Abstract
Introduction:
The diagnosis and management of narcolepsy in the Indian context needs to be revisited especially in the wake of concerns raised by sleep medicine experts that the entity could be formidably underdiagnosed, as well as undertreated in our setting.
Materials and Methods:
The history, clinical records, polysomnographic/multiple sleep latency test data, and treatment records of five hundred consecutive patients attending a dedicated sleep clinic between the years 2013 and 2016 were retrospectively analyzed. The response to treatment measures and improvement in daytime functioning were periodically assessed by personal/telephonic interview and E-mail communication.
Results:
Thirteen patients were diagnosed with narcolepsy based on the standard criteria of which three had cataplexy. The mean age of presentation was 23.23 years and the male:female ratio was 2.25:1. The mean duration from the onset of symptoms to diagnosis was 4.2 years. Two patients responded to nonpharmacological interventions alone, and six to modafinil, while two patients remained symptomatic and required treatment with methylphenidate. One patient was lost to follow-up, while two others are due for their first follow-up.
Conclusion:
A refurbished outlook of the diagnostic methodology and treatment paths tailored to our clinical scenario can potentially impact the future of narcolepsy management and research in our country.
Keywords: Cataplexy, modafinil, multiple sleep latency test, narcolepsy, scheduled naps
Introduction
The intriguing intrusions of the rapid eye movement (REM) sleep into the realm of wakefulness and the dissociation of its basic elements of atonia and active sleep leading to the dramatic picture of cataplectic attacks define one of the most elusive entities in clinical medicine-narcolepsy. The initial reports of Westphal and the observations made by Gélineau (who coined the term narcolepsy) in a wine cask maker who suffered from the classical phenomenology awakened the medical world to this mysterious illness.[1] In the 1930s, Daniels emphasized the association of daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations. The landmark discovery of sleep onset REM periods (SOREMPs) was made by Yoss, Daly, and Vogel.[2] The detection of HLA-DQB1*602 observed in nearly two-thirds of the patients, and reduced levels of hypocretin-1 in the cerebrospinal fluid (CSF) of patients with narcolepsy-cataplexy phenotype have broadened the perspective of this primary sleep disorder of central origin.[3,4,5] Autoreactive CD4+ T-cells triggered by environmental stimuli like viruses or vaccination, which are able to recognize fragments of hypocretin when presented by HLA-DQB1*602, are now believed to be the causative mechanism for destruction of the hypothalamic neurons resulting in narcolepsy.[2]
Based on published literature, the prevalence of disease varies widely between different populations.[6] But whether this represents a true difference or disparities in the diagnostic capabilities, criteria used for diagnosis and epidemiological investigations is a matter of debate. The compendium of published data pertaining to narcolepsy in our country is restricted to few case reports and a series of twenty cases from a tertiary care center.[7,8,9] The latter discussed the clinical and laboratory pattern of narcolepsy which has made us cognizant with the pattern of our patient population which was not significantly different from the world literature. This report attempts to present real-life data on a series of patients with narcolepsy covering all the aspects of diagnosis and management. This will empower the treating physician or sleep specialist to confidently diagnose as well as formulate a rational, comprehensive and effective strategy to manage this eminently treatable sleep disorder.
Materials and Methods
The clinical and polysomnographic data of all patients who underwent overnight polysomnography (PSG) at our dedicated sleep center between January 2013 and April 2016 were retrospectively analyzed. Of the 512 patients in our database, 17 were suspected to have narcolepsy on clinical grounds for which a 4–5 nap multiple sleep latency test (MSLT) was performed after an overnight PSG comprising at least 6 h of recorded sleep. The diagnosis of narcolepsy was conclusively established on the basis of the international classification of sleep disorders criteria (2nd or 3rd edition depending on the period of presentation to the center) in thirteen of them.[10] Patients whose daytime sleepiness was completely accounted for by an alternate cause like drug or substance abuse, primary sleep disorder such as sleep disordered breathing or periodic limb movement disorder, neurological or medical illness, or psychiatric disorders were excluded from the analysis. Fulfillment of MSLT criteria was mandatory for inclusion, while human leukocyte antigens (HLA) haplotype and CSF hypocretin levels were not. Measures of introspective sleep like the Epworth sleepiness scale (ESS) was also obtained as a part of the evaluation protocol of our center.
All patients included in the study had undergone a full night supervised PSG on the Alice 5 video PSG system. The study protocol included a six-channel electroencephalogram, two-channel electro-oculogram, electromyogram of the submentalis and right anterior tibialis muscle, electrocardiogram, airflow and respiratory effort channels comprising thermistors and nasal pressure transducers, piezoelectric belts to estimate the respiratory effort, and pulse oximetry to keep track of blood oxygen saturation. All studies were reviewed by the sleep specialist (MB) in the morning before a decision was made to proceed for MSLT. The scoring criteria for sleep stages, respiratory events (hypopnea, apnea, and respiratory event related arousals), and periodic limb movements as laid down by the American academy of sleep medicine (2014) were rigorously followed.[10]
The MSLT was performed in all patients by an experienced sleep technologist under the direct supervision of the lead author (MB) as per the guidelines proposed by the AASM task force.[11] After ensuring that the case has had sufficient nocturnal sleep in the past 2 weeks and was not exposed to medications or alcohol or other confounding factors, the patients were encouraged to fall asleep at 2 h intervals. The study commenced 2 h after awakening and provided the cases 20 min of multiple unperturbed opportunities to sleep. Once initiated, the sleep was not interrupted until 15 min of recording was completed. If the results were not conclusive after the fourth nap, a fifth nap was recorded. The most definitive parameter used in the series for narcolepsy was two or more SOREMPs. The mean sleep latency (defined as the time elapsed from the moment the lights are put out to the appearance of the first epoch of sleep) was also estimated in all cases.
After establishing the diagnosis, an individualized management plan was formulated for each patient based on the clinical profile, socioeconomic, educational and occupational characteristics, as well as the expectations and requirements of the patient and family members. Goals of therapy were defined and addressed one by one. Interventions were broadly divided into two categories: On pharmacological (scheduled naps and counseling) and pharmacological (modafinil, methylphenidate, and venlafaxine).[12,13,14,15,16] The details of treatment were gathered from carefully maintained case records and follow-up was maintained through clinic visits, telephonic, and E-mail communications.
Results
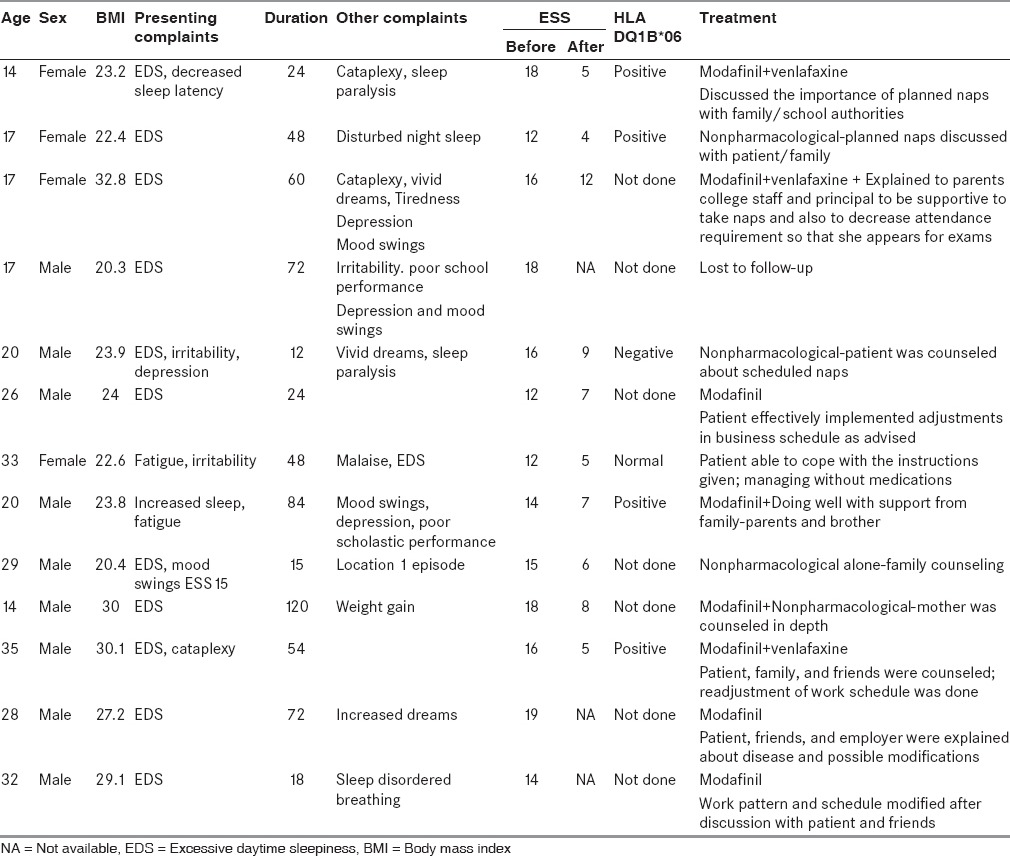
All 13 patients (100%) had excessive daytime sleepiness. Cataplexy was present in three patients (23.1%), while two patients (15.4%) had sleep paralysis. Two patients (15.4%) were found to have a decline in scholastic performance after the onset of symptoms. The mean age of onset was 23.23 years (range: 14–35 years); male: ESS (15.1) and duration of illness 4.2 years (15 months - 10 years). Males were more commonly affected than females (male:female ratio – 2.25:1). The family history of sleep-related breathing disorders was present in two cases, while none reported features of idiopathic hypersomnia, adjustment sleep disorder, insufficient sleep syndrome, circadian rhythm disorders, REM behavior disorder, or sleep talking. General physical and systemic examination was unremarkable with a mean body mass index of 25.4. Coexistent depression was present in five patients (38.5%). The clinical and demographic characteristics are summarized in Table 1.
Table 1.
Patient characteristics
Noncontrast magnetic resonance imaging of the brain performed in all patients returned normal findings. HLA-DQ1B*6 screening was suggested to all patients. Of the six patients who underwent the test, four were positive and two were negative for HLA-DQ1B1*602.
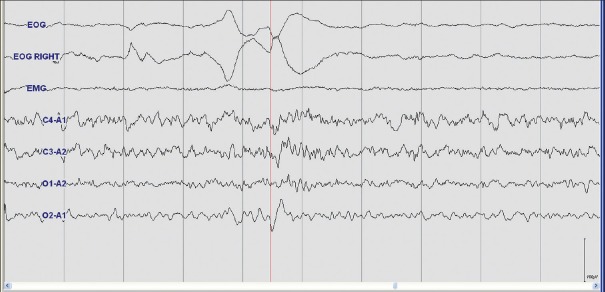
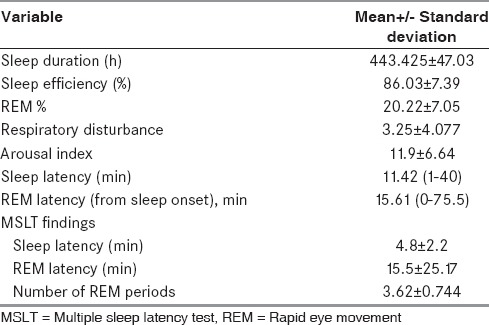
On PSG, there was no evidence of any respiratory event of significance. Sleep was fragmented in all patients. On MSLT, the mean sleep latency was found to be 4.8 min with a range from 11 s to 11 min. Eight (62%) out of 13 patients had two SOREMPs, three had three SOREMPs, and two had four SOREMPs on MSLT [Figure 1 and Table 2].
Figure 1.
Multiple sleep latency test showing sleep onset rapid eye movement - identified by the presence of rapid eye movements on electrooculogram, low electromyogram tone, and low amplitude mixed frequency electroencephalogram activity with sawtooth waves
Table 2.
Polysomnographic findings
All patients who were diagnosed as narcolepsy underwent neuropsychological assessment by a neuropsychologist with experience in sleep-related psychiatric issues. The family members of all the patients were counseled in detail about the symptoms and their consequences as well their impact on the quality of life of the patients. Nonpharmacological methods for combating daytime sleepiness like scheduled naps were explained and successfully incorporated into the routine of all patients. The timing of naps was adjusted according to the work/school schedules. The sustainability and long-term efficacy of these measures were ensured during periodic visits, telephonic interviews, and E-mail communication. However, two patients were lost to follow-up and repeated attempts to track them were unsuccessful. Two patients have resumed normal personal and social life with the help of nonpharmacological methods alone. The remaining patients were started on modafinil of which majority showed an excellent response after titrating the dose over a period of few weeks. Their daytime sleepiness and effect on the quality of life were reassessed to confirm and document the improvement. One patient deteriorated despite treatment with modafinil. His daytime sleepiness was still uncontrollable and bothersome for which he was initiated on methylphenidate which produced good but suboptimal benefit. Cataplexy showed an excellent response to treatment with 37.5–75 mg of venlafaxine. Nonpharmacological measures undertaken are elaborated in Table 1.
Discussion
The term “narcolepsy” originated from the French “narcolepsie,” a combined form of the Greek words “narke” (“numbness,” “stupor”) and “lepsis” (“an attack,” “seizure”), eloquently coined by Galineu himself.[1] As the manifold facets of the mystery continue to unfold even in this age, the scientific world seems to have come a long way in the diagnosis and management of this malady. However, resource limitations, as well as nonuniformity of clinical protocols, continue to challenge the developing world. Recent reports from our country have redirected the focus of the sleep medicine fraternity toward this treatable disorder of centrally mediated hypersomnolence. The presentation of our experience with narcolepsy with emphasis on diagnostic, as well as management aspects, we believe, will pave way for a more systematic- and consensus-based approach to the same in future.
The demographic characteristics showed an earlier age of presentation than seen in most Western studies, an observation similar to that made by the authors of a previous study from India.[7] Male predominance was noted, which has been almost universal finding in most studies. The mean duration of symptoms at the time of diagnosis (4.2 years) was comparable to other case series.[17,18] Wide variation in the duration of symptoms was evident in the retrospective data published by Gupta et al.[7] Several factors such as educational level, socioeconomic status, availability of medical resources, and the knowhow of sleep disorders among the medical professionals could all play important roles in determining the speed and ease of diagnosis. The phenotypic spectrum displayed in our sample was that of narcolepsy with cataplexy in three patients and without cataplexy in the remaining 11. Excessive daytime sleepiness and sleep attacks were a universal feature, but the other classical symptoms were seen in only a minority of patients. Seneviratne and Puvanendran reported cataplexy in 48%, sleep paralysis in 51, and hypnogogic hallucinations in 84%.[17] Gupta et al. found 40% of their patients to have cataplexy, while 70% had sleep paralysis.[7] Three of our patients had experiences in the night which they described as vivid dreaming in which they reported hearing words, being touched, and seeing vague indistinct images. The visual hallucinations in narcolepsy usually consist of simple forms (colored circles, parts of objects, and so forth) that are either constant or changing in size. The image of an animal or a person can occur abruptly and more often in color. Auditory hallucinations are also common although other senses are seldom involved. The auditory hallucinations can range from a collection of sounds to an elaborate melody. The patient may also be frightened by threatening sentences or harsh invectives. Another common and interesting type of hallucination reported at sleep onset involves elementary cenesthopathic feelings (i.e. experiencing picking, rubbing, or light touching), changes in location of body parts (e.g. arm or leg), or feelings of levitation or extracorporeal experiences (e.g. moving the body in space or floating above the bed) that may be quite elaborate. We need to reemphasize here that the absence of the other cardinal symptoms should not dissuade one from suspecting and investigating a patient for narcolepsy. The entity of monosymptomatic narcolepsy is also well established.[19] A detailed family history did not reveal clues to any of the members suffering from narcolepsy or other primary sleep disorder except probable sleep-related breathing disorder.[20] Previous studies have reported sleep disorders in up to 10% of first-degree relatives, which again probably reflects the lack of awareness or rather focus on the pivotal role of sleep and its distortions among our communities.
The PSG and MSLT findings in this study did not significantly deviate from prevalent observations.[7,8,9,10,11,12,13,14,15,16,17,18] They, however, reinforce the utility of these modalities in confirmation of the diagnosis, assessment of the severity of disease, as well as in the determination of the quantity and quality of sleep. On the overnight PSG, if there is an early onset of REM with or without sleep fragmentation coupled with the absence of an alternate sleep disorder to account for the patient's symptoms, an MSLT should be ordered to rule out the possibility of narcolepsy. An integral part of the message conveyed in this paper is the invaluable role of MSLT along with a consistent clinical picture in establishing the diagnosis. When the technical standards are adhered to and more definitive criteria are used, the specificity approaches 98%.[21] The other tools like HLA typing and CSF hypocretin levels although useful are not mandatory to make a positive diagnosis of narcolepsy.
Narcolepsy has one of the strongest known HLA association in the autoimmune arena, a variation of the HLA-DQB1 gene called HLA-DQB1*602 being the key feature. The finding is more common in the narcolepsy-cataplexy subtype.[3] In our series, only one of the four patients who tested positive for the allele suffered from cataplexy, while three of them had narcolepsy without cataplexy. Levels of CSF orexin/hypocretin-1 are another laboratory marker which has gained wider acceptance in recent years.[4,5] The investigation was not attempted in our patients due to the invasive nature of the procedure and nonavailability of the test in our country.
The negative impact the illness can have on the victim's professional, personal, and social life is insurmountable. Significant impairment of all domains of his quality of life has been echoed by many authors. Depending on the patients’ age and milieu, the brunt of impairment may be on school/work life, relationships, or functioning at home. The approach of spouse, family, peers at school or work, or society at large can hugely modify the person's ability to cope with the illness. Apart from this, many of these patients suffer from depression. Leisure activity is destined to decline with increasing daytime somnolence and sleep attacks.[22,23,24,25] Hence, there is a clear need to explore all these facets of the disease so that you can develop a comprehensive and holistic approach to management. A patient-based approach was followed in the management of each of our patients. Every attempt was made to harness the full potential of nonpharmacological interventions such as patient and family counseling, scheduled naps, as well as other behavioral and lifestyle modifications.[12,13,14,15] Two of our patients were restored to normalcy without drugs which underscore the central role of this often overlooked arm of narcolepsy management, which alone can be sufficient for milder forms of illness. Choice of pharmacotherapeutic agents was based on the symptomatology with modafinil being the most commonly used drug for excessive sleepiness and selective serotonin or serotonin-norepinephrine reuptake inhibitor for cataplexy.[26] A diagnostic scheme for diagnosis and management of narcolepsy is proposed [Figure 2].
Figure 2.
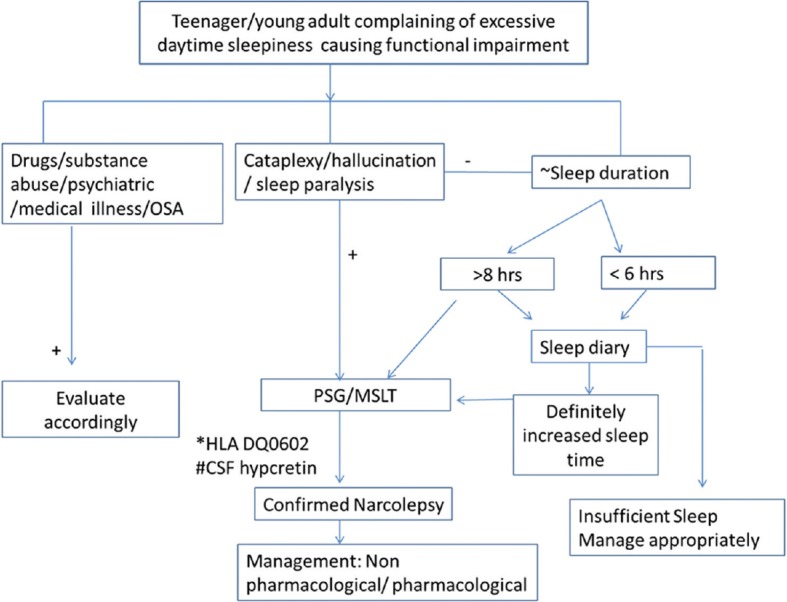
Algorithmic approach to diagnosis and management of narcolepsy. ~Sleep duration: Total hours of sleep/night; *Not mandatory for diagnosis; #Not available in India; OSA: Obstructive sleep apnea
Conclusion
Narcolepsy is a disorder of sleep with definite clinical and laboratory features which can be positively diagnosed and treated with the resources we have in our country. However, this requires a concerted effort to disseminate and reinstate scientific knowledge about this disorder among the general population and the medical community alike. The index of suspicion should be high for early diagnosis before the full-fledged clinical picture emerges. When astutely used overnight PSG and MSLT confirms the diagnosis in majority of patients and enables the clinician to embark on the management plan. Hence, this report is a step forward in understanding the clinical and diagnostic characteristics of narcolepsy, as well as the management strategies to combat its many torments that can be easily and systematically implemented. Nonpharmacological approaches combined with judicious use of carefully chosen therapeutic agents will ameliorate the majority of symptoms. Support from family and the society is of paramount importance in the fight against this seizure of sleepiness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Schenck CH, Bassetti CL, Arnulf I, Mignot E. English translations of the first clinical reports on narcolepsy and cataplexy by Westphal and Gélineau in the late 19th century, with commentary. J Clin Sleep Med. 2007;3:301–11. [PMC free article] [PubMed] [Google Scholar]
- 2.Mignot EJ. History of narcolepsy at Stanford University. Immunol Res. 2014;58:315–39. doi: 10.1007/s12026-014-8513-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mignot E, Hayduk R, Black J, Grumet FC, Guilleminault C. HLA DQB1 * 0602 is associated with cataplexy in 509 narcoleptic patients. Sleep. 1997;20:1012–20. [PubMed] [Google Scholar]
- 4.Kanbayashi T, Inoue Y, Chiba S, Aizawa R, Saito Y, Tsukamoto H, et al. CSF hypocretin-1 (orexin-A) concentrations in narcolepsy with and without cataplexy and idiopathic hypersomnia. J Sleep Res. 2002;11:91–3. doi: 10.1046/j.1365-2869.2002.00284.x. [DOI] [PubMed] [Google Scholar]
- 5.Nishino S, Ripley B, Overeem S, Lammers GJ, Mignot E. Hypocretin (orexin) deficiency in human narcolepsy. Lancet. 2000;355:39–40. doi: 10.1016/S0140-6736(99)05582-8. [DOI] [PubMed] [Google Scholar]
- 6.Longstreth WT, Jr, Koepsell TD, Ton TG, Hendrickson AF, van Belle G. The epidemiology of narcolepsy. Sleep. 2007;30:13–26. doi: 10.1093/sleep/30.1.13. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A, Shukla G, Goyal V, Srivastava A, Behari M. Clinical and polysomnographic characteristics in 20 North Indian patients with narcolepsy: A seven-year experience from a neurology service sleep clinic. Neurol India. 2012;60:75–8. doi: 10.4103/0028-3886.93602. [DOI] [PubMed] [Google Scholar]
- 8.Gupta R, Goel D, Farney R, Walker J. Narcolepsy: A case from India with polysomnographic findings. Neurol India. 2012;60:79–81. doi: 10.4103/0028-3886.93605. [DOI] [PubMed] [Google Scholar]
- 9.Bhatia M, Arif MA. Narcolepsy an often missed diagnosis:First documented case from India. Neurol India. 2009;57:509–11. doi: 10.4103/0028-3886.55588. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Sleep Medicine. International Classification of Sleep Disorders. International Classification of Sleep Disorders. Diagnostic and Coding Manual. 3rd ed. Chicago, Illinois: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 11.Littner MR, Kushida C, Wise M, Davila DG, Morgenthaler T, Lee-Chiong T, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28:113–21. doi: 10.1093/sleep/28.1.113. [DOI] [PubMed] [Google Scholar]
- 12.Mignot EJ. A practical guide to the therapy of narcolepsy and hypersomnia syndromes. Neurotherapeutics. 2012;9:739–52. doi: 10.1007/s13311-012-0150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mullington J, Broughton R. Scheduled naps in the management of daytime sleepiness in narcolepsy-cataplexy. Sleep. 1993;16:444–56. doi: 10.1093/sleep/16.5.444. [DOI] [PubMed] [Google Scholar]
- 14.Rogers AE, Aldrich MS, Lin X. A comparison of three different sleep schedules for reducing daytime sleepiness in narcolepsy. Sleep. 2001;24:385–91. doi: 10.1093/sleep/24.4.385. [DOI] [PubMed] [Google Scholar]
- 15.Morgenthaler TI, Kapur VK, Brown T, Swick TJ, Alessi C, Aurora RN, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30:1705–11. doi: 10.1093/sleep/30.12.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitler MM, Harsh J, Hirshkowitz M, Guilleminault C. Long-term efficacy and safety of modafinil (PROVIGIL((R))) for the treatment of excessive daytime sleepiness associated with narcolepsy. Sleep Med. 2000;1:231–43. doi: 10.1016/s1389-9457(00)00031-9. [DOI] [PubMed] [Google Scholar]
- 17.Seneviratne U, Puvanendran K. Narcolepsy in Singapore: Is it an elusive disease? Ann Acad Med Singapore. 2005;34:90–3. [PubMed] [Google Scholar]
- 18.Bassetti C, Aldrich MS. Idiopathic hypersomnia. A series of 42 patients. Brain. 1997;120(Pt 8):1423–35. doi: 10.1093/brain/120.8.1423. [DOI] [PubMed] [Google Scholar]
- 19.Šonka K, Šusta M, Billiard M. Narcolepsy with and without cataplexy, idiopathic hypersomnia with and without long sleep time: A cluster analysis. Sleep Med. 2015;16:225–31. doi: 10.1016/j.sleep.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 20.Honda Y, Asaka A, Tanimura M, Furosho T. A genetic study of narcolepsy and excessive daytime sleepiness in 308 families with a narcolepsy of hypersomnia proband. In: Guilleminault C, Lugaresi E, editors. Sleep/Wake Disorders. Natural History, Epidemiology, and Long-Term Evolution. New York: Raven; 1983. p. 187. [Google Scholar]
- 21.Arand D, Bonnet M, Hurwitz T, Mitler M, Rosa R, Bart Sangal R. The clinical use of the MSLT and MWT. Review by the MSLT and MWT Task Force of the Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 2005;28:123–44. doi: 10.1093/sleep/28.1.123. [DOI] [PubMed] [Google Scholar]
- 22.Daniels E, King MA, Smith IE, Shneerson JM. Health-related quality of life in narcolepsy. J Sleep Res. 2001;10:75–81. doi: 10.1046/j.1365-2869.2001.00234.x. [DOI] [PubMed] [Google Scholar]
- 23.Ozaki A, Inoue Y, Hayashida K, Nakajima T, Honda M, Usui A, et al. Quality of life in patients with narcolepsy with cataplexy, narcolepsy without cataplexy, and idiopathic hypersomnia without long sleep time: Comparison between patients on psychostimulants, drug-naïve patients and the general Japanese population. Sleep Med. 2012;13:200–6. doi: 10.1016/j.sleep.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 24.Vignatelli L, D’Alessandro R, Mosconi P, Ferini-Strambi L, Guidolin L, De Vincentiis A, et al. Health-related quality of life in Italian patients with narcolepsy: The SF-36 health survey. Sleep Med. 2004;5:467–75. doi: 10.1016/j.sleep.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Bayon V, Léger D, Philip P. Socio-professional handicap and accidental risk in patients with hypersomnias of central origin. Sleep Med Rev. 2009;13:421–6. doi: 10.1016/j.smrv.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 26.De la Herrán-Arita AK, García-García F. Current and emerging options for the drug treatment of narcolepsy. Drugs. 2013;73:1771–81. doi: 10.1007/s40265-013-0127-y. [DOI] [PubMed] [Google Scholar]