Highlights
-
•
A very rare type of retroperineal malignant cyst tumor is presented on two cases.
-
•
A very rare type of Mesothelioma tumor is presented on two cases.
-
•
A minimal invasive type of treatment is proposed instead of the regular open surgery.
-
•
A small literature review was performed.
Keywords: Retroperitoneum, Cysts, Laparoscopy, Mesothelioma
Abstract
Retroperitoneal cystic mesothelioma is a very rare lesion. The pathogeny is unclear and establishing a preoperative diagnosis versus others retroperitoneal cystic lesions is difficult.
Thus, with increasing experience in laparoscopic retroperitoneal surgery, the use of this approach for exploration of a retroperitoneal mass of unknown origin may provide an alternative to classic open surgery and all the benefits of laparoscopy. We present two cases treated laparoscopycally and review the literature.
1. Introduction
When identifying retroperitoneal cystic lesions, differential diagnosis must include mesenteric, omental and splenic cysts, enteric duplication cysts, and lesions originated in retroperitoneal organs, such as pancreas, kidneys or adrenal glands. Retroperitoneal cystic mesothelioma (CM) is a very rare lesion, usually originated in the peritoneal lining of pelvic organs, whose natural history differs from that of malignant mesothelioma [1], [2].
Pathogenesis of the CM is controversial, as it has been traditionally considered a benign lesion, but has a potential risk of malignancy [2], [3], [4]. It is more frequent in middle aged women and clinical features are non-specific [2], [5]. In spite of the development of multiple imaging techniques, preoperative diagnosis is difficult to achieve. Treatment of choice is complete surgical resection, either through laparoscopy or laparotomy, to avoid the risk of local recurrence. We present two cases laparoscopycally treated, and a review of the literature.
2. Clinical cases
2.1. Case 1
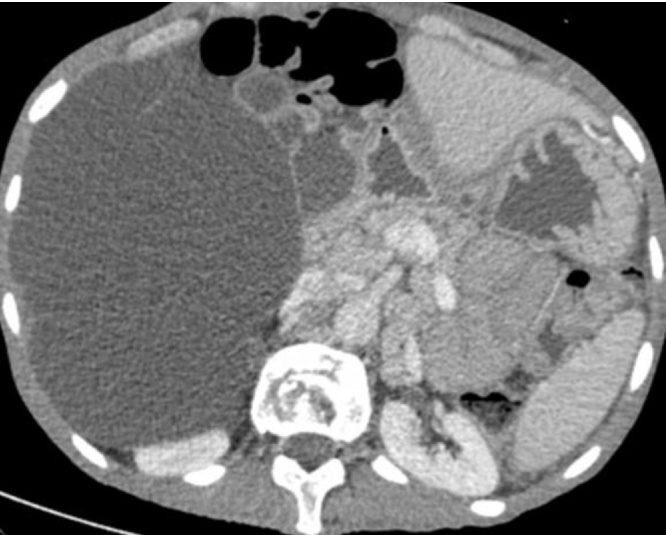
49 year old man, mentally retarded, admitted in hospital after a hip fracture. Marked leucocytosis is identified in blood analysis, so the department of Haematology studies the patient in search of a lymphoproliferative disease. The patient has neither fever nor digestive symptoms; the abdominal exam shows a palpable mass in the right flank. Computed tomography (CT) scan identifies a large cystic, lobulated lesion (19 × 13.5 × 30 cm) in the right abdomen, with thin septa and no calcifications or solid areas inside (Fig. 1) in close contact with the liver and the inferior renal pole, displacing the right colon and intestinal loops forward and to the left. A simple hepatic cyst is suspected preoperatively and surgery is indicated for the risk of rupture. The abdomen is accessed laparoscopically, with the patient in the French position, using a Veress needle, a 30° optics and three trocars (two 5 mm and one 10 mm). No intraperitoneal masses are seen and a very large, multiloculated retroperitoneal cyst is identified, in contact with the right adrenal gland, the VI hepatic segment and the ascending colon. After reducing the size of the cyst by percutaneous puncture and aspiration, it is dissected from adjacent structures with the harmonic ultrasound device; endoclips are used to separate it from fibrotic posterior adhesions, probably corresponding to the cyst́s origin. The specimen is extracted in a plastic bag. A suction drain is left and removed on the second postoperative day. Surgical time is 90 min. The patient has a favourable course and is discharged on the third day.
Fig. 1.
Abdominal CT scan. A septated cystic lesion of 19 cm on the abdominal right flank, displacing the intestinal loops, contacting with the hepatic right lobe and gall bladder.
Pathologic study reveals a cystic structure, coated with mesothelial flat cells, focally reactive and without malignancy. The specimen is walled by a dense fibrous tissue, with hyaline areas and lymphocytes.
Two years after surgery the patient remains asymptomatic and there is no recurrence on CT scan.
2.2. Case 2
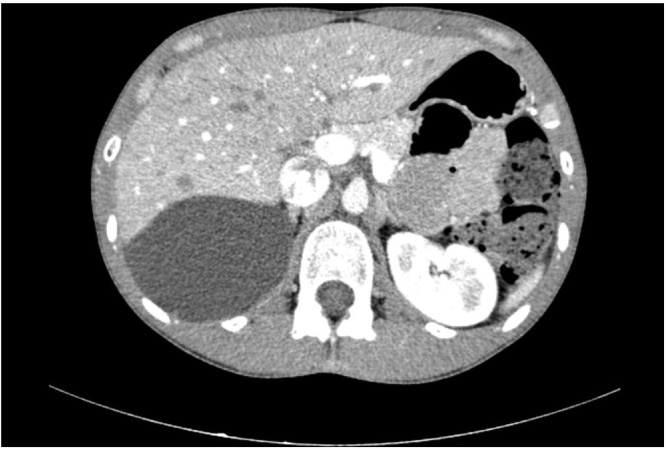
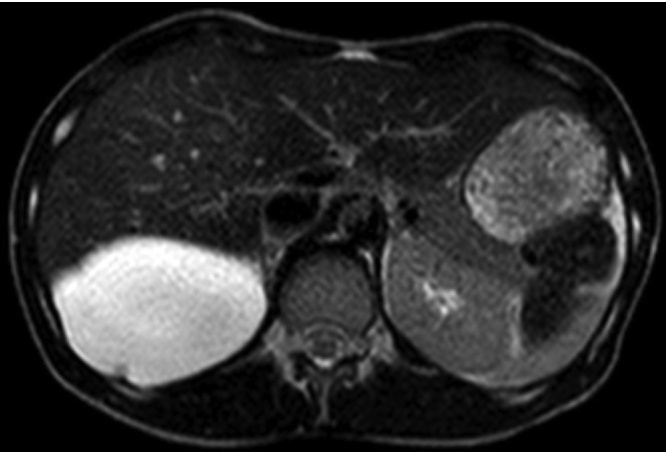
28 year old woman attended on outpatient clinic for profuse nocturnal sweating, without other symptoms. She has no history of previous surgery. There are no palpable masses on abdominal examination. On blood analysis, high levels of lactate dehydrogenase (LDH) are found, so an abdominal ultrasound is performed and a cystic retroperitoneal subhepatic, well delimited cystic mass is found, measuring 8 cm in diameter. The CT scan shows a cystic retroperitoneal lesion of 9, 4 cm, non-enhancing after venous contrast, with a short septum and without malignancy criteria (Fig. 2). The organ of origin (liver, right kidney or adrenal gland) cannot be established. On MRI, a 11 × 9 × 5 cm retrohepatic septated cystic lesion with homogeneous fluid content, without nodular enhancement or solid intralesional component, with low signal intensity on T1 and high signal intensity on T2 is found (Fig. 3). Given the lack of diagnosis after imaging studies, surgery is planned. Laparoscopic approach is similar to previously described in case 1 and complete excision of a large retroperitoneal right subphrenic cyst, with firm adhesions to the diaphragm, is performed. As no malignant signs were found on preoperative studies, percutaneous controlled needle aspiration is done before removal of the specimen inside a plastic bag. A suction drain is left in place for two days. Operative time is 140 min.
Fig. 2.
Abdominal CT scan. A septated cystic tumor of 9,4 cm with apparent no visceral relation.
Fig. 3.
Abdominal MRI. Homogenous cyst of 11 cm on the subphrenic right retroperitoneum.
The patient has an appropriate postoperative course and is discharged on the fourth day. Pathological study reveals a cystic lesion walled with fibrous tissue, with a cuboidal epithelial benign lining, consistent with a mesothelioma. On twelve monthś follow up she remains symptom free and no recurrence is found on CT scan.
3. Discussion
Retroperitoneal neoplasms are usually malignant and solid in nature (70–80%) [5]. Retroperitoneal cysts are rare, usually benign, and account for the 14.5% of cystic abdominal lesions [6]. According to Kurtz et al., incidence of retroperitoneal cysts is two cases for every million hospital admissions [6].
Primary retroperitoneal cystic lesions (PRCL) need to be differentiated both from cysts arising from retroperitoneal organs, such as pancreas, kidneys or adrenal glands, and from intraabdominal cysts, such as mesenteric, omental or splenic cysts, and duplication enteric cysts. Malignant PRCL such as mucinous cystadenoma and cystadenocarcinoma, pseudomyxoma retroperitonei and solid neoplasms with cystic transformation (leiomyosarcoma, paraganglioma), are rare [5], [7], [8], [9], [10]. On the contrary, a wide variety of benign retroperitoneal cystic lesions has been described [5], [8], [9], [10], [11], [12], [13], [14], [15], such as müllerian cyst, hydatid cyst, lymphangioma, cystic mesothelioma, cystic teratoma, tailgut cyst, epidermoid cyst, post-traumatic pseudocyst, lymphocele following abdominal surgery, urinoma, hematoma and bronchogenic subdiaphragmatic cyst.
Cystic mesothelioma is rare among retroperitoneal cystic lesions. Mesotheliomas arise from the serosal lining of pleura, pericardium and peritoneum [2]. Around a third of all mesotheliomas are located in the abdomen [16], where two different clinicopathologic variants have been described: well-differentiated papillary mesothelioma and multicystic mesothelioma [2]. Although traditionally considered as benign lesions, they have a low degree of malignancy and unlike malignant mesothelioma, they have no relation with asbestos exposure [4], [5], [10]. Peritoneal multicystic mesothelioma (CM) was first described by Mennemayer and Smith in 1979 [1]. From then on, around 150 cases have been reported in literature, although most reports refer to isolated cases or short series, the majority of them intraabdominal in location, what makes the precise incidence of retroperitoneal lesions difficult to establish [10], [17]. In a review of 25 peritoneal mesotheliomas, Ross et al., reported that 16% of them where retroperitoneal [18].
Pathogenesis of CM remains controversial. Some authors consider it an inflammatory reactive lesion, because 30% of the patients have a history of abdominal surgery or abdominal inflammatory chronic disease [2], [3]. Others support that unilocular CMs are due to an embryologic mis-development, because of the failure to coalescence of the posterior peritoneum sheets following intestinal rotation; consequently, this cysts would have no potential to recur [18]. The most accepted theory is that which considers CM a relatively benign neoplastic lesion, because most patients have no previous surgery or no history of abdominal inflammatory diseases, epithelial cells in the cysts have shown adenomatous changes an squamous methaplasia on histhologic analysis, half of the patients treated with partial resections have recurred and an indolent progressive growth of the lesions has been described in patients not undergoing surgery; even exceptional reports of malignant transformation with no local invasion or distant metastasis have been made [2], [4], [5], [9], [10], [19].
CM occurs predominantly in middle aged women. Unspecific abdominal pain is the most common symptom, although patients are usually asymptomatic and diagnosis is incidental [2], [5]. Ultrasound usually shows an anechoic multiseptated lesion [20]. CT scan is the imaging technique of choice for diagnosis. It demonstrates relations with surrounding structures, usually respecting adjacent organs, and shows a uni or multiloculated cyst, with a thin wall, with neither hemorrhage nor fat, calcifications or solid nodules, with an average size of 13 cm [5], [20], [21]. On MRI, CM typically shows low signal intensity on T1 and high signal intensity on T2, with minimal to mild peripheral and septal enhancement after IV contrast administration [20]. Its most common location is in the pelvis and differential diagnosis has to be made mainly with cystic lymphangioma [2], [17], [18], [19], [20], [21], [22]. Cysts located in the superior part of the retroperitoneum may be difficult to differentiate from simple renal, adrenal or hepatic cysts, as it occurred with our two cases.
Cytology of percutaneously aspirated fluid may show mesothelial cells; however, diagnostic efficiency is low for preoperative diagnosis, as it is with plasmatic and intracystic tumor markers [23]. Percutaneous needle aspiration and instillation of sclerosing agents has been described in the treatment of very large cysts, but recurrence rate is high, so it should only be used for symptomatic patients with a high surgical risk [3], [23]. The treatment of choice for CM is complete surgical resection, either through laparoscopy or laparotomy. Laparoscopy is more widespread and accepted for the treatment of cystic rather than solid retroperitoneal tumors [24]. However, laparoscopic excision of retroperitoneal CM has rarely been reported in literature [3], [17], most probably because of the large size of the tumors and the difficulty to exclude malignancy preoperatively. We used a four trocar approach in our two cases, although surgery can be done with three [3], [24]. Dissection from adjacent structures is quite easy during surgery, though incidental cyst rupture is not infrequent, due to its thin wall. Intraoperative aspiration of the lesion makes it easier to manipulate and reduces the risk of rupture and spillage of the cyst́s content [23], which most often consists of a clear serous fluid, but sometimes can be mucinous or gelatinous material [17], [18], [19]. Laparoscopic approach provides all the proven benefits of minimally invasive surgery (minimum morbidity, better cosmetic results, less pain and quicker recovery), though surgical time may be slightly superior (106 min average) to laparotomy. This is why we consider laparoscopic complete resection should be the treatment of choice for retroperitoneal CM. Only in cases when malignancy is highly suspected, laparotomy should be performed, in order to assure complete excision of the lesion and to avoid spillage of the cyst́s content, risking intraperitoneal or trocar site recurrence [4], [7]. Prognosis after complete resection is usually favourable, although long term follow up must be made, to exclude local recurrence.
In conclusion, retroperitoneal CM is a rare lesion, traditionally considered benign, though some cases of malignant transformation have been reported. Preoperative differential diagnosis with other retroperitoneal lesions is difficult to achieve. Laparoscopy is a valid and safe approach for highly suspected benign cystic retroperitoneal mesothelioma, as it allows complete excision and a favourable prognosis, given all the benefits proven for laparoscopy.
Conflict of interest
There is no financial or contractual relation between any of the author that may be considered a conflict of interest.
Funding
There is no sponsor of the present study. It was done as a part of the regular care of a patient in our institution.
Ethical approval
It was an observational case description of the treatment of a patient following clinical guides, so no Ethical Approval was needed.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contribution
C. García: writing the paper, paper preparation, images editing, paper formatting, patient care.
C. astellon: paper preparation, images editing, paper formatting, patient care.
Rest of authors: patient care, paper preparation contribution.
Guarantor
Carlos García Vasquez.
Camilo Castellon.
References
- 1.Mennemayer R., Smith M. Multicystic peritoneal mesothelioma: a case report with electron microscopy of a case mimicking intraabdominal cystic higroma (lymphangioma) Cancer. 1979;44:692–698. doi: 10.1002/1097-0142(197908)44:2<692::aid-cncr2820440242>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Weiss S., Tavassoli F.A. ystic mesothelioma: an analysis of pathologic findings and biologic behavior in 37 cases. Am. J. Surg. Pathol. 1988;12(10):737–746. [PubMed] [Google Scholar]
- 3.Birch D.W., Park A., Chen V. Laparoscopic resection of an intra-abdominal cystic mass: a cystic mesothelioma. Can. J. Surg. 1998;41(2):161–164. [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez-Moreno S., Yan H., Alcorn K.W., Sugarbaker P.H. Malignant transformation of benign cystic mesothelioma of the peritoneum. J. Surg. Oncol. 2002;79:243–251. doi: 10.1002/jso.10081. [DOI] [PubMed] [Google Scholar]
- 5.Rajiah P., Sinha R., Cuevas C., Dubinsky T.J., Bush W.H., Kolokythas O. Imaging of uncommon retroperitoneal masses. Radiographics. 2011;31:949–976. doi: 10.1148/rg.314095132. [DOI] [PubMed] [Google Scholar]
- 6.Kurtz R.J., Heimann T.M., Holt J., Beck A.R. Mesenteric and retroperitoneal cysts. Ann. Surg. 1986;203(1):109–112. doi: 10.1097/00000658-198601000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee S.E., Oh H.C., Park Y.G., Choi Y.S., Kim M.K. Laparoscopic excision of primary retroperitoneal mucinous cystadenoma and malignant predicting factors derived from literature review. Int. J. Surg. Case Rep. 2015;9:130–133. doi: 10.1016/j.ijscr.2015.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osman S., Lehnert B.E., Elojeimy S., Cruite I., Mannelli L., Bhargava P. A comprehensive review of the retroperitoneal anatomy: neoplasms, and pattern of disease spread. Curr. Probl. Diagn. Radiol. 2013;42(5):191–208. doi: 10.1067/j.cpradiol.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Scali E.P., Chandler T.M., Heffernan E.J., Coyle J., Harris A.C., Chang S.D. Primary retroperitoneal masses: what is the differential diagnosis. Abdom. Imaging. 2015;40:1887–1903. doi: 10.1007/s00261-014-0311-x. [DOI] [PubMed] [Google Scholar]
- 10.Yang D.M., Jung D.H., Kang J.H., Kim S.H., Kim J.H., Hwang H.Y. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24(5):1353–1365. doi: 10.1148/rg.245045017. [DOI] [PubMed] [Google Scholar]
- 11.Renzulli P., Candinas D. Symptomatic retroperitoneal cyst: a diagnostic challenge. Ann. R. Coll. Surg. Engl. 2009;91:1–3. doi: 10.1308/147870809X400877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marwah S., Kamal H., Marwah N. Laparoscopic management of a large primary retroperitoneal hydatid cyst. Clin. J. Gastroenterol. 2010;3(5):230–232. doi: 10.1007/s12328-010-0168-7. [DOI] [PubMed] [Google Scholar]
- 13.Uchinami M., Morioka K., Doi K., Nakamura T., Yoshida M., Tanaka K. Retroperitoneal laparoscopic management of a lymphocele after abdominal aortic surgery: a case report. J. Vasc. Surg. 2005;42:552–555. doi: 10.1016/j.jvs.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 14.Ishibashi Y., Tsujimoto H., Kouzu K., Horiguchi H., Nomura S., Ito N. Laparoscopic resection of a huge retroperitoneal cystic lymphangioma after successful reduction of tumor size with a double balloon catheter. Int. J. Surg. Case Rep. 2015;11:8–10. doi: 10.1016/j.ijscr.2015.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inaba K., Sakurai Y., Umeki Y., Kanaya S., Komori Y., Uyama I. Laparoscopic excision of subdiaphragmatic bronchogenic cyst ocurring in the retroperitoneum. Surg. Laparosc. Endosc. Percutan. Tech. 2010;20:e199–e203. doi: 10.1097/SLE.0b013e3181fcbe92. [DOI] [PubMed] [Google Scholar]
- 16.Lovell F., Cranston P.E. Well-differential papillary mesothelioma of the peritoneum. Am. J. Roentgenol. 1990;155:1245–1246. doi: 10.2214/ajr.155.6.2122674. [DOI] [PubMed] [Google Scholar]
- 17.Witek T.D., Marchese J.W., Farrell T.J. A recurrence of benign multicystic peritoneal mesothelioma treated through laparoscopic excision: a case report and review of the literature. Surg. Laparosc. Endosc. Percutan. Tech. 2014;24(2):70–73. doi: 10.1097/SLE.0b013e31828f7269. [DOI] [PubMed] [Google Scholar]
- 18.Ross M.J., Welch W.R., Scully R.E. Multilocular peritoneal inclusion cysts (so-called cystic mesotheliomas) Cancer. 1989;64:1336–1346. doi: 10.1002/1097-0142(19890915)64:6<1336::aid-cncr2820640628>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 19.Katsube Y., Mukai K., Silverberg S.G. Cystic mesothelioma of the peritoneum: a report of five cases and review of the literature. Cancer. 1982;50:1615–1622. doi: 10.1002/1097-0142(19821015)50:8<1615::aid-cncr2820500826>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 20.Özgen A., Akata D., Akhan O., Tez M., Gedikoglu G., Özmen M.N. Giant benign cystic peritoneal mesothelioma: US, CT and MRI findings. Abdom. Imaging. 1998;23:502–504. doi: 10.1007/s002619900387. [DOI] [PubMed] [Google Scholar]
- 21.Pitta X., Andreadis E., Ekonomou A., Papachristodoulou A., Tziouvaras C., Papapaulou L. Benign multicystic peritoneal mesothelioma: a case report. J. Med. Case Rep. 2010;4:385–389. doi: 10.1186/1752-1947-4-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ricci F., Borzellino G., Ghimenton C., Cordiano C. Benign cystic mesothelioma in a male: surgical treatment by the laparoscopic route. Surg. Laparosc. Endosc. 1995;5(2):157–160. [PubMed] [Google Scholar]
- 23.Vyas D., Pihl K., Kavuturu S., Vyas A. Mesothelioma as a rapidly developing giant abdominal cyst. World J. Surg. Oncol. 2012;10:277–280. doi: 10.1186/1477-7819-10-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sebbag G., Yan H., Shmookler B.M., Chang D., Sugarbaker P.H. Results of treatment of 33 patients with peritoneal mesothelioma. Br. J. Surg. 2000;87:1–7. doi: 10.1046/j.1365-2168.2000.01571.x. [DOI] [PubMed] [Google Scholar]