Abstract
BACKGROUND
SmokefreeVET is a text messaging smoking cessation program available to veterans enrolled in the Veterans Health Administration. SmokefreeVET was developed in collaboration with the National Cancer Institute as part of the SmokefreeTXT initiative.
PURPOSE
To evaluate the real world use of and effectiveness of the SmokefreeVET program for SmokefreeVET users who enrolled between 2013 and 2014.
METHODS
Demographics and smoking behavior of 1,470 SmokefreeVET users who enrolled between 2013 and 2014 were analyzed. Latent growth mixture modeling was used to identify discrete classes of SmokefreeVET users based on engagement patterns. Multi-level modeling determined class differences in abstinence.
RESULTS
The average age of the SmokefreeVET user was 48, 75% of users were male, and 84% were daily smokers. After five weeks, 13% of all users reported abstinence from smoking. Five statistically distinct engagement classes of SmokefreeVET users were identified. Highly engaged classes were significantly less likely to opt-out and more likely to report abstinence. Over 60% of users who were classified as high engagers throughout the program reported abstinence 5 weeks after their quit date. Users were more likely to report abstinence after two weeks if they used smoking cessation medication than those that did not use medication (OR=9.01, p<.001).
CONCLUSIONS
SmokefreeVET may be effective at supporting abstinence among a real world group of highly engaged users. Smoking cessation medication use was also associated with abstinence in SmokefreeVET users. Engagement appears to be a critical component when assessing the efficacy of a text messaging smoking cessation intervention.
Keywords: smoking, tobacco, cessation, mHealth, engagement, veteran
1. INTRODUCTION
The Veterans Health Administration (VHA) is the largest integrated health care system in the U.S. with over 9 million U.S. military veterans enrolled (U.S. Department of Veterans Affairs, 2015). Tobacco use is the leading cause of preventable death and disease in the United States (U.S. Department of Health and Human Services, 2014), and current smoking is more prevalent among veterans and service members than civilians (Brown, 2010; Shahoumian, Phillips, & Backus, 2016). Although VHA has made progress in reducing the rate of current smoking among its patients, in 2014 19.0% of VHA patients reported current every day smoking compared to 16.8% of the U.S. population (Jamal, et al., 2015; U.S. Department of Veterans Affairs, 2014a). Diseases caused by tobacco use are a significant burden, with an estimated $2.7 billion of VHA health care expenditures in 2010 attributable to smoking (Barnett, Hamlett-Berry, Sung, & Max, 2015). Because VHA serves a large and geographically diverse population—36% of all enrolled veterans are rural (U.S. Department of Veterans Affairs, 2014b)—timely access to health care is a priority for VHA. As such, VHA has invested in telehealth, mobile, and web resources to provide patients with remote access to care.
Mobile health (mHealth) interventions offer an opportunity to extend the reach of tobacco cessation interventions outside of traditional health care settings via a device that most adults already own, is generally always on, and is already used many times each day. Cell phone and text message use are commonplace in the U.S. with 91% of adults reporting cell phone ownership and 81% using their cell phone to send or receive text messages (Duggan, 2013). Likewise, a VHA patient sample surveyed found that 83% owned a cell phone (Houston, et al., 2013). Text messaging programs have demonstrated efficacy in improving tobacco abstinence rates. Randomized trials of the Text2Quit and Stop My Smoking USA programs in the U.S., the txt2stop program in the U.K., and a text messaging program in New Zealand each reported over a two-fold increase in abstinence rates in the intervention group compared to the control (Abroms, Boal, Simmens, Mendel, & Windsor, 2014; Free, et al., 2011; Rodgers, et al., 2005; Ybarra, Holtrop, Prescott, Rahbar, & Strong, 2013). Meta-analyses report slightly lower, although still significant, odds of abstinence with a text messaging program, overall indicating that text messaging programs are likely more effective than minimal or no intervention (Head, Noar, Iannarino, & Grant Harrington, 2013; Spohr, et al., 2015; Whittaker, et al., 2012). Despite the efficacy of text messaging programs in clinical trials, it is important to also evaluate the effectiveness of the programs in real world settings to inform the translation of research into clinical practice (Glasgow, Klesges, Dzewaltowski, Bull, & Estabrooks, 2004).
To increase veteran access to tobacco cessation treatment, VHA partnered with the National Cancer Institute (NCI) to establish SmokefreeVET, a text messaging program for veterans in care in VHA. SmokefreeVET was based on the NCI text messaging program, SmokefreeTXT, an automated intervention that provides text messages with encouragement, advice, and tips to help smokers quit and stay quit. Little is known about real world text messaging program users, particularly veteran users of such programs. We were interested in understanding how users engage with the SmokefreeVET program and in characterizing the real world users and monitoring program effectiveness. The findings are intended to provide information to improve text messaging programs for clinical use as well as to inform future VHA smoking cessation programs and clinical initiatives.
2. METHODS
2.1 SmokefreeVET program description and development
SmokefreeVET is a tobacco cessation program for veterans delivered entirely by text message. The intervention is based on a pre-programmed library of messages that are delivered daily and scheduled according to quit date. Users enroll online or by text message and provide demographic information, smoking frequency, and number of cigarettes smoked per day. Each user is required to set a quit date in order to receive text messages. Users can enroll at any point in their quit attempt and received messages accordingly. Between two and five messages are sent daily over the 8-week duration of the program, beginning 2 weeks prior to the user’s quit date and continuing for 6 weeks afterwards. Messages contain tips and encouragement to quit smoking and assessment questions to evaluate users’ cravings, mood, and abstinence. Daily messages end 42 days after the quit date, and three additional abstinence assessment questions are asked at 1, 3, and 6 months post-quit date. Thirty-one out of 143 total messages in the SmokefreeVET library are assessment questions, only two of which are asked in the 2 weeks of messages prior to the user’s quit date. SmokefreeVET was adapted from NCI’s SmokefreeTXT program by adding messages encouraging use of smoking cessation medications and referring users to other VHA resources, such as the VHA smoking quitline and their VHA health care provider. Follow-up assessment questions on the use of medications were also added to the SmokefreeVET library. VHA clinicians were consulted on content and word choice, and veteran patient input on program format and content was obtained through interviews.
In addition to the pre-programmed library, keywords (URGE, STRESS, SMOKED) provide on-demand tips for coping with a craving, stress, or a lapse. URGE and SMOKED messages were adapted from the SmokefreeTXT keywords CRAVE and SLIP, respectively. STRESS was adapted from SmokefreeTXT keyword MOOD by adding messages to address smoking triggers identified in Iraq- and Afghanistan-era veterans (Gierisch, et al., 2012). The keyword messages in general were modified to be veteran-specific in terms of word choice and to refer users to other VHA resources. CRISIS was an additional keyword added to SmokefreeVET to direct users to the Veterans Crisis Line (Christofferson, Hamlett-Berry, & Augustson, 2015). There are 13 messages throughout the library that contain prompts to use one or more of the keywords associated with the program.
2.2 Sample and procedure
The initial sample included 2,188 SmokefreeVET users who enrolled in the program between 12:00am May 30, 2013 and 12:00am May 1, 2014. SmokefreeVET was widely disseminated through the VA health care system beginning in May 2013, and users may have been referred to the program by their health care provider or learned about it through VA websites or social media platforms. Users were excluded if they did not receive the intervention, specifically if they enrolled with a device that could not receive text messages (n = 55), never sent a text to the program (n = 166), did not set a quit date (n = 281), set a quit date more than two weeks after May 1, 2014 (n = 1), opted out of the program before reaching their quit date (n = 204), or were located outside of VHA’s network area (n = 11). The final sample contained 1,470 users.
All data was obtained from the SmokefreeVET administrative database of non-identifiable data and was provided by users upon enrollment or during the course of the program. Users who lapsed could restart the program and set a new quit date (n = 392). All analyses were conducted on users’ most recent quit attempt as of May 1, 2014. To account for varying lengths of enrollments due to restarts, the number of days from initial enrollment until most recent quit date was co-varied throughout. Personally identifiable information was not included in the dataset. Because this analysis was designed for internal VA purposes to evaluate and improve the quality of the program, IRB approval was not required as outlined in the VHA Handbook 1058.05.
2.3 Statistical analysis
User engagement was measured by tallying the total number of text messages (prompted, unprompted, and keywords) sent each week by each user to the SmokefreeVET program during the 6 weeks following their quit date. Only the period following the quit date was analyzed in order to create a standard period of time for comparison of all users. In addition, 29% (n = 431) of users began the program on or after their quit date and did not receive any of the pre-quit messages. Users were asked an assessment question and prompted for a response by the program 9 times the first week following the quit date (week 1), 4 times each in weeks 2 and 5, and 3 times each in weeks 3, 4, and 6 in addition to receiving multiple reminders each week to use the keywords. Latent growth mixture modeling (LGMM) was employed to identify discrete classes of users based on engagement (Muthén, 2004).
Prior to LGMM, the distribution of users’ weekly text counts was determined for modeling purposes. Because the weekly counts were highly skewed (M = 0.86, SD = 1.79, maximum = 27) with a high prevalence of zeroes (65%), zero-inflated negative binomial and negative binomial modeling distributions were compared via a Vuong test performed on null models (i.e., models absent predictors) (Vuong, 1989). According to this, the zero-inflated negative-binomial model did not provide a better fit than the more parsimonious negative-binomial model, z = 0.89, p = .37. Hence, the latter was used.
LGMM was then conducted on each user’s weekly count of texts sent. Because users were enrolled in the intervention for varying times prior to their quit date, thereby posing a potentially systematic influence on texting behavior, the number of days enrolled prior to quit was co-varied. Within-class count intercepts were allowed to vary, but slopes (linear and quadratic) were fixed. Two-through eight-class solutions were modeled in Mplus (Version 7, Muthén & Muthén, Los Angeles, CA). Because mixture models are susceptible to converging on local, rather than global, log-likelihood maxima (McLachlan & Peel, 2000), 500 random sets of initial values for estimated model parameters were generated for each model to test solution replicability. Determination of the best-fitting solution was made based on BIC and the Lo-Mendell-Rubin (LMR) likelihood ratio test (Collins, Fidler, Wugalter, & Long, 1993; Hagenaars & McCutcheon, 2002; Lo, 2001; Magidson & Vermunt, 2004; Nylund, Asparouhov, & Muthén, 2007). The LMR test returns a p-value, which indicates whether a statistically significant improvement in fit is observed by increasing the number of classes from k – 1 to k.
Once a best-fitting LGMM solution was generated, baseline differences in demographics and smoking behavior were analyzed via ANOVA and contingency-table analyses. Group differences in self-reported smoking status (abstinent vs. smoking) at each week of the observation period were assessed using multilevel modeling (MLM). Users who opted out of the program were considered non-abstinent subsequent to the point of opt-out. Otherwise, missing data were treated as missing at random. Time until program opt-out was also modeled as a function of class membership via a Cox regression. In each model, the number of days of enrollment prior to quit was covaried. Analyses of group differences were conducted using SAS (Version 9.2, SAS Institute Inc., Cary, NC).
2.4 Smoking cessation medication analysis
The SmokefreeVET program asks each user 4 days after their quit date if they are using medication in their quit attempt: “SmokefreeVET: Are you using meds to help you quit? Text back: MEDS or NO MEDS”. In order to evaluate the effect of medication use on abstinence reported on weeks one through five post-quit date, logistic MLM was used.
3. RESULTS
3.1 User demographics and smoking behavior
The mean age of the sample analyzed was 48.33 years (SD = 13.19; range: 19 to 89). Male users comprised 75% of the sample. Eighty-four percent of the sample reported smoking every day, and 27% of users reported smoking more than one pack of cigarettes per day (Table 1). One thousand fifty-six users indicated whether or not their phones were web-enabled. Of these, 88% (n = 925) reported having web access, however only 20% (n = 295) of all users analyzed ever accessed a webpage from the SmokefreeVET program. Overall, users received an average of 72.53 (SD = 43.73) text messages from the SmokefreeVET program post-quit date.
Table 1.
Demographic and Smoking Characteristics of SmokefreeVET Users
| All (N = 1,470) | HE (n = 419) | IE (n = 53) | RD (n = 225) | DD (n = 247) | LE (n = 526) | |
|---|---|---|---|---|---|---|
| Ageh | ||||||
| 18–30 | 177 (12.04%) | 51 (12.17%) | 2 (3.77%) | 40 (17.78%) | 21 (8.50%) | 63 (11.98%) |
| 31–44 | 376 (25.58%) | 92 (21.96%) | 11 (20.75%) | 55 (24.44%) | 67 (27.13%) | 151 (28.71%) |
| 45–64 | 736 (50.07%) | 233 (55.61%) | 30 (56.60%) | 111 (49.33%) | 114 (46.15%) | 248 (47.15%) |
| 65+ | 159 (10.82%) | 41 (9.79%) | 9 (16.98%) | 16 (7.11%) | 42 (17.00%) | 51 (9.70%) |
| Males | 1081 (75%) | 320 (77%) | 42 (81%) | 167 (75%) | 174 (72%) | 378 (73%) |
| Daily cigarette consumption | ||||||
| 10 or less | 440 (36%) | 142 (40%) | 19 (40%) | 64 (35%) | 75 (37%) | 140 (31%) |
| 11–20 | 461 (38%) | 121 (34%) | 12 (26%) | 79 (43%) | 81 (40%) | 168 (38%) |
| 21–30 | 232 (19%) | 64 (18%) | 12 (26%) | 23 (13%) | 35 (17%) | 98 (22%) |
| 31 or more | 94 (8%) | 24 (7%) | 4 (9%) | 16 (9%) | 11 (5%) | 39 (9%) |
| Smoking frequencya,e,f,g, | ||||||
| Every day | 1112 (84%) | 310 (82%) | 29 (57%) | 177 (88%) | 177 (83%) | 419 (87%) |
| Most days | 120 (9%) | 45 (12%) | 5 (10%) | 15 (7%) | 22 (10%) | 33 (7%) |
| Some days | 39 (3%) | 10 (3%) | 2 (4%) | 6 (3%) | 7 (3%) | 14 (3%) |
| Less than that | 51 (4%) | 13 (3%) | 15 (29%) | 3 (1%) | 7 (3%) | 13 (3%) |
| Texts received prior to quita,b,e,f,g | 41.16 (65.77) | 46.51 (63.49) | 0.09 (0.69) | 30.92 (47.72) | 40.77 (62.80) | 45.59 (76.26) |
| Days enrolled prior to quita,g,i,j | 21.97 (45.08) | 22.50 (37.90) | 0.02 (0.14) | 12.86 (21.12) | 17.46 (31.89) | 29.79 (61.00) |
| Texts received after quita,b,c,d,f,h,j | 72.53 (43.73) | 114.28 (19.02) | 37.21 (20.13) | 49.41 (33.87) | 75.76 (23.93) | 51.21 (45.38) |
| Days enrolled after quitb,c,d,e,f,g,i | 70.33 (77.97) | 114.35 (71.30) | 141.70 (70.73) | 35.64 (63.27) | 44.39 (61.20) | 55.12 (76.68) |
| Medication Use (n = 469) | 227 (48%) | 113 (48%) | - | 29 (45%) | 72 (55%) | 13 (33%) |
Note. Means/frequencies and standard deviations/percentiles (in parentheses). HE=High Engagement; IE=Increasing Engagement; RD=Rapidly Decreasing Engagement; DD=Delayed Decreasing Engagement; LE=Low Engagement.
Significant difference between HE and IE, p < .005
Significant difference between HE and RD, p < .005
Significant difference between HE and DD, p < .005
Significant difference between HE and LE, p < .005
Significant difference between IE and RD, p < .005
Significant difference between IE and DD, p < .005
Significant difference between IE and LE, p < .005
Significant difference between RD and DD, p < .005
Significant difference between RD and LE, p < .005
Significant difference between DD and LE, p < .005
3.2 Engagement analysis
To analyze differences in user engagement with SmokefreeVET, LGMM was used as described (see Methods). Examination of the BICs across the seven models revealed that the 5-class solution yielded a BIC of 18,459.319, more than 80 points lower than the 2-(BIC = 18,780.056), 3-(BIC = 18,647.667), and 4-class (BIC = 18,542.613) solutions. Moreover, the LMR test for the 5-class solution indicated that it provided a significantly better fit than the 4-class solution, p < .001. The 6-, 7-, and 8-class models were non-identified, indicating poor model specification (Nylund, et al., 2007).
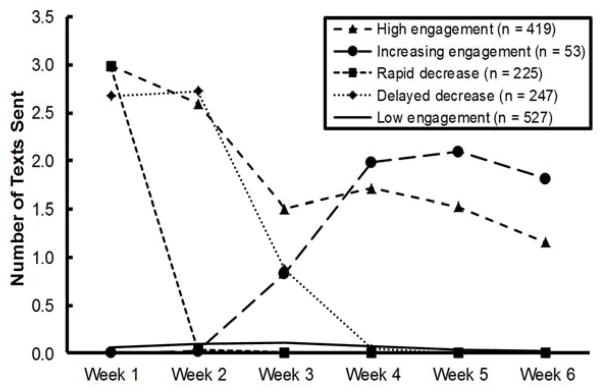
The 5-class solution produced trajectories corresponding to high engagement (HE, n = 419), increasing engagement (IE, n = 53), rapidly decreasing engagement (RD, n = 225), delayed decreasing engagement (DD, n = 247), and low engagement (LE, n = 526) (Figure 1). Although the magnitude of differences in weekly text counts between classes appeared to be slight, the five trajectories were statistically distinct according to a multilevel negative binomial model, F(20, 7,325) = 23.78, p < .001.
Figure 1. Texting activity by engagement class.
All text messages (prompted, unprompted, and keyword messages) sent by users in each engagement class were averaged and plotted according to week of the program. The quit date was set at the start of week 1. Week 6 marked the end of daily text messages from the program.
The demographics of each engagement class did not differ significantly by gender or by number of cigarettes smoked per day (Table 1). The average age of all users was 48 and did not significantly differ by engagement class. Further breakdown of the age distributions of each class reveals differences between each class with the IE having the lowest proportion of 18–30 year olds and the highest proportion of users over the age of 45 (73.6%), but only the RD and DD classes were significantly different from one another at the p < .005 level. Daily smoking frequency reported by the IE class (57%) was significantly lower than that of the other engagement classes (82–88%). The HE and IE classes were enrolled for a significantly higher number of days post-quit date than the classes with lower engagement levels (LE, RD, and DD). The number of texts received from SmokefreeVET post-quit date varied significantly by engagement class, but there was no clear association with engagement class or opt-out rates.
Six hundred ninety-nine users (48%) opted out of the text program prior to its conclusion 6 months after the quit date. Among this sample, mean post-quit date enrollment was 18.85 (SD = 27.01) days. The number of days users remained in the text program prior to opt-out was modeled via Cox regression as a function of class, with days enrolled prior to quit controlled. Users who did not opt-out were censored. According to the model, number of days enrolled prior to quit was associated with decreased risk of opting out, Hazard Ratio (HR) = 0.99, p < .001. HE (HR = 0.25, p < .001) and IE users (HR = 0.17, p < .001) were at less risk of opting out than LE users. RD users were at greater risk of opting out than LE users, HR = 1.55, p < .001. There was no difference in risk of opting out between DD and LE users, HR = 1.11, p = .31.
3.3 Abstinence rates
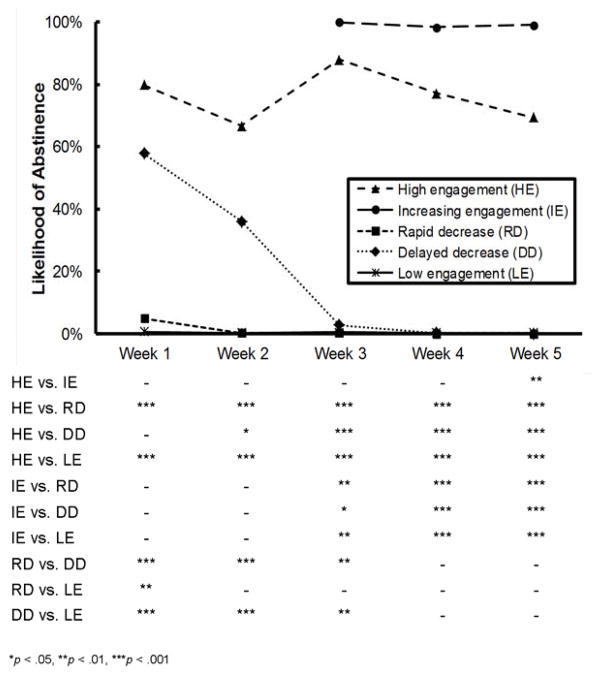
After 5 weeks, 193 of the SmokefreeVET users (13%) reported abstinence from smoking. Self-reported point prevalence abstinence status recorded at the end of weeks 1 through 5 was submitted to logistic MLM. The main effect for days enrolled prior to quit date failed to be significant at the p < .05 level, but there was a trend toward significance, F(1, 2,734) = 3.48, p = .06, reflecting a trend for greater abstinence rates among participants enrolled in the program longer prior to quit. The main effects for engagement class, F(4, 2,734) = 59.24, p < .001, and week, F(4, 2,734) = 26.45, p < .001, were significant. These were qualified by a significant interaction, F(14, 2,734) = 9.08, p < .001. According to the interaction, contrasts between the classes were evident at each week, Fs ≥ 37.33, ps < .001, mirroring texting activity (Figure 2). The more engaged classes (HE, IE) were significantly more likely to be abstinent at weeks 3, 4, and 5 compared to those classes with lower levels of engagement (RD, DD, LE).
Figure 2. Modeled likelihood of abstinence by engagement class.
Tukey-adjusted contrasts are presented for each week. No week 1 and week 2 abstinence data was available for the IE group. *p < .05, **p < .01, ***p < .001
3.4 Smoking cessation medication utilization
Of the sample analyzed, a subset of users (n = 469) responded to the assessment question about smoking cessation medication use four days subsequent to their quit date. Of those users, 227 (48%) reported using medication (Table 1). Medication use did not vary by engagement class, χ2(3) = 6.35, p = .10. Multilevel modeling was used to analyze self-reported abstinence at the end of weeks 1 through 5 post-quit date as a function of medication use at day 4, week, and their interaction. As in previous analyses, length of enrollment prior to quit was covaried. According to the model, the significant time effects indicate that abstinence rates fell after the first week post-quit date (Table 2). A main effect of medication use reflected greater odds of abstinence amongst participants reporting medication use at the end of week 1. Moreover, a significant interaction effect at Week 2 indicates that medication use was associated with increased odds of abstinence (OR = 9.01, p < .001) at that time point in comparison to no use of medication. Differences in abstinence rates by medication use were not significant in subsequent weeks.
Table 2.
Multilevel Logistic Model of Abstinence
| Parameter | Coeff. (SE) | OR (95% CI) |
|---|---|---|
| Within-person | ||
| Intercept | 0.53 (0.37) | 1.71 (0.82 – 3.55) |
| Med use | 1.08* (0.51) | 2.96 (1.08 – 8.09) |
| Week 2 | −1.84** (0.41) | 0.16 (0.07 – 0.36) |
| Week 3 | −0.69† (0.39) | 0.50 (0.23 – 1.07) |
| Week 4 | −2.08** (0.41) | 0.12 (0.06 – 0.28) |
| Week 5 | −2.27** (0.41) | 0.10 (0.05 – 0.23) |
| Between-person | ||
| Days enrolled prior to quit | −0.00 (0.00) | 1.00 (0.99 – 1.01) |
| Med use X Week 2 | 1.11* (0.56) | 3.05 (1.01 – 9.14) |
| Med use X Week 3 | −0.44 (0.54) | 0.64 (0.22 – 1.86) |
| Med use X Week 4 | −0.36 (0.57) | 0.70 (0.23 – 2.13) |
| Med use X Week 5 | −0.50 (0.57) | 0.61 (0.20 – 1.84) |
Note. Week 1 was used as a reference group, hence its omission from the Table.
p < .10,
p < .05,
p < .01
4. DISCUSSION
This analysis examines real world use of the SmokefreeVET text messaging smoking cessation program. Even though 18–24 year olds are the most prolific users of text messaging (Smith, 2011), the technology did not limit use of SmokefreeVET by older Veterans: the average age of all users was just under 50 years, and the oldest user was 89 years old. Women make up only 7.2% of VHA’s enrollee population yet comprised nearly a quarter of all SmokefreeVET users (U.S. Department of Veterans Affairs, 2014a). This finding is consistent with other studies that have reported women are more likely to use cessation services than men, including calling a quitline and using combination counseling and medication (Kruger, O’Halloran, Rosenthal, Babb, & Fiore, 2016; Shiffman, Brockwell, Pillitteri, & Gitchell, 2008a; S. Zhu, Melcer, Sun, Rosbrook, & Pierce, 2000; S. H. Zhu, Anderson, Johnson, Tedeschi, & Roeseler, 2000).
Among all SmokefreeVET users, 13% report abstinence after 5 weeks. However, users with consistently high engagement levels (HE) and increasing engagement levels over time (IE) were significantly more likely to quit smoking after 5 weeks than users with lower engagement levels. These encouraging findings indicate the SmokefreeVET text messaging program successfully supports abstinence among a real world group of highly engaged users. This result also demonstrates the importance of evaluating user engagement with a text messaging program and suggests that a user’s level of engagement may serve as a measure of intervention intensity. The literature has consistently shown that increased amounts of time spent receiving behavioral counseling or a higher number of counseling sessions promote abstinence from tobacco (Tobacco Use and Dependence Guideline Panel, 2008 ). In web-based interventions, higher numbers of visits and page views are associated with abstinence (Richardson, et al., 2013; Strecher, et al., 2008). A text message-based intervention is inherently different from other delivery mechanisms in that most tobacco cessation interventions require repeated action by the patient, whether visiting a clinic for in-person counseling, answering a telephone call from a quitline counselor, or visiting a website to view the self-help content. After initial enrollment in a text program like SmokefreeVET however, no action is needed from the participant to receive the intervention, action is only required to opt-out. As noted in the Methods, 65% of the weekly counts of texts sent by users to the SmokefreeVET program had values of zero although there were questions and prompts to engage with the SmokefreeVET program throughout. Characteristics of engagement with a text message program have not been extensively studied, but we speculate that this high prevalence of zeroes may have been due to the older age of this sample as studies suggest that adults between the ages of 18 and 24 send more text messages per day than any other adult age group (Smith, 2011). Of the participants in the Text2Quit program, 75% reported reading all or most of the texts they received (Abroms, et al., 2012). Thus, the majority of participants received the intervention regardless of direct engagement. However, those that actively engaged with a text program were more likely to quit, indicating that engagement may be a key factor when assessing the ‘dose’ or ‘intensity’ of a text message intervention. In support of this hypothesis, our analysis did not find an association between the numbers of texts received post-quit date with engagement class: the IE class received significantly fewer texts post-quit date but had a significantly higher abstinence rate than any other engagement class after five weeks. It remains a topic for further study to determine whether engagement can be influenced to increase abstinence rates. It will also be interesting to examine how user engagement with various text messaging programs may differ depending on the population.
SmokefreeVET text messages encouraged the use of medication since use of smoking cessation medications is A-level evidence from the U.S. Public Health Service Clinical Practice Guidelines and proven to increase abstinence both when used alone and when combined with counseling (Tobacco Use and Dependence Guideline Panel, 2008 ). Outcomes of medication use together with a text messaging program have not been studied. SmokefreeVET users who reported using medication four days after their quit date were more likely to abstain from smoking in the first two weeks post-quit date than those users that did not report using medication, however this effect did not persist to later time points. These short-term findings are promising and further study is needed to evaluate the efficacy of medication together with a smoking cessation text messaging program.
4.1 Limitations
Data from users was self-reported and collected in an administrative database with personally identifiable information removed so that biochemical confirmation of abstinence was not possible. This analysis contains point prevalence abstinence outcomes only through five weeks. Since smoking is a chronic, relapsing condition, longer term abstinence rates and outcomes are necessary to evaluate this intervention. Follow-up analyses based on self-reported abstinence at three and six months post-quit date on SmokefreeVET users are planned to address this concern.
Users who opted out of the program prior to its completion were considered to have returned to smoking subsequent to the point of opt-out for a conservative estimation of abstinence rate. There is no user data collected on the reason for opting out of the SmokefreeVET program, therefore the accuracy of this assumption is unknown. As mHealth interventions are relatively new to the health care landscape, little is known about user motivations for beginning or ending use of a text messaging intervention. The literature on reasons for attrition is mixed and fairly inconclusive, but studies suggest that the number of cigarettes smoked per day, psychological symptoms, confidence in quitting, and length of previous quit attempts in addition to age and gender may influence attrition (Borrelli, et al., 2002; Bowen, McTiernan, Powers, & Feng, 2000; Curtin, Brown, & Sales, 2000; Leeman, et al., 2005; Nevid, Javier, & Moulton, 1996).
This study identified classes of users based on their engagement pattern with the text program. The characteristics of the IE class stood out from the other engagement classes, with a significantly lower proportion reporting daily smoking and fewer text messages received post-quit date. However, distinctions between classes were limited by the demographic and smoking information collected and there were few significant differences between the classes in terms of demographics. There may be additional factors not collected in this study that influenced user engagement and abstinence, such as education level, income, readiness to quit, or history of previous quit attempts. As VHA patients, SmokefreeVET users were also eligible to receive a range of additional tobacco cessation services from VHA and texts encouraged users to utilize these additional modes of care. Data was not collected on additional tobacco cessation care received besides the use of smoking cessation medications. It is possible that additional interventions received by the user may have influenced abstinence, however most smokers who attempt to quit do so with any behavioral or pharmacotherapy support: 64.2% of smokers in the U.S. who attempted to quit did not use any cessation treatment and only 14.1% utilized two or more cessation treatments (Shiffman, Brockwell, Pillitteri, & Gitchell, 2008b). Heavier smokers are more likely to use treatment, but only 26% of the SmokefreeVET sample analyzed reported smoking more than one pack per day. In addition, men are less likely to use assistance in quitting, and 75% of the SmokefreeVET sample was male (Kruger, et al., 2016; Shiffman, et al., 2008a, 2008b).
Text messages have a 160 character limit, and delivery of a smoking cessation intervention through this modality requires some creativity in order to comply with this requirement. As an example, smoking cessation medications are typically referred to as “meds” throughout the SmokefreeVET program. This terminology was chosen after consulting with VA pharmacists however it may still be unclear to the SmokefreeVET user and could have contributed to the low response rate (32%) to the question about medication usage.
4.2 Conclusion
Analysis of the SmokefreeVET program provides important information on the demographics of real world users, suggesting that use of the program is not limited to younger age groups that are more active users of text messaging and that women veterans may be more likely to use the program than men. Combination of smoking cessation medication with the text messaging program promoted abstinence in the first few weeks compared to those who did not use medication and this promising finding should be further studied. The main finding of this analysis was that users varied in their level of engagement with the program and highly engaged users were significantly more likely to report short-term abstinence from smoking. This important insight may apply to other populations and text messaging programs and should be the subject of longer-term evaluation.
References
- Abroms LC, Ahuja M, Kodl Y, Thaweethai L, Sims J, Winickoff JP, Windsor RA. Text2Quit: results from a pilot test of a personalized, interactive mobile health smoking cessation program. J Health Commun. 2012;17(Suppl 1):44–53. doi: 10.1080/10810730.2011.649159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abroms LC, Boal AL, Simmens SJ, Mendel JA, Windsor RA. A randomized trial of Text2Quit: a text messaging program for smoking cessation. Am J Prev Med. 2014;47:242–250. doi: 10.1016/j.amepre.2014.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett PG, Hamlett-Berry K, Sung HY, Max W. Health care expenditures attributable to smoking in military veterans. Nicotine Tob Res. 2015;17:586–591. doi: 10.1093/ntr/ntu187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B, Hogan JW, Bock B, Pinto B, Roberts M, Marcus B. Predictors of quitting and dropout among women in a clinic-based smoking cessation program. Psychol Addict Behav. 2002;16:22–27. doi: 10.1037//0893-164x.16.1.22. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, McTiernan A, Powers D, Feng Z. Recruiting women into a smoking cessation program: who might quit? Women Health. 2000;31:41–58. doi: 10.1300/j013v31n04_03. [DOI] [PubMed] [Google Scholar]
- Brown DW. Smoking prevalence among US veterans. J Gen Intern Med. 2010;25:147–149. doi: 10.1007/s11606-009-1160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christofferson DE, Hamlett-Berry K, Augustson E. Suicide Prevention Referrals in a Mobile Health Smoking Cessation Intervention. Am J Public Health. 2015;105:e7–9. doi: 10.2105/AJPH.2015.302690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Fidler PL, Wugalter SE, Long JD. Goodness-of-Fit Testing for Latent Class Models. Multivariate Behavioral Research. 1993;28:375–389. doi: 10.1207/s15327906mbr2803_4. [DOI] [PubMed] [Google Scholar]
- Curtin L, Brown RA, Sales SD. Determinants of attrition from cessation treatment in smokers with a history of major depressive disorder. Psychol Addict Behav. 2000;14:134–142. doi: 10.1037//0893-164x.14.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M. Pew Internet & American Life Project. 2013. Cell Phone Activities 2013. [Google Scholar]
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, Rodgers A, Cairns J, Kenward MG, Roberts I. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet. 2011;378:49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gierisch JM, Straits-Troster K, Calhoun PS, Beckham JC, Acheson S, Hamlett-Berry K. Tobacco use among Iraq- and Afghanistan-era veterans: a qualitative study of barriers, facilitators, and treatment preferences. Prev Chronic Dis. 2012;9:E58. doi: 10.5888/pcd9.110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27:3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- Hagenaars JA, McCutcheon AL. Applied Latent Class Analysis. Cambridge University Press (CUP); 2002. [Google Scholar]
- Head KJ, Noar SM, Iannarino NT, Grant Harrington N. Efficacy of text messaging-based interventions for health promotion: a meta-analysis. Soc Sci Med. 2013;97:41–48. doi: 10.1016/j.socscimed.2013.08.003. [DOI] [PubMed] [Google Scholar]
- Houston TK, Volkman JE, Feng H, Nazi KM, Shimada SL, Fox S. Veteran internet use and engagement with health information online. Mil Med. 2013;178:394–400. doi: 10.7205/MILMED-D-12-00377. [DOI] [PubMed] [Google Scholar]
- Jamal A, Homa DM, O’Connor E, Babb SD, Caraballo RS, Singh T, Hu SS, King BA. Current Cigarette Smoking Among Adults - United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2015;64:1233–1240. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- Kruger J, O’Halloran A, Rosenthal AC, Babb SD, Fiore MC. Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC Public Health. 2016;16:141. doi: 10.1186/s12889-016-2798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman RF, Quiles ZN, Molinelli LA, Terwal DM, Nordstrom BL, Garvey AJ, Kinnunen T. Attrition in a multi-component smoking cessation study for females. Tob Induc Dis. 2005;3:59–71. doi: 10.1186/1617-9625-3-2-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Magidson J, Vermunt JK. The SAGE Handbook of Quantitative Methodology for the Social Sciences. SAGE Publications; 2004. Latent Class Models; pp. 176–199. [Google Scholar]
- McLachlan G, Peel D. Wiley Series in Probability and Statistics. John Wiley & Sons, Inc; 2000. Finite Mixture Models. [Google Scholar]
- Muthén B. The SAGE Handbook of Quantitative Methodology for the Social Sciences. SAGE Publications; 2004. Latent Variable Analysis: Growth Mixture Modeling and Related Techniques for Longitudinal Data; pp. 346–369. [Google Scholar]
- Nevid JS, Javier RA, Moulton JL., 3rd Factors predicting participant attrition in a community-based, culturally specific smoking-cessation program for Hispanic smokers. Health Psychol. 1996;15:226–229. doi: 10.1037//0278-6133.15.3.226. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. [Google Scholar]
- Richardson A, Graham AL, Cobb N, Xiao H, Mushro A, Abrams D, Vallone D. Engagement promotes abstinence in a web-based cessation intervention: cohort study. J Med Internet Res. 2013;15:e14. doi: 10.2196/jmir.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, Jones M. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14:255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahoumian TA, Phillips BR, Backus LI. Cigarette Smoking, Reduction and Quit Attempts: Prevalence Among Veterans With Coronary Heart Disease. Prev Chronic Dis. 2016;13:E41. doi: 10.5888/pcd13.150282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Individual differences in adoption of treatment for smoking cessation: demographic and smoking history characteristics. Drug Alcohol Depend. 2008a;93:121–131. doi: 10.1016/j.drugalcdep.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Use of smoking-cessation treatments in the United States. Am J Prev Med. 2008b;34:102–111. doi: 10.1016/j.amepre.2007.09.033. [DOI] [PubMed] [Google Scholar]
- Smith A. Pew Internet & American Life Project. Washington, D.C: 2011. Americans and text messaging. [Google Scholar]
- Spohr SA, Nandy R, Gandhiraj D, Vemulapalli A, Anne S, Walters ST. Efficacy of SMS text message interventions for smoking cessation: A meta-analysis. J Subst Abuse Treat. 2015 doi: 10.1016/j.jsat.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, McClure J, Alexander G, Chakraborty B, Nair V, Konkel J, Greene S, Couper M, Carlier C, Wiese C, Little R, Pomerleau C, Pomerleau O. The role of engagement in a tailored web-based smoking cessation program: randomized controlled trial. J Med Internet Res. 2008;10:e36. doi: 10.2196/jmir.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: US Department of Health and Human Services; 2008. [Google Scholar]
- U.S. Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: 2014. [Google Scholar]
- U.S. Department of Veterans Affairs. Report of the 2014 Survey of Veteran Enrollees’ Health and Reliance Upon VA. Burlington, VT: 2014a. [Google Scholar]
- U.S. Department of Veterans Affairs. VHA Office of Rural Health Fact Sheet. 2014b;2016 http://www.ruralhealth.va.gov/docs/factsheets/ORH_General_FactSheet_2014.pdf. [Google Scholar]
- U.S. Department of Veterans Affairs. VA Benefits & Health Care Utilization. 2015;2015 [Google Scholar]
- Vuong QH. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica: Journal of the Econometric Society. 1989;57:307–333. [Google Scholar]
- Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD006611. doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- Ybarra ML, Holtrop JS, Prescott TL, Rahbar MH, Strong D. Pilot RCT results of stop my smoking USA: a text messaging-based smoking cessation program for young adults. Nicotine Tob Res. 2013;15:1388–1399. doi: 10.1093/ntr/nts339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000;18:305–311. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]
- Zhu SH, Anderson CM, Johnson CE, Tedeschi G, Roeseler A. A centralised telephone service for tobacco cessation: the California experience. Tob Control. 2000;9(Suppl 2):II48–55. doi: 10.1136/tc.9.suppl_2.ii48. [DOI] [PMC free article] [PubMed] [Google Scholar]