Abstract
Empirical evidence has suggested that social support from family can help patients take their medicines correctly. This study aims to evaluate the role of a family member-based supervision package in the management of hypertension using a cluster randomized trial in rural China. We recruited patients with hypertension from four villages in Yangzhong and randomly allocated them to the control group (n=288) and the intervention group (n=266). A family member-based supervision package was applied to the intervention group, while the usual service was applied to the controls. Patients were followed for 12 months and completed face-to-face interviews at the end of 6 and 12 months. The primary outcomes were patients' medication adherence and frequency of blood pressure measurement. Secondary outcomes included changes in blood pressure, altered risk behaviours and occurrence of hypertension-related complications. To control for the effects of cluster randomization, multilevel mixed-effects regression models were used to compare group changes. We observed that the intervention improved patients' blood pressure measurement frequency (OR: 9.00, 95% CI: 4.52–17.91) and adherence to antihypertensive treatment (OR: 1.74, 95% CI: 0.91–3.32). Its effect on the blood pressure control rate was significant at the mid-term investigation (OR: 0.67, 95% CI: 0.40–0.93), but the long-term effect was not significant (OR: 0.89, 95% CI: 0.64–1.26). After 6 months of intervention, either systolic or diastolic blood pressure was significantly decreased in the intervention group. However, this difference was not significant at the final investigation. Findings from this study revealed that the family member-based supervised therapy may have positive effects on patients' adherence to blood monitoring and hypertensive medications.
Introduction
Despite progress in the prevention and treatment of elevated blood pressure, hypertension remains a major health challenge worldwide.1, 2, 3 High blood pressure has been related to an increased risk of mortality and morbidity from stroke, coronary heart disease, congestive heart failure and end-stage renal disease and has been shown to have a negative impact on health-related quality of life.1, 4, 5, 6 Hypertension has been identified as a major risk factor in China, accounting for 24.6% of deaths and 12.0% of Disability-Adjusted Life Years in 2010.7 Nearly 2.3 million total cardiovascular deaths and 1.3 million premature cardiovascular deaths are attributable to raised blood pressure in China every year.8 The prevention and control of hypertension is a top public health priority in China.
Most hypertensive patients need two or more drugs to control their blood pressure and concomitant statin treatment to reduce cardiovascular risk factors. Despite the availability of various effective and safe antihypertensive drugs, hypertension and its concomitant risk factors remain uncontrolled in most patients.9 Worldwide successful control of hypertension is poor, with only 5–58% of people taking antihypertensive medications achieving a blood pressure <140/90 mm Hg.10 One of the major factors in this poor control is lack of patient adherence to treatment.11 Adherence can be defined as the extent to which a person's behaviour corresponds with agreed recommendations from a health-care provider.12 The poor medication adherence of hypertensive patients is a major cause of unsatisfactory blood pressure control.13, 14, 15 Previous studies have reported that up to 50% of patients discontinue treatment within the first year.12 Thus, long-term antihypertensive treatment should be monitored, as blood pressure can be effectively controlled through better adherence.16, 17
Hypertensive patients may fail to take their medication due to the long duration of therapy, the symptomless nature of the condition, adverse drug reactions, complicated drug regimens, a lack of understanding about hypertension management, a lack of motivation and the challenge to their health beliefs.18 Typically, patients seek health care at different levels of a hospital based on their knowledge of and attitudes toward the disease, health insurance, economic background and accessibility of physicians or health-care institutions. There exists an obvious gap between the health care need and the services provided by community health facilities.19, 20 It was estimated that only 20% of patients' health care occurred in a doctor's office and that the other 80% was performed at patients' homes.21 Traditional medical care focuses on one-on-one doctor/patient interactions during the medical centre visit, missing many opportunities to positively influence patient care. Empirical evidence has suggested that social support from family and friends can help patients take their medicines correctly.22, 23 Thus, family-based case management is of particular interest because it is easy to access and provides assistance to patients in the management of their chronic conditions with the goal of achieving better outcomes.24 In a pilot study, we observed the acceptability and feasibility of family member-based supervision of patients with hypertension in a rural Chinese population.25 However, this finding was based on a quasi-experimental study design and has not been validated.
Thus, we performed a randomized control trial in a rural county of China with the aims of evaluating whether family member-based supervision improves patients' adherence to regular blood pressure monitoring and antihypertensive medications as well as the effect of such supervision on blood pressure management.
MATERIALS and methods
Study design
A cluster randomized trial was performed in a rural Chinese population. We registered this study through the Chinese Clinical Trial Register (http://www.chictr.org.cn/). The registration number was ChiCTR-TRC-13003051. The manuscript was drafted following the CONSORT Checklist (http://www.consort-statement.org/).
Ethical consideration
The Institutional Review Board of Nanjing Medical University approved the study. Written informed consent was obtained from all participants. The investigation was conducted according to the principles expressed in the Declaration of Helsinki.26, 27
Study sites
We purposely selected Yangzhong as the study area. Yangzhong is a county-level city in Jiangsu Province. It is located in the middle south of Jiangsu and in the cradle of the Yangtze River. It occupies an area of approximately 332 square kilometres. From the five towns in Yangzhong, we randomly selected two (Xinba and Baqiao) as the study settings. From each of the two towns, we randomly selected two villages. Then, these four villages were randomly assigned to the control group (two villages) and the intervention group (two villages). The randomization function in Excel 2013 was used to generate the random allocation sequence. The sequence was concealed until interventions were assigned.
Study subjects
We identified eligible patients with prevalent essential hypertension in the study areas through the local disease surveillance system. After patients provided informed consent, they were invited to participate in a baseline investigation. The inclusion criteria were as follows: (1) patients with essential hypertension (defined as a rise in blood pressure of unknown cause that increases risk for cerebral, cardiac and renal events; blood pressure ⩾140/90 mm Hg9; (2) living with family members; and (3) willing to participate in this study. The exclusion criteria were as follows: (1) with severe complications of hypertension such as hypertensive heart disease, stroke or renal failure and (2) could not be followed for 12 months.
Sample size
The sample size was estimated using an online tool (http://www.openepi.com/) based on the following parameters: (1) percent of unexposed with outcome, p1=60% (2) percent of exposed with outcome, p2=75% (3) α=0.05; (4) β=0.2. The estimated sample size was 152 in each arm, which was calculated according to the Fleiss formula. To take into account the lack of independence between patients in clusters, the 'variance inflation factor' (design effect, deff) was considered to increase the sample size. The deff was defined as 1+(n−1)ρ, where n was the average cluster size and ρ was the intracluster correlation coefficient for the particular outcome.28 Based on the findings from the pilot study, we defined the average cluster size as 130 and intracluster correlation coefficient as 0.008. Then, the estimated sample size was 308 in each arm. Considering the possibility of loss to follow-up, 10% more cases were added. Thus, the estimated sample size was 340 for each group.
Intervention
A modified family member-based education package, which was designed in the pilot study,25 was applied to the intervention group. The intervention that lasted for 12 months included the following aspects: (1) observer selection: each patient designated a family member as the supervisor. The supervisor could be the patient's spouse, child, parent or other family member; (2) supervisor training: both the patient and the selected family member were trained regularly. They were invited to attend the group educational sessions at the local village clinics. Doctors from the town hospitals and Center for Disease Control and Prevention gave the lectures. The content of the lectures covered the current situation of hypertension, risk factors of the disease, methods of prevention and treatment and the adverse effects of uncontrolled blood pressure. Furthermore, we regularly recommended the SMS (Short Messages Service) on knowledge of hypertension control and prevention to family supervisors and patients; (3) supervision: the designated family member supervised the patient's adherence to the antihypertensive medication and blood pressure measurement; (4) reminding: family supervisors were responsible for reminding patients to seek health care in a timely manner and to regularly monitor their blood pressure. If blood pressure could not be well controlled, they should urge patients to seek professional doctors in a timely fashion; (5) accessory appliances: we designed a calendar to help observers record patients' blood pressure values and treatment adherence (we listed some printed materials, photos of lectures and calendar in Supplementary File 1). Patients in the control group adopted the usual health-care services (self-administered therapy) without specific interventions.
Data collection
Trained master students from Nanjing Medical University administered a questionnaire to all participants. The modified questionnaire was designed based on the previous pilot study.25 We collected patients' demographic characteristics, socioeconomic status, treatment history, frequency of blood pressure measurement, adherence to antihypertensive drugs and attitudes toward the expected family member-based service package. Patients were followed for 12 months and completed face-to-face interviews at the end of 6 and 12 months. The primary outcomes were patients' medication adherence and frequency of blood pressure measurement. Secondary outcomes included changes in blood pressure, health behaviours and hypertension-related complications. We examined patients' self-reported medication adherence during last month prior to the interview. A participant was considered non-adherent if he or she reported missing one or more pills per week or if he or she was not currently taking previously prescribed antihypertensive medication. Complications of hypertension were defined as clinical outcomes that resulted from persistent elevation of blood pressure, including hypertensive heart disease, stroke and renal failure. After 6 and 12 months of observation, we also asked participants whether they had changed their behaviours such as reducing salt consumption, increasing physical activities and controlling tobacco smoking as compared with the state of the baseline survey.
Statistical methods
Data were entered with Epidata 3.1 (Epidata Association, Odense, Denmark) and analysed using STATA 11.0 (College Station, TX, USA). Baseline characteristics between groups were compared using t-tests (for continuous variables) or Chi-square tests (for categorical variables). To control for the effects of cluster randomization, mixed linear and nonlinear modelling for normally and non-normally distributed data, respectively.29 To test the effect of intervention on blood pressure, we used a multilevel mixed-effects linear regression model (xtmixed module in STATA software). For the binary responses, such as treatment adherence, blood pressure measurement or blood pressure control rate, we used the multilevel mixed-effects logistic regression models (xtmelogit module in STATA software). The effects of intervention were estimated as odds ratios (ORs) and 95% confidence intervals (CIs) as well as the corresponding P-values. The test level was set at 0.05. Subgroup analysis was performed to compare the effects of intervention on patient's behaviour between men and women. The forest plot was drawn using the meta-analysis module in STATA software.
Results
Study progress and general information
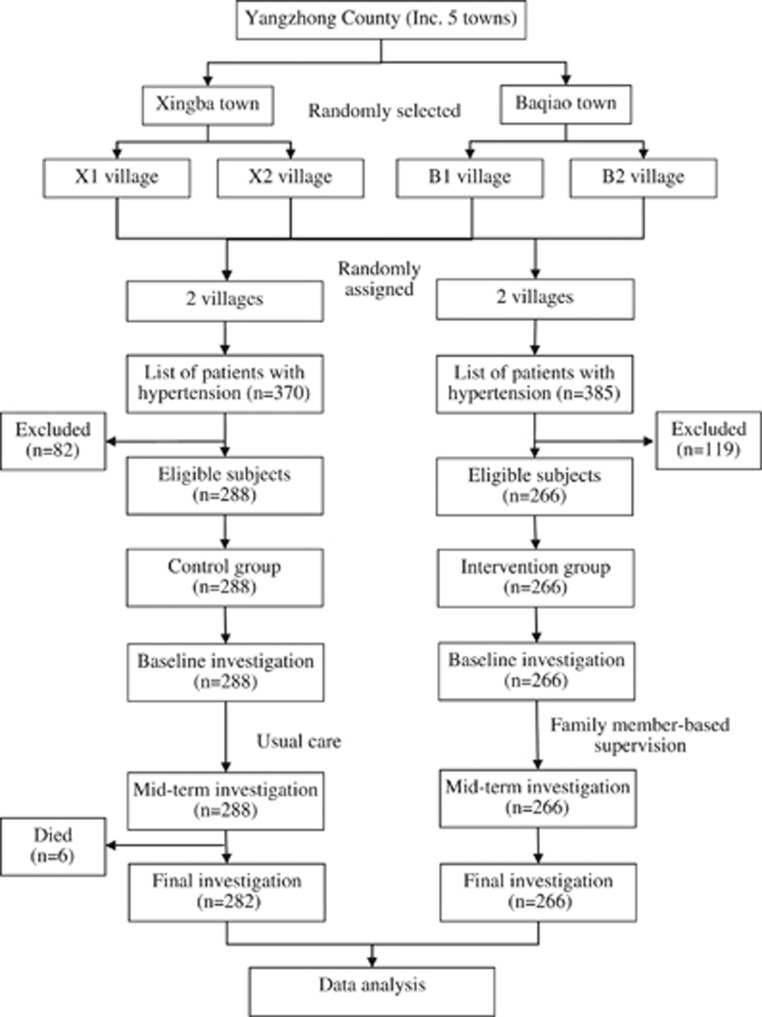
This study began in January 2013 and ended in January 2014. First, we identified 370 hypertensive patients in the control villages and 385 hypertensive patients in the intervention villages. After excluding ineligible patients, we enrolled 288 patients in the control group and 266 patients in the intervention group. The average age was 67.3±9.7 years in the control group and 66.2±9.2 years in the intervention group. As shown in Table 1, there was no significant difference in the distribution of sex, age, marital status, educational background or tobacco smoking history between the two groups. During the follow-up period, six patients in the control group died. The flow chart of this study is illustrated in Figure 1.
Table 1. Basic characteristics of study subjects.
| Characteristics | Control group N=288, n (%) | Intervention group N=266, n (%) | χ2 | P |
|---|---|---|---|---|
| Sex | 0.05 | 0.822 | ||
| Male | 137 (47.57) | 124 (46.62) | ||
| Female | 151 (52.43) | 142 (53.38) | ||
| Age | 0.15 | 0.700 | ||
| <60 | 60 (20.83) | 59 (22.18) | ||
| ⩾60 | 228 (79.17) | 207 (77.82) | ||
| Marital status | 2.33 | 0.312 | ||
| Single | 3 (1.04) | 4 (1.50) | ||
| Married | 222 (77.08) | 217 (81.58) | ||
| Divorced or bereft of spouse | 63 (21.88) | 45 (16.92) | ||
| Education | 4.35 | 0.226 | ||
| Illiterate | 74 (25.69) | 53 (19.92) | ||
| Primary school | 132 (45.83) | 119 (44.74) | ||
| Junior high school | 61 (21.18) | 73 (27.44) | ||
| Senior high school or above | 21 (7.29) | 21 (7.89) | ||
| Tobacco smoking | <0.01 | 0.996 | ||
| No | 197 (68.4) | 182 (68.42) | ||
| Yes | 91 (31.6) | 84 (31.58) |
Figure 1.
Flow chart of the study design.
Frequency of blood pressure measurement
At the baseline investigation, the blood pressure measurement frequency of the two groups was similar (χ2=4.55, P=0.208). However, after the intervention, there was a significant difference. For example, among patients in the intervention group, the proportion that measured their blood pressure more than one time per month increased from 56.0 to 95.8% at the mid-term investigation and to 96.2% at the final stage investigation. Among patients in the control group, the proportion that frequently obtained blood pressure measurements more than one time per month only increased to 66.3% at the mid-term investigation and to 74.7% at the final stage investigation (Table 2). After controlling for the effects of cluster randomization and baseline data, the adjusted OR (95% CI) of the intervention was 12.4 (6.4–23.8) for the mid-term evaluation and 9.0 (4.5–17.9) for the final evaluation (data not shown).
Table 2. Changes in blood pressure measurement frequency.
| Frequency (times/month) | Control group N=288, n (%) | Intervention group N=266, n (%) | χ2 | P |
|---|---|---|---|---|
| Baseline | ||||
| <1 | 113 (39.24) | 117 (43.98) | 4.55 | 0.208 |
| 1– | 92 (31.94) | 91 (34.21) | ||
| 2– | 25 (8.68) | 22 (8.27) | ||
| 3– | 58 (20.14) | 36 (13.53) | ||
| Mid terma | ||||
| <1 | 97 (33.68) | 11 (4.17) | 85.08 | <0.001 |
| 1– | 65 (22.57) | 122 (46.21) | ||
| 2– | 74 (25.69) | 76 (28.79) | ||
| 3– | 52 (18.06) | 55 (20.83) | ||
| Finalb | ||||
| <1 | 72 (25.53) | 10 (3.76) | 54.04 | <0.001 |
| 1– | 82 (29.08) | 103 (38.72) | ||
| 2– | 57 (20.21) | 84 (31.58) | ||
| 3– | 71 (25.18) | 69 (25.94) | ||
Missing two values from patients in the intervention group.
Six patients who died before the final investigation were not included.
Adherence to antihypertensive treatment
Considering the baseline difference in medication adherence between the two groups, we used a multilevel mixed-effects logistic regression model to adjust for the baseline data. After controlling for the effects of cluster randomization and baseline adherence, the adjusted OR (95% CI) was 3.8 (2.5–5.8) for the mid-term evaluation and 1.7 (0.9–3.3) for the final evaluation (Table 3).
Table 3. Differences in treatment adherence between groups.
| Characteristics | Control group N=288, n (%) | Intervention group N=266, n (%) | Za | Pa | OR (95% CI)a,b | Pa,b |
|---|---|---|---|---|---|---|
| Baseline | ||||||
| No | 110 (38.19) | 79 (29.70) | ||||
| Yes | 178 (61.81) | 187 (70.30) | 1.84 | 0.066 | 1.47 (0.98–2.22) | 0.066 |
| Mid term | ||||||
| No | 116 (40.28) | 39 (14.66) | 1 | |||
| Yes | 172 (59.72) | 227 (85.34) | 6.48 | 0.000 | 3.82 (2.50–5.83) | <0.001 |
| Final | ||||||
| No | 98 (34.03) | 61 (22.93) | 1 | |||
| Yes | 190 (65.97) | 205 (77.07) | 1.69 | 0.091 | 1.74 (0.91–3.32) | 0.097 |
Based on the multilevel mixed-effects logistic regression model.
Adjusted for the baseline adherence.
Blood pressure pre- and post-intervention
After 6 months of the intervention, either systolic or the diastolic blood pressure was significantly decreased in the intervention group. However, this difference was not significant at the final investigation (Table 4).
Table 4. Blood pressure values pre- and post- intervention.
| Blood pressure (mean±s.d. mm Hg) | Control group (N=288) | Intervention group (N=266) | Za | Pa |
|---|---|---|---|---|
| Baseline blood pressure | ||||
| SBP | 138.3±13.2 | 139.6±12.0 | 1.19 | 0.233 |
| DBP | 86.0±8.6 | 86.4±8.0 | 0.56 | 0.577 |
| Mid-term blood pressure | ||||
| SBP | 133.2±9.8 | 130.9±12.2 | −2.49 | 0.013 |
| DBP | 83.8±6.3 | 79.6±7.9 | −5.42 | <0.001 |
| Final blood pressure | ||||
| SBP | 138.4±12.6 | 139.0±13.4 | 0.43 | 0.668 |
| DBP | 85.4±8.2 | 84.5±8.0 | −1.18 | 0.240 |
| Changes in blood pressure | ||||
| Mid term vs baseline | ||||
| SBP | −5.0±13.9 | −8.6±13.9 | −3.05 | 0.002 |
| DBP | −2.3±9.1 | −6.8±8.9 | −4.62 | <0.001 |
| Final vs baseline | ||||
| SBP | 0.1±16.1 | −0.5±15.5 | −0.49 | 0.623 |
| DBP | −0.7±10.6 | −1.9±9.9 | −1.40 | 0.162 |
Abbreviations: DBP, diastolic blood pressure; SBP, systolic blood pressure.
Based on the multilevel mixed-effects linear regression model.
Blood pressure control rate
At the baseline investigation, the blood pressure control rate was higher in the control group than in the intervention group. Thus, we performed a multilevel mixed-effects logistic regression analysis to adjust for the baseline data. A positive significant effect was observed on the blood pressure control rate at the mid-term investigation (OR=0.7, 95% CI: 0.4–0.9), but the long-term effect was not significant (OR=0.9, 95% CI: 0.6–1.3) (Table 5).
Table 5. Differences in blood pressure control rate between the two groups.
| Characteristics (mm Hg) | Control group N=288, n (%) | Intervention group N=266, n (%) | Za | Pa | OR (95% CI)a,b | Pa,b |
|---|---|---|---|---|---|---|
| SBP | ||||||
| Baseline | ||||||
| <140 | 177 (61.46) | 129 (48.5) | 1 | |||
| ⩾140 | 111 (38.54) | 137(51.5) | 3.06 | 0.002 | 1.69 (1.21–2.37) | 0.002 |
| Mid term | ||||||
| <140 | 225 (78.13) | 215 (80.83) | 1 | |||
| ⩾140 | 63 (21.88) | 51 (19.17) | 0.09 | 0.925 | 0.93 (0.36–2.41) | 0.876 |
| Final | ||||||
| <140 | 165 (57.29) | 149 (56.02) | 1 | |||
| ⩾140 | 123 (42.71) | 117 (43.98) | 0.30 | 0.762 | 0.96 (0.68–1.36) | 0.835 |
| DBP | ||||||
| Baseline | ||||||
| <90 | 212 (73.61) | 161 (60.53) | 1 | |||
| ⩾90 | 76 (26.39) | 105 (39.47) | 2.73 | 0.006 | 1.86 (1.19–2.89) | 0.006 |
| Mid term | ||||||
| <90 | 242 (84.03) | 244 (91.73) | 1 | |||
| ⩾90 | 46 (15.97) | 22 (8.27) | −2.21 | 0.027 | 0.41(0.24–0.72) | 0.002 |
| Final | ||||||
| <90 | 201 (69.79) | 188 (70.68) | 1 | |||
| ⩾90 | 87 (30.21) | 78 (29.32) | −0.25 | 0.799 | 0.88 (0.60–1.27) | 0.494 |
| BP | ||||||
| Baseline | ||||||
| Normal | 154 (53.47) | 105 (39.47) | 1 | |||
| Abnormal | 134 (46.53) | 161 (60.53) | 3.29 | 0.001 | 1.76 (1.26–2.47) | 0.001 |
| Mid term | ||||||
| Normal | 207 (71.88) | 208 (78.20) | 1 | |||
| Abnormal | 81 (28.13) | 58 (21.80) | −0.17 | 0.046 | 0.67 (0.40–0.93) | 0.024 |
| Final | ||||||
| Normal | 142 (49.31) | 132 (49.62) | 1 | |||
| Abnormal | 146 (50.69) | 134 (50.38) | −0.07 | 0.940 | 0.89 (0.64–1.26) | 0.524 |
Abbreviations: BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Based on the multilevel mixed-effects logistic regression model.
Adjusted for the baseline data.
Hypertension-related complications
During the follow-up period, 32 patients in the control group developed hypertension-related complications (stroke: 20; coronary heart disease: 6; death: 6) and 26 patients in the intervention group developed hypertension-related complications (stroke: 18; coronary heart disease: 7; hypertensive renal disease: 1). There was no significant difference in incidence between the two groups (Z=−0.51, P=0.608). However, the case fatality rate was significantly higher in the control group than in the intervention group (20.3% vs 0%, Fisher's exact test P=0.031) (data not shown).
Behaviour changes after intervention
After 6 months of observation, patients in the intervention group had significantly reduced salt consumption (OR: 4.0, 95% CI: 2.6–6.1), increased physical activities (OR: 2.5, 95% CI: 1.7–3.7) and an increased tobacco smoking control rate (OR: 4.9, 95% CI: 2.1–11.1). However, the long-term effect was only significant for reduced salt consumption (OR: 2.4, 95% CI: 1.3–4.4) (Table 6).
Table 6. Behaviour changes after intervention.
| Characteristics | Control group | Intervention group | Za | OR (95% CI)a | Pa |
|---|---|---|---|---|---|
| N=288, n (%) | N=266, n (%) | ||||
| Mid term | |||||
| Reduced salt consumption | |||||
| No | 113 (39.24) | 37 (13.91) | |||
| Yes | 175 (60.76) | 229 (86.09) | 6.46 | 4.00 (2.63–6.08) | <0.001 |
| Increased physical activities | |||||
| No | 150 (52.08) | 81 (30.45) | |||
| Yes | 138 (47.92) | 185 (69.55) | 4.54 | 2.49 (1.68–3.70) | <0.001 |
| Reduced tobacco smokingb | |||||
| No | 48 (68.57) | 13 (30.95) | |||
| Yes | 22 (31.43) | 29 (69.05) | 3.75 | 4.87 (2.13–11.12) | <0.001 |
| Final | |||||
| Reduced salt consumption | |||||
| No | 69 (24.56) | 33 (12.41) | |||
| Yes | 212 (75.44) | 233 (87.59) | 2.93 | 2.42 (1.34–4.38) | <0.001 |
| Increased physical activities | |||||
| No | 106 (37.72) | 89 (33.46) | |||
| Yes | 175 (62.28) | 177 (66.54) | 1.04 | 1.20 (0.85–1.71) | 0.298 |
| Reduced tobacco smokinga | |||||
| No | 24 (39.34) | 12 (34.29) | |||
| Yes | 37 (60.66) | 23 (65.71) | 0.48 | 1.31 (0.43–3.97) | 0.632 |
Based on the multilevel mixed-effects logistic regression model.
Only analysed those who had a history of tobacco smoking at the baseline investigation.
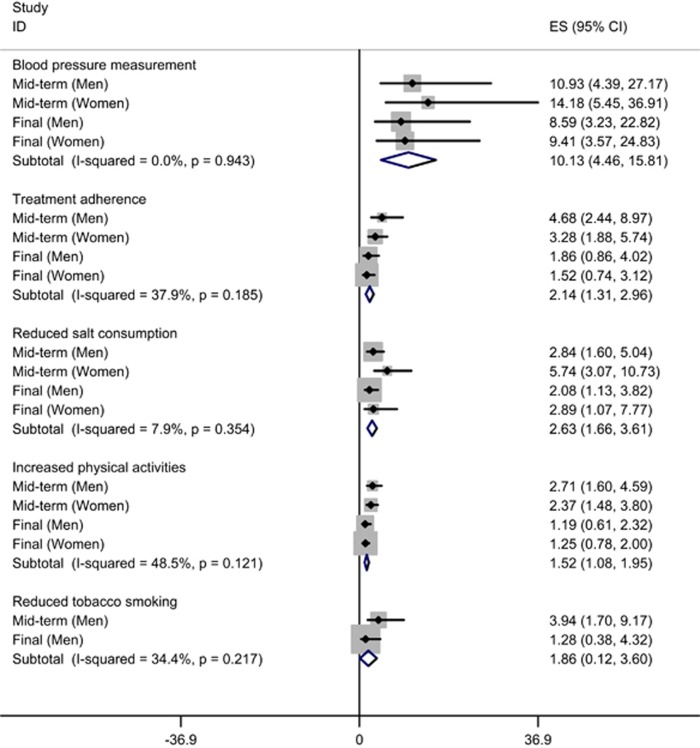
Subgroup analysis by sex
We further performed a subgroup analysis by patient's sex to compare the effects of intervention on the frequency of blood pressure measurement, treatment adherence, reduced salt consumption, increased physical exercises and reduced tobacco smoking. As shown in Figure 2, no significant difference was found between men and women.
Figure 2.
The forest plot of the effects of intervention on patient's behaviour between men and women. As there is only one female smoker, the effect of intervention on reduced tobacco smoking among women is not plotted.
Discussion
In this field intervention trial, we evaluated the role of a patient's family members on the management of hypertension. Findings from this study suggest that family member-based supervision can be a way to promote medication adherence and better outcomes, but it requires more comprehensive strategies. Further patient-centred studies are required to improve the management of patients with hypertension in China.
Poor adherence toward antihypertensive drugs is a worldwide problem.30 A community-based cross-sectional study in Dharan Municipality of Eastern Region of Nepal reported that only 56.5% patients were adherent to antihypertensive medication.30 The prevalence of hypertension in China is similar to that in other countries, but the control rate has remained low in the past few decades.31 Lack of adherence to blood pressure-lowering medication is a major reason for poor control of hypertension worldwide.18 In spite of the availability of various antihypertensive agents, patients' medication adherence and blood pressure management are inadequate.2 Current methods of improving adherence to treatment for chronic health problems are rather complex. Reviews have reported that much of the intervention work has generally taken a pragmatic one-size-fits-all approach to enhancing adherence; however, most of these interventions have been shown to be ineffective.11, 18, 32 A Cochrane systematic review found that simplifying dosing regimens had a relative increase in medication adherence of 8–19.6% motivational strategies had small increases in adherence up to a maximum of 23% and complex interventions involving more than one technique increased adherence ranging from 5% to a maximum of 41%.18
Non-adherence seems to be a patient problem, but it is directly influenced by health-care providers and the health-care system. Researchers should continue to develop new technology and approaches to monitoring patients' treatment adherence, support better blood pressure control and decrease hypertension-related mortality and morbidity.33 Adverse drug reactions should be identified early and managed promptly to address the safety of drugs. Treatment should be monitored, as better adherence to antihypertensive medications can lead to effective blood pressure control and a reduction in the risk of complications.16 Several interventions such as health education, family-support, self-management, health-care management changes and the training of providers have been performed in some communities of China.34 In recent years, increasing number of studies have been performed to explore innovative ways to improve patients' treatment adherence and outcomes, such as physician-level and practice-level financial incentives for hypertension care,35, 36 shared decision making in antihypertensive therapy,37 an interdisciplinary education programme38 and home-based blood pressure tele-monitoring.39 Considering that causes of noncompliance are complicated, individualized intervention strategies should be designed based on the characteristics of patients in the local context.
In this study, we examined a family member-based supervision package that aimed to provide social support to patients in a effective and acceptable manner. We observed a positive effect of intervention on the patients' adherence to blood pressure monitoring. However, the intervention's effect on the blood pressure control rate was only obvious at the mid-term investigation; it was not significant at the final investigation. Thus, research should consider how to achieve a long-term effect of family member-based intervention. It is noteworthy that according to the Fourth National Health and Nutrition Survey, the prevalence, treatment and control rates of hypertension were 18.8, 24.7 and 6.1%, respectively.31 In our study, the control rate of blood pressure was relatively high at the baseline investigation (53.5% in the control group and 39.5% in the intervention group). Also, the baseline medication adherence was higher in this study than that reported in other populations.30, 40 These may weaken the intervention effect of the family member-based supervision.
Complications of hypertension are clinical outcomes that result from the persistent elevation of blood pressure. Uncontrolled blood pressure remains the most common cause of death, accounting for more than seven million deaths per year worldwide.41 Hypertension is an independent predisposing factor for heart failure, coronary artery disease, stroke, renal disease and peripheral arterial disease. In this study, we did not observe a significant difference in the incidence of hypertension-related complications between groups. This result may be attributed to a greater cases-searching effort for the intervention group. Of note, the fatality rate was significantly decreased after the intervention.
Although salt's effect on blood pressure has recently gained interest,42 public health interventions to reduce salt intake with the goal of decreasing adverse outcomes have been launched in numerous countries.43 Reduction in salt intake can cause a significant decrease in blood pressure, irrespective of sex and ethnic group.44 In the current study, we observed a significant reduction of salt intake among patients receiving family member-based supervision. Our regular training of family supervisors may play an important role. Unlike the effect on salt intake, the intervention has limited long-term effects on patients' active physical exercises and tobacco smoking. Physical inactivity is linked to several chronic diseases, including coronary heart disease, type 2 diabetes, obesity, some cancers and poor mental health.45 The mortality risk of being inactive was estimated to be equivalent to an increase of approximately 40 mm Hg in systolic blood pressure or 20 mm Hg in diastolic blood pressure, a number relevant to patients with hypertension.46 However, it has been proven that encouraging people to be more active is not easy.45 Additional support at the organizational level should be encouraged, and wider contextual factors that impinge on the delivery of and response to the intervention should be considered. Future studies should attempt to adopt an approach that is tailored to individual patients and addresses barriers to adherence. Combinations of strategies include simpler dosage regimens, patient motivation and shared decision making in a partnership between patient and practitioner.18
There are several limitations to this study. First, we used a cluster randomization method to allocate study subjects. The advantage of using a cluster randomized trial design is that it overcomes practical and contamination problems that can arise when simple random allocation is used.28 However, the limitation of cluster randomization was obvious, and it was difficult to ensure that the basic characteristics of study subjects were comparative. As shown in this study, the baseline treatment adherence and proportion of patients with uncontrolled blood pressure differed between the groups, which could influence the assessment of effects, although we adjusted it using a regression model. Second, the number of clusters in a cluster randomized controlled trial usually should be >10. This study randomly allocated only four villages into two arms. Moreover, the sample size of eligible participants was lower than the prior estimation. Given the number of clusters and the average number of participants in each cluster, the actual power would be smaller than 80%, resulting in the risk of false negative findings. Third, since 2009, China's government has carried out an essential public health service programme, and the management of patients with hypertension is one of the major tasks of this programme. This programme may also affect our study subjects' medication adherence and blood pressure control rate. This can be demonstrated in the control group, as this group also displayed improved treatment adherence and behaviour changes. Fourth, the representativeness of the study subjects should be noted. This study was conducted in one rural area of China, and the generalization of the results to other populations should be done with caution.
In conclusion, the family member-based supervised therapy may have positive effects on patients' adherence to blood monitoring and hypertensive medications. However, its effect was weakened over a long time period. High priority should be given to fundamental and applied research concerning innovations to assist patients in following medication prescriptions for long-term medical disorders.
Acknowledgments
This study was supported by the China Medical Board (CMB991), Qing Lan Project (2014), Six Talent Peaks Project in Jiangsu Province (2014-YY-023), Philosophy and Social Science Research Fund of Jiangsu College (2014SJB164) and Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on the Journal of Human Hypertension website (http://www.nature.com/jhh)
Supplementary Material
References
- Israili ZH, Hernandez-Hernandez R, Valasco M. The future of antihypertensive treatment. Am J Ther 2007; 14: 121–134. [DOI] [PubMed] [Google Scholar]
- Mensah GA, Bakris G. Treatment and control of high blood pressure in adults. Cardiol Clin 2010; 28: 609–622. [DOI] [PubMed] [Google Scholar]
- Cheung BM. The hypertension-diabetes continuum. J Cardiovasc Pharmacol 2010; 55: 333–339. [DOI] [PubMed] [Google Scholar]
- Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 2001; 10: 621–635. [DOI] [PubMed] [Google Scholar]
- Cao Y, Tang X, Yang L, Li N, Wu YQ, Fan WY et al. [Influence of chronic diseases on health related quality of life in middle-aged and elderly people from rural communities: application of EQ-5D scale on a Health Survey in Fangshan, Beijing]. Zhonghua Liu Xing Bing Xue Za Zhi 2012; 33: 17–22. [PubMed] [Google Scholar]
- Tan Z, Liang Y, Liu S, Cao W, Tu H, Guo L et al. Health-related quality of life as measured with EQ-5D among populations with and without specific chronic conditions: a population-based survey in Shaanxi Province, China. PLoS ONE 2013; 8: e65958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2013; 381: 1987–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J, Gu D, Chen J, Wu X, Kelly TN, Huang JF et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009; 374: 1765–1772. [DOI] [PubMed] [Google Scholar]
- Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet 2007; 370: 591–603. [DOI] [PubMed] [Google Scholar]
- Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens 2004; 22: 11–19. [DOI] [PubMed] [Google Scholar]
- Alhalaiqa F, Deane KH, Nawafleh AH, Clark A, Gray R. Adherence therapy for medication non-compliant patients with hypertension: a randomised controlled trial. J Hum Hypertens 2012; 26: 117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhart PV, Sabate E. Adherence to long-term therapies: evidence for action. J Nurs Scholarsh 2003; 35: 207. [PubMed] [Google Scholar]
- Waeber B, Burnier M, Brunner HR. How to improve adherence with prescribed treatment in hypertensive patients? J Cardiovasc Pharmacol 2000; 35(Suppl 3): S23–S26. [DOI] [PubMed] [Google Scholar]
- Hedna K, Hakkarainen KM, Gyllensten H, Jönsson AK, Andersson Sundell K, Petzold M et al. Adherence to antihypertensive therapy and elevated blood pressure: should we consider the use of multiple medications? PLoS ONE 2015; 10: e0137451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarti S, Hajj A, Karam L, Jabbour H, Sarkis A, El Osta N et al. Association between adherence, treatment satisfaction and illness perception in hypertensive patients. J Hum Hypertens (e-pub ahead of print 27 August 2015; doi:10.1038/jhh.2015.86). [DOI] [PubMed]
- Corrao G, Parodi A, Nicotra F, Zambon A, Merlino L, Cesana G et al. Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens 2011; 29: 610–618. [DOI] [PubMed] [Google Scholar]
- Zanchetti A. From dietary factors to drug adherence: approaches to improve understanding and treatment of hypertension. J Hypertens 2015; 33: 895–896. [DOI] [PubMed] [Google Scholar]
- Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev 2004; (3): CD004804. [DOI] [PMC free article] [PubMed]
- Murphy K, Chuma T, Mathews C, Steyn K, Levitt N. A qualitative study of the experiences of care and motivation for effective self-management among diabetic and hypertensive patients attending public sector primary health care services in South Africa. BMC Health Serv Res 2015; 15: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng XL, Pang M, Beard J. Health system strengthening and hypertension awareness, treatment and control: data from the China Health and Retirement Longitudinal Study. Bull World Health Organ 2014; 92: 29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BB, Ralston JD, Fishman PA, Catz SL, Cook A, Carlson J et al. Electronic communications and home blood pressure monitoring (e-BP) study: design, delivery, and evaluation framework. Contemp Clin Trials 2008; 29: 376–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson VR, Jacobson KL, Gazmararian JA, Blake SC. Does social support help limited-literacy patients with medication adherence? A mixed methods study of patients in the Pharmacy Intervention for Limited Literacy (PILL) study. Patient Educ Couns 2010; 79: 14–24. [DOI] [PubMed] [Google Scholar]
- De Geest S, Abraham I, Gemoets H, Evers G. Development of the long-term medication behaviour self-efficacy scale: qualitative study for item development. J Adv Nurs 1994; 19: 233–238. [DOI] [PubMed] [Google Scholar]
- Alderman MH. Blood pressure control to reduce cardiovascular morbidity and mortality: today and tomorrow. Eff Clin Pract 1998; 1: 23–25. [PubMed] [Google Scholar]
- Huang S, Chen Y, Zhou J, Wang J. Use of family member-based supervision in the management of patients with hypertension in rural China. Patient Prefer Adherence 2014; 8: 1035–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markman JR, Markman M. Running an ethical trial 60 years after the Nuremberg Code. Lancet Oncol 2007; 8: 1139–1146. [DOI] [PubMed] [Google Scholar]
- Iyalomhe GB, Imomoh PA. Ethics of clinical trials. Niger J Med 2007; 16: 301–306. [DOI] [PubMed] [Google Scholar]
- Sedgwick P. Cluster randomised controlled trials: sample size calculations. BMJ 2013; 346: f2839. [Google Scholar]
- Campbell MK, Mollison J, Steen N, Grimshaw JM, Eccles M. Analysis of cluster randomized trials in primary care: a practical approach. Fam Pract 2000; 17: 192–196. [DOI] [PubMed] [Google Scholar]
- Bhandari B, Bhattarai M, Bhandari M, Ghimire A, Pokharel PK, Morisky DE. Adherence to antihypertensive medications: population based follow up in Eastern Nepal. J Nepal Health Res Counc 2015; 13: 38–42. [PubMed] [Google Scholar]
- Wang JG, Li Y. Characteristics of hypertension in Chinese and their relevance for the choice of antihypertensive drugs. Diabetes Metab Res Rev 2012; 28(Suppl 2): 67–72. [DOI] [PubMed] [Google Scholar]
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev 2008; (2): CD000011. [DOI] [PubMed]
- Erdine S, Arslan E. Monitoring treatment adherence in hypertension. Curr Hypertens Rep 2013; 15: 269–272. [DOI] [PubMed] [Google Scholar]
- Lu Z, Cao S, Chai Y, Liang Y, Bachmann M, Suhrcke M et al. Effectiveness of interventions for hypertension care in the community - a meta-analysis of controlled studies in China. BMC Health Serv Res 2012; 12: 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen LA, Simpson K, Pietz K, Urech TH, Hysong SJ, Profit J et al. Effects of individual physician-level and practice-level financial incentives on hypertension care: a randomized trial. JAMA 2013; 310: 1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolor RJ, Schulman KA. Financial incentives in primary care practice: the struggle to achieve population health goals. JAMA 2013; 310: 1031–1032. [DOI] [PubMed] [Google Scholar]
- Tinsel I, Buchholz A, Vach W, Siegel A, Dürk T, Buchholz A et al. Shared decision-making in antihypertensive therapy: a cluster randomised controlled trial. BMC Fam Pract 2013; 14: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauziere TA, Chevarie N, Poirier M, Utzschneider A, Belanger M. Effects of an interdisciplinary education program on hypertension: a pilot study. Can J Cardiovasc Nurs 2013; 23: 12–19. [PubMed] [Google Scholar]
- Margolis K, Asche S, Bergdall A, Trower N, Sekenski J, Pritchard R et al. A3-1: Outcomes of a randomized trial of home blood pressure telemonitoring with pharmacist case management. Clin Med Res 2013; 11: 134. [Google Scholar]
- Al-Hajje A, Awada S, Rachidi S, Zein S, Bawab W, El-Hajj Z et al. Evaluation of medication adherence in Lebanese hypertensive patients. J Epidemiol Glob Health (e-pub ahead of print 29 July 2015; doi:10.1016/j.jegh.2015.07.002). [DOI] [PMC free article] [PubMed]
- Hering D, Esler MD, Krum H, Mahfoud F, Böhm M, Sobotka PA et al. Recent advances in the treatment of hypertension. Expert Rev Cardiovasc Ther 2011; 9: 729–744. [DOI] [PubMed] [Google Scholar]
- Farquhar WB, Edwards DG, Jurkovitz CT, Weintraub WS. Dietary sodium and health: more than just blood pressure. J Am Coll Cardiol 2015; 65: 1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Li H, Hong S, Yin X. Salt reduction and hypertension in China: a concise state-of-the-art review. Cardiovasc Diagn Ther 2015; 5: 191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev 2013; 4: CD004937. [DOI] [PubMed] [Google Scholar]
- Procter S, Mutrie N, Davis A, Audrey S. Views and experiences of behaviour change techniques to encourage walking to work: a qualitative study. BMC Public Health 2014; 14: 868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li CS, Liu CC, Tsai MK, Tai YP, Wai JP, Tsao CK et al. Motivating patients to exercise: translating high blood pressure into equivalent risk of inactivity. J Hypertens 2015; 33: 287–293. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.