Abstract
Objective
To determine the lesion characterization capability by low dose CT for localized lung lesions in comparison with standard dose CT.
Subjects and methods
Approval for this study was granted by our Institutional Review Board. Fifty-two consecutive patients (36 males and 16 females, median age of 71 years.) who had CT examinations for evaluation of lung lesions comprise the study population. Two chest CT scans were performed with current time product of 50 and 150 mAs at 120 kVp, with the same scan length with a 16 detector-row CT scanner. Three readers evaluated 52 target lesions and assigned an overall impression score to each target lesion, using a 5 point scale from 1 (definitely benign) to 5 (definitely malignant). Six features of the lesions including lesion type, margin characteristics, calcification, lobulation, speculation, and pleural indentation were also reported with 5-point scales. The weighted kappa analyses and receiver operating characteristic analysis were used for analysis.
Results
The mean kappa value between low-and standard-dose CT was 0.82 for overall impression of the lesions, showing almost perfect agreement. Area under the curve of low-dose CT (Az = 0.74) had no significant difference from that of standard-dose CT (Az = 0.74) (p = 0.61). The kappa values for six lesion features ranged from 0.45 to 0.83, showing moderate to almost perfect agreement.
Conclusion
Lesion characterization capability by low-dose CT images was comparable to that by standard-dose CT images and therefore sufficient for evaluation of localized lung lesions.
Keywords: Radiation dose reduction, Lung nodules, Lung masses, Chest CT
1. Introduction
Low dose CT examinations are currently employed to detect lung nodules and to find treatable lung cancer cases [1], [2], [3], [4], [5], [6], [7], [8]. Low dose CT is much more effective as a screening process than chest X-ray, but the drawback is that low dose CT examinations uncover many nodules or larger localized lesion which should be differentiated from lung cancers. The nodules or larger localized lesions that are found by low dose screening CT may be further evaluated with standard dose CT, for more detailed assessment of the lesion characteristics. If the lesion was judged to require further follow-up, repeated use of standard dose CT may be needed. Thus, screening for malignant tumor may require additional CT examinations, elevating the cumulative radiation dose to the patient. The repeated use of CT examination is of concern as CT examinations are reportedly significant causes of malignant tumor [9], [10], [11]. If lesion characteristics can be evaluated satisfactorily with low dose CT, low dose CT examinations can be used for initial assessment and follow-up examinations, contributing to reduction of radiation exposure to the patients with localized lung lesions. Comparison of lesion characteristics assessed by readers between low dose CT and standard dose CT may determine whether low dose CT is adequate in these settings.
The purpose of this study is to determine whether low-dose chest CT with 50 mAs can substitute standard-dose chest CT with 150 mAs to evaluate localized lesions and assess the likelihood of malignancy of the lesions.
2. Subjects and methods
Institutional Review Board of the participating institutions approved this study. To build an image database containing localized lung lesions or nodules, patients who were referred for suspected nodular lung lesions or masses were prospectively enrolled in the study. In compliance with the study protocol authorized by the Institutional Review Board, written informed consents were obtained from all patients prior to study participation. Collection and review of the patient data, including medical record and image data, was conducted according to the protocol authorized by the review board.
2.1. Subjects
52 patients with lung nodules or masses participated in the study protocol. After the completion of the enrollment into the study, one of the authors (Y.O.) selected patients with clinical diagnoses of the nodular lung lesions or masses, by reviewing the medical records, the results of the histological examinations and the available chest CT and chest X-ray films, including ones obtained prior to the participation into the study. First, the author identified the lesion for which the patients were referred for diagnosis and treatment. Then the clinical diagnoses of those lesions were determined as follows: if the patient had histologically confirmed diagnosis of that lesion, the clinical diagnosis was the same as histological diagnosis. For lesions without histological diagnoses, when the lesion was followed up for more than 2 years with no growth, the clinical diagnosis of the lesion was benign lesion. Thus, 52 lesions in 52 patients were identified for which the clinical diagnoses of the determined. The patients consist of 36 male and 16 female patients with an age range of 56–84 years (median; 71 years). The body mass indices of the patients range from 14.3 to 35.7 with a mean of 22.8.
2.2. CT examinations
All CT examinations were performed on a 16 detector-row CT scanner (Aquilion 16; Toshiba Medical Systems, Otawara, Tochigi, Japan). The patients who were registered in the study underwent both standard dose CT and low dose CT examinations. Whole chest was scanned with a single breath hold. The two scans had the same craniocaudal coverage and field of view but two different current time product settings (50 mAs and 150 mAs). Other scan parameters were the same for both scans: peak tube voltage of 120 kV, gantry speed of 0.5 s per rotation, slice collimation 0.5 mm × 16, table feed 7.5 mm/rotation, pitch factor 0.94. A series of contiguous 2 mm-thick images was reconstructed from each of two projection data sets (150 mAs and 50 mAs) using a standard lung reconstruction algorithm (FC 51, Fig. 1, Fig. 2, Fig. 3, Fig. 4 ). The images were reconstructed using a three-dimensional adaptive filter (BOOST 3D) to lessen the streak artifacts which tend to be prominent especially in low dose CT images [12], [13], [14].
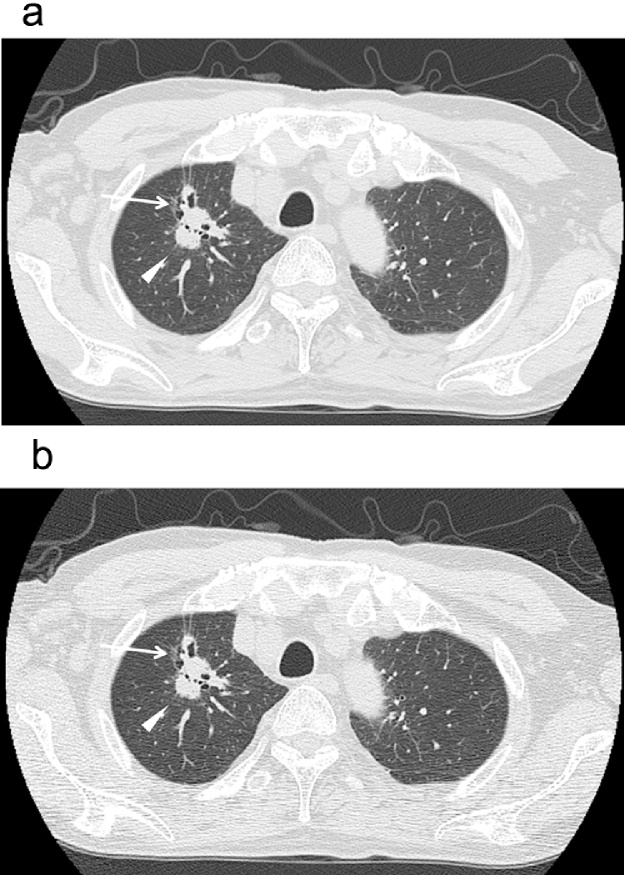
Fig. 1.
(a, standard dose image; b, low dose image) 75 year-old-male (body weight 46 kg) who had a chest CT examination for a suspected lung tumor in the right upper lobe. Visualization of a tumor with partially irregular margin and spicula (arrow) is clear in both images.
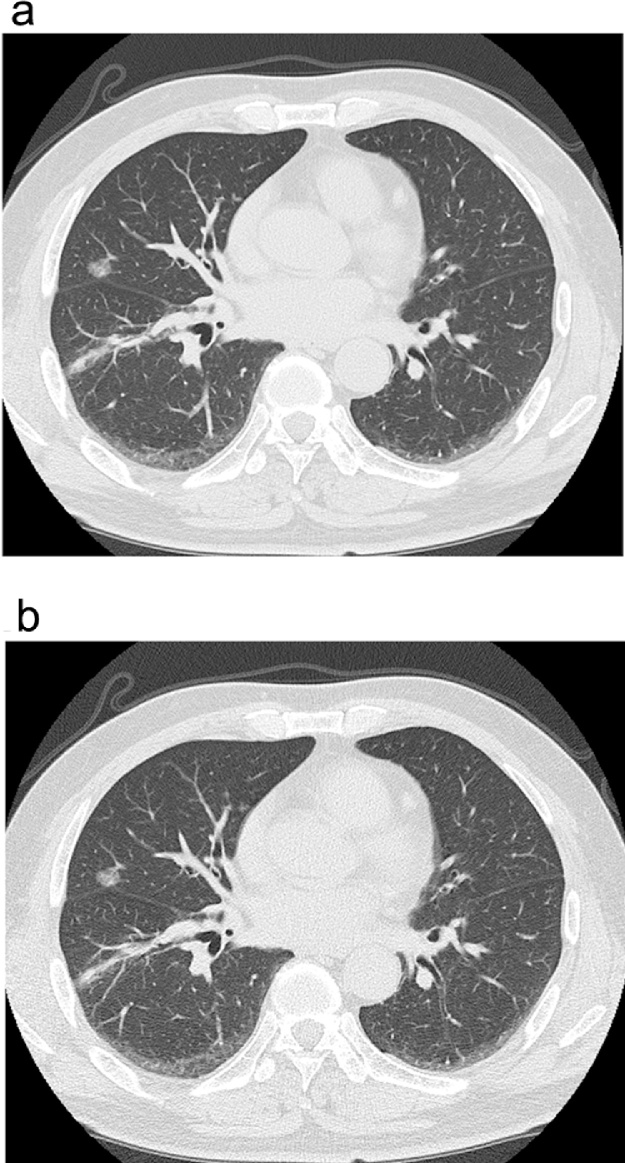
Fig. 2.
(a, standard dose image; b, low dose image) 69 year old male (body weight 56 kg) who underwent preoperative CT examination for a lung tumor in the right upper lobe. Peripheral ground-glass opacity (arrow) and spicula (arrowhead) are appreciated clearly in both low dose and standard dose images.
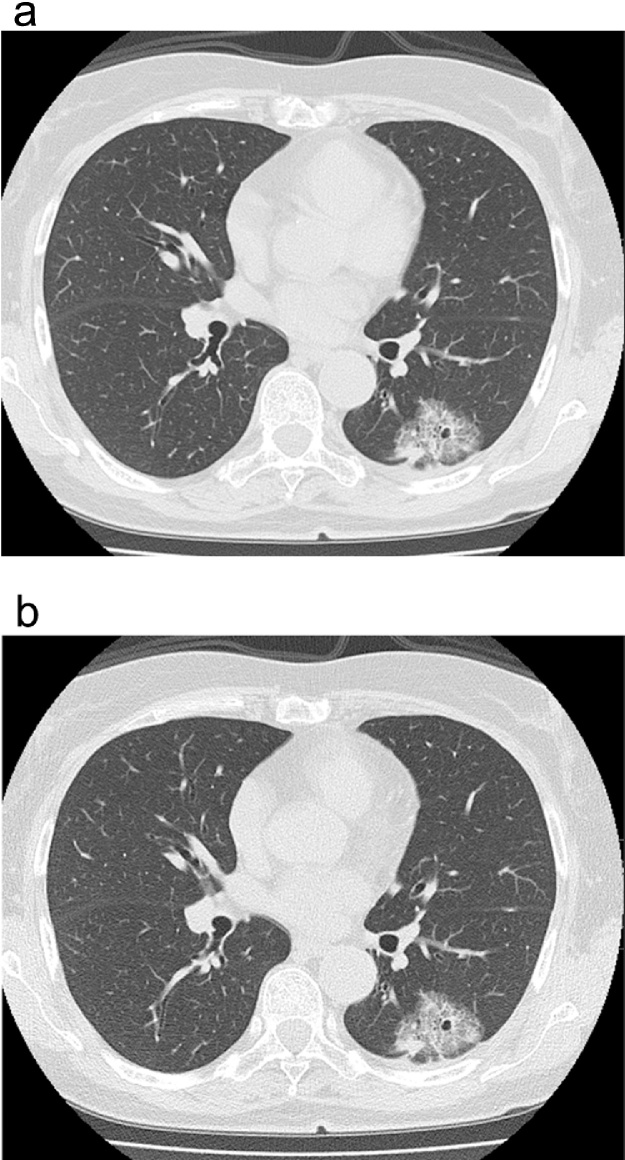
Fig. 3.
(a, standard dose image; b, low dose image) 67 year-old male (body weight 77 kg) who had a chest CT examination for evaluation of a suspected nodule in the right middle lobe which turned out to be lung cancer. A well-demarcated ground-glass nodule is finely visualized with vascular structures inside the nodule.
Fig. 4.
(a, standard dose image; b, low dose image) 67 year-old female (body weight 55 kg) who had a chest CT examination for evaluation of a suspected mass in the left lower lobe. A mixed ground-glass nodule with internal web-like structures is equally visualized in both images. The tumor was removed surgically and confirmed to be a lung cancer.
2.3. Image analysis
To assess the lesion characterization capability of low dose CT and determine the feasibility of substituting low-dose CT for standard-dose CT, comparison of low dose images and standard dose images was conducted in two ways: (1) the readers’ overall impressions of the lesions (the likelihood of malignant or benign) were compared between low dose CT and standard dose CT protocols and (2) the individual CT features of the lesions that were identified by the readers were compared between low dose CT and standard dose CT protocols.
One of the authors (Y.O.), who selected the eligible study subjects, reviewed all the images acquired for the study to identify the target lesion for which the clinical diagnoses were made. One target lesion was determined for each patient. The author compiled a list of target lesions to be analyzed by readers. The target lesions ranged from 7 to 82 mm in diameter, with mean diameter of 28 mm. There are 104 (52 × 2) target lesions, each of 52 unique lesions being imaged with both standard-dose and low-dose methods. All 104 images containing target lesions were presented to three board-certified chest radiologists (H.H., H.K. and N.M.)for evaluation. Readers were offered a list of the locations of target lesions on 104 image series, so that all readers can correctly identify the same target lesion in a given patient. The radiologists were not working at the site of patient enrollment were selected as readers for unbiased interpretation of images. The readers have more than 10 years of experience as thoracic radiologists. The images were anonymized and presented in a random order and readers were not informed of scan protocol of individual image series. The evaluation was made on the diagnostic grade LCD monitors of a picture archiving and communications systems viewer (TPC-7200G3, Toshiba Medical Systems). The readers evaluated images with fixed window settings (lung, window level/width = −500/1500; soft tissue = 50/350).
First, readers looked at the designated target lesion on the list to assess the features of the lesions. Correct identification of target lesions by the individual readers was confirmed on site by one of the authors (Y.O.) who prepared the list of analyzable lesions. The type of the lesion was reported with a 5-point score (1, purely ground-glass attenuation lesion; 2, predominantly ground-glass attenuation lesion; 3, mixed solid and ground-glass attenuation lesion; 4, predominantly solid lesion; 5, purely solid lesion). The readers also reported conspicuity of selected CT findings of the lesions to assess the consistency CT feature recognition by the readers. The readers reported with a 5-point lesion feature scores the conspicuity of the five commonly-used CT lesion features including (1) margin characteristics, (2) calcification, (3) lobulation, (4) spiculation and (5) pleural indentation. The scoring criteria for CT features are shown in Table 1. The readers evaluated these CT features independently. Then, the readers independently reported an overall impression on the lesion characteristics (i.e., the likelihood of being a benign or a malignant lesion). The overall impression scores were assigned using a 5 point scale (1, definitely benign; 2, probably benign; 3, equivocal; 4, probably malignant; 5, definitely malignant).
Table 1.
The scoring criteria for individual CT features of the target lesions.
| CT features |
||||
|---|---|---|---|---|
| Lesion type | Margin characteristics | Calcification | Lobulation, Spiculation Pleural indentation | |
| 5 | Solid | Unclear | Absent | Definitely present |
| 4 | Predominantly solid | Probably unclear | Probably absent | Probably present |
| 3 | Mixed solid and GGA | Equivocal | Equivocal | Equivocal |
| 2 | Predominantly GGA | Probably clear | Probably present | Probably absent |
| 1 | Pure GGA | Clear | Present | Definitely absent |
GGA, ground-glass attenuation.
2.4. Statistical analysis
The consistency of lesion characterization by the readers was assessed by comparing overall impression scores between low dose CT and standard dose CT images using McNemar's test and weighted kappa analysis. Then, receiver operating characteristic (ROC) analysis was performed to compare diagnostic capabilities of both protocols. Fifty two overall impression scores by individual readers (1–5) were transformed into binary predictions (suspected benign lesion or suspected malignant lesion). For example, if the threshold of binary transformation is between 2 and 3, scores of 1 and 2 mean “suspected benign” prediction, while scores of 3, 4 and 5 mean “suspected malignant” prediction. This binary predictions were produced with variable threshold T (T < 1, 1 <T < 2, 2 < T <3, 3 < T < 4, 4 < T < 5, 5 < T) and the sensitivity and specificity values of readers' predictions were calculated for each threshold. A receiver operating characteristic curve was drawn and the area under the ROC curve (AUC) was calculated and the difference in AUC was analyzed. To determine the consistency of CT features judged by the observers, the intraobserver agreement (between low dose and standard dose images by the same observer) and interobserver agreement (among three observers with the same mAs setting) were tested with weighted kappa analysis. A personal computer software program (LABMRMC; Charles E. Metz, University of Chicago) was used in the ROC analysis. Other data analysis was performed using SAS software (SAS Institute Inc., Cary, NC). When the kappa value was <0.00, 0.00–0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, and 0.81–1.00, the strength of agreement was judged as poor, slight, fair, moderate, substantial, and almost perfect, respectively. A p-value of less than 0.05 was considered significant for other statistical tests.
3. Results
3.1. Overall impression scores
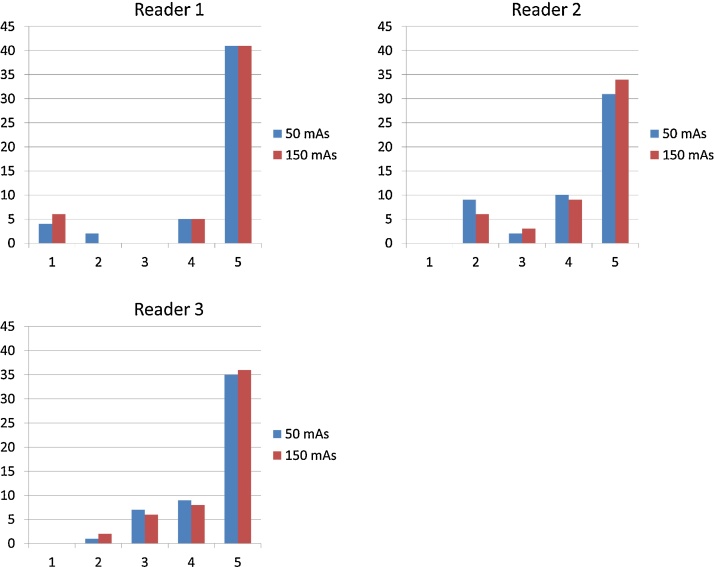
The overall impression scores assigned by the individual readers are summarized in Fig. 5. The result of McNemar's test showed that there is no significant difference in the distribution of scores assigned by the readers between low dose images and standard dose images (p > 0.05).
Fig. 5.
Overall impression scores assigned on low dose images and standard dose images by reader 1, 2 and 3.
The kappa values for intraobserver agreement between low-dose images and standard-dose images were 0.92, 0.63 and 0.90 for observer 1, 2 and 3, respectively, with an average of 0.82. The kappa values for 50 mAs images between reader 1 and reader 2, reader 2 and reader 3, reader 1 and reader 3 were 0.49, 0.52 and 0.37, respectively, with an average kappa value of 0.46. The kappa values for 150 mAs images between reader 1 and reader 2, reader 2 and reader 3, reader 1 and reader 3 were 0.45, 0.49 and 0.50, respectively, with an average kappa value of 0.48.
The ROC curve of the readers were shown in Fig. 6, showing the reader's performance of lesion characterization using 150 mAs images and 50 mAs images. Area under the curve of low-dose CT (Az = 0.74) had no significant difference from that of standard-dose CT (Az = 0.74) (p = 0.61).
Fig. 6.
Receiver operating characteristic (ROC) curves of the lesion characterization (benign vs. malignant) for three readers. Solid lines represent the curves for 50 mAs images and broken lines represent the curves for 150 mAs images. No significant difference was found in area under the curve (AUC) between 50 mAs and 150 mAs images.
3.2. CT features of the lesions
The CT feature scores are shown in Table 2. The kappa values for intraobserver agreement between low dose CT and standard dose CT on individual lesion feature scores were shown in Table 3. The kappa values for interobserver agreement of these lesion feature scores were shown in Table 4.
Table 2.
The numbers of CT feature scores assigned by three readers.
| Lesion feature scores |
||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Lesion type | 50 mAs | 8 | 10 | 15 | 22 | 101 |
| 150 mAs | 8 | 5 | 16 | 26 | 101 | |
| Margin characteristics | 50 mAs | 10 | 32 | 0 | 47 | 67 |
| 150 mAs | 11 | 40 | 3 | 43 | 59 | |
| Calcification | 50 mAs | 21 | 23 | 14 | 6 | 92 |
| 150 mAs | 33 | 9 | 3 | 11 | 100 | |
| Lobulation | 50 mAs | 5 | 13 | 3 | 21 | 114 |
| 150 mAs | 5 | 7 | 0 | 28 | 116 | |
| Spiculation | 50 mAs | 13 | 17 | 4 | 25 | 97 |
| 150 mAs | 15 | 15 | 1 | 22 | 103 | |
| Pleural indentation | 50 mAs | 24 | 11 | 1 | 20 | 100 |
| 150 mAs | 25 | 4 | 2 | 23 | 102 | |
Table 3.
The kappa values for intraobserver agreement between low- and standard-dose CT on individual lesion feature scores.
| Reader |
||||
|---|---|---|---|---|
| 1 | 2 | 3 | Average | |
| Type | 0.86 | 0.83 | 0.80 | 0.83 |
| Margin characteristics | 0.51 | 0.37 | 0.45 | 0.45 |
| Calcification | 0.69 | 0.17 | 0.72 | 0.47 |
| Lobulation | 0.63 | 0.38 | 0.67 | 0.58 |
| Spiculation | 0.74 | 0.65 | 0.64 | 0.70 |
| Pleural indentation | 0.87 | 0.82 | 0.67 | 0.83 |
Table 4.
The kappa values for interobserver agreement between low- and standard-dose CT on individual lesion feature scores.
| r1-r2 | r2-r3 | r3-r1 | Mean | ||
|---|---|---|---|---|---|
| Type | 50 mAs | 0.67 | 0.72 | 0.78 | 0.72 |
| 150 mAs | 0.66 | 0.78 | 0.67 | 0.70 | |
| Margin characteristics | 50 mAs | 0.36 | 0.34 | 0.45 | 0.38 |
| 150 mAs | 0.15 | 0.34 | 0.24 | 0.25 | |
| Calcification | 50 mAs | 0.11 | 0.23 | 0.49 | 0.28 |
| 150 mAs | 0.37 | 0.74 | 0.49 | 0.53 | |
| Lobulation | 50 mAs | 0.44 | 0.34 | 0.44 | 0.41 |
| 150 mAs | 0.41 | 0.40 | 0.32 | 0.37 | |
| Spiculation | 50 mAs | 0.28 | 0.41 | 0.27 | 0.32 |
| 150 mAs | 0.42 | 0.28 | 0.58 | 0.43 | |
| Pleural indentation | 50 mAs | 0.59 | 0.48 | 0.41 | 0.49 |
| 150 mAs | 0.59 | 0.53 | 0.61 | 0.58 |
r1-r2, Between reader 1 and 2; r2-r3, between reader 2 and 3; r3-r1, between reader 3 and 1.
4. Discussion
The current study showed that diagnostic performance and characterization capability of the low-dose images were comparable to that of standard dose images. In consideration of risk related to medical radiation exposure, radiation dose to the patient should be kept as low as possible while securing the diagnostic image quality needed in patient care. Practice of low dose CT has been investigated in an effort to minimize the patient risk [15]. The application of low dose CT technique has been facilitated by various techniques, including automatic exposure systems and imaging filters [13], [14], [16], [17], [18], [19], [20]. As chest CT examinations are frequently used for lung lesion detection, detection of lung nodules using low dose CT images has been investigated by several groups [1], [2], [3], [4], [5], [21]. These results showed that detection of pulmonary nodules is possible with low dose CT images obtained with 20–50 mAs. When pulmonary nodules or masses are discovered on low dose CT images, a question arises whether additional standard dose CT examinations are needed to properly assess the likelihood of malignancy of the lesion, which has not been addressed so far. If we can confidently rely on low dose CT to make a decision on the management of the patient, without making additional radiation exposure to the patient by having another CT examination with higher mAs setting, it will spare CT examinations and radiation exposure. Moreover, the follow-up CT examinations are possible with low dose CT scans, contributing the reduction of radiation exposure to the patients. On the other hand, a possible adverse effect of the radiation dose reduction would include failed or erroneous recognition of those CT features are essential for correct CT characterization. Incorrectly identified CT features of the lesion could affect the management of patients who have lesions suspicious of lung cancer: lung cancers would be left untreated on the wrong assumption of benignity, or benign nodules could be overtreated as suspected lung cancers. Therefore, clarification of diagnostic accuracy in lesion characterization of low dose CT in comparison with standard dose CT will help reduce radiation exposure from CT examinations.
The result of the current study showed that low dose CT images have lesion characterization capability comparable to that of standard dose CT images. Comparison of overall impression scores revealed no significant scoring difference between low dose CT and standard dose CT images. The agreement of individual readers between low dose CT impression scores and standard dose CT impression scores was almost perfect, substantial and almost perfect for reader 1–3, respectively, while the interobserver agreement was moderate, except for the fair agreement (kappa = 0.37) between reader 1 and 2 on 50 mAs images. At the same time, ROC analysis showed no significant difference in diagnostic performance between low dose CT images and standard dose CT images.
Our results suggest that the low dose CT is an adequate initial decision tool for lung cancers. The decisions on the lesion found at low dose CT images are as reliable as those made on standard dose CT images. If the lesions are likely to be benign, the lesion does not need additional standard CT examination for better visualization. For selected cases where lung cancer is strongly suspected, standard dose CT examinations, preferably with intravenous contrast, may be appropriate to examine the findings in the hilum and mediastinum. The result also indicates that low dose CT exams are adequate tool for follow up examinations because the nodule characteristics can be appreciated properly with low dose CT images. The use of standard dose CT for follow-up examinations may be unnecessary. This study showed that radiation dose reduction is possible both in screening and follow-up settings, contributing wise use of reduced dose CT examinations to improve patient safety.
Comparison of individual CT feature scores also demonstrated high degree of agreement between low dose CT and standard dose CT images. Agreement in lesion type and pleural indentation was almost perfect, with a mean kappa value more than 0.80. Correlation of scores was substantial for the presence or absence of spiculation. Other CT feature scores, lobulation, calcification and margin characteristics had lower kappa scores, average kappa value ranging from 0.45 to 0.58, the agreement of scores being moderate.
The study showed lower agreement rate in the detection of calcification, being 0.17 for one of the readers. A possible explanation for this low agreement rate is that artifactual high CT value pixels could simulate microcalcifications. Lung images are reconstructed with high-frequency reconstruction algorithms and objects tend to be encircled with pixels with high CT values due to edge enhancement. This effect occasionally adds seemingly high-dense spots in the lesions, especially when the image is contaminated with heavy spotty noises as in low dose images. Hence, exclusive use of lung images in this study could be responsible for this lower rate of agreement on calcification assessment. If soft tissue images were also available for review at the time of the reading experiment, the inconsistent recognition of calcification could be avoided. Despite lower score agreement regarding some CT features including margin characteristics, calcification and lobulation, the overall impression of the lesion made by the radiologists was highly consistent, with almost equal receiver operation curve characteristics. The present study showed that radiation dose reduction did not affect lesion characterization capability despite the image quality degradation.
The current study has a couple of limitations. First, majority of lesions that are included in this study are relatively large (>2 cm), mostly solid. Diagnostic accuracy of smaller nodules (e.g. <10 mm) or nodules showing ground-glass attenuation by low dose CT is not fully evaluated in this study. Dedicated study may be needed that focuses on micronodules or nodules of ground glass attenuation. Second, only lung images were prepared and analyzed in this study. It is true that findings in the hilum and mediastinum, especially lymphadenopathy, may contribute to better characterization of the lesion. Lymphadenopathy will be visualized more clearly with standard dose CT. The effect of radiation dose on mediastinal structures are not assessed in this study. Lastly, scans were performed with a fixed mAs value in this study without automatic exposure control system. Automatic exposure control system has been reported to be effective in radiation dose reduction [16], [17], [18], [19]. If the study was performed with automatic exposure control system activated for images of adequate image quality, the radiation exposure will be lowered further and CT characteristics of the lesions may be more consistently identified by preventing image quality degradation in areas with high image noise level.
The result of this study shows that low-dose CT images acquired with current time product of 50 mAs offers the tumor characterization capability comparable to that of standard-dose CT images. Low dose chest CT protocol at 50 mAs may be substituted for standard dose CT with 150 mAs, not only for the detection of lesion, but also characterization of the lesion necessary for the management decision. Therefore, additional standard-dose CT examination is not recommended for patients that presented with lung nodules detected by low-dose CT examination. Use of low dose protocol contributes to substantial dose sparing for patient who has indeterminate lung lesions.
In conclusion, low-dose CT images acquired with current time product of 50 mAs offers diagnostic performance and lesion characterization capability comparable to that of standard-dose CT images and consequently can substitute standard-dose CT with 150 mAs for diagnostic evaluation of lung lesions.
Funding
The study was supported by a research grant from Toshiba Medical Systems Corporation. Toshiba Medical Systems Corporation helped organize The International Multicenter Study for Low-Dose Chest CT Examination and Diagnosis (iLEAD) and provided technical support in preparation of reading experiment for this study.
Acknowledgments
iLEAD (International multi-center study for Low dose chest CT Examination And Diagnosis) is a study project dedicated to the investigation of radiation dose reduction in chest CT examinations. Three institutions participates this study group (Beth Israel Deaconess Medical Center, Boston, USA; German Cancer Research Center, Heidelberg, Germany and Kobe University, Kobe, Japan). The iLEAD study group consists of Takeshi Kubo, Boston, MA; Yoshiharu Ohno, Kobe, Japan; Shiva Gautam, Boston, MA; Pei-Jan P. Lin, Boston, MA; Masaya Takahashi, Boston, MA; Mizuki Nishino, Boston, MA; Arkadiusz Sitek, Boston, MA; Daisuke Takenaka, Kobe, Japan; Munenobu Nogami, Kobe, Japan; Hisanobu Koyama, Kobe, Japan; Julia Ley-Zaporozhan, Heidelberg, Germany; Wolfram Stiller, Heidelberg, Germany; Sebastian Ley, Heidelberg, Germany; Hiroyasu Inokawa, Tochigi, Japan; Yasuko Fujisawa, Tochigi, Japan; Hiroyuki Kura, Tochigi, Japan; Vassilios Raptopoulos, Boston, MA; Kazuro Sugimura, Kobe, Japan; Hans-Ulrich Kauczor, Heidelberg, Germany; and Hiroto Hatabu, Boston, MA.
The authors express gratitude to Alba Cid for editorial assistance.
Footnotes
The study was supported by a research grant from Toshiba Medical Systems Corporation.
References
- 1.Rusinek H., Naidich D.P., McGuinness G. Pulmonary nodule detection: low-dose versus conventional CT. Radiology. 1998;209:243–249. doi: 10.1148/radiology.209.1.9769838. [DOI] [PubMed] [Google Scholar]
- 2.Gartenschlager M., Schweden F., Gast K. Pulmonary nodules: detection with low-dose vs conventional-dose spiral CT. Eur. Radiol. 1998;8:609–614. doi: 10.1007/s003300050445. [DOI] [PubMed] [Google Scholar]
- 3.Diederich S., Lenzen H., Windmann R. Pulmonary nodules: experimental and clinical studies at low-dose CT. Radiology. 1999;213:289–298. doi: 10.1148/radiology.213.1.r99oc29289. [DOI] [PubMed] [Google Scholar]
- 4.Karabulut N., Toru M., Gelebek V., Gulsun M., Ariyurek O.M. Comparison of low-dose and standard-dose helical CT in the evaluation of pulmonary nodules. Eur. Radiol. 2002;12(11):2764–2769. doi: 10.1007/s00330-002-1368-4. [DOI] [PubMed] [Google Scholar]
- 5.Hetmaniak Y., Bard J.J., Albuisson E. Pulmonary nodules: dosimetric and clinical studies at low dose multidetector CT. J. Radiol. 2003;84:399–404. [PubMed] [Google Scholar]
- 6.O'Connor G.T., Hatabu H. Lung cancer screening, radiation, risks, benefits, and uncertainty. JAMA. 2012;307(22):2434–2435. doi: 10.1001/jama.2012.6096. [DOI] [PubMed] [Google Scholar]
- 7.National Lung Screening Trial Research Team Aberle, Adams A.M., Aberle D.R. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Lung Screening Trial Research Team Church T.R., Black W.C. Results of initial low-dose computed tomographic screening for lung cancer. N. Engl. J. Med. 2013;368(21):1980–1991. doi: 10.1056/NEJMoa1209120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brenner DJ, Estimating cancer risks from pediatric CT: going from the qualitative to the quantitative. Pediatr. Radiol. 2002;32(4):242–244. doi: 10.1007/s00247-002-0671-1. (228,1; discussion) [DOI] [PubMed] [Google Scholar]
- 10.Brenner D.J., Hall E.J. Computed tomography–an increasing source of radiation exposure. N. Engl. J. Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 11.Berrington dG. Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345–351. doi: 10.1016/S0140-6736(04)15433-0. [DOI] [PubMed] [Google Scholar]
- 12.Kazama M., Tsukagoshi S., Okumura M. Image quality improvement and exposure dose reduction with the combined use of X-ray modulation and Boost3D. Proc. SPIE Int. Soc. Opt. Eng. 2006;6142:847–855. [Google Scholar]
- 13.Kubo T., Nishino M., Kino A. 3-Dimensional adaptive raw-Data filter: evaluation in low dose chest multidetector-Row computed tomography. J. Comput. Assist. Tomogr. 2006;30(6):933–938. doi: 10.1097/01.rct.0000221951.60393.64. [DOI] [PubMed] [Google Scholar]
- 14.Kubo T., Ohno Y., Gautam S. Use of 3D adaptive raw-data filter in CT of the lung: effect on radiation dose reduction. AJR Am. J. Roentgenol. 2008;191(4):1071. doi: 10.2214/AJR/07.2630. [DOI] [PubMed] [Google Scholar]
- 15.Kubo T., Lin P.J., Stiller W. Radiation dose reduction in chest CT: a review. AJR Am. J. Roentgenol. 2008;190(2):335–343. doi: 10.2214/AJR.07.2556. [DOI] [PubMed] [Google Scholar]
- 16.Greess H., Nomayr A., Wolf H. Dose reduction in CT examination of children by an attenuation-based on-line modulation of tube current (CARE dose) Eur. Radiol. 2002;12:1571–1576. doi: 10.1007/s00330-001-1255-4. [DOI] [PubMed] [Google Scholar]
- 17.Kalra M.K., Maher M.M., Toth T.L. Techniques and applications of automatic tube current modulation for CT. Radiology. 2004;233(3):649–657. doi: 10.1148/radiol.2333031150. [DOI] [PubMed] [Google Scholar]
- 18.Mulkens T.H., Bellinck P., Baeyaert M. Use of an automatic exposure control mechanism for dose optimization in multi-detector row CT examinations: clinical evaluation. Radiology. 2005;237(1):213–223. doi: 10.1148/radiol.2363041220. [DOI] [PubMed] [Google Scholar]
- 19.Kalra M.K., Rizzo S., Maher M.M. Chest CT performed with z-axis modulation: scanning protocol and radiation dose. Radiology. 2005;237:303–308. doi: 10.1148/radiol.2371041227. [DOI] [PubMed] [Google Scholar]
- 20.Kubo T., Ohno Y., Kauczor H.U., Hatabu H. Radiation dose reduction in chest CT-review of available options. Eur. J. Radiol. 2014;83(10):1953–1961. doi: 10.1016/j.ejrad.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 21.Funama Y., Awai K., Liu D. Detection of nodules showing ground-glass opacity in the lungs at low-dose multidetector computed tomography: phantom and clinical study. J. Comput. Assist. Tomogr. 2009;33(1):49–53. doi: 10.1097/RCT.0b013e31815e6291. [DOI] [PubMed] [Google Scholar]