Abstract
Men who have sex with men (MSM) are the demographic group most severely affected by HIV in the USA. Global association studies have shown that MSM who binge drink are more likely to engage in risky sexual behaviors and day- and event-level analyses have linked binge drinking to sexual risk behavior on specific days and during specific sexual encounters. Despite this strong foundation of research, no studies have examined the association between the frequency of situational binge drinking (i.e. binge drinking concurrent with sexual activity) and aggregated sexual risk over periods of longer duration. We used multivariable logistic regression to assess the relationship between situational binge drinking (i.e. binge drinking concurrent with anal intercourse) and condomless anal intercourse and among a cross-sectional sample of 124 MSM in San Francisco, CA. There was a positive relationship between frequency of situational binge drinking and CAI (1 to 5 times vs. never: adjusted odds ratio = 2.78, 95% CI = 1.01-7.63; 6 to 10 times vs. never: 6.19, 1.27-30.22; more than 10 times vs. never: 11.88, 1.31-107.60). By filling a methodological gap and complementing existing global and event-level analyses, this positive situational relationship strengthens the evidence linking binge drinking and sexual risk, enhances the comparability of the existing literature, and further suggests that the integration of dual strategies that aim to prevent HIV and reduce binge drinking may be warranted.
Keywords: Binge drinking, men who have sex with men, HIV, sexual risk, substance use
INTRODUCTION
Men who have sex with men (MSM) are the demographic group most severely affected by HIV in the USA and HIV diagnoses attributable to male-to-male sexual contact increased between 2010 and 2014 (Centers for Disease Control and Prevention, 2015). Interventions that target modifiable risk factors associated with the transmission of HIV are a critical component of HIV prevention efforts among MSM (Lorimer et al., 2013).
Research has linked drinking alcohol to sexual HIV risk behaviors among MSM, including condomless anal intercourse (CAI), multiple concurrent partners, and having HIV serodiscordant partners (Colfax et al., 2004; Folch, Esteve, Zaragoza, Munoz, & Casabona, 2010; Irwin, Morgenstern, Parsons, Wainberg, & Labouvie, 2006). However, reconciling the results of different studies assessing alcohol use and sexual risk has been challenged by a high degree of variability in how alcohol use is measured. Binge drinking, defined as consuming five or more alcoholic drinks on a single occasion, has received heightened attention as part of the intersection of alcohol consumption and sexual risk among MSM. Binge drinking is three times more prevalent among MSM compared to the general U.S. population (Centers for Disease Control and Prevention, 2012, 2014), conforms to a standard definition (National Institute on Alcohol Abuse and Alcoholism, 2004), and generates a major public health impact beyond its implications for the HIV epidemic (Naimi et al., 2003; National Institute on Alcohol Abuse and Alcoholism, 2000).
Research has shown that MSM who binge drink are more likely to engage in risky sexual behaviors (i.e. global association studies) (Ekstrand, Stall, Paul, Osmond, & Coates, 1999; Greenwood et al., 2001; Hess et al., 2015). Also, day- and event-level analyses have shown that binge drinking is associated with sexual risk behavior on specific days and during specific sexual encounters among MSM (Kahler et al., 2015; Vosburgh, Mansergh, Sullivan, & Purcell, 2012). Despite this strong foundation of research, no studies have examined the association between the frequency of situational binge drinking (i.e. binge drinking concurrent with sexual activity) and aggregated sexual risk over periods of longer duration. Although event-level analyses are generally considered to provide stronger temporal evidence linking substance use and sexual risk than situational association studies, they require more burdensome assessments and are vulnerable to a loss of precision that naturally accompanies the higher level of detail involved (Leigh & Stall, 1993; Pinkerton et al., 2010). By assessing the relationship between situational binge drinking frequency and aggregate sexual risk behaviors, we aim to complement the existing global and event-level evidence and enhance comparability to future studies that may not have the design or resources to conduct event-level analyses.
MATERIALS AND METHODS
STUDY SAMPLE
We conducted a convenience-based cross-sectional survey of MSM aged 18+ in the San Francisco Bay Area from May 2013 to July 2014 as part of the screening phase of a randomized-controlled trial assessing the feasibility, acceptability, and tolerability of targeted naltrexone for non-dependent methamphetamine-using and binge-drinking MSM (Santos, Coffin, et al., 2015). Participants were recruited through active outreach at STI and HIV clinics, syringe access programs, community organizations, MSM bars and events, and on the street in areas frequented by MSM. Passive outreach included recruitment flyers and online advertisements on websites and social media. All participants provided informed consent and study procedures were approved by the Committee on Human Research, University of California San Francisco.
DATA COLLECTION
Trained staff administered structured telephone questionnaires to MSM willing to be screened for the parent trial. Demographics, overall binge alcohol and methamphetamine use, situational binge alcohol use (i.e., concurrent with sex ), as well as condom usage during anal intercourse encounters (AI) that involved methamphetamine or binge drinking were collected. All substance use and sexual behaviors were assessed in the last three months. Overall binge drinking frequency was assessed with the response categories presented in Table 1. Situational binge drinking was assessed with the question, “How many times have you had five or more drinks containing alcohol before or during anal sex with men?” and possible responses: none, 1-5 times, 6-10 times, and 10+ times. Condom usage during situational binge alcohol episodes was then assessed with the question, “Of those times, how many times were without a condom?” and the same four possible responses. Global methamphetamine use was assessed with the response categories presented in Table 1. Condom usage during AI encounters that involved methamphetamine was assessed in the same way as for those that involved binge drinking. Current use of pre-exposure prophylaxis (PrEP) was also collected.
Table 1.
Demographic and behavioral characteristics of study sample (n=124)
| N mean | (%) (SD) | |
|---|---|---|
| Total | 124 | |
| Race | ||
| White | 47 | (37.9) |
| Black or African American | 39 | (31.5) |
| Latino/Hispanic | 19 | (15.3) |
| Other† | 19 | (15.3) |
| Age, mean (SD) | 40.5 | (11.3) |
| Self-reported HIV status | ||
| Negative | 66 | (53.2) |
| Positive | 58 | (46.8) |
| Binge alcohol use frequency | ||
| Never | 12 | (9.7) |
| Less than once per month | 6 | (4.8) |
| About once per month | 10 | (8.1) |
| Two days per month | 2 | (1.6) |
| Three days per month | 4 | (3.2) |
| Four days per month | 27 | (21.8) |
| Two days per week | 20 | (16.1) |
| Three days per week | 14 | (11.3) |
| Four days per week | 11 | (8.9) |
| Five to six days per week | 9 | (7.3) |
| Every day | 9 | (7.3) |
| Situational binge drinking (i.e. concurrent with anal sex) in the last three months | ||
| Never | 45 | (36.3) |
| 1 to 5 times | 48 | (38.7) |
| 5 to 10 times | 17 | (13.7) |
| More than 10 times | 14 | (11.3) |
| Methamphetamine Use Frequency | ||
| Never | 12 | (9.7) |
| Less than once per month | 4 | (3.2) |
| About once per month | 2 | (1.6) |
| Two days per month | 13 | (10.5) |
| Three days per month | 11 | (8.9) |
| Four days per month | 25 | (20.2) |
| Two to three days per week | 48 | (38.7) |
| Four to six days per week | 7 | (5.6) |
| Every day | 2 | (1.6) |
| Condomless anal sex concurrent with binge drinking or methamphetamine use in last three months | 85 | (68.5) |
“Other” race/ethnicity includes Asian, Pacific Islander, Native American, mixed, and other racial/ethnic groups not otherwise specified.
STATISTICAL ANALYSIS
Because exact counts of CAI episodes were not available, we used multivariable logistic regression to examine the relationship between situational binge drinking frequency and the odds of any CAI in the last three months, controlling for demographic and clinical characteristics and frequency of methamphetamine use. For this study, our measure for CAI included only CAI that was reported to be concurrent with methamphetamine use or binge drinking—these two substances were the focus of the parent study. Consistent with previous studies (Colfax et al., 2004; Santos et al., 2013), frequency of methamphetamine use was categorized as no use, less than weekly, and weekly or more. To mitigate potential recall or precision issues with our measure of situational binge drinking frequency, we conducted a sensitivity analysis in which situational binge drinking was included in the model as a binary variable indicating any situational binge drinking.
RESULTS
STUDY SAMPLE CHARACTERISTICS
Participants were excluded if they were female sex at birth (n=1), identified as transfemale (n=7), did not speak English (n=1), reported their HIV status as “unknown” (n=1), or reported current use of PrEP (n=1), as this reduces the sexual risk associated with CAI. The final sample included 124 of the original 135 MSM surveyed. Ninety percent reported binge drinking and 64% reported situational binge drinking in the last three months. Sixty-nine percent of participants reported any CAI in the last three months.
STATISTICAL ANALYSIS
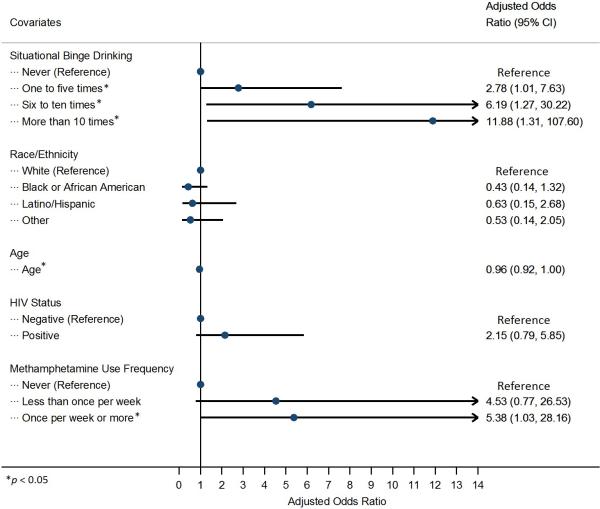
In multivariable analysis, there was a positive relationship between frequency of situational binge drinking and CAI (1 to 5 times vs. never: adjusted odds ratio = 2.78, 95% CI = 1.01-7.63; 6 to 10 times vs. never: 6.19, 1.27-30.22; more than 10 times vs. never: 11.88, 1.31-107.60) (Figure 1). In our sensitivity analysis, there was a positive relationship between any situational binge drinking and CAI (3.88, 1.50-10.02).
Figure 1.
Multivariable logistic regression assessing odds of any condomless anal intercourse concurrent with methamphetamine or binge alcohol use in the last three months (n=124)
DISCUSSION
We found a positive relationship between situational binge drinking and risky sexual behavior. By filling a methodological gap and complementing existing global and event-level analyses, the present study strengthens the evidence linking binge drinking and CAI. Although mounting research supports this link, interventions to address binge drinking have failed to reach MSM. Indeed, only 20% of MSM who use alcohol or non-injection drugs have ever participated in alcohol or drug treatment programs (Finlayson et al., 2011). In a large quasi-probability sample of MSM in San Francisco, only 13% of binge-drinking MSM had ever sought alcohol treatment (Santos, Jin, & Raymond, 2015), highlighting the need to expand the reach of existing interventions as well as explore novel interventions (Santos, Das, & Colfax, 2011). However, a recent systematic review of studies assessing the efficacy of alcohol-reduction interventions among MSM noted that such research is “alarmingly scarce” (Wray et al., 2015). Despite this gap, a small number of studies suggest that interventions utilizing motivational interviewing, cognitive behavioral therapy, or pharmacologic agents may be effective in reducing heavy drinking among MSM (Morgenstern et al., 2007; Morgenstern et al., 2012; Santos, Coffin, et al., 2015; Velasquez et al., 2009). Regardless of these advances, it is clear that efforts to identify effective strategies to reduce problematic alcohol use in this population need to be greatly expanded.
Our study has several limitations. First, our non-probability sample reported higher prevalence of methamphetamine use and binge drinking compared to MSM nationally thus may not be generalizable to the broader MSM population (Centers for Disease Control and Prevention, 2016). Second, the self-reported data used in this study may be subject to social desirability bias and the three month recall for substance use and sexual behaviors may make responses vulnerable to recall bias. Third, although our analysis adds to existing global and event-level analyses and provides a nuanced approach to assessing the link between binge drinking and sexual risk, our aggregate measure of situational binge drinking frequency precludes the establishment of a causal link with risky sexual behavior. Fourth, our CAI measure only included CAI that occurred concurrently with methamphetamine use or binge drinking so may not capture all CAI events among our participants. Fifth, because we leveraged limited phone screen data, we did not have access to other potential confounders associated with substance use and sexual risk, including the total number of AI events beyond those that were concurrent with methamphetamine use or binge drinking.
By establishing a positive relationship between situational binge drinking frequency and aggregate sexual risk behavior, the present study strengthens the evidence in support of this link, enhances the comparability of the existing literature, and further suggests that the integration of dual strategies that aim to prevent HIV and reduce binge drinking may be warranted.
Acknowledgments
FUNDING
This study was funded by the National Institutes of Drug Abuse (NIDA) under grant number R36DA035109A.
Footnotes
DISCLAIMER
The authors are solely responsible for the content of this article, which does not necessarily represent the official views of the San Francisco Department or Public Health.
REFERENCES
- Centers for Disease Control and Prevention Vital signs: binge drinking prevalence, frequency, and intensity among adults - United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61(1):14–19. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV Risk, Prevention, and Testing Behaviors— National HIV Behavioral Surveillance System: Men Who Have Sex With Men, 20 U.S. Cities, 2011. HIV Surveillance Special Report. 2014;8 [Google Scholar]
- Centers for Disease Control and Prevention Diagnoses of HIV infection in the United States and dependent areas, 2014. HIV Surveillance Report. 2015;26 [Google Scholar]
- Centers for Disease Control and Prevention HIV Infection Risk, Prevention, and Testing Behaviors among Men Who Have Sex With Men—National HIV Behavioral Surveillance, 20 U.S. Cities, 2014. HIV Surveillance Special Report. 2016 [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Team ES. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159(10):1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Ekstrand ML, Stall RD, Paul JP, Osmond DH, Coates TJ. Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS. 1999;13(12):1525–1533. doi: 10.1097/00002030-199908200-00013. [DOI] [PubMed] [Google Scholar]
- Finlayson TJ, Le B, Smith A, Bowles K, Cribbin M, Miles I. HIV risk, prevention, and testing behaviors among men who have sex with men--National HIV Behavioral Surveillance System, 21 U.S. cities, United States, 2008. MMWR Surveill Summ. 2011;60(14):1–34. Prevention. [PubMed] [Google Scholar]
- Folch C, Esteve A, Zaragoza K, Munoz R, Casabona J. Correlates of intensive alcohol and drug use in men who have sex with men in Catalonia, Spain. Eur J Public Health. 2010;20(2):139–145. doi: 10.1093/eurpub/ckp091. doi: 10.1093/eurpub/ckp091. [DOI] [PubMed] [Google Scholar]
- Greenwood GL, White EW, Page-Shafer K, Bein E, Osmond DH, Paul J, Stall RD. Correlates of heavy substance use among young gay and bisexual men: The San Francisco Young Men's Health Study. Drug Alcohol Depend. 2001;61(2):105–112. doi: 10.1016/s0376-8716(00)00129-0. [DOI] [PubMed] [Google Scholar]
- Hess KL, Chavez PR, Kanny D, DiNenno E, Lansky A, Paz-Bailey G, Group NS. Binge drinking and risky sexual behavior among HIV-negative and unknown HIV status men who have sex with men, 20 US cities. Drug Alcohol Depend. 2015;147:46–52. doi: 10.1016/j.drugalcdep.2014.12.013. doi: 10.1016/j.drugalcdep.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin TW, Morgenstern J, Parsons JT, Wainberg M, Labouvie E. Alcohol and sexual HIV risk behavior among problem drinking men who have sex with men: An event level analysis of timeline followback data. AIDS Behav. 2006;10(3):299–307. doi: 10.1007/s10461-005-9045-7. doi: 10.1007/s10461-005-9045-7. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Wray TB, Pantalone DW, Kruis RD, Mastroleo NR, Monti PM, Mayer KH. Daily associations between alcohol use and unprotected anal sex among heavy drinking HIV-positive men who have sex with men. AIDS Behav. 2015;19(3):422–430. doi: 10.1007/s10461-014-0896-7. doi: 10.1007/s10461-014-0896-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorimer K, Kidd L, Lawrence M, McPherson K, Cayless S, Cornish F. Systematic review of reviews of behavioural HIV prevention interventions among men who have sex with men. AIDS Care. 2013;25(2):133–150. doi: 10.1080/09540121.2012.699672. doi: 10.1080/09540121.2012.699672. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux DA, Jr., Schulz-Heik J. A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. J Consult Clin Psychol. 2007;75(1):72–84. doi: 10.1037/0022-006X.75.1.72. doi: 10.1037/0022-006X.75.1.72. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Kuerbis AN, Chen AC, Kahler CW, Bux DA, Jr., Kranzler HR. A randomized clinical trial of naltrexone and behavioral therapy for problem drinking men who have sex with men. J Consult Clin Psychol. 2012;80(5):863–875. doi: 10.1037/a0028615. doi: 10.1037/a0028615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Denny C, Serdula MK, Marks JS. Binge drinking among US adults. JAMA. 2003;289(1):70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism . Tenth Special Report to the U.S. Congress on Alcohol and Health. National Institutes of Health; Bethesda, MD: 2000. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism NIAAA Newsletter Winter 2004. 2004 Retrieved from http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf.
- Pinkerton SD, Galletly CL, McAuliffe TL, DiFranceisco W, Raymond HF, Chesson HW. Aggregate versus individual-level sexual behavior assessment: how much detail is needed to accurately estimate HIV/STI risk? Eval Rev. 2010;34(1):19–34. doi: 10.1177/0193841X09353534. doi: 10.1177/0193841X09353534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Coffin P, Santos D, Huffaker S, Matheson T, Euren J, Batki SL. Feasibility, acceptability and tolerability of targeted naltrexone for non-dependent methamphetamine-using and binge-drinking men who have sex with men. J Acquir Immune Defic Syndr. 2015 doi: 10.1097/QAI.0000000000000922. doi: 10.1097/QAI.0000000000000922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Coffin PO, Das M, Matheson T, DeMicco E, Raiford JL, Herbst JH. Dose-response associations between number and frequency of substance use and high-risk sexual behaviors among HIV-negative substance-using men who have sex with men (SUMSM) in San Francisco. J Acquir Immune Defic Syndr. 2013;63(4):540–544. doi: 10.1097/QAI.0b013e318293f10b. doi: 10.1097/QAI.0b013e318293f10b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Das M, Colfax GN. Interventions for non-injection substance use among US men who have sex with men: what is needed. AIDS Behav. 2011;15(Suppl 1):S51–56. doi: 10.1007/s10461-011-9923-0. doi: 10.1007/s10461-011-9923-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Jin H, Raymond HF. Pervasive Heavy Alcohol Use and Correlates of Increasing Levels of Binge Drinking among Men Who Have Sex with Men, San Francisco, 2011. J Urban Health. 2015;92(4):687–700. doi: 10.1007/s11524-015-9958-z. doi: 10.1007/s11524-015-9958-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velasquez MM, von Sternberg K, Johnson DH, Green C, Carbonari JP, Parsons JT. Reducing sexual risk behaviors and alcohol use among HIV-positive men who have sex with men: a randomized clinical trial. J Consult Clin Psychol. 2009;77(4):657–667. doi: 10.1037/a0015519. doi: 10.1037/a0015519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16(6):1394–1410. doi: 10.1007/s10461-011-0131-8. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Wray TB, Grin B, Dorfman L, Glynn TR, Kahler CW, Marshall BD, Operario D. Systematic review of interventions to reduce problematic alcohol use in men who have se x with men. Drug Alcohol Rev. 2015 doi: 10.1111/dar.12271. doi: 10.1111/dar.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]