of myocardial I/R injury58, 59, 60 (Fig. 6). Macedo et al., in 2016 reported the cardioprotective effect of angiotensin converting enzyme 2 activator (diminazene aceturate) in cardiomyocytes hypertrophy.61 Qi et al., in 2013 reported that diminazene aceturate attenuates ischemia induced cardiovascular diseases by enhancing the activity of angiotensin converting enzyme 2. Diminazene aceturate also attenuate left ventricular remodeling, post-myocardial infarction and play a major role in the treatment of myocardial infarction. ACE2 activates the circulating endothelial progenitor cells in the blood which decreases the inflammatory cells and increases the cardiac progenitor cells in the region of peri-infarct cardiac muscles.62 It also enhances the function of heart and increases the level of angiotensin 1–7 in the both human and rats. ACE inhibitors (e.g. captopril) as well as ACE 2 activators (e.g. diminazene aceturate) alone or in combination have shown to attenuate the myocardial (I/R) injury by decreasing the level of angiotensin II, increasing the level of angiotensin 1–7 and infarct size reduction63 (Fig. 6). Angiotensin II antagonist drugs like valsartan inhibits the angiotensin II and reduces infarct size. Combined treatment of ACE inhibitors (e.g. captopril) and angiotensin II antagonist (e.g. valsartan) has shown to attenuate the myocardial (I/R) injury by decreasing the level of angiotensin II64, 65 (Fig. 6).
Fig. 6.
Role of heart renin angiotensin system in I/R injury and IPC: with the treatment of ACE inhibitors, ACE2 activator and angiotensin II antagonist.
6. Conclusions
Myocardial damage of tissue during reperfusion after ischemia insult is known as myocardial ischemia–reperfusion (I/R) injury. Myocardial I/R injury increase the excessive expression of oxygen, sodium and calcium ions which are responsible for activation of proteases (e.g. calpaines and phospholipase) and lead to cardiac cell death. In heart RAS, angiotensin-(1–7) is responsible for vasodilation and angiotensin II is for vasoconstriction. In this article, we have reported that I/R injury get upregulated by angiotensin II which leads to increased infarct size. Above evidences suggests that infarct size can be reduced by ACE inhibitors, ACE2 activators and angiotensin II antagonist.
Conflicts of interest
The authors have none to declare.
Acknowledgments
The authors are grateful to Shri Narayan Das Agrawal Ji, Chancellor, GLA University, Prof. D.S. Chauhan, Vice Chancellor, GLA University, Prof. Pradeep Mishra, Director, Institute of Pharmaceutical Research, GLA University, and Prof. Meenakshi Bajpai, Head of Department, Institute of Pharmaceutical Research, GLA University, Mathura, for their praiseworthy inspiration and constant support for this study.
References
- 1.Shanthi M., Pekka P. vol. 13. World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization; 2010. pp. 3–18. (Global Atlas on Cardiovascular Diseases Prevention and Control). [Google Scholar]
- 2.Bernard J.G., Karen S., Bongani M.M., Salim Y. The epidemic of cardiovascular disease in the developing world: global implications. Eur Heart J. 2010;31:642–648. doi: 10.1093/eurheartj/ehq030. [DOI] [PubMed] [Google Scholar]
- 3.Charlson F.J., Moran A.E., Freedman G. The contribution of major depression to the global burden of ischemic heart disease: a comparative risk assessment. BMC Med. 2013;11:250. doi: 10.1186/1741-7015-11-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collard C.D., Gelman S. Pathophysiology, clinical manifestation and prevention of ischemia reperfusion injury. Anesthesiology. 2001;94:1133–1138. doi: 10.1097/00000542-200106000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Hearse D. Reperfusion of the ischemic myocardium. J Mol Cell Cardiol. 1977;9:605–616. doi: 10.1016/s0022-2828(77)80357-x. [DOI] [PubMed] [Google Scholar]
- 6.Jepson P.N. Ischemic contracture: experimental study. Ann Surg. 1926;84:785. doi: 10.1097/00000658-192612000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dostal D.E., Baker K.M. The cardiac renin–angiotensin system conceptual or a regulator of cardiac function. Circ Res. 1999;85:643–650. doi: 10.1161/01.res.85.7.643. [DOI] [PubMed] [Google Scholar]
- 8.Paul M., Poyan M.A., Kreutz R. Physiology of local renin–angiotensin system. Physiol Rev. 2006;86(3):747–803. doi: 10.1152/physrev.00036.2005. [DOI] [PubMed] [Google Scholar]
- 9.Lawata M., Cowling R.T., Yeo S., Greenberg B. Targeting the ACE2-Ang-(1–7) pathway in cardiac fibroblasts to treat cardiac remodeling and heart failure. J Mol Cell Cardiol. 2011;51(4):542–547. doi: 10.1016/j.yjmcc.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamming I., Timens W., Bulthuis M.L., Lely A.T., Navis G. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus: a first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):6317. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi L., Mao C., Xu Z., Zhang L. Angiotensin-converting enzymes and drug discovery in cardiovascular diseases. Drug Discov Today. 2013;15(9):332–341. doi: 10.1016/j.drudis.2010.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryu W.S., Kim S.W., Kim C.J. Overview of the renin–angiotensin system. Korean Circ J. 2007;37:91–96. [Google Scholar]
- 13.Schwarz E.R., Montio H., Fleischhauer J., Klues H.G., Vom Dal J., Hanrath P. Angiotensin II receptor antagonist EXP 3174 reduces infarct size comparable with enalapril and augment preconditioning in the pig heart. Cardiovasc Drugs Ther. 1997;11(5):687–695. doi: 10.1023/a:1007743125918. [DOI] [PubMed] [Google Scholar]
- 14.Martnez L.A., Molina R.V. Early and chronic captopril or losarten therapy reduce infarct size and avoids congestive heart failure after myocardial infarction in rats. Arch Med Res. 2003;34:357–361. doi: 10.1016/S0188-4409(03)00076-6. [DOI] [PubMed] [Google Scholar]
- 15.Dzau V.J., Ellison K.E., Brody T., Ingelfinger J., Pratt R. A comparative study of the distribution of renin and angiotensinogen messenger ribonucleic acids in rat and mouse tissues. Endocrinology. 1987;120:2334–2338. doi: 10.1210/endo-120-6-2334. [DOI] [PubMed] [Google Scholar]
- 16.Campbell D.J., Habener J.F. The angiotensinogen gene is expressed and differentially regulated in multiple tissues of the rat. J Clin Invest. 1986;78:31–39. doi: 10.1172/JCI112566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hellmann W., Suzuki F., Ohkubo H., Nakanishi S., Ludwig G., Ganten D. Angiotensinogen gene expression in extrahepatic rat tissues: application of a solution hybridization assay. Naunyn Schmiedebergs Arch Pharmacol. 1988;338:327–331. doi: 10.1007/BF00173408. [DOI] [PubMed] [Google Scholar]
- 18.Ulfendahl H.R., Aurell M. Portland Press; London: 1998. Renin–Angiotensin: A Centenary Symposium of the Discovery of the Renin–Angiotensin System; pp. 1–12. [Google Scholar]
- 19.Samani N.J., Morgan K., Brammar W.J., Swales J.D. Detection of renin messenger RNA in rat tissues: increased sensitivity using an RNAse protection technique. J Hypertens. 1987;5:19–21. doi: 10.1097/00004872-198707002-00005. [DOI] [PubMed] [Google Scholar]
- 20.Paul M., Wagner D., Metzger R. Quantification of renin mRNA in various mouse tissues by novel solution hybridization assays. J Hypertens. 1988;6:247–252. doi: 10.1097/00004872-198803000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Lindpaintner D., Lu W., Neidermajer N. Selective activation of cardiac angiotensinogen gene expression in post-infarction ventricular remodeling in the rat. J Mol Cell Cardiol. 1993;25:133–143. doi: 10.1006/jmcc.1993.1017. [DOI] [PubMed] [Google Scholar]
- 22.Berk B.C., Corson M.A. Angiotensin II signals transduction in vascular smooth muscle: role of tyrosine kinases. Circ Res. 1997;80:607–616. doi: 10.1161/01.res.80.5.607. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Y., Griendling K.K., Dikalova A., Owens G.K., Taylor W.R. Vascular hypertrophy in angiotensin II-induced hypertension is mediated by vascular smooth muscle cell-derived H2O2. Hypertension. 2005;46:732–737. doi: 10.1161/01.HYP.0000182660.74266.6d. [DOI] [PubMed] [Google Scholar]
- 24.De Leeuw P.W. How do angiotensin II receptor antagonists affect blood pressure? Am J Cardiol. 1999;84:5–6. doi: 10.1016/s0002-9149(99)00399-9. [DOI] [PubMed] [Google Scholar]
- 25.Dielis A.W., Smid M., Spronk H.M. The prothrombotic paradox of hypertension: role of the renin–angiotensin and kallikreinkinin systems. Hypertension. 2005;46:1236–1242. doi: 10.1161/01.HYP.0000193538.20705.23. [DOI] [PubMed] [Google Scholar]
- 26.Brown N.J., Vaughan D.E. Angiotensin-converting enzyme inhibitors. Circulation. 1998;97:1411–1420. doi: 10.1161/01.cir.97.14.1411. [DOI] [PubMed] [Google Scholar]
- 27.Schiffrin E.L. Effects of antihypertensive drugs on vascular remodeling: do they predict outcome in response to antihypertensive therapy? Curr Opin Nephrol Hypertens. 2001;10:617–624. doi: 10.1097/00041552-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Rigat B., Hubert C., Alhenc-Gelas F., Cambien F., Corvol P., Soubrier F. An insertion/deletion polymorphism in the angiotensin I-converting enzyme gene accounting for half the variance of serum enzyme levels. J Clin Invest. 1990;86:1343–1346. doi: 10.1172/JCI114844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Farmer J.A. Renin angiotensin system and ASCVD. Curr Opin Cardiol. 2000;15:141–150. doi: 10.1097/00001573-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Krum H., Gilbert R.E. Novel therapies blocking the renin–angiotensin–aldosterone system in the management of hypertension and related disorders. J Hypertens. 2007;25:25–35. doi: 10.1097/HJH.0b013e3280113950. [DOI] [PubMed] [Google Scholar]
- 31.Cerra F.B., Lajos T.Z., Montes M., Siegel J.H. Hemorrhagic infarction: a reperfusion injury following prolonged myocardial ischemic anoxia. Surgery. 1975;78:95–104. [PubMed] [Google Scholar]
- 32.Grunenfelder J., Miniati D.N., Murata S. Upregulation of bcl-2 through caspase-3 inhibition ameliorates ischemia/reperfusion injury in rat cardiac allografts. Circulation. 2001;104:202–206. doi: 10.1161/hc37t1.094833. [DOI] [PubMed] [Google Scholar]
- 33.Balakumar P., Singh H., Singh M., Srivastava A. The impairment of preconditioning mediated cardioprotective in pathological conditions. Pharmacol Res. 2009;60:18–23. doi: 10.1016/j.phrs.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Becker L.B. New concepts in reactive oxygen species and cardiovascular reperfusion physiology. Cardiovasc Res. 2004;61:461–470. doi: 10.1016/j.cardiores.2003.10.025. [DOI] [PubMed] [Google Scholar]
- 35.Balakumar P., Singh M. Anti-TNF-therapy in heart failure: future directions. Basic Clin Pharmacol Toxicol. 2006;99:391–397. doi: 10.1111/j.1742-7843.2006.pto_508.x. [DOI] [PubMed] [Google Scholar]
- 36.Szocs K. Endothelial dysfunction and reactive oxygen species production in ischemia/reperfusion and nitrite tolerance. Gen Physiol Biophys. 2004;23:265–295. [PubMed] [Google Scholar]
- 37.Malek M., Nematbakhsh M. Renal ischemia/reperfusion injury from pathophysiology to treatment. J Renal Inj Prev. 2015;4(2):20–27. doi: 10.12861/jrip.2015.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sharfuddin A.A., Molitoris B.A. Pathophysiology of ischemic acute kidney injury. Nat Rev Nephrol. 2011;7:189–200. doi: 10.1038/nrneph.2011.16. [DOI] [PubMed] [Google Scholar]
- 39.Chamoun F., Burne M., Donnell M.O., Rabb H. Pathophysiologic role of selectins and their ligands in ischemia reperfusion injury. Front Biosci. 2000;5(1):103–109. doi: 10.2741/chamoun. [DOI] [PubMed] [Google Scholar]
- 40.Solaini G., Harris D.A. Biochemical dysfunction in heart mitochondria exposed to ischaemia and reperfusion. Biochem J. 2005;390:377–394. doi: 10.1042/BJ20042006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Powers S.K., Murlasits Z., Wu M., Kavazis A.N. Ischemia–reperfusion-induced cardiac injury: a brief review. Med Sci Sports Exerc. 2007;39:1529–1536. doi: 10.1249/mss.0b013e3180d099c1. [DOI] [PubMed] [Google Scholar]
- 42.Baines C.P. The mitochondrial permeability transition pore and ischemia–reperfusion injury. Basic Res Cardiol. 2009;104:181–188. doi: 10.1007/s00395-009-0004-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cardone M.H., Roy N., Stennicke H.R. Regulation of cell death protease caspase-9 by phosphorylation. Science. 1998;282:1318–1321. doi: 10.1126/science.282.5392.1318. [DOI] [PubMed] [Google Scholar]
- 44.Detmers P.A., Lo S.K., Olsen-Egbert S.K.E., Walz A. Neutrophil-activating protein-1/interleukin-8 stimulates the binding activity of the leukocyte adhesion receptor CD11b/CD18 on human neutrophils. J Exp Med. 1999;171:1155–1162. doi: 10.1084/jem.171.4.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Elimadi A., Sapena R., Settaf A., Louet H. Attenuation of liver normothermic ischemia–reperfusion injury by preservation of mitochondrial functions with S-15176, a potent trimetazidine derivative. Biochem Pharmacol. 2000;62:509–516. doi: 10.1016/s0006-2952(01)00676-1. [DOI] [PubMed] [Google Scholar]
- 46.Halestrap A.P., Clarke S.J., Javadov S.A. Mitochondrial permeability transition pore opening during myocardial reperfusion – a target for cardioprotection. Cardiovasc Res. 2004;61:372–385. doi: 10.1016/S0008-6363(03)00533-9. [DOI] [PubMed] [Google Scholar]
- 47.Bolli R., Jeroudi M.O., Patel B.S. Direct evidence that oxygen-derived free radicals contribute to post ischemic myocardial dysfunction in the intact dog. Proc Natl Acad Sci U S A. 1989;86:4695–4699. doi: 10.1073/pnas.86.12.4695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zong W., Thompson C.B. Necrotic death as a cell fate. Genes Dev. 2006;20:1–15. doi: 10.1101/gad.1376506. [DOI] [PubMed] [Google Scholar]
- 49.Ajmani P., Yadav H.N., Singh M., Sharma P.L. Possible involvement of caveolin in attenuation of cardioprotective effect of ischemic preconditioning in diabetic rat heart. BMC Cardiovasc Disord. 2011;11:43. doi: 10.1186/1471-2261-11-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Skovsted G.F., Kruse L.S., Larsen R., Pedersen A.F. Heart ischemia–reperfusion induces local up-regulation of vasoconstriction endothelin ETB receptors in rat coronary arteries downstream of occlusion. Br J Pharmacol. 2004;171(11):2726–2738. doi: 10.1111/bph.12606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Charan K., Goyal A., Gupta J.K., Yadav H.N. Role of atrial natriuretic peptide in ischemia preconditioning-induced cardioprotection in the diabetic rat heart. J Surg Res. 2016;201:272–275. doi: 10.1016/j.jss.2015.10.045. [DOI] [PubMed] [Google Scholar]
- 52.Wang S.Y., Cui X.L., Xue F.S. Combined morphine and limb remote and ischemia preconditioning provides an enhanced protection against myocardial ischemia/reperfusion injury by antiapoptosis. J Surg Res. 2016;202(1):13–25. doi: 10.1016/j.jss.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 53.Sharma A., Singh M. Role of angiotensin in cardioprotective effect of ischemia preconditioning. J Cardiovasc Pharmacol. 1999;33(5):772–778. doi: 10.1097/00005344-199905000-00014. [DOI] [PubMed] [Google Scholar]
- 54.Nunez R.E., Castro M., Javadov S., Escobales N. Angiotensin II and ischemia preconditioning synergize to improve mitochondrial function while showing additive effects on ventricular post-ischemia recovery. J Cardiovasc Pharmacol. 2014;64(2):172–179. doi: 10.1097/FJC.0000000000000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Loot A., Roks A.J., Henning R.H. Angiotensin (1–7) attenuates the development of heart failure after myocardial infarction in rat. Circ AHA J. 2002;105(13):1548–1550. doi: 10.1161/01.cir.0000013847.07035.b9. [DOI] [PubMed] [Google Scholar]
- 56.Trask A.J., Ferrario C.M. Angiotensin-(1–7): pharmacology and new perspectives in cardiovascular treatments. Cardiovasc Drug Rev. 2007;25(2):162–174. doi: 10.1111/j.1527-3466.2007.00012.x. [DOI] [PubMed] [Google Scholar]
- 57.Pfeffer M.A., Greaves S.C., Arnold M.O. Early versus delayed angiotensin-converting enzyme inhibition therapy in acute myocardial infarction: the healing and early after load reducing therapy trial. Circulation. 1997;95:2643–2651. doi: 10.1161/01.cir.95.12.2643. [DOI] [PubMed] [Google Scholar]
- 58.Yang J., Jiang H., Yang J. Valsartan preconditioning protect against myocardial ischemia reperfusion injury through TLR4/NF-kappaB signaling pathway. Mol Cell Biochem. 2009;330:39–46. doi: 10.1007/s11010-009-0098-1. [DOI] [PubMed] [Google Scholar]
- 59.Arendell R., Lawson J.D., Petracek M.R. Study of Sat-l-Alas angiotensin II (saralasin) responsiveness in hypertension of renal origin. J Surg Res. 1978;24:284–287. doi: 10.1016/0022-4804(78)90093-8. [DOI] [PubMed] [Google Scholar]
- 60.Hartman J.C., Wall T.M., Hullinger T.G., Shebuski R.J. Reduction of myocardial infarct size in rabbits by ramiprilat: reversal by the bradykinin antagonist HOE 140. J Cardiovasc Pharmacol. 1993;21:996–1003. doi: 10.1097/00005344-199306000-00022. [DOI] [PubMed] [Google Scholar]
- 61.Macedo L.M., Souza D.S., Pedrino G.R. Cardioprotective effect of diminazene aceturate in pressure overloaded rat heart. Life Sci. 2016;3205(16):30256–30259. doi: 10.1016/j.lfs.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 62.Qi Y., Zhang J., Cole-Jeffrey C.T. Diminazene aceturate enhances angiotensin converting enzyme 2 activity and attenuates ischemic induced cardiac pathophysiology. Hypertension. 2013;62(4):746–752. doi: 10.1161/HYPERTENSIONAHA.113.01337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ohtsuki M., Morimoto S., Izawa H. Angiotensin converting enzyme 2 gene expression increased compensatory for left ventricular remodeling in patients with end-stage heart failure. Int J Cardiol. 2010;145:333–334. doi: 10.1016/j.ijcard.2009.11.057. [DOI] [PubMed] [Google Scholar]
- 64.Qiu Y., Shil P.K., Zhu P. Angiotensin-converting enzyme 2 (ACE2) activator diminazene aceturate ameliorates endotoxin induced uveitis in mice. Invest Ophthalmol Vis Sci. 2014;55:3809–3818. doi: 10.1167/iovs.14-13883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vishwakarma V.K., Qureshi S.S., Agrawal V., Gupta J.K. Role of atrial natriuretic peptides in various conditions. Int J Pharm Biol Sci. 2016;7(3):20–27. [Google Scholar]