Abstract
Purpose
We aimed to assess the effects of comorbidities on COPD costs and to investigate the relationship between comorbidities and clinical variables.
Patients and methods
All patients hospitalized with a diagnosis of COPD exacerbation between January 1, 2014, and December 31, 2014, at all state hospitals of Aydın province, a city located in the western part of Turkey, were included in this study. The costs examined in the study pertained to medications, laboratory tests, hospital stays, and other treatment-related factors, such as consumption of materials, doctor visits, and consultation fees.
Results
A total of 3,095 patients with 5,237 exacerbations (mean age, 71.9±10.5 years; 2,434 males and 661 females) were evaluated. For 880 of the patients (28.9%), or 3,852 of the exacerbations (73.1%), at least one comorbid disease was recorded. The mean cost of each exacerbation was $808.5±1,586, including $325.1±879.9 (40.7%) for hospital stays, $223.1±1,300.9 (27.6%) for medications, $46.3±49.6 (0.9%) for laboratory expenditures, and $214±1,068 (26.5%) for other treatment-related factors, such as consumption of materials, doctor visits, and consultation fees. The cost of each exacerbation was $1,014.9 in patients with at least one comorbidity, whereas it was $233.6 in patients without comorbidity (P<0.001). Age >65 years, female gender, hospitalization in an intensive care unit, invasive or noninvasive mechanical ventilation, and a long duration of hospitalization were all found to be significant factors in increasing total costs during the exacerbations requiring hospitalization (P<0.05 for all).
Conclusion
Comorbidities have an important role in the total costs of acute exacerbations of COPD. Strategies for the prevention, diagnosis, and effective management of comorbidities would decrease the overall financial burden associated with acute exacerbations of COPD.
Keywords: COPD, exacerbation, cost, comorbidity, morbidity, intensive care unit
Introduction
COPD, a common public health problem worldwide, is characterized by irreversible progressive airway obstruction and systemic inflammation as a result of exposure to smoking, noxious gases, and particles.1
According to the World Health Organization (WHO), COPD is the fourth most common cause of death and is estimated to be third by the year 2020.2,3 In addition to its high mortality and morbidity rates, COPD is a very expensive disease and constitutes a significant liability to a nation’s health care costs. For example, the annual cost of treatment for a patient with COPD is $9,981 in the USA and $3,224 in the UK.4 Because of continued exposure to COPD risk factors and an aging population, the global burden of COPD is expected to increase further in the coming years.
The main cost load of COPD consists of acute exacerbations, a finding that has been highlighted in studies conducted in Turkey.5–7 On average, patients with COPD experience one to three exacerbations per year. These exacerbations comprise the main reason for emergency department treatment and hospitalization. Acute exacerbations adversely affect the prognosis of the disease and accelerate the process of severe respiratory failure. Also, exacerbations become more frequent and more severe as the disease progresses.8,9 In turn, severe COPD exacerbations requiring mechanical ventilation and intensive care trigger higher costs.
Another important component of COPD-related costs is the disease’s comorbidities. Multisystem involvement with significant extrapulmonary manifestations is associated with COPD, and patients frequently suffer from comorbidities such as cardiovascular disease, osteoporosis, depression, malnutrition, metabolic syndrome, diabetes, and lung cancer.1 These comorbidities have a major impact on the patient’s quality of life and survival. Previous reports have shown that >60% of COPD patient deaths are caused by comorbidities rather than by COPD itself.10,11
Although the high costs associated with COPD and the disease’s comorbidity rates are well known,12,13 studies on the effects of comorbidities on the disease’s costs are both limited and controversial.14–17 However, the management of comorbidities and their prevention might provide some benefit in reducing the global cost load. Accordingly, in this study, we aimed to assess the effects of comorbidities on COPD costs and to investigate the relationship between comorbidities and clinical variables such as age, gender, and the requirement of intensive care or mechanical ventilation.
Patients and methods
Study design and population
This retrospective descriptive case-series study included all patients older than 40 years who were hospitalized with a diagnosis of COPD exacerbation between January 1, 2014, and December 31, 2014, at all state hospitals of Aydın province, a city located on the Aegean Seacoast in the western part of Turkey and having a population of one million. In this study, COPD exacerbation was defined as an acute change in baseline dyspnea as well as cough and/or sputum production.1 Patients who were admitted to a hospital more than once were excluded. The study was approved by the Institutional Ethics Committee of Adnan Menderes University Faculty of Medicine (no 2015/617). The informed consent requirement was waived by the Institutional Ethics Committee due to the study’s retrospective design.
Study procedures and data collection
The data on demographics, diagnoses, comorbid diseases, treatment procedures, total costs and a breakdown of cost per exacerbation, hospitalization duration, length of intensive care unit stay, and spirometric measures were obtained from the hospitals’ databases.
The costs examined in the study pertained to medications, laboratory tests, hospital stays, and other treatment-related factors such as consumption of materials, doctor visits, and consultation fees. Costs recorded as Turkish lira (TL) in the hospital data were converted into US dollars based on 2014 average currency (1$ was equal to 2.24 TL in 2014 and to 3.06 TL in 2016).
Statistical analysis
The study data were summarized by the descriptive statistics (mean, standard deviation, minimum, median, maximum, frequency, and percentage). The difference between two independent groups showing a nonnormal distribution was investigated using Mann–Whitney U test. The relation between categorical variables was tested either by the chi-square test or by the Fisher’s exact test. A linear regression analysis was performed to estimate the relation between the cost and duration of a hospitalization. The level of statistical significance was determined as 0.05. Analyses were performed using the MedCalc statistical software program (Version 12.7.7; MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2013).
Results
Study patients
A total of 3,095 patients with 5,237 exacerbations (mean age, 71.9±10.5 years; 2,434 males and 661 females) were evaluated. The patients’ mean forced expiratory volume per 1 second (FEV1) was 32%±4.8%.
Cost of COPD exacerbations
The mean cost of each exacerbation was $808.5±1,586 including $325.1±879.9 (40.7%) for hospital stays, $223.1±1,300.9 (27.6%) for medications, $46.3±49.6 (0.9%) for laboratory expenditures, and $214±1,068 (26.5%) for other treatment-related factors, such as consumption of materials, doctor visits, and consultation fees. The portion of antibiotic expenditures included in the medication costs was $44.4±94.4 on average (Table 1).
Table 1.
The breakdown of the costs for COPD exacerbations
| Variable | Cost in $ (mean ± standard deviation) | Breakdown of cost (%) |
|---|---|---|
| Cost of hospital stay | 325.1±879.9 | 40.7 |
| Cost of medication | 223.1±1,300.9 | 27.6 |
| Cost of laboratory | 46.3±49.6 | 0.9 |
| Other costs (consumption materials, doctor visits, and consultation fee) | 214±1,068 | 26.5 |
| Total cost | 808.5±1,586 | 100 |
Eight hundred forty-one of the exacerbations required hospitalization in intensive care units. For 303 of these attacks, invasive mechanical ventilation was applied, whereas noninvasive mechanical ventilation was applied in 406 cases, and 130 cases were followed up solely by monitoring. The cost related to the exacerbations requiring stays in intensive care units was $1,978±2,459. The mean duration of hospitalization for all exacerbations was 8.1±6.3 days, whereas it was 10.4±8.9 days for those of patients hospitalized in intensive care units.
Age >65 years, female gender, hospitalization in an intensive care unit, invasive or noninvasive mechanical ventilation, and a long duration of hospitalization were all found to be significant factors in increasing total costs during the exacerbations requiring hospitalization (P<0.05 for all) (Table 2). The duration of hospitalization was positively correlated with all costs, including laboratory (r=0.220, P<0.001), medication (r=0.681, P<0.001), hospital stay (r=0.712, P<0.001), and total (r=0.660, P<0.001) costs.
Table 2.
The relationship between demographic/clinical variables and the cost
| Variable | n | Cost of laboratory ($) | Cost of medication ($) | Cost of hospital stay ($) | Total cost ($) |
|---|---|---|---|---|---|
| Age (years) | |||||
| <65 | 1,193 | 44.4±52.4 | 200.4±637.5 | 293.5±754.9 | 738.9±1,368 |
| ≥65 | 4,044 | 46.8±48.8 | 229.9±1,439.7 | 334.5±913.8 | 829.1±1,644.7 |
| P-value | 0.004 | 0.076 | <0.001 | 0.003 | |
| Gender | |||||
| Female | 841 | 58±60.8 | 175.7±460.7 | 399.1±1,019.1 | 922.5±1,597.5 |
| Male | 4,396 | 44.1±46.9 | 232.2±1,405.4 | 311±850.5 | 786.8±1,583 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Intensive care stay | |||||
| Absent | 4,396 | 39.6±40.7 | 205.2±1,149.6 | 200.3±494.6 | 584.9±1,236.8 |
| Present | 841 | 84.1±71 | 316.6±1,910.5 | 976.2±1,749.1 | 1,976.2±2,465.1 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Intubation | |||||
| Absent | 4,932 | 43.1±45.5 | 205±1,095.3 | 232.9±477.5 | 656.1±1,232.6 |
| Present | 305 | 97.5±78 | 516.6±3,099.8 | 1,816.1±2,697 | 3,273.3±3,495.8 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Noninvasive mechanical ventilation | |||||
| Absent | 4,831 | 43.7±47.6 | 215.8±1,339.7 | 290.3±888.6 | 730.7±1,562 |
| Present | 406 | 76.9±61.6 | 310.3±689 | 739.5±642.6 | 1,735.7±1,581 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
Cost of comorbidities
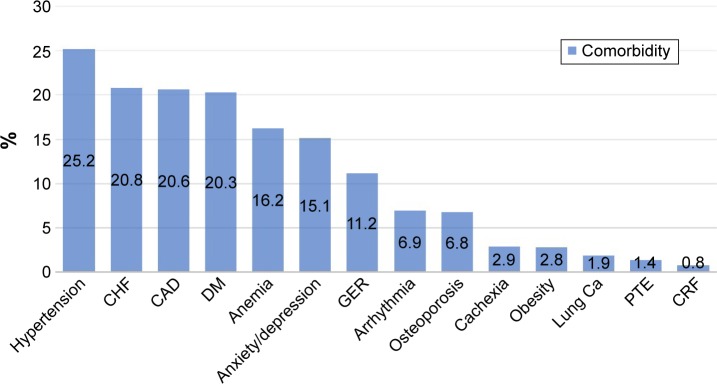
For 880 of the patients (28.9%), or 3,852 of the exacerbations (73.1%), at least one comorbid disease was recorded. The comorbidities constituted hypertension in 780 patients (25.2%), congestive heart failure in 645 patients (20.8%), coronary artery disease in 637 patients (20.6%), diabetes mellitus in 628 patients (20.3%), anemia in 501 patients (16.2%), gastroesophageal reflux in 348 patients (11.2%), anxiety/depression in 467 patients (15.1%), arrhythmia in 213 patients (6.9%), lung cancer in 58 patients (1.9%), pulmonary thromboembolism in 44 patients (1.4%), chronic renal failure in 25 patients (0.8%), cachexia in 91 patients (2.9%), obesity in 88 patients (2.8%), and osteoporosis in 211 patients (6.8%) (Figure 1).
Figure 1.
The prevalence of comorbidities.
Abbreviations: Ca, cancer; CAD, coronary artery disease; CHF, congestive heart failure; CRF, chronic renal failure; DM, diabetes mellitus; GER, gastroesophageal reflux; PTE, pulmonary thromboembolism.
Total cost was significantly higher in patients with exacerbations accompanied by any comorbidity than in those having no comorbidity. Considering comorbid diseases, total cost was found to be statistically and significantly much higher in cases with pneumonia, diabetes mellitus, cardiac failure, hypertension, coronary artery disease, anemia, lung cancer, arrhythmia, anxiety/depression, and osteoporosis (Table 3).
Table 3.
Diseases concomitant to COPD exacerbations and their effects on the cost
| Kind of comorbidity | n | Cost of laboratory ($) | Cost of medication ($) | Cost of hospital stay ($) | Total cost ($) |
|---|---|---|---|---|---|
| Pneumonia | |||||
| Absent | 4,297 | 44.6±46.8 | 206.5±1,151.3 | 291.1±667.1 | 726±1,281.3 |
| Present | 940 | 53.7±60.4 | 229.2±1,835.4 | 480.5±1,501.6 | 1,185.9±2,519 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Diabetes | |||||
| Absent | 4,182 | 42.5±46 | 182.6±1,134.8 | 245.3±524 | 630.2±1,114.5 |
| Present | 1,055 | 61.1±59.1 | 383.8±1,808.8 | 641.5±1,623 | 1,515.5±2,635.3 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Heart failure | |||||
| Absent | 4,252 | 40.7±42.9 | 188.2±1,366.4 | 222±63.1 | 583.3±9,425.6 |
| Present | 985 | 70.6±66.7 | 374.3±955.9 | 770.1±1,660.4 | 1,780.8±2,894.2 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Hypertension | |||||
| Absent | 4,040 | 38.7±38.75 | 164.7±1,351.7 | 194.3±423.9 | 502.2±750 |
| Present | 1,197 | 72±69.8 | 420.3±1,091.7 | 766.5±1,591 | 1,841±2,780.5 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Coronary artery disease | |||||
| Absent | 4,225 | 40.6±40.8 | 165.8±1,081.8 | 211.3±544.9 | 553.1±984.3 |
| Present | 1,012 | 70.1±71.1 | 462.7±1,951.1 | 800.3±1,578.6 | 1,875.1±2,751.3 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Anemia | |||||
| Absent | 4,510 | 40.8±40.9 | 179.9±1,302.9 | 213.7±699.3 | 595.4±1,133 |
| Present | 727 | 80.4±77.5 | 489.2±1,258.8 | 904.9±1,469.6 | 2,131.2±2,852.4 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Reflux | |||||
| Absent | 4,608 | 46.6±50.7 | 225±1,375.5 | 315.8±898.6 | 795.1±1,622.9 |
| Present | 629 | 44.2±41.2 | 209.7±483.4 | 393.2±728.7 | 906.4±1,281.8 |
| P-value | 0.982 | <0.001 | <0.001 | <0.001 | |
| Lung cancer | |||||
| Absent | 5,143 | 46.1±49.7 | 213.1±1,078.6 | 325±884.2 | 806.5±1,589.7 |
| Present | 94 | 54.6±47 | 771.9±5,539.3 | 331.3±629.2 | 919.6±1,387.4 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Pulmonary thromboemboli | |||||
| Absent | 5,158 | 46.3±49.7 | 219.6±1,289.6 | 323±862.1 | 803.6±1,556.2 |
| Present | 79 | 44.1±44.3 | 450.1±1,910.6 | 462.1±1,687.8 | 1,110.8±3,639 |
| P-value | 0.011 | 0.006 | 0.126 | 0.028 | |
| Arrhythmia | |||||
| Absent | 4,903 | 45.7±48.6 | 215.7±1,327.1 | 311.1±883.5 | 774.8±1,574.8 |
| Present | 333 | 55.4±62.7 | 332.8±821.3 | 531.9±802.9 | 1,306.9±1,671.7 |
| P-value | 0.001 | <0.001 | <0.001 | <0.001 | |
| Malnutrition | |||||
| Absent | 5,072 | 46.3±49.7 | 224.1±1,321 | 324.2±85.4 | 807±1,602.7 |
| Present | 165 | 47.8±46.3 | 194±305 | 354±546.3 | 858±952.1 |
| P-value | 0.495 | 0.155 | 0.001 | 0.003 | |
| Obesity | |||||
| Absent | 5,089 | 46±49.33 | 220.5±1,313 | 324.4±888.3 | 804.6±1,594.3 |
| Present | 148 | 54.4±58.9 | 314.5±788.9 | 349.1±84.6 | 954.4±1,272.5 |
| P-value | 0.150 | 0.005 | 0.042 | 0.014 | |
| Anxiety/depression | |||||
| Absent | 4,173 | 42.3±46.3 | 201±1,162.8 | 289.8±925 | 729.6±1,655.7 |
| Present | 1,063 | 61.8±58.5 | 310±1,740 | 463.9±658.9 | 1,118.7±1,230.8 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
| Osteoporosis | |||||
| Absent | 4,952 | 45.5±48.7 | 222.8±1,334.7 | 310.5±818.9 | 784.5±1,548.1 |
| Present | 285 | 59.5±61.4 | 227.9±396.1 | 578.4±1,589.5 | 1,226.5±2,102.6 |
| P-value | <0.001 | 0.001 | <0.001 | <0.001 | |
| Total comorbidities | |||||
| Absent | 1,383 | 27.5±22.94 | 120±1,744.6 | 79±101.2 | 233.6±176.5 |
| Present | 3,852 | 53±54.6 | 260.1±1,097.1 | 413.4±1,009.4 | 1,014.9±1,801.9 |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |
Discussion
COPD is a disease that affects patients’ quality of life due to its progressive and continuously symptomatic nature. Almost all patients have reduced physical activity, and they experience two or more symptoms every day. For this reason, patients with COPD must continuously use a high volume of medications, which produces a significant cost load. Although the possibility of reducing the cost of chronic medication is low, exacerbations might be reduced or prevented. Exacerbations constitute 50%–75% of the economic load of COPD because of extra emergency department applications and increased hospitalizations.18 Studies on the causality between treating exacerbations and slowing down the progression of COPD have indicated that successful management of the exacerbations is the main approach for reducing the costs, both directly and also indirectly, by slowing the progression of the disease.1,16 In this study, the total cost of hospitalization due to COPD exacerbations was found to be $808. Previous studies have reported a wide range of cost per hospitalization (between $612 and $9,545).5–7,19–24
In this study, while the cost of hospital stays composes the main portion of total costs (40.7%), other costs such as those for medication, consumption of materials, consultations, and doctor visits, plus laboratory expenditures, constitute a significant percentage of total costs. In previous studies, the main cost is associated with hospital stays, followed by laboratory expenditures and medication costs.19,20 Therefore, a major reduction in COPD-related costs could be achieved by reducing the expenditures of staying in hospital.
Comorbidities in COPD
The main reason for the hospitalization of COPD patients is the presence of comorbidities with or without exacerbation: these patients have a higher prevalence of comorbid diseases compared to the general population.12,13 Although the mechanisms by which COPD-related comorbidities develop are still unclear, it has been suggested that systemic inflammation contributes to the disease process. However, the causes of comorbidities are more likely to be multifactorial (eg, inactivity, poor diet, hypoxia, and inflammation).1 Comorbidity existence is a critical factor associated with high mortality in COPD.12,13 Diabetes, heart failure, renal failure, cancer, and neuropsychiatric diseases are common with aging and often occur together;25,26 if any of these diseases exists, the possibility that others exist is higher in these individuals compared to healthy adults.27 In a previous study, more than three comorbid disorders were observed in 46% of COPD patients.28 In our study, two comorbid diseases were recorded in 28.9% of patients, the most common being hypertension, followed by other cardiovascular diseases, such as coronary artery disease and congestive heart failure, as well as diabetes mellitus. Similarly, in the literature, cerebrovascular disease, mainly hypertension, was reported to be the most common comorbidity in patients with COPD.13,14,29 In a study by Miyazaki et al,30 36% of patients with COPD had hypertension and 32% had cardiovascular disease, while 25% had cancer, 17% had mental disorders, and 15% had diabetes mellitus. In this study, comorbid disease was observed in 808 patients; the most common comorbid disease was hypertension, followed by other cardiovascular diseases and diabetes, anemia, anxiety/depression, and other disorders.
Cost of COPD exacerbations and comorbidities
In this study, the exacerbation-related costs for patients with at least one comorbidity totaled $2,273, whereas the costs for patients with COPD exacerbations but no comorbidity totaled $523. The presence of comorbidities significantly increased the total costs associated with COPD exacerbations. The costs of COPD exacerbation associated with pneumonia, diabetes mellitus, heart failure, hypertension, coronary artery disease, anemia, lung cancer, arrhythmia, and anxiety/depression were found to be significantly higher than those associated with COPD without comorbidities. Comorbidities most significantly related to high costs were anemia, coronary artery disease, and hypertension, likely because they are the most common comorbid diseases.
Previous studies have demonstrated a direct relationship between the yearly costs of COPD and the number of comorbid diseases.15,23,31 Perera et al23 assessed the factors responsible for increasing costs for patients hospitalized due to exacerbation and reported a significant relation between increased costs and comorbidities, such as acute myocardial infarction, congestive heart failure, cerebrovascular disease, lung cancer, arrhythmia, pulmonary thromboembolism, and low body weight. COPD patients with comorbidities require hospitalization, which lead to increased costs. Moreover, ~50% of COPD patients use cardiovascular medications and, more frequently, analgesic, antibiotics, and psychotherapeutic drugs.31 One study of COPD patients with comorbid diseases showed direct costs that were 4.7 times higher than those for COPD patients with no comorbidity.14 Similarly, our study found that the costs associated with comorbid diseases were 4.3 times higher. Pneumonia was found to be associated with both direct and indirect costs. Some studies have demonstrated that pneumonia increases total direct costs by 1.9–2.5 times for outpatients and by 3.39–4.72 times for hospitalized patients.15,32 In this study, costs were 1.6 times higher in patients with pneumonia compared to those without pneumonia.
Dalal et al22 observed that yearly direct costs were 38% more in COPD patients with cardiovascular disease compared to patients with COPD only. Pasquale et al16 investigated the yearly costs of COPD cases and noted that the existence of cardiovascular disease (1.69 times higher) and diabetes mellitus (1.46 times higher) was found to be associated with increased yearly costs for COPD patients. In our study, cardiovascular disease (3.4 times higher) and diabetes mellitus (2.4 times higher) were found to be related to increased costs. In a study performed by Halpern et al,17 anemia increased costs for hospitalized patients by ~2.5 times. This ratio was 3.5 times in our study. In addition, in previous studies, hypertension, cor pulmonale, chronic renal failure, peptic ulcer, liver disease, and apnea were shown to increase the total cost of COPD.6,7,33–35
Other clinical factors affecting the cost of COPD
In this study, age >65 years, female gender, hospitalization in an intensive care unit, intubation, noninvasive mechanical ventilation, and a long duration of hospitalization were factors increasing costs for patients with COPD exacerbations who required hospitalization. The mean duration of hospitalization was 8.1 days in this study. In previous studies, the mean duration was 4.5–14.5 days.5–7,19,22–24 A longer hospital duration is also associated with increased daily costs due to treatment-resistant, severe cases with many accompanying comorbidities in addition to increased expenditures for hospital stays. The relationship between increased costs and a lengthy hospital stay has been demonstrated in many studies.6,23,33
In our study, the rate of exacerbations requiring hospitalization in intensive care units was 16% (n=841), and the mean hospitalization duration was 10.4 days. The mean cost of hospitalization in an intensive care unit was $1,977, which was 3.4 times higher compared to cases without intensive care unit hospitalization. Being followed by noninvasive mechanical ventilation or intubation was also found to be associated with increased costs. In cases who require hospitalization in intensive care units, the costs of laboratory tests and medications increase as hospitalization time is extended. Similar to our study, Dalal et al22 reported that the duration of hospitalization was longer in terms of exacerbations requiring hospitalization in intensive care units and the cost was nearly doubled for cases in which patients were hospitalized in intensive care units compared to those who did not require intensive care hospitalization. Stanford et al36 found that costs were nearly six times higher, and Örnek et al6 noted that costs were tripled for COPD patients hospitalized in intensive care units.
Limitations
Although this study is valuable because it included a large number of patients and exacerbations, it had some limitations that need to be mentioned. First, the retrospective design may have led to data loss, which precludes a definitive conclusion. Furthermore, our results reflect COPD-related costs in Turkey, which complicates the generalization of our data to other countries.
Conclusion
Comorbidities have an important role in the total costs of acute exacerbations of COPD. Strategies for the prevention, diagnosis, and effective management of comorbidities would decrease the overall financial burden associated with acute exacerbations of COPD.
Clinical implications
The costs of acute exacerbations of COPD are mainly associated with comorbidities. During routine follow-up, questioning the patient about, as well as managing the most common comorbidities, such as diabetes mellitus, hypertension, and arrhythmia might reduce the cost load. Furthermore, COPD patients have a sedentary lifestyle due to limitations of daily physical activities, which causes a tendency toward anxiety and depression. Thus, during routine visits, patients with advanced COPD should be evaluated with respect to their psychological mood and be provided with psychosocial support, pulmonary rehabilitation, and physical exercise programs. The implementation of these measures would decrease the cost load of COPD and increase the cost-effectivity of managing the disease. Finally, the prevention of pneumonia through vaccination of COPD patients and avoiding the usage of unnecessary and high-dose inhaled steroids should also be considered in efforts to decrease the cost of COPD management.
Footnotes
Author contributions
SD designed the study, collected the data, and prepared the article. AŞ and YA prepared the article, analyzed the data, and searched the literature. JÇE and MHÖ reviewed the article. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. 2016. [Accessed August 20, 2016]. Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/
- 2.World Health Organization [webpage on the Internet] Global Health Observatory Data Repository. 2016. [Accessed August 20, 2016]. Available from: http://apps.who.int/gho/data/node.main.CODWORLD?lang=en.
- 3.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349(9064):1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 4.Foo J, Landis SH, Maskell J, et al. Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLoS One. 2016;11(4):e0152618. doi: 10.1371/journal.pone.0152618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozkaya S, Findik S, Atici AG. The costs of hospitalization in patients with acute exacerbation of chronic obstructive pulmonary disease. Clinicoecon Outcomes Res. 2011;3:15–18. doi: 10.2147/CEOR.S14820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Örnek T, Tor M, Altın R, et al. Clinical factors affecting the direct cost of patients hospitalized with acute exacerbation of chronic obstructive pulmonary disease. Int J Med Sci. 2012;9(4):285–290. doi: 10.7150/ijms.4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emre JC, Özdemir O, Baysak A, et al. Clinical factors affecting the costs of hospitalized chronic obstructive pulmonary disease exacerbations. Eurasian J Pulmonol. 2014;16:180–183. [Google Scholar]
- 8.O’Reilly CF, Williams AE, Holt K, Rice L. Defining COPD exacerbations: impact on estimation of incidence and burden in primary care. Prim Care Respir J. 2006;15(6):346–353. doi: 10.1016/j.pcrj.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hurst JR, Vestbo J, Anzueto A, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. doi: 10.1056/NEJMoa0909883. [DOI] [PubMed] [Google Scholar]
- 10.Berry CE, Wise RA. Mortality in COPD: causes, risk factors, and prevention. COPD. 2010;7(5):375–382. doi: 10.3109/15412555.2010.510160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA, TORCH Clinical Endpoint Committee Ascertainment of cause-specific mortality in COPD: operations of the TORCH clinical endpoint committee. Thorax. 2007;62(5):411–415. doi: 10.1136/thx.2006.072348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–1257. doi: 10.1183/09031936.00133805. [DOI] [PubMed] [Google Scholar]
- 13.Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32(4):962–969. doi: 10.1183/09031936.00012408. [DOI] [PubMed] [Google Scholar]
- 14.Mapel DW, Hurley JS, Frost FJ, Petersen HV, Picchi MA, Coultas DB. Health care utilization in chronic obstructive pulmonary disease. A case-control study in a health maintenance organization. Arch Intern Med. 2000;160(17):2653–2658. doi: 10.1001/archinte.160.17.2653. [DOI] [PubMed] [Google Scholar]
- 15.Polsky D, Bonafede M, Suaya JA. Comorbidities as a driver of the excess costs of community-acquired pneumonia in U.S. commercially-insured working age adults. BMC Health Serv Res. 2012;12:379. doi: 10.1186/1472-6963-12-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. doi: 10.2147/COPD.S36997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Halpern MT, Zilberberg MD, Schmier JK, Lau EC, Shorr AF. Anemia, costs and mortality in chronic obstructive pulmonary disease. Cost Eff Resour Alloc. 2006;4:17. doi: 10.1186/1478-7547-4-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Celli BR, MacNee W, ATS/ERS Task Force Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23(6):932–946. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 19.Simoens S, Decramer M, De Coster S, Celis G, Laekeman G. Clinical and economic analysis of antimicrobial therapy of chronic obstructive pulmonary disease exacerbations. Int J Clin Pract. 2007;61(2):200–206. doi: 10.1111/j.1742-1241.2006.01240.x. [DOI] [PubMed] [Google Scholar]
- 20.O’Reilly JF, Williams AE, Rice L. Health status impairment and costs associated with COPD exacerbation managed in hospital. Int J Clin Pract. 2007;61(7):1112–1120. doi: 10.1111/j.1742-1241.2007.01424.x. [DOI] [PubMed] [Google Scholar]
- 21.Niederman MS, McCombs JS, Unger AN, Kumar A, Popovian R. Treatment cost of acute exacerbations of chronic bronchitis. Clin Ther. 1999;21(3):576–591. doi: 10.1016/S0149-2918(00)88310-1. [DOI] [PubMed] [Google Scholar]
- 22.Dalal AA, Shah M, D’Souza AO, Rane P. Costs of COPD exacerbations in the emergency department and inpatient setting. Respir Med. 2011;105(3):454–460. doi: 10.1016/j.rmed.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Perera PN, Armstrong EP, Sherrill DL, Skrepnek GH. Acute exacerbations of COPD in the United States: inpatient burden and predictors of costs and mortality. COPD. 2012;9(2):131–141. doi: 10.3109/15412555.2011.650239. [DOI] [PubMed] [Google Scholar]
- 24.Varol Y, Varol U, Başer Z, Usta L, Balcı G, Özacar R. The cost of COPD exacerbations managed in hospital. Turk Toraks Derg. 2013;14(1):19–23. [Google Scholar]
- 25.Bousquet J, Anto JM, Sterk PJ, et al. Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Med. 2011;3(7):43. doi: 10.1186/gm259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 27.Hidalgo CA, Blumm N, Barabasi AL, Christakis NA. A dynamic network approach for the study of human phenotypes. PLoS Comput Biol. 2009;5(4):e1000353. doi: 10.1371/journal.pcbi.1000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharafkhaneh A, Petersen N, Yu HJ, Dalal AA, Johnson ML, Hanania NA. Burden of COPD in a government health care system: a retrospective observational study using data from the US Veterans Affairs population. Int J Chron Obstruct Pulmon Dis. 2010;5:125–132. doi: 10.2147/copd.s8047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fumagalli G, Fabiani F, Forte S, et al. INDACO project: a pilot study on incidence of comorbidities in COPD patients referred to pneumology units. Multidiscip Respir Med. 2013;8(1):28. doi: 10.1186/2049-6958-8-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miyazaki M, Nakamura H, Chubachi S, et al. Analysis of comorbid factors that increase the COPD assessment test scores. Respir Res. 2014;15:13. doi: 10.1186/1465-9921-15-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halpin DM, Miravitlles M. Chronic obstructive pulmonary disease: the disease and its burden to society. Proc Am Thorac Soc. 2006;3(7):619–623. doi: 10.1513/pats.200603-093SS. [DOI] [PubMed] [Google Scholar]
- 32.Lin J, Li Y, Tian H, et al. Costs and health care resource utilization among chronic obstructive pulmonary disease patients with newly acquired pneumonia. Clinicoecon Outcomes Res. 2014;6:349–356. doi: 10.2147/CEOR.S65824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen YH, Yao WZ, Cai BQ, et al. Economic analysis in admitted patients with acute exacerbation of chronic obstructive pulmonary disease. Chin Med J. 2008;121(7):587–591. [PubMed] [Google Scholar]
- 34.Agusti A. Systemic effects of chronic obstructive pulmonary disease: what we know and what we don’t know (but should) Proc Am Thorac Soc. 2007;4(7):522–525. doi: 10.1513/pats.200701-004FM. [DOI] [PubMed] [Google Scholar]
- 35.Shaya FT, Lin PJ, Aljawadi MH, Scharf SM. Elevated economic burden in obstructive lung disease patients with concomitant sleep apnea syndrome. Sleep Breath. 2009;13(4):317–323. doi: 10.1007/s11325-009-0266-2. [DOI] [PubMed] [Google Scholar]
- 36.Stanford RH, Shen Y, McLaughlin T. Cost of chronic obstructive pulmonary disease in the emergency department and hospital. Treat Respir Med. 2006;5(5):343–349. doi: 10.2165/00151829-200605050-00005. [DOI] [PubMed] [Google Scholar]