Highlights
-
•
We planned to confirm the efficiency of low dose CT protocol at 50 mAs as a routine protocol.
-
•
We examined the difference in the diagnostic result between the low dose CT images and standard dose CT image protocol.
-
•
Fundamental chest CT abnormal findings including both lung and soft tissue abnormality were recorded and compared between two protocols.
-
•
The difference in the diagnostic result of a reader from the other two readers is not greater in low dose CT images.
-
•
The result of present study supported the use of routine low dose CT protocol.
Keywords: Radiation dose reduction, Chest CT, Diagnostic accuracy
Abstract
Purpose
To determine the diagnostic capability of low-dose CT (50 mAs) in comparison to standard-dose CT (150 mAs).
Materials and methods
Fifty-nine consecutive patients underwent two non-contrast chest CT scans with different current-time products (50 and 150 mAs at 120 kVp) on a 64-detector row CT scanner. Three board certified chest radiologists independently reviewed 118 series of 2 mm-thick images (2 series for each of 59 patients) in a random order. The readers assessed abnormal findings including emphysema, ground-glass opacity, reticular opacity, micronodules, bronchiectasis, honeycomb, nodules (>5 mm), aortic aneurysm, coronary artery calcification, pericardial and pleural effusion, pleural thickening, mediastinal tumor and lymph node enlargement. Five-point scale from 1 (definitely absent) to 5 (definitely present) was used to record the results. The rates of score agreement between two images were calculated. Deviation of one observer's score from other two observers was compared between low dose CT and standard dose CT.
Results
Mean agreement rate of the lung parenchymal findings between low dose CT and standard dose CT images was 0.836 (range, 0.746–0.926). Mean agreement rates for mediastinal and pleural findings were 0.920 (range, 0.735–1.000). There was no statistically significant difference in the deviation of the observers' scores between low-dose CT and standard-dose CT.
Conclusion
Low dose CT protocol at 50 mAs can produce the screening results consistent with standard dose CT protocol (150 mAs), supporting routine use of low dose chest CT protocol.
1. Introduction
There is an increasing awareness of the possible adverse effects of diagnostic radiation exposure to the patients, because the medical radiation exposure has grown significantly as we utilize medical imaging more often. CT examinations account for majority of radiation exposure related to medical imaging [1], [2]. Considering the possible adverse effect, the practice of keeping radiation dose as low as reasonably possible (ARALA principle) should be observed in medical imaging involving ionizing radiation.
As CT is a major cause of radiation exposure buildup, low dose CT techniques is advisable unless it affects management decision. However, replacing a conventional chest CT routine protocol with a low-dose protocol is not a simple task, mainly because of the concern that the image quality degradation might make the correct recognition of findings difficult and consequently influence the diagnostic conclusion. Although there are several studies that assess the efficacy of low-dose CT protocols for various purposes, the evidence that standard-dose CT protocols can be routinely substituted for by low-dose CT is lacking [3], [4], [5]. To facilitate the use of low dose chest CT, adequacy of a low dose CT protocol as a routine protocol needs to be confirmed. Direct comparison of the detection rate of several basic lung abnormalities between the low dose CT and standard dose CT will provide the useful data regarding the diagnostic accuracy of low dose CT examinations.
The purpose of this study is to determine whether it is reasonable to accept a 50 mAs chest CT protocol as a routine protocol for general purposes.
2. Materials and methods
2.1. Study approval
Approval for this study was granted by our Institutional Review Board. The data collection and review of the medical record and image data, was conducted according to the protocol that is authorized by the review board.
2.2. Study subjects
59 consecutive patients who underwent non-contrast chest CT were prospectively enrolled in the study. The patients less than 50 years old were excluded, as cancer risk related to ionizing radiation exposure is relatively high in younger population.
The patient enrollment was conducted, in compliance with the study protocol authorized by the Institutional Review Board. One of the authors (TK) explained the purpose of the study and the risk that may be associated with participation of the study to all subject candidates in the study. The patients had opportunity to read a document on detailed study plan. They were informed of their rights to opting out from the study without any possible disadvantage in their care. A written informed consent form signed by the subject was obtained from all patients who agreed to take part in the study.
2.3. Study population
The subjects who opted to participate in the study consists of 51 white Americans, four Asian Americans, two African Americans, two Hispanic Americans. The subjects consist of 32 female and 27 male patients with a mean age of 69.6 years. The body weight of the patients was 75.6 ± 19.7 (mean ± SD). The body mass index of the patient was 27.3 ± 6.9 (mean ± SD), ranging from 15.5 to 46.2. The study population included 35 smokers. The patients had an average of 17.3 pack-year (range, 0–90) history of smoking.
The patients underwent CT examinations for the evaluation of known lung nodules (22 patients), evaluation of suspected lung lesion(s) discovered on chest X-ray (17 patients), interstitial lung disease (5 patients), suspected pleural or pericardial abnormalities (4 patients), screening for lung lesion (4 patients), evaluation of pneumonia (3 patients) and other miscellaneous reasons (4 patients).
2.4. CT scanning protocols
All CT examinations were performed on a 64 detector-row CT scanner (Aquilion 64; Toshiba Medical Systems, Otawara, Tochigi, Japan). Patients participating in this study underwent two helical scans successively. Each scan was performed with a single breath hold using the same scan parameter, except for mAs settings (50 mAs for low-dose scan and 150 mAs for standard-dose scan). Other scan parameters were the same for both scans: peak tube voltage of 120 kV, gantry speed of 0.5 s per rotation, slice collimation 0.5 mm × 64, table feed 53 mm/s, pitch factor 0.828. Weighted CT dose index (CTDIw) was measured for axial scanning (64 × 0.5 mm detector configuration), using 32 cm acrylic dosimetry phantom and 100 mm ionization chamber.
2.5. Image preparation
A series of contiguous 2 mm-thick images was reconstructed from each of two raw data sets (150 mAs and 50 mAs) using a standard lung reconstruction algorithm (FC 51, Fig. 1). The images were anonymized by removing all the patient-specific data. The scan parameters were deleted from DICOM files for blind interpretation using PACS (Picture Archiving and Communication Systems) viewers. 118 image series, consisting of 59 low dose images and the same number of standard dose images were arranged in a random order. The representative images are presented in Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5 .
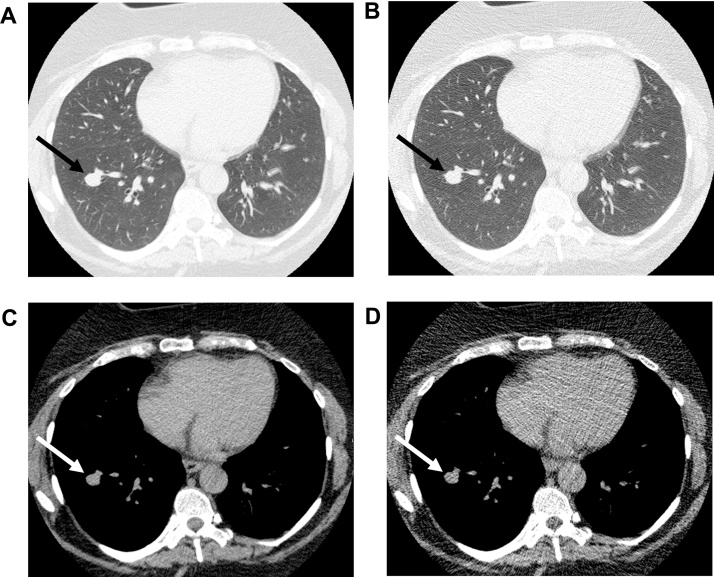
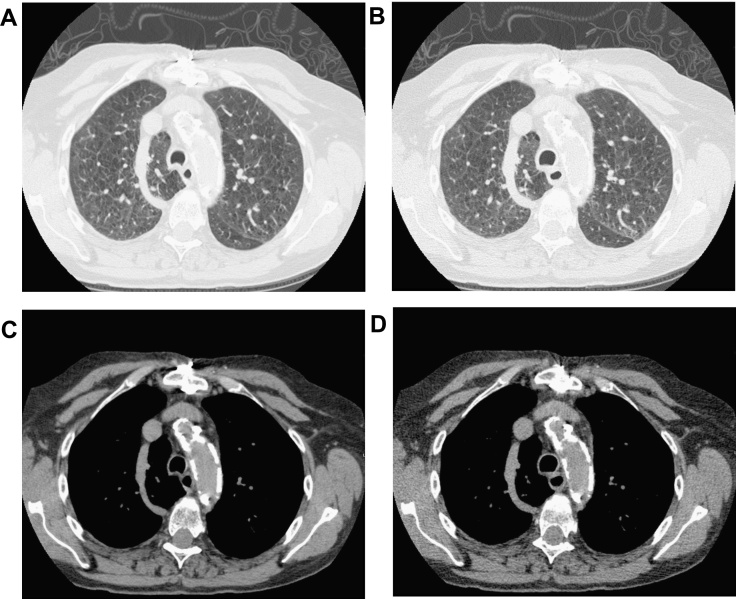
Fig. 1.
(a and c, standard dose images; b and d, low dose images) 57 year-old female (body weight 120 kg) who underwent chest CT for a follow-up of solitary pulmonary nodule in the right lower lobe. The nodule appears as an oval smoothly marginated nodule on both standard dose CT image and low dose CT image (arrow).
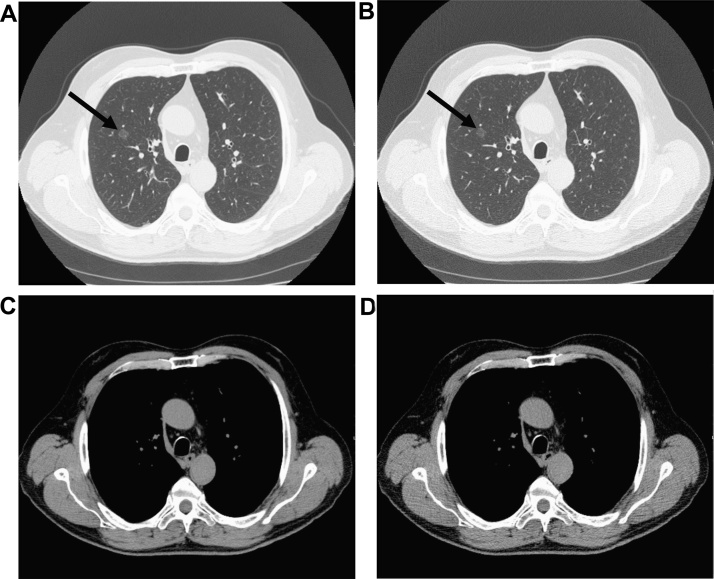
Fig. 2.
(a and c, standard dose images; b and d, low dose images) 76 year-old male (body weight 73 kg) who underwent chest CT as a follow-up study for a ground-glass pulmonary nodule. A purely ground-glass nodule in right upper lobe was clearly visualized both with standard dose CT and low dose CT (arrow).
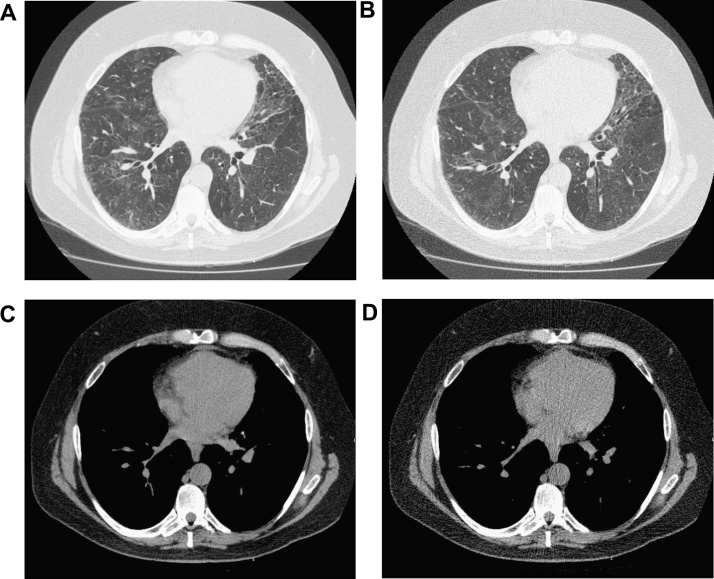
Fig. 3.
(a and c, standard dose images; b and d, low dose images) 53 year-old male (body weight 86 kg) who underwent chest CT as a follow-up study for ground-glass opacity in both lungs. The difference in the lung parenchymal opacity can be recognized with a well-defined border between the ground-glass area and the normal-appearing area (arrows).
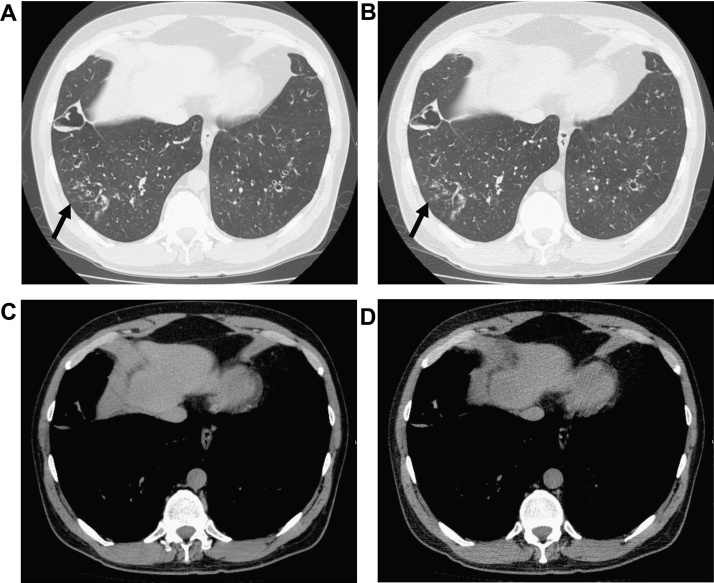
Fig. 4.
(a and c, standard dose images; b and d, low dose images) 51 year-old male (body weight 91 kg) who underwent chest CT for suspected bronchiectasis and bronchial wall thickening. Bronchiectasis, bronchial wall thickening and centrilobular nodules are clearly visualized both with standard dose CT and low dose CT.
Fig. 5.
(a and c, standard dose images; b and d, low dose images) 77 year-old female (body weight 53 kg) who had chest CT for suspected interstitial pneumonia. Mosaic attenuation and thickening of interlobular septa is visible with low dose CT as well as with standard dose CT. On soft tissue images, aortic calcification was well visualized equally in two images.
2.6. Image interpretation
The CT image data were interpreted by three readers (Y.O., K.H and H.H.) who have more than ten years’ experience as thoracic radiologists in there different countries (Germany, Japan and united states of America). The 118 image series were presented to the readers in a random order and the readers were blinded to the patient information and scan parameters which they interpreted. The images were viewed on a PACS viewer (TPC-7200G3, Toshiba Medical Systems, Otawara, Tochigi, Japan). The presence or absence of abnormal CT findings were recorded using a five-point CT finding scale (1, definitely absent; 2, probably absent; 3, equivocal; 4, probably present; 5, definitely present). Mediastinal and pleural findings evaluated in this study include aortic aneurysm, coronary artery calcification, pericardial effusion, pleural effusion, calcified pleural thickening, non-calcified pleural thickening, mediastinal tumor, lymph node enlargement. Lung parenchymal findings evaluated in this study include emphysema, ground-glass opacity, reticular opacity, micronodules, bronchiectasis, honeycomb, nodules larger than 5 mm.
The readers viewed five selected images to find lung parenchymal abnormality except for nodules. For these abnormal findings, the readers filled in one score each for five selected images.
The slice level for evaluation of these findings were selected by one of the author (T.K.), prior to the reading experiment at five image slices at apices, at aortic arch level, at carina level, at inferior pulmonary vein level and at hepatic vein level. The readers were instructed to read the five image slices first, according to table where image locations to be evaluated were designated. Then, readers viewed all lung images to detect lung nodules larger than 5 mm. A detected nodule was recorded according to the selected five image levels closest to the nodule. Then, readers read through soft tissue images to look for mediastinal and pleural abnormalities. The readers provided one score for these abnormal findings. Finally, the image quality at the level of carina was recorded by the readers a using five-point CT image quality scale (1, excellent; 2, good; 3, fair; 4, poor; 5, non-diagnostic).
2.7. Statistical analysis
An agreement rates of the CT abnormal finding scores are defined as a number of cases with the identical score for both low dose CT and standard dose CT images, divided by the number of cases (n = 59). To evaluate the difference in the CT scores between the low dose and the standard dose CT, a reader's score results were compared with the scores recorded by other two readers for standard dose CT. Specifically, the mean scores of the other two readers were used as benchmarks for the evaluation of the difference between two images. The score deviation of a reader from the other two readers is defined as the reader's score (low dose CT or standard dose CT) minus mean of the standard dose CT scores by the two other readers. For example, score deviation for reader 1 is calculated as follows:
The score deviation values of 59 patients and three readers were calculated for all image locations, CT findings and CT image types (low dose or standard dose).
The differences in the score deviations and the image quality between low dose CT and standard dose CT were evaluated with Wilcoxon signed rank test. The difference of scores was considered significant when p value was less than 0.05.
3. Results
3.1. Radiation dose measurement
The weighted CT dose index (CTDIw) was 5.36 mGy for low dose (50 mAs) scans and 16.1 mGy for standard dose (150 mAs) scans. Assuming that the length of the scan is 30 cm, estimated effective dose was 3.57 mSv for low dose CT and 10.7 mSv for standard dose CT.
3.2. CT abnormality scores
The CT scores recorded by the readers for five images were summarized in Table 1. Three readers recorded five CT scores of lung parenchymal abnormality for 59 cases. As a result, there were 885 (n = 3 × 5 × 59) scores for each lung abnormal finding. For mediastinal and pleural findings there were 177 (n = 3 × 59) scores for each finding. All the scores for honeycombing by three readers were 1 (definitely absent) for standard dose CT images. It was impossible to evaluate the diagnostic accuracy of honeycomb because it is detected too infrequently in the selected images taken from current study subjects. Therefore, the scores of honeycomb were not used for further analysis.
Table 1.
Distribution of CT abnormality scores recorded by three readers.
| Standard dose |
Low dose |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 5 | 4 | 3 | 2 | 1 | 5 | 4 | 3 | 2 | 1 | ||
| Lung | Emphysema | 320 | 11 | 3 | 0 | 551 | 274 | 26 | 1 | 7 | 577 |
| Ground-glass opacity | 347 | 34 | 4 | 10 | 490 | 309 | 44 | 17 | 17 | 498 | |
| Reticular opacity | 378 | 30 | 11 | 4 | 462 | 342 | 24 | 11 | 0 | 508 | |
| Micronodules | 245 | 18 | 2 | 0 | 620 | 193 | 14 | 0 | 1 | 677 | |
| Bronchiectasis | 276 | 18 | 2 | 4 | 584 | 238 | 19 | 3 | 3 | 622 | |
| Nodules (>5 mm) | 183 | 0 | 2 | 0 | 700 | 185 | 0 | 0 | 1 | 699 | |
| Mediastinum and pleura | Aortic aneurysm | 5 | 1 | 1 | 1 | 169 | 8 | 3 | 0 | 1 | 165 |
| Coronary artery calcification | 131 | 6 | 0 | 1 | 39 | 123 | 8 | 0 | 3 | 43 | |
| Pericardial effusion | 13 | 4 | 0 | 1 | 159 | 11 | 3 | 0 | 1 | 162 | |
| Pleural effusion | 32 | 0 | 0 | 0 | 145 | 28 | 1 | 0 | 0 | 148 | |
| Non-calcified pleural thickening | 117 | 5 | 0 | 0 | 55 | 92 | 9 | 0 | 0 | 76 | |
| Calcified pleural thickening | 14 | 0 | 0 | 0 | 163 | 13 | 1 | 2 | 0 | 161 | |
| Mediastinal tumor | 1 | 1 | 0 | 0 | 175 | 1 | 1 | 0 | 0 | 175 | |
| Lymph node enlargement | 174 | 2 | 0 | 0 | 1 | 165 | 7 | 1 | 0 | 4 | |
The sums of the numbers by three readers are shown in this table. The numbers for the lung abnormalities appearing in this table are the total of numbers at five image levels.
The agreement rates for lung abnormal findings are summarized in Table 2. Mean agreement rate of the lung parenchymal findings was 0.836 (range, 0.746–0.926). The agreement rate for aortic aneurysm, coronary artery calcification, pericardial effusion, pleural effusion, calcified pleural thickening, non-calcified pleural thickening, mediastinal tumor and lymph node enlargement were 0.943, 0.881, 0.966, 0.977, 0.735, 0.943, 1.000 and 0.915, respectively. Table 3, Table 4 summarize the score deviations of three readers for lung parenchymal findings and mediastinal and pleural findings, respectively. There were no significant difference between the scores for standard dose CT and low dose CT for all lung parenchymal, mediastinal and pleural findings.
Table 2.
Agreement rates of CT abnormality scores recorded by three readers.
| Emphysema | Ground-glass opacity | Reticular opacity | Micro-nodules | Bronchiectasis | Nodules (>5 mm) | |
|---|---|---|---|---|---|---|
| Apex | 0.819 | 0.825 | 0.876 | 0.848 | 0.926 | 0.898 |
| Aortic arch level | 0.848 | 0.881 | 0.859 | 0.819 | 0.791 | 0.904 |
| Carina level | 0.853 | 0.842 | 0.757 | 0.791 | 0.746 | 0.853 |
| Inferior PV level | 0.802 | 0.825 | 0.830 | 0.814 | 0.751 | 0.881 |
| Hepatic vein level | 0.819 | 0.808 | 0.785 | 0.853 | 0.859 | 0.926 |
| Mean | 0.828 | 0.836 | 0.822 | 0.825 | 0.815 | 0.893 |
An agreement rate is defined as a number of cases with the identical score for both low dose CT and standard dose CT images, divided by the number of cases (59).
Table 3.
Deviations of CT abnormality scores for lung parenchymal abnormalities.
| Emphysema | GGOa | Reticular | Micronodules | Bronchiectasis | Nodulesb | |
|---|---|---|---|---|---|---|
| Standard dose | ||||||
| Apex level | 0.70 ± 1.20 | 1.14 ± 1.35 | 1.63 ± 1.47 | 0.76 ± 1.30 | 0.79 ± 1.31 | 0.49 ± 1.11 |
| Aortic arch level | 0.64 ± 1.17 | 1.21 ± 1.42 | 1.45 ± 1.49 | 0.92 ± 1.38 | 1.10 ± 1.41 | 0.59 ± 1.19 |
| Carina level | 0.58 ± 1.15 | 1.91 ± 1.40 | 1.89 ± 1.43 | 1.05 ± 1.41 | 1.25 ± 1.44 | 0.81 ± 1.34 |
| Inferior PV level | 0.93 ± 1.35 | 2.05 ± 1.35 | 2.01 ± 1.37 | 0.66 ± 1.20 | 1.28 ± 1.46 | 0.90 ± 1.38 |
| Hepatic vein level | 0.72 ± 1.23 | 1.89 ± 1.37 | 1.77 ± 1.43 | 0.64 ± 1.18 | 0.81 ± 1.31 | 0.41 ± 1.03 |
| Low dose | ||||||
| Apex level | 0.86 ± 1.36 | 1.09 ± 1.32 | 1.68 ± 1.50 | 0.99 ± 1.49 | 0.80 ± 1.32 | 0.60 ± 1.23 |
| Aortic arch level | 0.73 ± 1.29 | 1.18 ± 1.40 | 1.48 ± 1.49 | 1.05 ± 1.46 | 1.13 ± 1.43 | 0.51 ± 1.08 |
| Carina level | 0.72 ± 1.33 | 1.94 ± 1.40 | 1.97 ± 1.42 | 1.06 ± 1.41 | 1.40 ± 1.51 | 0.81 ± 1.34 |
| Inferior PV level | 1.12 ± 1.48 | 2.19 ± 1.32 | 2.06 ± 1.36 | 0.84 ± 1.40 | 1.43 ± 1.50 | 0.84 ± 1.32 |
| Hepatic vein level | 0.92 ± 1.42 | 2.07 ± 1.37 | 1.69 ± 1.44 | 0.72 ± 1.29 | 1.36 ± 3.97 | 0.50 ± 1.16 |
| p-valuec | ||||||
| Apex level | 0.312 | 0.908 | 0.705 | 0.151 | 0.957 | 0.463 |
| Aortic arch level | 0.762 | 0.758 | 0.810 | 0.426 | 0.854 | 0.637 |
| Carina level | 0.386 | 0.836 | 0.603 | 0.997 | 0.393 | 1.000 |
| Inferior PV level | 0.314 | 0.279 | 0.649 | 0.268 | 0.321 | 0.684 |
| Hepatic vein level | 0.299 | 0.201 | 0.565 | 0.649 | 0.082 | 0.530 |
The score deviation of a reader is defined as the reader’s score (low dose CT or standard dose CT) minus mean of the standard dose CT scores by the two other readers.
GGO, ground-glass opacity.
Nodules measuring >5 mm.
Wilcoxon signed rank test.
Table 4.
Deviations of CT abnormality scores for mediastinal and pleural findings.
| Standard dose | Low dose | p value* | |
|---|---|---|---|
| Aortic aneurysm | 0.395 ± 0.984 | 0.322 ± 0.871 | 0.527 |
| Coronary artery calcification | 0.237 ± 0.668 | 0.379 ± 0.974 | 0.454 |
| Pericardial effusion | 0.062 ± 0.352 | 0.113 ± 0.540 | 0.622 |
| Pleural effusion | 0.079 ± 0.455 | 0.136 ± 0.662 | 0.568 |
| Non-calcified pleural thickening | 1.68 ± 1.44 | 1.74 ± 1.46 | 0.647 |
| Calcified pleural thickening | 0.667 ± 1.21 | 0.582 ± 1.14 | 0.515 |
| Mediastinal tumor | 0.079 ± 0.455 | 0.079 ± 0.455 | 1.000 |
| Lymph node enlargement | 0.249 ± 0.725 | 0.164 ± 0.532 | 0.406 |
The score deviation of a reader is defined as the reader’s score (low dose CT or standard dose CT) minus mean of the standard dose CT scores by the two other readers.
Wilcoxon signed rank test.
3.3. Image quality
The image quality score recorded by three readers were summarized in Table 5. Mean image quality scores for soft tissue images were 4.38 and 3.69 for standard dose CT and low dose CT, respectively. Mean image quality scores for lung images were 4.28 and 3.66 for standard dose CT and low dose CT, respectively. There were statistically significant difference between the image quality scores of standard dose CT and low dose CT images in both soft tissue images and lung images (p < 0.001).
Table 5.
Distribution of image quality scores recorded by three readers.
| Excellent |
Good |
Fair |
Poor |
Non-diagnostic |
||
|---|---|---|---|---|---|---|
| Scores | 5 | 4 | 3 | 2 | 1 | |
| Lung | Standard dose | 93 | 51 | 23 | 10 | 0 |
| Low dose | 41 | 56 | 59 | 21 | 0 | |
| Soft tissue | Standard dose | 103 | 43 | 27 | 4 | 0 |
| Low dose | 45 | 53 | 59 | 19 | 1 |
The numbers for scores in this table are the total of numbers by three readers.
4. Discussion
The result demonstrated that comparison of the interpretation results did not reveal any significant difference between the low dose CT images and standard dose CT images, suggesting that the image interpretation results of low dose CT are comparable to that of standard dose CT images.
Medical imaging has become a significant source of radiation exposure. In the developed nations, the contribution from medical imaging can be greater. In the United States, medical radiation exposure is reported to have exceeded natural background radiation from environment [6]. If we leave this upward trend unchecked, we will take a risk of increase in malignant disease in the future. Prevention of further expansion of medical radiation exposure is necessary. Growth of medical radiation exposure is largely attributable to the increase in the number of CT examinations [7]. The increase is due to excellent image quality of state-of-art CT scanner and also thanks to improved availability of CT examinations, which has been made possible by advent of high performance scanners. There is an argument on the possible overutilization of CT examinations [8]. Hence, efforts should be made to use CT examinations wisely for patients who are expected to benefit substantially from the examination. Nevertheless, it is true that the application of chest CT examinations is expanding and decreasing low-yield CT requests is not a simple task. Therefore, the further efforts to reduce the radiation dose in individual examinations are critical. For that purpose, evidences to support the use of low dose CT protocol for more general purpose are required.
There are several investigations on the radiation dose reduction for specific abnormal findings including pulmonary nodules [9], [10], emphysema severity [11], [12], [13] and bronchiectasis [14]. There are also several studies on the radiation dose reduction for CT pulmonary angiography [15], [16], [17]. Other studies focus on specific clinical situations, rather than on individual abnormal findings. Follow-up studies of oncology patients using low dose CT has been investigated [18], [19], [20], which showed detection of abnormal findings using low dose CT being comparable to standard dose CT. There were also reports in which diagnostic efficacy of low dose CT was examined for more general purposes. Two studies showed no statistically significant difference in the detection of abnormalities between standard-dose and reduced-dose CT [21], [22]. Takahashi et al. showed no significant difference in the detection rate of lung abnormalities between 250 mAs and 50 mAs images. Mayo et al. reported that the 20 mAs images may be acceptable for the interpretation of lung images. On the other hand, Mayo et al. reported significant difference in accuracy of lung findings in both 40 mAs and 100 mAs images, compared with conventional tube current images [23].
The current lack of generally accepted low dose protocol for routine CT limits the use of low dose technique to selected conditions. The purpose of this study is to determine whether it is reasonable to accept a 50 mAs chest CT protocol as a routine protocol for possible lung parenchymal abnormality. The current study revealed no significant difference in score deviation between two images. It also showed high agreement between low dose CT and standard dose CT in CT abnormality score. At the same time, the study showed that the image quality is decreased by the reduced radiation exposure. Therefore this study showed the possibility that the low dose CT (50 mAs) can produce interpretation result comparable to standard dose CT (150 mAs) in routine chest CT, despite the image quality degradation.
The score deviation of one reader from those of two other readers showed no statistically significant difference between the low dose CT images and standard dose CT images. Both low dose CT and standard dose CT scores of one reader are compared against the other two readers' score for standard dose images. Suboptimal quality images supposedly may make it difficult to discover subtle abnormality or, conversely, may give readers false impression of the lesions that are not actually present, which might enhance or reduce the score deviations. The lack of difference in score deviations between two images supports that the diagnostic results of the low dose CT images are not affected by the image quality degradation due to radiation dose reduction at 50 mAs.
Mediastinal and pleural findings showed high agreement rate (range, 0.735–1.000), with the lowest rate being for non-calcified pleural thickening. Consistent identification of thin localized non-calcified pleural findings might have been challenging task for readers. Mean agreement rate of the lung parenchymal findings was 0.836 (range, 0.746–0.926) and generally lower than those of mediastinal and pleural findings. The agreement rate for bronchiectasis was the lowest rate (0.746). This may be partly because of the effects of cardiac motion on the appearance of bronchus were different in two separate scans.
This study confirmed that there was noticeable image quality degradation. Theoretically, increase in noise and streak artifacts in low dose CT will invariably lead to image degradation to some degree. The least current time product for acceptable images cited in the reports varies form 13–140 mAs [22], [24], [25], [26], [27], probably depending on the criteria of image quality. This study indicates that image quality degradation is evident at current-time product of 50 mAs for readers and also confirmed that the diagnostic accuracy can be preserved even with noticeable image quality degradation.
The results from the current study demonstrated that fundamental lung parenchymal and soft tissue abnormalities which radiologists are expected to detect on CT images can be evaluated appropriately using a low dose CT protocol. This study assessed not only lung parenchymal findings but also mediastinal and pleural findings. For lung abnormalities, it is not practical to test the diagnostic accuracy of whole gamut of lung abnormal findings. Therefore, the study is planned to cover those essential lung parenchymal abnormalities which in combination may make up more complex patterns. The evaluated lung findings cover the all types of manifestation of lung abnormality on CT, i.e., area of hazy parenchymal increased opacity (ground-glass opacity), decreased opacity (emphysema), localized nodules (>5 mm) or micronodules (<5 mm), irregular combination of linear opacities (reticular opacities), sequel of fibrosis or other destructive process (honeycomb) and increased airway caliber (bronchiectasis). The lack of significant difference in the interpretation results in this study suggests that readers can identify the findings in the lungs, mediastinum and pleura on low dose CT as correctly as on standard dose CT.
We did not measure the final outcome, i.e., diagnosis or clinical decision, but it seems reasonable the result interpretation with a level of confidence can be a surrogate marker of diagnostic accuracy. Therefore, the results of this study implies that low-dose technique of current-time product of 50 mAs produces acceptable images which allow radiologists to discover the abnormal findings as confidently as with standard 150 mAs CT scans. The result supported that low dose CT images can be used to assess those CT image findings, suggesting the feasibility of low dose CT application for general screening purpose, not only for examinations performed for a specific purpose.
There are limitations to this study. First, we have chosen five images to look for lung parenchymal abnormality except for nodule measuring 5 millimeters or larger. The slight shift of patient position between two scans may make it hard to detect the same abnormal findings consistently on the same level, which may have lowered the agreement within readers. However, there are drawbacks to the whole lung evaluation for comparison of two images. It is hard to keep scrutinizing all the potential variation from normal anatomical structures. Subtle abnormality probably frequently missed by the readers, possibly underestimating the diagnostic accuracy of low dose CT images. Also, if the whole lung is reviewed for abnormalities, there is no guarantee that the same structure is identified as abnormal in two images. Therefore, in this particular study, we chose to use selected images to gauge the accuracy of interpretation. The second limitation to this study is that we were unable to assess the diagnostic accuracy of honeycomb, because almost no case was judged to have honeycomb at the selected image levels. The recognition of honeycomb is important for the diagnosis of interstitial lung disease as it is a key CT feature for the diagnosis of idiopathic pulmonary fibrosis [28]. However, the identification of two other almost invariable features of pulmonary fibrosis, i.e., reticular abnormalities and ground-glass opacity, were not affected by the low dose CT. Therefore, detection of diffuse interstitial lung disease is possible with low dose CT. The accuracy of classification of interstitial pneumonia using low dose CT might need to be investigated in a population with high prevalence of interstitial lung disease. Finally, lack of objective standard of abnormal findings may be one of limitations. For descriptive CT findings that are assessed in this study, such as ground glass opacities, clear-cut gold standard is hard to establish. Therefore, in this study one reader's interpretations were compared using other two readers’ CT finding scores based on standard dose CT images as benchmarks. Because the purpose of this study is to detect any degradation of diagnostic accuracy by employing low dose CT instead of standard dose CT, using other two reader's standard dose CT interpretation results should serve as good working standard with which the other reader's results were gauged.
In conclusion, this study showed the feasibility of routine use of low dose CT scan at 50 mAs for evaluation of essential Chest CT abnormal findings. A 50 mAs CT protocol may serve as an adequate protocol for routine chest CT examination not only for lungs, mediastinum and pleura. The result demonstrated that the degradation of image quality can be accepted at this level, without affecting the interpretation result, supporting broader application of low dose CT examination.
Funding
The study was supported by a research grant from Toshiba Medical Systems Corporation. Toshiba Medical Systems Corporation helped organize The International Multicenter Study for Low-Dose Chest CT Examination and Diagnosis (iLEAD) and provided technical support in preparation of reading experiment for this study.
Acknowledgments
The International Multicenter Study for Low-Dose Chest CT Examination and Diagnosis (iLEAD) is dedicated to the investigation of radiation dose reduction in chest CT examinations. Three institutions participated in this study group: Beth Israel Deaconess Medical Center, Boston, MA; German Cancer Research Center, Heidelberg, Germany; and Kobe University, Kobe, Japan. The iLEAD study group consists of Takeshi Kubo, Boston, MA; Yoshiharu Ohno, Kobe, Japan; Shiva Gautam, Boston, MA; Pei-Jan P. Lin, Boston, MA; Masaya Takahashi, Boston, MA; Mizuki Nishino, Boston, MA; Arkadiusz Sitek, Boston, MA; Daisuke Takenaka, Kobe, Japan; Munenobu Nogami, Kobe, Japan; Hisanobu Koyama, Kobe, Japan; Julia Ley-Zaporozhan, Heidelberg, Germany; Wolfram Stiller, Heidelberg, Germany; Sebastian Ley, Heidelberg, Germany; Hiroyasu Inokawa, Tochigi, Japan; Yasuko Fujisawa, Tochigi, Japan; Hiroyuki Kura, Tochigi, Japan; Vassilios Raptopoulos, Boston, MA; Kazuro Sugimura, Kobe, Japan; Hans-Ulrich Kauczor, Heidelberg, Germany; and Hiroto Hatabu, Boston, MA.
The authors express gratitude to Alba Cid for editorial assistance.
References
- 1.Mettler F.A., Jr., Bhargavan M., Faulkner K. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources-1950–2007. Radiology. 2009;253(2):520–531. doi: 10.1148/radiol.2532082010. [DOI] [PubMed] [Google Scholar]
- 2.Schauer D.A., Linton O.W. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Radiology. 2009;253(2):293–296. doi: 10.1148/radiol.2532090494. [DOI] [PubMed] [Google Scholar]
- 3.Kubo T., Lin P.J., Stiller W. Radiation dose reduction in chest CT: a review. AJR Am. J. Roentgenol. 2008;190(2):335–343. doi: 10.2214/AJR.07.2556. [DOI] [PubMed] [Google Scholar]
- 4.Kubo T., Ohno Y., Kauczor H.U., Hatabu H. Radiation dose reduction in chest CT-Review of available options. Eur. J. Radiol. 2014;83(10):1953–1961. doi: 10.1016/j.ejrad.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 5.Golding S.J. Radiation exposure in CT: what is the professionally responsible approach? Radiology. 2010;255(3):683–686. doi: 10.1148/radiol.10100449. [DOI] [PubMed] [Google Scholar]
- 6.National Council on Radiation Protection and Measurements, Ionizing Radiation Exposure of the Population of the United States : NCRP report No. 160 (2009) 160.
- 7.O’Connor G.T., Hatabu H. Lung cancer screening, radiation, risks, benefits, and uncertainty. JAMA. 2012;307(22):2434–2435. doi: 10.1001/jama.2012.6096. [DOI] [PubMed] [Google Scholar]
- 8.Hendee W.R., Becker G.J., Borgstede J.P. Addressing overutilization in medical imaging. Radiology. 2010;257(1):240–245. doi: 10.1148/radiol.10100063. [DOI] [PubMed] [Google Scholar]
- 9.Karabulut N., Toru M., Gelebek V., Gulsun M., Ariyurek O.M. Comparison of low-dose and standard-dose helical CT in the evaluation of pulmonary nodules. Eur. Radiol. 2002;12(11):2764–2769. doi: 10.1007/s00330-002-1368-4. [DOI] [PubMed] [Google Scholar]
- 10.Funama Y., Awai K., Liu D. Detection of nodules showing ground-glass opacity in the lungs at low-dose multidetector computed tomography: phantom and clinical study. J. Comput. Assist. Tomogr. 2009;33(1):49–53. doi: 10.1097/RCT.0b013e31815e6291. [DOI] [PubMed] [Google Scholar]
- 11.Bastarrika G., Wisnivesky J.P., Pueyo J.C. Low-dose volumetric computed tomography for quantification of emphysema in asymptomatic smokers participating in an early lung cancer detection trial. J. Thorac. Imaging. 2009;24(3):206–211. doi: 10.1097/RTI.0b013e3181a65263. [DOI] [PubMed] [Google Scholar]
- 12.Zaporozhan J., Ley S., Weinheimer O. Multi-detector CT of the chest: influence of dose onto quantitative evaluation of severe emphysema a simulation study. J .Comput. Assist. Tomogr. 2006;30:460–468. doi: 10.1097/00004728-200605000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Zompatori M., Fasano L., Mazzoli M. Spiral CT evaluation of pulmonary emphysema using a low-dose technique. Radiol. Med. 2002;104:13–24. [PubMed] [Google Scholar]
- 14.Yi C.A., Lee K.S., Kim T.S., Han D., Sung Y.M., Kim S. Multidetector CT of bronchiectasis: effect of radiation dose on image quality. AJR Am. J. Roentgenol. 2003;181:501–505. doi: 10.2214/ajr.181.2.1810501. [DOI] [PubMed] [Google Scholar]
- 15.Heyer C.M., Mohr P.S., Lemburg S.P., Peters S.A., Nicolas V. Image quality and radiation exposure at pulmonary CT angiography with 100- or 120-kVp protocol: prospective randomized study. Radiology. 2007;245(2):577–583. doi: 10.1148/radiol.2452061919. [DOI] [PubMed] [Google Scholar]
- 16.Matsuoka S., Hunsaker A.R., Gill R.R. Vascular enhancement and image quality of MDCT pulmonary angiography in 400 cases: comparison of standard and low kilovoltage settings. AJR Am. J. Roentgenol. 2009;192:1651–1656. doi: 10.2214/AJR.08.1730. [DOI] [PubMed] [Google Scholar]
- 17.Szucs-Farkas Z., Schaller C., Bensler S., Patak M.A., Vock P., Schindera S.T. Detection of pulmonary emboli with CT angiography at reduced radiation exposure and contrast material volume: comparison of 80 kVp and 120 kVp protocols in a matched cohort. Invest. Radiol. 2009;44:793–799. doi: 10.1097/RLI.0b013e3181bfe230. [DOI] [PubMed] [Google Scholar]
- 18.Yamada T., Ono S., Tsuboi M. Low-dose CT of the thorax in cancer follow-up. Eur. J. Radiol. 2004;51:169–174. doi: 10.1016/j.ejrad.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 19.Chiu C.H., Chern M.S., Wu M.H. Usefulness of low-dose spiral CT of the chest in regular follow-up of postoperative non-small cell lung cancer patients: preliminary report. J. Thorac. Cardiovasc. Surg. 2003;125:1300–1305. doi: 10.1016/s0022-5223(03)00033-3. [DOI] [PubMed] [Google Scholar]
- 20.Dinkel H.P., Sonnenschein M., Hoppe H., Vock P. Low-dose multislice CT of the thorax in follow-up of malignant lymphoma and extrapulmonary primary tumors. Eur. Radiol. 2003;13:1241–1249. doi: 10.1007/s00330-002-1647-0. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi M., Maguire W.M., Ashtari M. Low-dose spiral computed tomography of the thorax: comparison with the standard-dose technique. Invest. Radiol. 1998;33:68–73. doi: 10.1097/00004424-199802000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Mayo J.R., Hartman T.E., Lee K.S., Primack S.L., Vedal S., Muller N.L. CT of the chest: minimal tube current required for good image quality with the least radiation dose. AJR Am. J. Roentgenol. 1995;164:603–607. doi: 10.2214/ajr.164.3.7863879. [DOI] [PubMed] [Google Scholar]
- 23.Mayo J.R., Kim K.I., MacDonald S.L. Reduced radiation dose helical chest CT: effect on reader evaluation of structures and lung findings. Radiology. 2004;232(3):749–756. doi: 10.1148/radiol.2323030899. [DOI] [PubMed] [Google Scholar]
- 24.Naidich D.P., Marshall C.H., Gribbin C., Arams R.S., McCauley D.I. Low-dose CT of the lungs: preliminary observations. Radiology. 1990;175:729–731. doi: 10.1148/radiology.175.3.2343122. [DOI] [PubMed] [Google Scholar]
- 25.Ravenel J.G., Scalzetti E.M., Huda W., Garrisi W. Radiation exposure and image quality in chest CT examinations. AJR Am. J. Roentgenol. 2001;177:279–284. doi: 10.2214/ajr.177.2.1770279. [DOI] [PubMed] [Google Scholar]
- 26.Prasad S.R., Wittram C., Shepard J.A., McLoud T., Rhea J. Standard-dose and 50%-reduced-dose chest CT: comparing the effect on image quality. AJR Am. J. Roentgenol. 2002;179:461–465. doi: 10.2214/ajr.179.2.1790461. [DOI] [PubMed] [Google Scholar]
- 27.Zhu X., Yu J., Huang Z. Low-dose chest CT: optimizing radiation protection for patients. AJR Am. J. Roentgenol. 2004;183:809–816. doi: 10.2214/ajr.183.3.1830809. [DOI] [PubMed] [Google Scholar]
- 28.Raghu G., Collard H.R., Egan J.J. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]