Abstract
Background
Hepatopancreatobiliary (HPB) surgery experience during residency in the Americas is limited. Residents interested in HPB surgery have different options available for further training. This study evaluated training in HPB surgery received during general surgery (GS) residency, and sought to determine the perception of fellowship training in HPB surgery.
Methods
An anonymous survey was distributed to all 259 GS residency programs in the United States. Questions evaluated demographics, program structure, overall training & HPB experience in particular during residency, plans for fellowship training and understanding of training in HPB surgery.
Results
Of the 340 respondents, 162 (48%) were from university programs, 145 (43%) from community hospitals and 48 (14%) from independent medical centers. 117 (34%) were residents in postgraduate year 4 or 5 (PGY4/PGY5). 275 (81%) respondents were planning to pursue fellowship training after finishing residency. Three quarters of all respondents did not feel comfortable about performing liver, biliary and pancreatic procedures. Fellowships accredited by the Americas Hepato-Pancreatico-Biliary Association (AHPBA) are the most common pathway considered by residents for HPB training.
Conclusions
GS residents are not comfortable in considering performing complex HPB cases on completion of residency training. GS residents consider AHPBA accredited fellowships to be more suitable for advanced training in HPB surgery.
Introduction
HPB surgery involves advanced surgical procedures of the liver, pancreas and biliary systems. The field of HPB surgery has matured significantly in the last 20 years and is now emerging as a separate discipline.1 HPB surgery is usually practiced by either a surgical oncologist, a transplant surgeon, HPB fellowship trained surgeon or a general surgeon without subspecialty training.
HPB surgeries have always been considered as challenging for general surgeons. These procedures require comprehensive knowledge, meticulous surgical technique and a good institutional support system.2 HPB surgery has been an integral part of general surgical residency training. In the United States, GS residents are required to undertake four liver resections, three pancreatic resections and 50 laparoscopic cholecystectomies, by the Accreditation council for Graduate Medical Education (ACGME).3 These numbers are not sufficient to be trained as a GS resident in the field of HPB surgery.2 However, there are residency programs where GS residents receive enough HPB training during their residency.4 The International Hepatopancreatobiliary Association (IHPBA) defines a HPB surgeon as an expert, who has received additional training and experience in the multidisciplinary management of hepatobiliary and pancreatic disease after GS residency.5
A recent survey of graduating senior residents showed that over 80% of respondents were pursuing fellowship training.6, 7 The most common reason cited was inadequate training during residency for advanced procedures. This is particularly true for HPB procedures, which are infrequently performed by residents and hence have resulted in the emergence and evolution of HPB fellowships.8 Advanced training in HPB surgery can be obtained through different pathways in North America. These include fellowships accredited by the Americas Hepato-Pancreatico-Biliary Association (AHPBA), the Society of Surgical Oncology (SSO) and the American Society of Transplant Surgeons (ASTS).
The purpose of this study is to determine the current level of training in HPB surgery received during GS residency in the United States and assess what residents think about advanced training in the field of HPB. This study proposed to identify the factors which are important for residents to choose one particular type of fellowship over other. We also sought to determine the perception of fellowship training in different tracks in HPB surgery in the United States among GS residents.
Methods
Study participants
All GS residency programs in the United States were invited to participate. The Survey was sent to program directors (PD's) and program coordinators (PC's) and requested to be forwarded to the residents in their program.
Survey
Survey questions were developed after review of current literature. The questions were converted to an online format and beta tested to ensure brevity, clarity, relevance and consistent interpretation. The survey was then refined, incorporating feedback from the beta test of the survey. Survey included 24 multiple choice questions. The survey queried demographics, program structure, overall training and HPB experience in particular during residency, plans for fellowship training and understanding of training in HPB surgery. The survey is summarized in Appendix A1.
An online platform (SurveyMonkey; SurveyMonkey Inc, Palo Alto, CA, USA) was utilized to deliver the survey. A link to a SurveyMonkey survey was e-mailed to all 259 PDs and PC's listed on the Association of Program Directors in Surgery website (www.apds.org). Reminder emails to encourage participation were distributed every two weeks. For a period of six weeks, three electronic mailings were completed every two weeks. Responses were captured anonymously to maintain confidentiality.
Statistical analysis
To summarize the data, descriptive statistical analysis were performed.
Results
Study population demographics
340 GS residents completed the online survey (Table 1). Off the respondents, 163 (48%) residents were from intermediate size residency programs. 115 (34%) from small size programs and 62 (18%) from large size programs.
Table 1.
Demographics of respondents
| Q1. Geographical location | |
| South | 58/340 (17%) |
| West | 32/340 (9%) |
| Northeast | 123/340 (36%) |
| Midwest | 125/340 (37%) |
| Q2. Current year of clinical training | |
| PGY1 | 61/340 (18%) |
| PGY2 | 69/340 (20%) |
| PGY3 | 93/340 (27%) |
| PGY4 | 55/340 (16%) |
| PGY5 | 62/340 (18%) |
| Q3. Type of institution | |
| University hospital | 162/340 (48%) |
| Community with university affiliation | 145/340 (43%) |
| Independent medical center | 48/340 (14%) |
| Military medical center | 4/340 (1%) |
| NIH designated cancer center | 6/340 (2%) |
| Q4. Number of chief residents | |
| 1–3 | 116/340 (34%) |
| 4–6 | 164/340 (49%) |
| >6 | 60/340 (18%) |
| Q5. Years of training in your residency | |
| 5 | 255/340 (75%) |
| 6–7 | 83/340 (25%) |
| 8–10 | 2/340 (1%) |
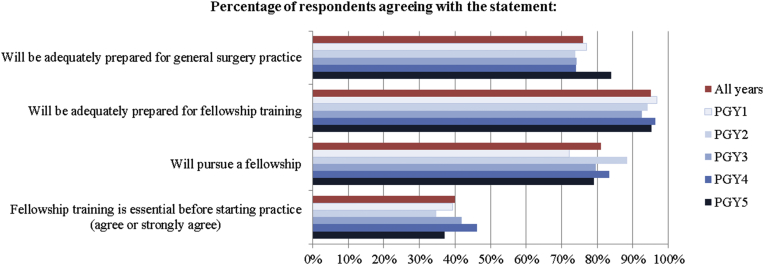
Fellowship training
275 respondents (81%) were planning to pursue fellowship training after finishing GS residency (Table 2). Three quarters felt residency prepared them adequately for GS practice immediately following graduation and almost all felt residency prepared them adequately for any further fellowship training following residency. When asked to respond to the question “Do you think fellowship training is essential before starting practice?” 40% respondents agreed and 32% respondents disagreed. The percentage of respondents planning to pursue fellowship training relative to PGY level is shown in Fig. 1.
Table 2.
Fellowship training
| Q6. Plans of pursuing fellowship after general surgery training | |
| Yes | 275/340 (81%) |
| No | 65/340 (19%) |
| Q7. Do you feel residency will adequately prepare you for general surgery practice | |
| Yes | 262/340 (77%) |
| No | 78/340 (23%) |
| Q8. Do you feel residency will adequately prepare you for fellowship training | |
| Yes | 323/340 (95%) |
| No | 17/340 (5%) |
| Q9. Is fellowship training essential before starting practice | |
| Strongly agree | 44/340 (13%) |
| Agree | 92/340 (27%) |
| Neutral | 94/340 (28%) |
| Disagree | 72/340 (21%) |
| Strongly disagree | 38/340 (11%) |
| Q10. Plans to pursue which type of fellowship | |
| Surgical oncology | 35/275 (13%) |
| Hepatobiliary | 18/275 (7%) |
| Transplant | 12/275 (4%) |
| MIS/Bariatric | 38/275 (14%) |
| Colorectal | 23/275 (8%) |
| Trauma & Critical care | 42/275 (15%) |
| Endocrine | 6/275 (2%) |
| Breast | 14/275 (5%) |
| Vascular | 27/275 (10%) |
| Cardiothoracic | 25/275 (9%) |
| Plastics | 16/275 (6%) |
| Pediatrics | 13/275 (5%) |
| Others | 6/275 (2%) |
| Q11. Number of respondents who had different fellowships available at host institution | |
| Surgical oncology | 18/340 (5%) |
| Breast | 38/340 (11%) |
| Liver transplant | 76/340 (22%) |
| Kidney transplant | 80/340 (24%) |
| HPB | 51/340 (15%) |
| MIS/Bariatric | 133/340 (39%) |
| Colorectal | 89/340 (26%) |
| Endocrine | 40/340 (12%) |
| Vascular | 164/340 (48%) |
| Pediatric | 46/340 (14%) |
| Cardiothoracic | 98/340 (29%) |
| Plastics | 85/340 (25%) |
| Trauma & Critical care | 119/340 (35%) |
| Others | 7/340 (2%) |
Figure 1.
Description of respondent need for fellowship training
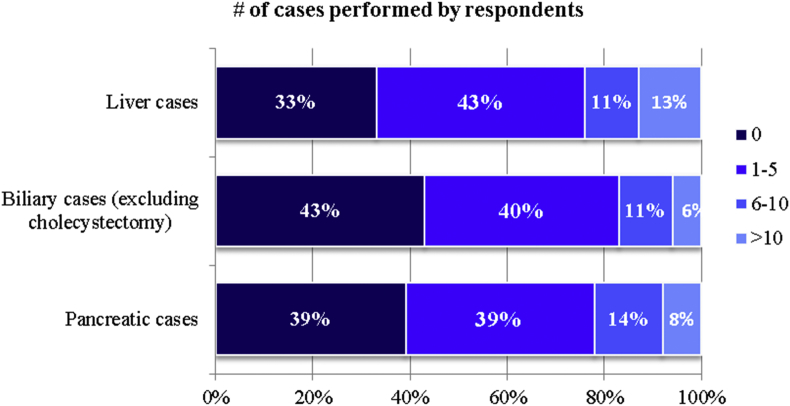
HPB surgery training
The description of respondent HPB case volume by respondents is summarized in Fig. 2.
Figure 2.
Description of respondent HPB case experience during residency
Three quarters of all respondents did not feel comfortable about performing liver, biliary and pancreatic procedures after residency.
The principal reason given for selecting a HPB fellowship was to learn technically demanding and complex nature of HPB cases. More than 40% respondents thought mentorship played an important role (Table 3).
Table 3.
HPB training
| Q13. Liver cases performed | |
| 0 | 112/340 (33%) |
| 1–5 | 143/340 (42%) |
| 6–10 | 37/340 (11%) |
| >10 | 45/340 (13%) |
| Don't know | 3/340 (1%) |
| 14. Biliary cases excluding cholecystectomies performed | |
| 0 | 145/340 (43%) |
| 1–5 | 132/340 (39%) |
| 6–10 | 37/340 (11%) |
| >10 | 20/340 (6%) |
| Don't know | 6/240 (2%) |
| Q15. Pancreatic cases performed | |
| 0 | 132/340 (39%) |
| 1–5 | 132/340 (39%) |
| 6–10 | 46/340 (14%) |
| >10 | 26/340 (8%) |
| Don't know | 4/340 (1%) |
| Q16. What types of fellowship to seek for training in HPB | |
| Surgical oncology | 160/430 (37%) |
| Liver transplant | 55/430 (13%) |
| HPB | 214/430 (50%) |
| Q17. If planning to pursue other fellowships, reasons behind your selection | |
| Interest | 227/263 (86%) |
| More defined path of training | 63/263 (24%) |
| Job security | 63/263 (24%) |
| Lifestyle | 117/263 (44%) |
| Length of fellowship | 56/263 (21%) |
| Geographic location | 20/263 (8%) |
| Other factors | 10/263 (4%) |
| Q18. In home institution, who performs HPB cases | |
| Surgical oncologist | 212/337 (63%) |
| Transplant surgeon | 150/337 (45%) |
| HPB fellowship trained surgeon | 168/337 (50%) |
| General surgeons | 169/337 (50%) |
| None | 6/337 (2%) |
| Q19. Comfortable in performing liver procedures directly after residency | |
| Yes | 78/339 (23%) |
| No | 261/339 (78%) |
| Q20. Comfortable in performing biliary procedures directly after residency | |
| Yes | 76/339 (23%) |
| No | 262/339 (78%) |
| Q21. Comfortable in performing pancreatic procedures directly after residency | |
| Yes | 93/339 (28%) |
| No | 246/339 (73%) |
| Q22. If considering training in HPB, what are factors behind your selection | |
| Technical demanding and complexity of procedures | 131/151 (87%) |
| Care of complex patients | 86/151 (57%) |
| Job security | 10/151 (7%) |
| Life style | 13/151 (9%) |
| Geographical location | 6/151 (4%) |
| Mentorship at your institution | 62/151 (41%) |
| Other factors | 5/151 (3%) |
| Q23. What are requirements of training in HPB Surgery | |
| Good technical experience | 305/332 (92%) |
| Care of complex patients | 267/332 (80%) |
| Mentorship | 204/332 (61%) |
| Minimally invasive training | 99/332 (30%) |
| Training at high volume centers | 296/332 (89%) |
| Others | 7/332 (2%) |
| Q24. Important factors to achieve good outcomes in HPB surgery | |
| Fellowship training of surgeon | 135/332 (40%) |
| Volume of hospital | 217/332 (65%) |
| Volume of surgeon | 278/332 (83%) |
| Experience of surgeon | 307/332 (92%) |
| Other factors | 11/332 (3%) |
50% respondents expressed a preference for an AHPBA fellowship, whereas 37% would choose a SSO fellowship. Respondents thought adequate fellowship training in HPB surgery should include good technical experience, care of complex patients, training at high volume center, excellent mentorship and exposure to minimally invasive techniques.
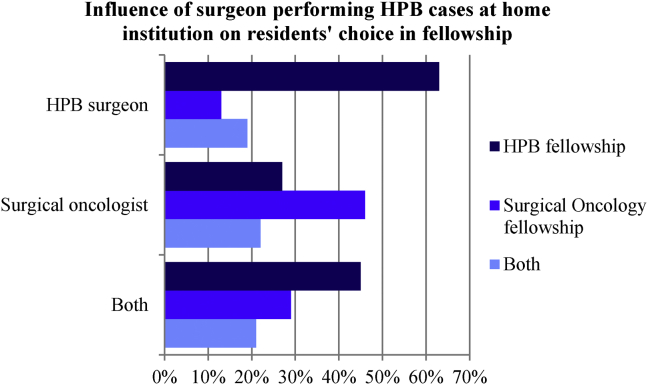
At the host institutions of respondents, HPB procedures were performed by all surgical specialists. The fellowship track chosen for HPB training did depend on surgeons performing HPB cases at the host institution (Fig. 3).
Figure 3.
Choice of fellowship depending on who performs HPB cases at home institution
Respondents thought outcomes in HPB surgeries were affected by the experience of surgeon, surgical volume, and volume of hospital and prior fellowship training of the surgeon.
Discussion
HPB surgery is considered an essential part of GS training. Most HPB procedures are performed by fellowship trained HPB surgeons, surgical oncologists and transplant surgeons. The graduating GS resident in 2012 only performed a mean of 9.4 ± 3.4 liver, 11.3 ± 4.3 pancreas, and 3.8 ± 2.1 biliary operations excluding cholecystectomy.9
This study was carried out with the goal of establishing how GS residents feel about HPB training and what they think about fellowship training in HPB field. Our study also concurred that GS residents receive limited HPB training during residency, which is not enough to perform HPB cases following training. About 30% residents felt they will be comfortable performing HPB cases. We believe this could be due to lack of understanding of the nuances of complex HPB procedures. However, residents graduating from HPB heavy programs may feel comfortable in performing certain types of HPB procedures. We think PD's should try to maximize the exposure of residents to these complicated cases. Exposure to these complex cases help residents to develop their skills, regardless of the practice they choose in future. If programs do not enough of these procedures, arranging for an external rotation may help. The Flexibility in Surgery training, which has been approved by the American Board of Surgery allows GS residents up to 12 months of flexible rotations within PGY3–5 years so as to tailor training to the resident's future career interests. It would appear that this option should be implemented more often.
Previous studies had identified more than 80% of GS residents seek fellowship training after graduation.6 Our study also identified that more than 80% respondents were planning to pursue fellowship training on completion of GS residency. However, three of every four residents felt that they will be adequately prepared to take GS practice after completion of residency. Furthermore, only 40% thought that fellowship training is essential before starting practice. This disparity may result from GS residents believing that completing a fellowship will give them a career advantage. On the other hand, they may feel it is now expected that they should be fellowship trained, even though they do not consider this necessary. Furthermore, the residents seeking to pursue fellowship training may be adequately prepared for GS practice but want to specialize in other fields. Friedell and colleagues also reported that, of the graduating GS chief residents pursuing fellowship training, 67% of the graduating GS chief residents pursue fellowship training because of a genuine interest in that specialty.10
The current state of training in HPB surgery in North America is defined through three pathways.11 These offer variable experiences in pancreas, liver and biliary cases, and each pathway offers unique training foci.12 In this study, an AHPBA rather than a SSO fellowship was the preferred pathway for residents who seek training in HPB surgery. Our study found that the type of fellowship pathway chosen by residents for HPB training depends on who performs these cases at host institutions. This may be due to the mentorship provided by the faculty at these institutions and 40% residents actually identified mentorship as an important factor in deciding fellowship. The principal reason to choose training in HPB surgery was to learn technically demanding and complex nature of HPB cases. Respondents agree that fellowship training programs in HPB surgery should provide adequate exposure to these complex cases, along with mentorship by training faculty.
The main study limitation includes the relatively small sample of responding GS residents. However, this has been a chronic problem with surveys conducted through PD's. The respondent group seems to be representative of entire GS residents, as it has a similar percentage of residents from each PGY level of training and a similar distribution from university and community programs. The survey-based acquisition of data has an inherent limitation in that it reflects the subjective opinions of respondents and is also subject to recall bias. Nonetheless, it adds to the current overview of residency and fellowship training, delivering useful insight into the thinking of training surgeons and their aspirations in regard to independent practice in HPB surgery.
In conclusion, GS residents are not comfortable in performing HPB procedures after graduation from residency. The majority of GS residents wish to pursue fellowship training after completion of residency. US residents consider AHPBA fellowships to be more suitable for advanced HPB training. The main reason behind pursuing training in HPB surgery is to learn the technically demanding and complex nature of HPB cases. Mentorship also plays an important role in selection of the fellowship.
Conflicts of interest
None declared.
Appendix A1. Survey
-
1.What is your geographic Location?
-
•South
-
•West
-
•Northeast
-
•Midwest
-
•
-
2.Current year of clinical training?
-
•PGY1
-
•PGY2
-
•PGY3
-
•PGY4
-
•PGY5
-
•
-
3.Which of the following describes your institution? (Check all that apply)
-
•University hospital
-
•Community hospital with university affiliation
-
•Independent medical center
-
•Military medical center
-
•NIH designated cancer center
-
•
-
4.How many chief residents are in your program?
-
•1–3
-
•4–6
-
•>6
-
•
-
5.How many years of training is your residency?
-
•5
-
•4–6
-
•>6
-
•
-
6.Are you planning to pursue fellowship after general surgery training?
-
•Yes
-
•No
-
•
-
7.Do you feel general surgery residency will adequately prepare you for general surgery practice immediately following graduation?
-
•Yes
-
•No
-
•
-
8.Do you feel general surgery residency will adequately prepare you for fellowship training immediately following graduation?
-
•Yes
-
•No
-
•
-
9.Do you think fellowship training is essential before starting practice?
-
•Strongly agree
-
•Agree
-
•Neutral
-
•Disagree
-
•Strongly disagree
-
•
-
10.If you are planning to pursue fellowship, which one?
-
•Surgical oncology
-
•Hepatobiliary
-
•Transplant surgery
-
•MIS/Bariatric
-
•Colorectal
-
•Trauma critical care
-
•Endocrine
-
•Breast
-
•Vascular
-
•Cardiothoracic
-
•Plastics
-
•Pediatrics
-
•Other (please specify)
-
•
-
11.Are any of following fellowships available at your institution? (Check all that apply)
-
•Surgical oncology
-
•Breast
-
•Liver transplant surgery
-
•Kidney transplant surgery
-
•Hepatopancreatobiliary fellowship
-
•MIS/Bariatric
-
•Colorectal
-
•Endocrine
-
•Vascular
-
•Pediatric
-
•Cardiothoracic
-
•Plastics
-
•Trauma critical care
-
•Other (please specify)
-
•
-
12.
In your opinion, what constitutes Hepatopancreatobiliary (HPB) surgery?
-
13.How many major liver cases have you done so far?
-
•0
-
•1–5
-
•6–10
-
•>10
-
•I don't know
-
•
-
14.How many major biliary cases (excluding cholecystectomy) have you done so far?
-
•0
-
•1–5
-
•6–10
-
•>10
-
•I don't know
-
•
-
15.How many pancreatic cases have you done so far?
-
•0
-
•1–5
-
•6–10
-
•>10
-
•I don't know
-
•
-
16.If you were to train and practice in hepatobiliary surgery, which type of fellowship would you seek? (Check all that apply)
-
•Surgical oncology
-
•Liver transplant
-
•Hepatopancreatobiliary surgery
-
•Other (please specify)
-
•
-
17.If you are planning to pursue another fellowship (Like colorectal, plastics breast, endocrine, thoracic), what are the reasons behind your selection? (Check all that apply)
-
•Interest
-
•More defined path of training
-
•Job security
-
•Lifestyle
-
•Length of fellowship
-
•Geographical location
-
•Other (please specify)
-
•
-
18.In your home institution, which surgeons perform hepatobiliary cases? (Check all that apply)
-
•Surgical oncologist
-
•Transplant surgeons
-
•HPB fellowship trained surgeons
-
•General surgeons
-
•None
-
•Other (please specify)
-
•
-
19.If you were to enter general surgery practice directly from residency, would you feel comfortable performing liver procedures?
-
•Yes
-
•No
-
•
-
20.If you were to enter general surgery practice directly from residency, would you feel comfortable performing complex biliary procedures (excluding cholecystectomy)?
-
•Yes
-
•No
-
•
-
21.If you were to enter general surgery practice directly from residency, would you feel comfortable performing pancreatic procedures?
-
•Yes
-
•No
-
•
-
22.If you are considering training in HPB, what are the factors behind your selection? (Check all that apply)
-
•Technical demanding and complexity of HPB cases
-
•I like taking care of complex patients
-
•Job security
-
•Life style
-
•Geographical location
-
•Mentorship at your program
-
•Other (please specify)
-
•
-
23.What do you think is required during training to make someone qualified to perform advanced HPB procedures? (Check all that apply)
-
•Good technical experience
-
•Care of complex patients
-
•Mentorship
-
•Minimally invasive training
-
•Training at high volume center
-
•Other (please specify)
-
•
-
24.In your opinion what factors are important to achieve good outcomes in HPB surgery? (Check all that apply)
-
•Prior fellowship training of surgeon
-
•Volume of hospital
-
•Volume of surgeon
-
•Experience of surgeon
-
•Other (please specify)
-
•
References
- 1.Dixon E., Vollmer C.M., Jr., Bathe O., Sutherland F. Training, practice, and referral patterns in hepatobiliary and pancreatic surgery: survey of general surgeons. J Gastrointest Surg. 2005;9:109–114. doi: 10.1016/j.gassur.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Chang Y.J., Mittal V.K. Hepato-pancreato-biliary training in general surgery residency: is it enough for the real world? Am J Surg. 2009;197:291–295. doi: 10.1016/j.amjsurg.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. Defined category minimum numbers: General Surgery. Available at: www.ACGME.org (last accessed 4 Jan 2016).
- 4.Daee S.S., Flynn J.C., Jacobs M.J., Mittal V.K. Analysis and implications of changing hepatopancreatobiliary (HPB) case loads in general surgery residency training for HPB surgery accreditation. HPB. 2013;15:1010–1015. doi: 10.1111/hpb.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International Hepato-Pancreato-biliary Association. Standards for Hepato-Pancreato-biliary Training. Available at: http://www.ihpba.org/media/hpb_training_standards.pdf. (last accessed 4 April 2016).
- 6.Borman K.R., Vick L.R., Biester T.W., Mitchell M.E. Changing demographics of residents choosing fellowships: longterm data from the American Board of Surgery. J Am Coll Surg. 2008;206:782–788. doi: 10.1016/j.jamcollsurg.2007.12.012. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 7.Stitzenberg K.B., Sheldon G.F. Progressive specialization within general surgery: adding to the complexity of workforce planning. J Am Coll Surg. 2005;201:925–932. doi: 10.1016/j.jamcollsurg.2005.06.253. [DOI] [PubMed] [Google Scholar]
- 8.Rassadi R., Dickerman R.M., Dunn E.L., Tarnasky P.R., Linder J.D., Mejia M.A. Hepatopancreaticobiliary (HPB) surgery: what is the right fellowship for the right training? J Surg Educ. 2008;65:186–190. doi: 10.1016/j.jsurg.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Sachs T.E., Ejaz A., Weiss M., Spolverta G., Ahuja N., Makary M.A. Assessing the experience in complex hepatopancreatobiliary surgery among graduating chief residents: is the operative experience enough? Surgery. 2014;156:385–393. doi: 10.1016/j.surg.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedell M.L., VanderMeer T.J., Cheatham M.L., Fuhrman G.M., Schenarts P.J., Mellinger J.D. Perceptions of graduating general surgery chief residents: are they confident in their training? J Am Coll Surg. 2014;218:695–703. doi: 10.1016/j.jamcollsurg.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 11.Jeyarajah D.R., Berman R.S., Doyle M., Geevarghese S.K., Posner M.C., Farmer D. Consensus Conference on North American training in hepatopancreaticobiliary surgery: a review of the Conference and Presentation of Consensus Statements. Ann Surg Oncol. 2016;23:2153–2160. doi: 10.1245/s10434-016-5111-9. [DOI] [PubMed] [Google Scholar]
- 12.Warner S.G., Alseidi A.A., Hong J., Pawlik T.M., Minter R.M. What to expect when you're expecting a hepatopancreatobiliary surgeon: self-reported experiences of HPB surgeons from different training pathways. HPB. 2015;17:785–790. doi: 10.1111/hpb.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]