Abstract
Percutaneous coronary intervention (PCI) in bifurcation lesions is associated with lower success rate, higher acute complication rates and higher event rates in follow-up.
The reason for this higher than usual complication rate relates to the relationship between anatomy, flow, and atheroma distribution in bifurcation lesions.
Further, stenting these lesions can be a prolonged procedure and can be technically more demanding. The most common complication is the loss of significant side branch (SB). Main vessel (MV) stenting may enhance the carina displacement and atheroma shift across the SB ostium leading to SB ostium narrowing.
Finally, complications, if they occur, are more difficult to manage. Dedicated bifurcation stent has been developed to overcome the number of limitations associated with conventional bifurcation PCI. The main advantage of most dedicated bifurcation stents is to allow the operator to perform the procedure on a bifurcation lesion without the need to rewire the SB.
Keywords: Bifurcation, Lesions, Main vessel stenting, Proximal bifurcation stent, SB stent
1. How bifurcation lesion is mechanistically different from other lesions?
Blood flow through a bifurcation vessel is governed by the ramification law of the epicardial coronary tree which simply means that there is a good correlation between side branch (SB) diameter and length and the mass supplied by this vessel. Thus, longer and larger diameter vessels have more blood flowing through them.2
Three diameters rule: The size of a vessel (as also the flow through it) is dictated by the three-diameter rule which states that the relation between true size of the main branch (MV) and distal main branch (DMV) and side-branch (SB) can be dictated by scaling laws like Murrays's Law ({MV}3 = {DMV}3 + {SB},3 or simplistically by Law of Finet which states that size of MV is 2/3rd of sum of both the distal branches (MV = 0.678{DMV + SB})1, 2.
Atheroma distribution and thrombus formation in bifurcation lesion: The atheroma distribution in bifurcation situation is also different from non-bifurcation areas. Physiologically atheroma is distributed in the areas of: (a) low endothelial shear stress (inner areas of curvatures, upstream of stenosis) and (b) oscillatory endothelial shear stress (lateral wall of bifurcation, downstream of stenosis, irregular arterial regions, branch points: plaques are located opposite the SB take-off and are more concentric proximal to the SB and more eccentric just distal to side-branch). The plaques are also influenced by the angle of SB take-off, it being deposited preferentially toward acute angle (toward an inner radius of curvature) and away from obtuse angle. Atheroma is less common in the region of carina but more common where there is wide bifurcation angle, increased ratio of SB dimension in relation to main branch, or increased bifurcation tortuosity. On the other hand, late stent thrombosis (ST) is more common in the areas of high shear stress where less re-endothelisation occurs such as carina.
As a consequence of all these mechanistic differences, the outcomes of percutaneous coronary intervention (PCI) in these subset of patients may be much different than non-bifurcated lesions.
1.1. Correlates of clinical outcomes in bifurcation lesions
-
1.
Final angiographic result in MV: this is generally the single most important predictor of the clinical outcome. Thus, many 2-stent strategies which lead to a high metal mass at carina (which actually requires least scaffolding because carina is the flow divider with high shear stress and therefore generally free of plaques), as also alter the flow dynamics but also go against the 3-diameter rule. That is why most studies demonstrate that irrespective of type of stents used and in all types of lesion classifications (except for Medina 0, 0, 1, i.e. isolated SB stenosis or those lesions with diffuse involvement of the SB), a single stent strategy is nearly always better than a 2-stent strategy.3 The superiority lies in lower peri-procedural MI and possibly lower major adverse cardiac event (MACE), restenosis and ST rates as also in lower procedural time, contrast volume and radiation exposure with provisional SB stenting strategy. The 2-stent strategy is especially associated with a worse outcome if bifurcation angle is >50°.
-
2.
Result in the ostium of SB while not co-relative of major events is still responsible for minor events. Thus, when SB is important and diffusely diseased, it does increase requirement of re-intervention. Further, in some cases with a single stent strategy, the SB may be irretrievably lost. In those cases 2-stent strategy, which provides definitive scaffolding of SB ostium may be useful.
1.2. When to use 2 stent strategies?
The major limitation of a single stent strategy is an inability to provide enough scaffolding to the ostium of the SB, which can lead to higher restenosis rate and higher need for target lesion revascularization (TLR). Therefore, in those cases, where SB is very important and likely to get compromised with 1-stent only strategy, a 2-stent strategy may be required initially (≈10% of cases). Possible situations where a 2-stent strategy can be recommended to begin with are:
-
1.
SB is large in diameter (>2.5 mm) and territory of distribution and there is a risk of hemodynamic deterioration, if SB is lost (poor LVEF, distal left main).
-
2.
SB has severe disease (>50%) that extends beyond the ostium (10–20 mm or more).
-
3.
Have an unfavorable angle (narrow angle A: the angle between proximal MV and SB) for re-crossing after MV stent implantation.N.B. Remember that when angle A is narrow (<120°), insertion of guidewire increases the angle by an average of 33°.
1.3. How to choose 2 stent strategies?
-
1.
Strategies with minimal metal overlap of 2 stents are the best: Mini-crush is better than classical crush because metal overlap is less, residual metallic stenosis at ostium is less, and there is a better scaffolding of ostium. The long-term re-endothelization is also better, which may translate into lower restenosis and late ST (most serious limitations of classical crush). T stenting with minimal protrusion (TAP) is better than classical T stenting, because there are fewer gaps in ostial coverage (better scaffolding) leading to lower restenosis.
-
2.
If angle between the distal MV and SB (Angle B) is wide, a T stenting type of strategy like TAP technique may be preferable.
-
3.
If angle between the distal MV and SB is narrow (<50°), a V type of strategy like Culottes or Mini Crush may be preferable.
-
4.
Culottes technique may be superior to classical crush technique because of lesser risk of SB restenosis and can be performed through a 6-F guide but is technically more demanding. Moreover, it should not be performed, if there is huge mismatch between the main and daughter vessels.
-
5.
If the procedure has to be done quickly, a simultaneous kissing stent (SKS) may be preferable, because this technique is simple but requires an 8-F guide and produces a metallic neo-carina upstream from the bifurcation that may be prone to ST. Furthermore, if an upstream dissection occurs, it will be difficult to manage.
Thus several techniques have been proposed and used successfully in the true bifurcation lesions.4
1.4. Limitations of current 2-stent strategies: need for dedicated bifurcation stents
-
1.
The main limitation of the current strategies is a high rate of restenosis and re-intervention (in double figures) despite the use of DES especially in SB even with best of the techniques.
-
2.
Higher risk of ST.
Difficulties in techniques and some mechanistic reasons account for poor short- and long-term clinical outcomes are (Table 1):
-
1.
High metal mass where the two stents meet.
-
2.
Irregular overlapping of struts at the carina.
-
3.
Distorted SB stent.
-
4.
Polymer rupture and uneven distribution of stent struts at origin of the SB.
-
5.
Noncompliance with 3-diameter rule and alteration in natural flow dynamics.
Table 1.
Mechanistic characteristics of two-stent techniques.
| Characteristics | T/TAP | Culottes | SKS | Mini-crush |
|---|---|---|---|---|
| Change in flow dynamics | Very little | Little change because double layer of stent struts in proximal MV | Maximum change in flow dynamics because of formation of neo-carina in the proximal MV and also by presence of two additional circulating channels at the junction of two stents implanted in this segment | Some change because of crushed 3 layer of stents at MV adjacent to SB osmium |
| Conformity with 3-diameter rule (bifurcation branching laws) | Somewhat compliant | Less compliant because 2 layers of stent strut in proximal MV | Most compliant | Least compliant as 3 layers of crushed stent struts occluding the MV near the osmium of SB |
| Apposition of stent struts to vessel wall | Impossible to optimally scaffold the SB and at the same time properly appose stent in the MV | Good SB scaffolding can be achieved but apposition of 2 stent struts to proximal MV may be difficult. If apposed twice drug delivered to proximal MV | Impossible to appose all struts to vessel wall because of formation of double barrel which are also likely to become entwined and also formation of neo-carina | Good SB scaffolding, 3 layers of struts are often inadequately apposed to MV predisposing to risk of stent thrombosis. If they are opposed adequately 3 times drug delivered in MV |
1.5. Stent thrombosis
These mechanistic limitations lead to several issues in long-term outcomes; higher MACE, higher TLR, higher restenosis rate, however, the most dreaded one is ST. However, several studies have demonstrated that when properly done, the risk is no greater when 2 stents versus 1 stent is used.5, 6
Besides higher event rate, there may be several technical difficulties with 2-stent techniques as well (Table 2).
-
1.
Mal-orientation/apposition of MV stent (Side-hole stents).
-
2.
SB access not guaranteed (Crush, Culottes technique).
-
3.
Wire-wrap (double wire systems).
-
4.
Difficulty in re-crossing deployed struts.
Table 2.
Technical characteristic.
| Characteristics | T/TAP | Culottes | SKS | Mini-crush |
|---|---|---|---|---|
| Guiding catheter used (Fr) | 6 (classical T), 7 (modified T because 2 stents are delivered simultaneously) | 6 | 7 or 8 (2 stents are delivered simultaneously) | 7 or 8 (2 stents are delivered simultaneously), 6 Fr if double kiss crush is performed |
| Provisional SB stenting possible | Possible | Possible, if first branch to be stented is MV | Not possible | Not possible |
| Ease of handling: Number of steps in the technique | 5 | 7 (most cumbersome) | 1 (easiest) | 3, 6 if double kiss crush performed |
| Number of times rewiring done | 1 | 2 | 0 (rewiring not required) | 1, 2 if double kiss crush is performed |
| Layer of stent struts at the SB (ease of crossing into SB) | 1 | 2 | 0 | 3 |
| Bifurcation angle (B) <70° | Not ideal | Possible | Possible | Ideal |
| Bifurcation angle (B) >70° | Ideal | Possible (can be used in widest spectrum of angles) | Not ideal | Not ideal (MACE increases with angle >50° |
| Diameter of proximal and distal MV nearly same (SB small) | Possible | Not possible | Not possible | Ideal |
| Re-intervention | Easy | Somewhat difficult | Difficult to treat because of formation of membrane at neo-carina and possibility of entwined double barrel | Somewhat difficult |
1.6. Role of dedicated bifurcation stents
In this context, dedicated bifurcation stents lead to excellent results in the MV while providing excellent scaffold in SB as well. Being a complete fit, there are no anatomic or physiologic challenges.
2. Classification of dedicated bifurcation stents
Dedicated bifurcation stents can be broadly divided into 4 categories: (A) MV stenting with SB scaffold; (B) SB stent with MV access; (C) Proximal bifurcation stent, and (D) Bifurcated stent (Table 3).
Table 3.
Classification of dedicated bifurcation devices.
| Device system | Variety |
|---|---|
| MB stenting with some SB scaffold | Frontier |
| Pathfinder | |
| Petal | |
| Side-kick | |
| Trireme | |
| Twin-rail | |
| Nile | |
| Stentys | |
| SB Stent | Side-Guard |
| Tryton | |
| Proximal bifurcation stent | Axxess |
| True bifurcated stent | Medtronic |
Mechanistically, bifurcation stents are divided into 2 types.
-
1.
Stents for provisional SB stenting that facilitate or maintain access to the SB after MB stenting, and do not require recrossing of MB stent struts. These stents allow placement of a second stent on the SB only if needed.
-
2.
Stents that usually require another stent implanted in the bifurcation. Generally these stents (Tryton™ and Sideguard™) are designed to treat the SB first and then doing the MV. However, at the end of the procedure they require re-crossing into the SB for final kissing balloon dilatation (FKBD). On the other hand, Axxess Plus™ is first implanted in the proximal MV at the level of the carina and does not require re-crossing into the SB but may require the additional implantation of 2 further stents to completely treat some types of bifurcation lesions.
2.1.1. MV stenting with SB scaffold
This is most popular approach to bifurcation stenting. It is useful for all types of bifurcation lesions except only SB (001). Here the priority is MV stenting; however, SB scaffold is superior to provisional stenting. It improves drug delivery and reduces the chance of stent and polymer fracture. However, the main limitations are risk of wire wrap, risk of misalignment, a relatively low procedural success: 85–92% and a long learning curve. The advantages and disadvantages of these stents are discussed in Table 4. Several stents of this type are available: Frontier™, Pathfinder™, Petal™, Side-kick™, Trireme™, Twin-rail™, Nile™, Stentys™, etc. (Fig. 1).
Table 4.
Advantages and disadvantages of main vessel stents with side-branch access.
| Alignment of devices | Varieties | Advantages | Disadvantages |
|---|---|---|---|
| Self alignment | 1. Twin Rail | 1. Simple to use | 1. Risk of wire wrap |
| 2. Nile | 2. Intuitive alignment by device | 2. Risk of misalignment | |
| 3. Petal | 3. Relatively low procedural success | ||
| 4. Frontier | 4. Relatively long learning curve | ||
| 5. Abbott SB | |||
| Controlled alignment | 1. Trieme | 1. Less wire wrap | 1. Three guidewires have to be inserted |
| 2. Side-kick | 2. Lower profile | ||
| No alignment required | 1. Stentys | 1. No risk of wire wrap or misalignment | |
| 2. Lower profile | |||
| 3. Only 1 wire required | |||
Fig. 1.
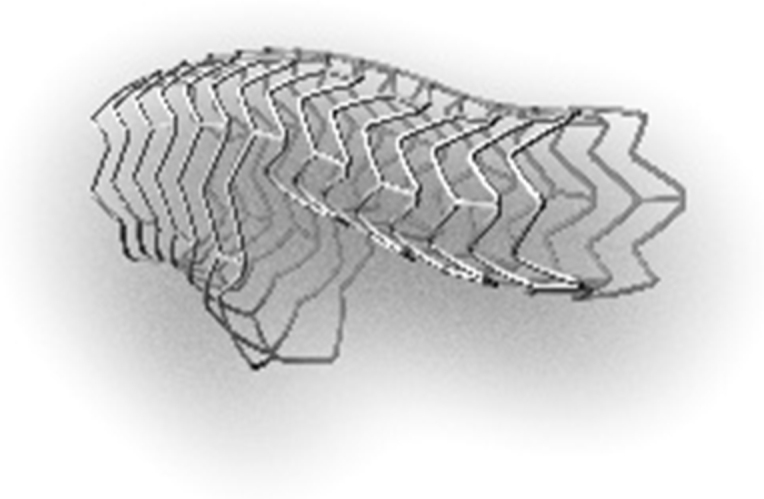
Main vessel stent with side-branch scaffold.
2.1.2. SB stent
These stents are specifically designed to secure the SB and are useful only for true bifurcation lesions. The deliverability is good, and there is no risk of wire wrap. Further, stent positioning is relatively easy, and there is no need for stent rotation to conform to configuration of bifurcation. Finally, MV access is really good. The only disadvantage is that one is committed to 2-stent use; therefore, risk of peri-procedural MI and late ST could be higher. Two stents of this type are available: Capella Side-Guard™ and Tryton™.
2.1.3. Proximal bifurcation stent
Technically, this is the most ideal system of a bifurcation stent. However, the only limitation is difficulty in accurately positioning this stent.
2.1.4. Bifurcated stent
Bifurcated stent system is a novel platform designed reproducibly to permit stenting in bifurcation lesions regardless of branch angulation or plaque location, in a short simple procedure. It consists of 2 balloon catheters and two stents; the mother balloon catheter has a sleeve, through which daughter balloon catheter and stent is loaded. The system is loaded on two wires and both catheters can be simultaneously or independently maneuvered. Two varieties are available: (1) Medtronic Bifurcated Stent; (2) Advanced Bifurcation Systems. Advantage of this system is that it can be a short simple procedure; it can scaffold any bifurcation regardless of size, angle, or plaque location. However, the disadvantages are that the profile is larger, because there is daughter balloon-stent system inside mother balloon-stent system, flexibility is less and being a dual wire system, risk of wire wrap and misalignment is high. Further, all the accompanying disadvantages of 2-stent strategy exist.
3. Bifurcation stent hardware and technique
3.1. Nile Pax™
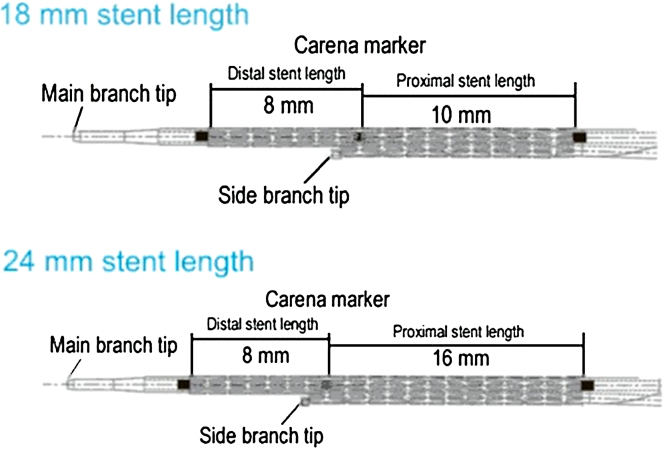
It is a Cobalt Chromium Alloy L605 available in 2 sizes (18 mm and 24 mm). Its strut thickness is 73 μm, coated with 5 μm polymer free abluminal paclitaxel (dose 2.5 μg/mm2) and it is compatible with a 6F sheath. The size refers to total length of the stent where the distal length (for the D MV) is 8 mm and the remaining length is for MV I (Fig. 2). The stent has 3 radio-opaque markers; one each at 2 ends and a central marker at SB tip.
Fig. 2.
Nile Pax™ stent.
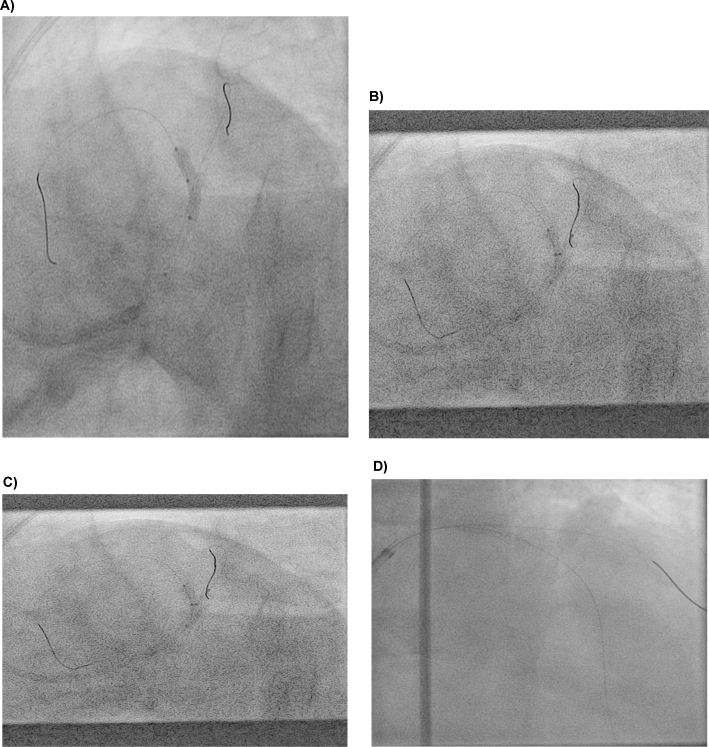
3.2. Deployment sequence (Fig. 3 (A–D))
Fig. 3.
Deployment steps of Nile Pax™ stent. System positioned and main branch balloon dilated. (A) System positioned and main branch balloon dilated; (B) Side-branch balloon positioning; (C) Final kissing balloon dilatation; (D) Distal stents placed if required.
-
1.
System is positioned.
-
2.
Main branch balloon is dilated.
-
3.
SB balloon is positioned.
-
4.
FKBD.
-
5.
Distal stents placed through the stent if required.
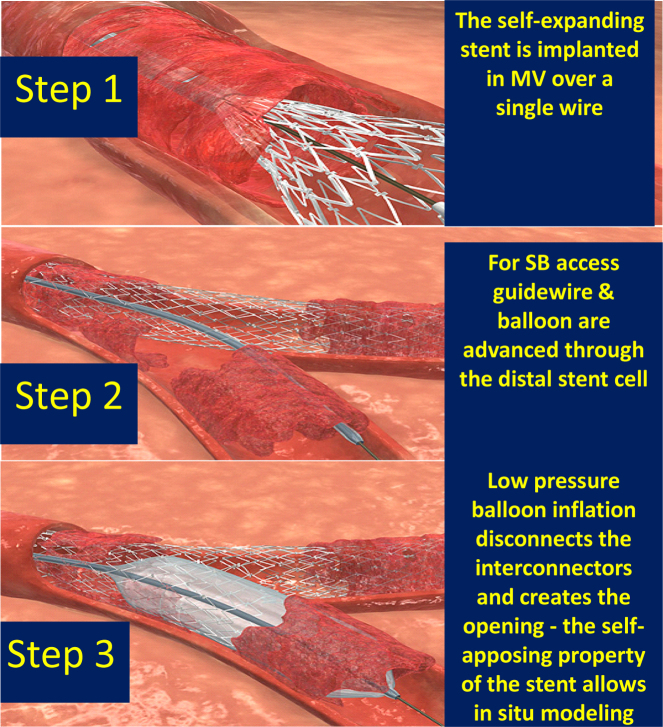
3.3. Stentys™
The STENTYS™ technology consists of a unique, self-expanding nitinol stent platform. The STENTYS DES(P)™ has a bio-stable, poly-sulphone (of polysulphone and soluble polyvinylpyrrolidone) polymer which acts as an excipient eluting Paclitaxel. The STENTYS BMS and DES(P) stents are available in small (2.5–3.0 mm), medium (3.0–3.5 mm), and large (3.5–4.5 mm) and in lengths 17 mm, 22 mm, and 27 mm. The large size stent (indicated for vessels from 3.5 to 4.5 mm) can even expand further up to over 6 mm. It is designed with small distinctive interconnectors that can be utilized to create an opening through the stent. Thus an ordinary DES stent can be converted into a bifurcation stent (MV with SB access). Technically, the procedure is like Provisional T but when the stent is re-crossed by wire into SB and dilated with an angioplasty balloon the stent interconnectors become disconnected and the stent converts into a bifurcation stent with MV scaffold and side-branch access independent of the SB ostium location. The interconnectors are placed all along the length and the circumference of the stent, apart from the first and last 2 mm. Further, its short, expandable segments and its self-expansion feature allow for excellent vessel conformability as well as continuous apposition along the arterial wall, superior to existing balloon-expandable stents (Fig. 4).
Fig. 4.
Design aspects of Stentys™ stent.
3.4. Steps in Stentys stent deployment
-
1.
The stent is implanted in the MV over a single wire, like a standard stent, without any specific positioning related to the SB.
-
2.
If access or treatment of the SB is required, a guidewire and a balloon are advanced through the distal stent cell.
-
3.
A low-pressure balloon inflation disconnects the interconnectors and creates the opening – the self-apposing property of the Stentys™ stent allows the in situ modeling of the stent to within the vessel (Fig. 5).
Fig. 5.
Steps in Stentys™ stent deployment.
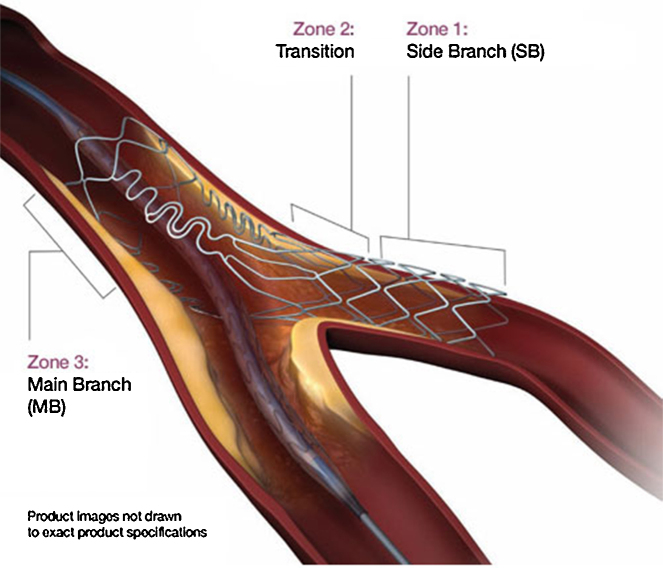
3.5. Tryton™ bifurcation device
It is 84 μm cobalt chromium balloon expandable bare metal stent. It is available in 2 sizes: short (15 mm) and standard (19 mm) compatible with 5F and 6F guide catheters. The stent has a unique design known as Tri-ZONE™ technology. Technically, it has 3 zones. Zone 1: SB zone, which provides superior scaffolding within the SB, securing it acting like any workhorse stent. Zone 2: It is the Transition zone, which provides radial strength and complete coverage to the SB and ostium regardless of bifurcation angle and geometry. Zone 3: Main Branch zone, which because of minimal metal to artery ratio (M:A) allows seamless integration with SB stent. If required, a DES can be placed in this zone (Fig. 6).
Fig. 6.
Tryton™ stent design.
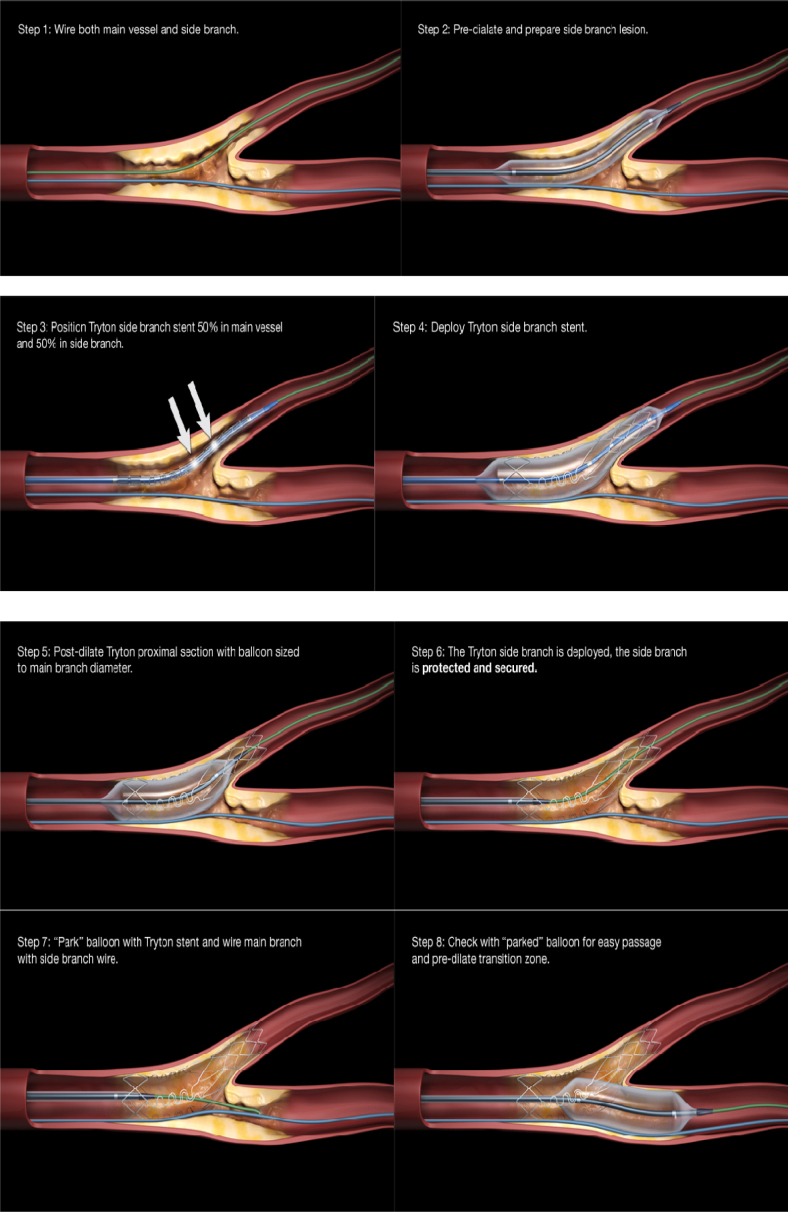
3.6. Deployment sequence
-
1.
Both MV and SB are wired.
-
2.
SB is predilated.
-
3.
Position Tryton™ SB stent 50% in MV and 50% in SB.
-
4.
Deploy Tryton™ SB stent.
-
5.
Post-dilate Tryton™ proximal segment with balloon sized to MV diameter but also extending till SB ostium.
-
6.
The Tryton™ stent is deployed and the SB secured and protected.
-
7.
Park the balloon within Tryton™ stent and wire the main branch with the wire in SB.
-
8.
Check that the “parked” balloon passes easily to DMV and dilate the transition zone with it.
-
9.
Position MV DES 1 mm proximal to SB arm of Tryton™ stent to ensure optimal scaffolding.
-
10.
After properly positioning the MV DES removed the jailed MV wire.
-
11.
Deploy MV stent.
-
12.
Rewire SB.
-
13.
Perform FKBD (Fig. 7).
Fig. 7.
Steps in Tryton™ stent deployment.
3.7. Axxess Plus™
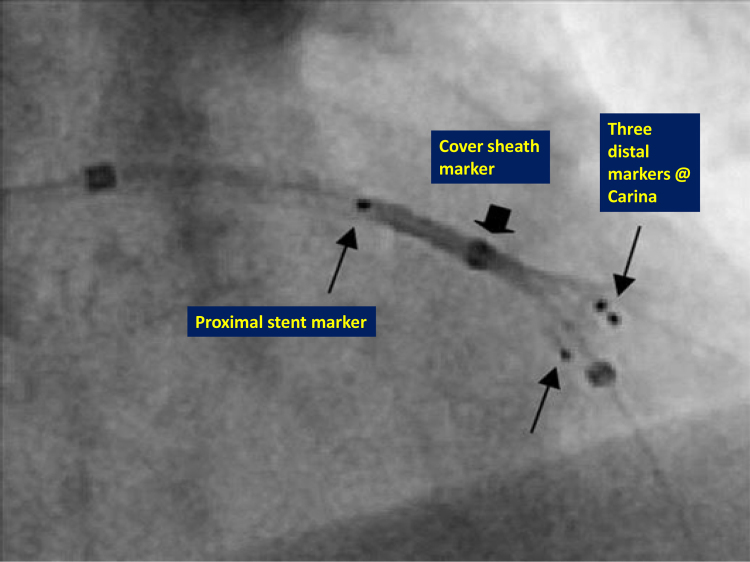
The Axxess™ stent is made from a self-expanding nitinol in the austenitic (superelastic) phase. The stent elutes Biolimus A9 (which has the highest lipophilicity among the common limus group of drugs). Drug release is mediated by a bioabsorbable polylactic acid-based polymer (which is metabolized over time into carbon dioxide and water within 6–9 months) applied to the abluminal surface of the stent. The nominal drug loading is 22 μg/mm of stent length for all sizes. It is available in two lengths of 11 mm and 14 mm and two diameters of 3 mm and 3.5 mm (Fig. 8).
Fig. 8.
Markers on the Axxess™ stent.
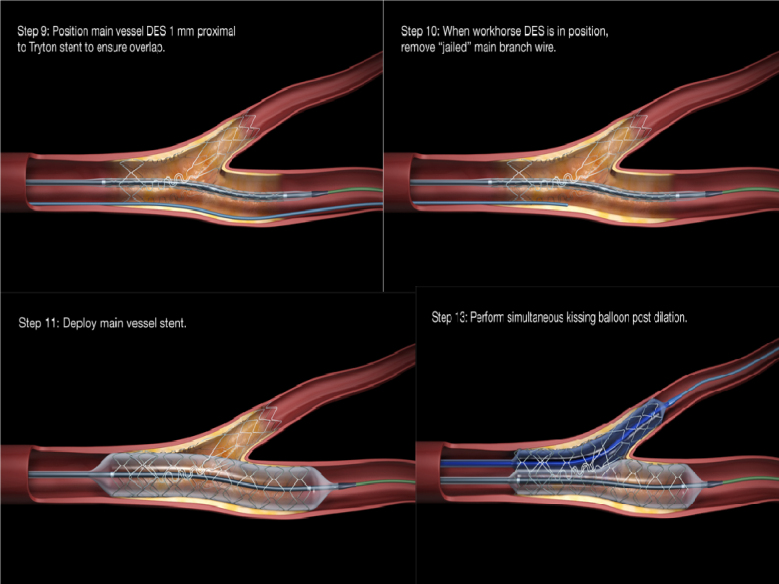
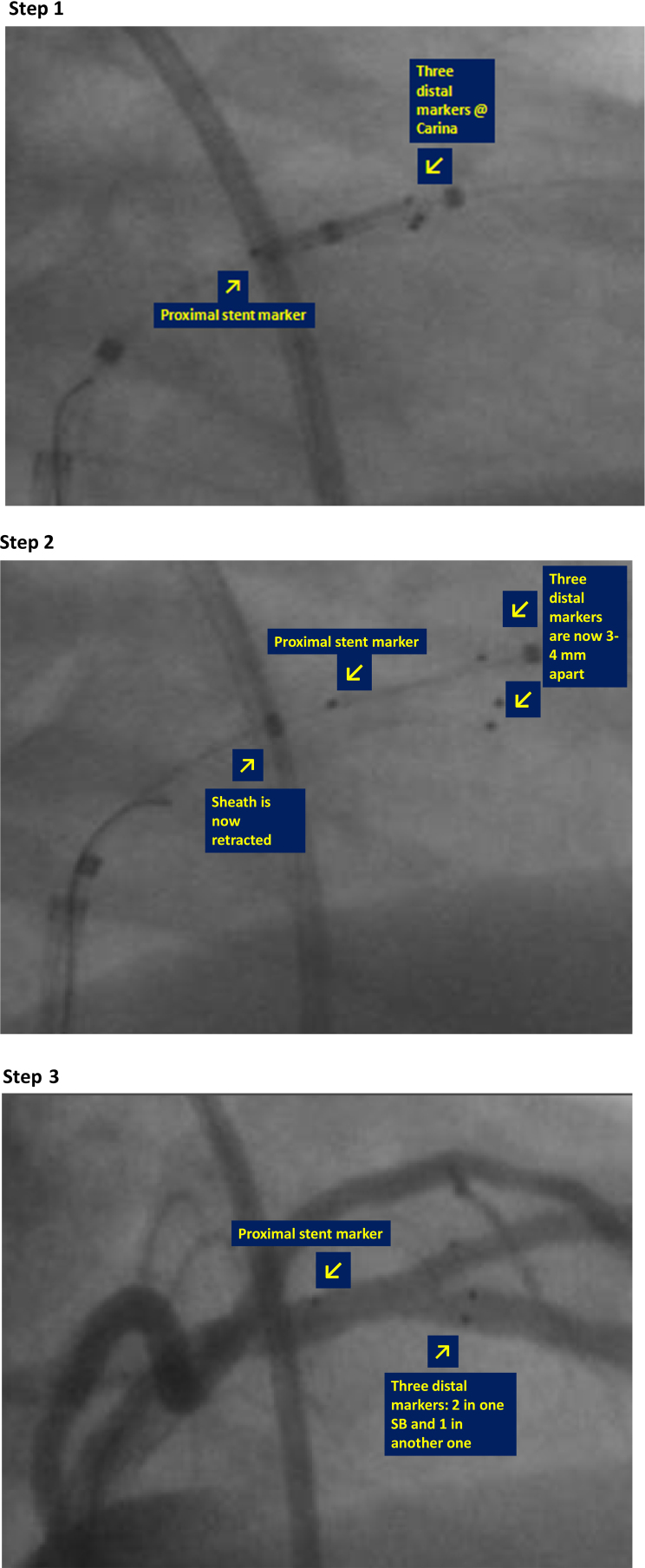
3.8. Deployment sequence
-
1.
Wire both branches of the lesion.
-
2.
Pre-dilate MV, DMV, and the SB to provide space for the self-expanding stent. The stent is inserted in the wire positioned in the most angulated distal branch relative to the proximal segment (or the branch expected to be more difficult to re-wire after Axxess™ stent placement (smaller, dissected or more diseased branch).
-
3.
The delivery system is positioned (kept in place by a covering sheath) just distal to the bifurcation carina by means of distal stent markers, which is clearly visible under fluoroscopy.
-
4.
The removable sheath that covers the Axxess™ stent may be retracted and Axxess™ stent deployment is initiated.
-
5.
The sheath is partially retracted enough to expose the 3 markers (approximately 3 mm).
-
6.
The stent is advanced forward in order to bridge the carina as much as possible.
-
7.
The sheath is fully retracted, and the stent is deployed (Fig. 9).
Fig. 9.
Steps in Axxess™ stent deployment. Step 1: Axxess™ stent positioned and sheath partially retracted (both 1 proximal and 3 distal markers visible); Step 2: Axxess stent advanced (both 1 proximal and 3 distal markers visible; Step 3: Sheath fully retracted and stent deployed. The proximal and distal markers span the extent of stent and position with the vessels.
4. Conclusions
There are several limitations of conventional bifurcation techniques, which range from both anatomic and mechanistic. 1-stent strategy is limited by lack of scaffolding in SB, whereas 2-stent strategy may be limited by the result obtained in MV. Dedicated bifurcation stents offer a logical solution to this problem, but are limited by procedural complexity and the limited choice and sizes of device available.
Conflicts of interest
The authors have none to declare.
References
- 1.Seiler C., Kirkeeide R.L., Gould K.L. Basic structure-function relations of the epicardial coronary vascular tree. Basis of quantitative coronary arteriography for diffuse coronary artery disease. Circulation. 1992;85:1987–2003. doi: 10.1161/01.cir.85.6.1987. [DOI] [PubMed] [Google Scholar]
- 2.Finet G., Gilard M., Perrenot B. Fractal geometry of arterial coronary bifurcations: a quantitative coronary angiography and intravascular ultrasound analysis. EuroIntervention. 2008;3:490–498. doi: 10.4244/eijv3i4a87. [DOI] [PubMed] [Google Scholar]
- 3.Katristis D.G., Ciontis G.C.M., Ioannidis J.P.A. Double versus single stenting for coronary bifurcation lesions: a meta-analysis. Circ Cardiovasc Intervent. 2009;2:409–415. doi: 10.1161/CIRCINTERVENTIONS.109.868091. [DOI] [PubMed] [Google Scholar]
- 4.Movahed M.R. Coronary artery bifurcation lesions: a review and a guide for specific interventional techniques. Iran J Med Sci. 2008;33:187–194. [Google Scholar]
- 5.Steigen T.K., Maeng M., Wiseth R. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006;114:1955–1961. doi: 10.1161/CIRCULATIONAHA.106.664920. [DOI] [PubMed] [Google Scholar]
- 6.Kuchulakanti P.K., Chu W.W., Torguson R. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus- and paclitaxel-eluting stents. Circulation. 2006;113:1108–1113. doi: 10.1161/CIRCULATIONAHA.105.600155. [DOI] [PubMed] [Google Scholar]