Abstract
AIM
To evaluate the effect of punctal occlusion using thermosensitive (smart plug) versus silicone plug for management of aqueous deficient dry eye on corneal sensitivity, ocular surface health and tear film stability.
METHODS
A comparative prospective interventional case study included 45 patients with bilateral severe form of aqueous deficient dry eye. In each patient, the smart plug was inserted in the lower punctum of the right eye which was considered as study group 1 and silicone plug was inserted in the lower punctum of the left eye of the same patient which was considered as study group 2. All patients were subjected to careful history taking and questionnaire for subjective assessment of severity of symptoms. Corneal sensitivity, corneal fluorescein, rose bengal staining, Schirmer's I test, tear film break up time and conjunctival impression cytology were performed pre and 1, 3 and 6mo post plug insertion.
RESULTS
A statistically significant improvement in subjective and objective manifestations occurred following treatment with both types of plugs (P<0.01). The thermosensitive plug caused significant overall improvement, decrease in frequency of application of tear substitutes and improvement of conjunctival impression cytology parameters in the inserted side (P<0.01). Canaliculitis was reported in two eyes (4.4%) following punctal occlusion using thermosensitive plug (study group 1). Spontaneous plug loss occurred in 21 eyes (46.6%) in the silicone plug group (study group 2).
CONCLUSION
Improvement of subjective and objective manifestations of aqueous deficient dry eye occurs following punctal plug occlusion. Thermosensitive plug has good patient's compliance with fewer complications and lower rates of loss compared to the silicone plug.
Keywords: conjunctival impression cytology, corneal sensitivity, corneal fluorescein staining, dry eye syndrome, Schirmer's test, silicone plug, thermosensitive smart plug
INTRODUCTION
Dry eye syndrome is common, its prevalence around the world varies from 5% to 34%[1]. It is both a primary disease and a secondary result of many pathological states of the eye. The symptoms range from mild to severe itching, burning, irritation, eye fatigue, and even vision loss that can lead to disability[2]. Despite its high prevalence, it is frequently under recognized. Owing to its negative influence on patients' visual function and quality of life, dry eye represents a big burden in public healthcare[3]–[4].
It was traditionally thought to be a disease of age and more common in females. A younger population is the most rapidly growing segment of dry eye sufferers, likely in part to shifts in our lifestyles toward frequent computer and visual display tasking[2]. It is subdivided into two forms, aqueous-deficient (tear deficiency) and hyper-evaporative (increased evaporation)[5]–[6], however, mixed forms are common[7]. It is an inflammatory disease that has many features in common with autoimmune disease. Stress to the ocular surface (environmental factors, infection, endogenous stress, antigens, genetic factors) is postulated as the pathogenic triggering mechanism[8]–[9]. Better understanding of complex pathophysiology and underlying mechanisms of dry eye syndrome has led to development of numerous pharmacological and non-pharmacological treatment options for this disease[10]–[11]. The primary determinant for the therapeutic strategy of dry eye is the severity of the disease. Additionally, a stepwise guide to approach the best combination of medications to avoid symptoms was also recommended [4].
Punctal occlusion is a non-pharmacological therapy for dry eye symptoms insufficiently treated by other methods[6]. The method in common use is to occlude the punctum with silicone plugs of various sizes and designs[12]. Recognized complications of conventional silicone plugs force the development of new designs [13]. The intracanalicular smart plug (Medennium, Inc. Irvine, California, USA) made from a thermosensitive hydrophobic acrylic polymer has been in clinical use since 2002. The smart plug is solid at room temperature but becomes a soft gel at body temperature, thus fixating it in the canaliculus[14]–[15].
The aim of this study was to evaluate the effect of punctal occlusion using thermosensitive (smart plug) versus silicone plug for management of severe aqueous deficient type of dry eye on corneal sensitivity, ocular surface health and tear film stability. The patients included in the study were on maximally tolerable topical preservative free artificial tear supplements for more than 6mo prior to plug insertion.
SUBJECTS AND METHODS
Study Design
A comparative prospective interventional case study was conducted at Ophthalmology and Pathology Departments, Ain Shams University in the period from October 2009 to March 2013. The study included 90 eyes of 45 patients with aqueous deficient type of dry eye syndrome who were symptomatic despite maximally tolerable lubricant therapy. Right eye of each patient was treated with insertion of the thermosensitive acrylic hydrophobic plug (smart plug) in the lower punctum and considered as study group 1. The left eye of the same patient was treated by insertion of the silicone plug in the lower punctum and this was considered as study group 2.
Study inclusion criteria required the presence of subjective symptoms of dry eye, in addition to Schirmer's test of ≤5 mm/5min with topical anesthesia, a tear film break up time (TBUT) of ≤5s and evidence of ocular surface damage on either rose bengal or fluorescein staining. All patients had used frequent preservative free artificial tear supplements for 6mo without subjective or objective improvement.
Exclusion criteria included patients having blepharitis, eye lid deformity (triachiasis, entropion and ectropion), contact lens wearers, previous use of punctal plugs, proptosis and history of previous ophthalmic surgical procedures. Also patients who had nasolacrimal duct obstruction.
All patients participated in this study signed a written informed consent before the procedure. The study was approved by the Research Ethical Committee at Faculty of Medicine, Ain Shams University and all procedures conformed to the guidelines provided by World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Humans.
Clinical Examination and Tear Function Measures
Patients were assessed by careful history taking and ophthalmological examination for proper selection of cases prior to plug insertion and at 1, 3 and 6mo after plug insertion. At each visit, subjects were asked to complete the ocular surface disease index (OSDI), an established valid and reliable measure of patient's dry eye symptoms[16] before any clinical measures were made. The OSDI was developed by Allergan Pharmaceuticals (Irvine, CA, USA) to reliably assess overall and categorized patient dry eye symptoms. Scores range from 0 to 100 for the overall score and in each category. A score of 0 to 12 indicates a normal eye, 13 to 22 considered mild dry eye, 23 to 32 considered moderate dry eye, and over 33 indicates severe dry eye. It should be noted that a decrease in OSDI score indicates an improvement.
Objective clinical tests included corneal sensitivity measurement, assessment of tear production (Schirmer's I test with anesthesia), tear film stability (fluorescein TBUT), ocular surface health (fluorescein and rose bengal surface staining) were performed for both eyes. Ocular surface changes were evaluated on histological basis using conjunctival impression cytology.
Schirmer's I Test
Schirmer's I test was performed with anesthesia. Topical anesthetic; benoxinate hydrochloride ophthalmic solution 0.4% (E.I.P.I.C.O. Egyptian Int. Pharmaceutical Industries Co.) was administered to the conjunctiva and both lid margins, to obtain the anesthesia of all the ocular structures. Schirmer strips (Whatmann No.41 quality, 5 mm wide and 35 mm long) were placed on the lower lid 2 mm medial to the lateral canthus. Patients sat in the dark with both eyes closed for 5min. The strips were removed and a measurement (in millimeters) of the wet area of the strip was made[17].
Tear Film Break up Time
Fluorescein TBUT was determined following the procedure suggested by Lemp[18]. A fluorescein strip was dampened with a drop of non-preserved saline solution, and the strip was touched to the inferior palpebral conjunctiva. Patients were asked to blink several times to mix the fluorescein with the tear film. They were asked to open their eyes and not blink, and the time between the opening of the eyes and the appearance of the first dry spot was measured 3 times in seconds. The average of the 3 measurements was recorded as the final TBUT.
Ocular Surface Vital Staining
The corneal fluorescein stain was evaluated 3min after fluorescein instillation by observing the cornea through the slit lamp with a cobalt blue light[17]. Corneal staining was graded using a scale of 0 to 3; grade 0:<1/3 of corneal surface stained, grade 1: 1/3 of corneal surface stained, grade 2: >1/3 and ≤2/3 of corneal surface stained, grade 3: >2/3 of corneal surface stained.
Rose bengal vital staining was used to evaluate the health of the conjunctival epithelium. After all tests utilizing fluorescein, rose bengal staining was performed by using a rose bengal ophthalmic strip wetted with sterile benoxinate hydrochloride ophthalmic solution 0.4% and allowed to sit for 3min. The wetted strip was touched to the inferior bulbar conjunctiva while the patient looked up, and the lower lid was pulled away from the globe[19]–[20]. Care was taken by the examiner to instill adequate dye (both fluorescein and rose bengal) while attempting to minimize reflex tearing[21]. The conjunctival epithelium was assessed after patients were instructed to blink repeatedly to mix the rose bengal with the tear film[22]. Three fields are evaluated: the cornea, the nasal conjunctiva and the temporal conjunctiva; grade 0: no spots of stain, grade 1: up to 9 spots of stain, grade 2: 10 to 50 spots of stain, grade 3: >50 spots of stain.
Corneal Sensitivity
Corneal sensitivity measurements were performed pre-plug insertion, 3 and 6mo post-insertion using Cochet-Bonnet Aesthesiometer (Luneau; Western Ophthalmics, Lynnwood, WA, USA). Measurements were taken at five different areas within each cornea; the centre of the cornea and the four quadrants (superotemporal, superonasal, inferotemporal, and inferonasal). The stimulus from the Cochet-Bonnet consists of a nylon filament that can be varied in length from 0 to 6 cm. The procedure for measuring ocular surface sensitivity was according to Yen et al[23]
Conjunctival Impression Cytology
Conjunctival impression cytology was performed prior to plug insertion, 3 and 6mo post insertion. Specimens were obtained after application of topical anesthetic. Specimens were taken from the temporal bulbar conjunctiva just below the horizontal midline of the cornea, about 2 to 3 mm from the limbus of both eyes of each patient. Cellulose acetate filter sheets with 0.025 µm pores were cut into small triangular strips of about 5×5×7 mm, and applied to the bulbar conjunctiva dull side down. With a flat, round-tipped forceps, the strips were gently pressed onto the ocular surface for a few seconds, and removed with a peeling motion. With this method, one to two epithelial cell sheets can be harvested. The filter strips were put directly into clean glass bottle with a sufficient amount of 97% ethyl alcohol to cover it. The samples were then stained according to Tseng[24].
Microscopic Examination
This was carried out using a light microscope (ERMA model KD) with ×50 magnification to evaluate the overall relation of the cells and with ×250 magnification to study individual cells. Any slide that showed poor cell pickup was discarded as unreliable. The samples were then examined for the following cytological features: cohesion power, cell size, nuclear cytoplasmic ratio (N/C), distribution of goblet cells and degree of keratinization. Cohesion power was graded as follows: grade 1, one large sheet of coherent cells; grade 2, a group of cells; grade 3, separate individual cells (a half point was added to each grade to represent intermediate forms). Cell size was graded as follows: average size=0; enlarged=1; and shrunken=−1. N/C normally ranged from 1: 1 to 1: 2. Only the denominator was represented by N/C. Distribution of goblet cells on the conjunctival side (in 4 high power field) was as follows: present=1; absent=0. Degree of keratinization was as follows: grade 0=normal (deep staining of the cytoplasm); grade 1=mild (average staining of the cytoplasm); grade 2=moderate (pale cytoplasm); and grade 3=severe (very faint cytoplasm) (A half point was added to each grade to represent intermediate form). The overall grading system used was based on morphological appearance of conjunctival epithelial and goblet cells according to Nelson et al[25].
Thermosensitive (Smart Plug) Insertion (Study Group 1)
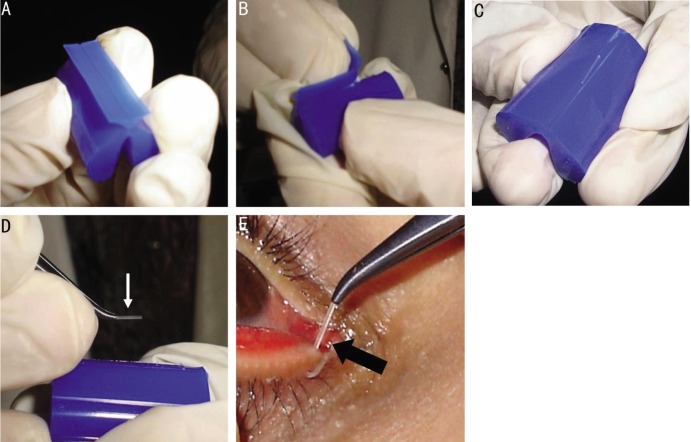
Smart plug (Medennium, Inc. Irvine, CA, USA) was packaged in a silicone carrier that prevented premature expansion due to elevated temperature (Figure 1A). Grasping the top and bottom of the carrier in a twisted action was done to separate the carrier and expose the smart plug (Figure 1B, 1C). Insertion of the smart plug was performed under topical anesthesia with aseptic condition. It was grasped with specifically designed grooved forceps covered with silicone sleeves in order to avoid any mechanical damage to the sensitive material (Medennium, Inc. Irvine, CA, USA) (Figure 1D). Measurement of the punctal size was not needed. It is rod shaped (0.4 wide and 12 mm long). The punctum was gently dilated using a lacrimal dilator. Upon exposure to body temperature, the plug spontaneously shortened to 1.5-2 mm, while the diameter simultaneously increased to well over 1 mm, so this ensures complete occlusion of the canaliculus (Figure 1E). After 20min, the material filled the ampulla of the lacrimal canaliculus completely.
Figure 1. Technique of handling of smart plug.
A: The plug is protected within a silicone carrier; B: Separation of the top of the carrier and the bottom part in a twisted action to expose the plug; C: The plug is in a groove inside its carrier; D: Grasping the smart plug rod by a special forceps (white arrow); E: The plug is inserted under topical anesthesia (black arrow).
Silicone Plug Insertion (Study Group 2)
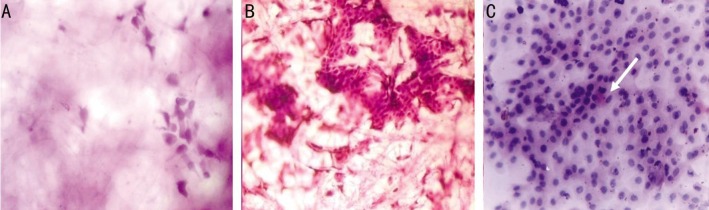
The insertion of the plug was performed under sterile conditions. A cotton wool tip soaked in topical anesthetic was directly applied onto the conjunctiva in the caruncular region. Eagle Flex plug (Eagle vision, Inc. Memphis, USA) has been used (Figure 2A). The Eagle Vision punctual systems were used to size the punctual opening ensuring a custom fit with maximal retention and patient comfort. Plug sizes are the same diameters as the gauge, with a slightly oversized nose for maximum plug retention. The dilator end of the inserter was gently inserted (this is a double-ended instrument with an additional lacrimal dilator) no more than 1-2 mm into the vertical canaliculus (Figure 2B). To insert the lacrimal plug, the instrument was hold as a pencil, between the thumb and the middle finger just above the release button. Using a gentle, downward rotation motion, the plug was inserted until the rim was flushed against the punctual opening. Once the plug was properly positioned, the release button on the inserter, was fully depressed and released and so the inserter pin had been withdrawn from the plug. The fit of the plug was assessed at the slit lamp, ensuring that the dome of the plug was flushed with the lid margin contour (Figure 2C). Patients were instructed not to rub or press the medial canthus and warned about persistent of irritation for several days.
Figure 2. Technique of handling of silicone plug.
A: Eagle Flex plug package (Eagle vision, Inc. Memphis, USA); B: The dilator end of the inserter is gently inserted no more than 1-2 mm into the vertical canaliculus; C: Proper position of the plug in the lower lacrimal punctum, the dome of the silicone plug (black arrow) is flushed with the lid margin contour.
Post Plug Insertion
Following both plug insertion, the patients were instructed to return in 2wk after placement and according to the follow up schedule later on. All patients used preservative free artificial tear eye drops for at least three times per day then the frequency of its use was adjusted according to the subjective and objective improvement of ocular surface integrity and gradual withdrawal of the lubricant drops was done.
Confirmation of the presence of the smart plug in place was detected by the persistent lower tear clearance rates and the absence of fluorescein dye back flow on lacrimal sac pressure throughout the follow-up period in all eyes. These signs suggested that the plugs were in place. Assessing the subjective and objective improvement of ocular surface integrity, the tear dynamic was done as mentioned before.
Statistical Analysis
Data were collected, statistically analyzed using the SPSS program version 13 for Windows (SPSS Inc., South Wacker Drive, Chicago, USA). Quantitative data were presented in mean and standard deviation. Qualitative data were presented in frequency and percentage. Comparison of qualitative data was done using Chi-square test while of quantitative data was done using paired t-test within one treatment group and unpaired t-test when comparison was performed between the two groups. P≤0.05 was considered as statistically significant.
RESULTS
This study included 27 (60.0%) females and 18 (40.0%) males. The mean age at diagnosis was 48.2±9.3y. History of rheumatoid arthritis was reported in 33 patients (73.3%). Silicone plug loss was reported in 6 (13.0%) and another 15 (33.0%) patients at 3, 6mo post plug insertion respectively, the remaining 24 (54.0%) patients in (group 2, silicone plug) who retaining the plugs, were statistically compared to (group 1, smart plug) who did not suffer any plug loss.
The mean sum of questionnaire score was initially 81.24±10.3 (range: 62.5-97.2) which decreased to 66.32±17.92 (range: 46.9-93.8) in study group 1 and 73.83±15.7 (range: 46.9-93.8) in group 2. A statistically significant improvement in symptoms and a reduction of mean (OSDI) score were reported in both groups, started 3mo following insertion and continued at 6mo of treatment (P<0.01 compared to baseline data). There was no statistically significant difference between both groups at each follow up period despite of more improvement in the mean score in study group 1 compared to study group 2 (P>0.05) (Table 1). Following plug insertion at the end of follow up in study group 1, the mean score decreased in 42 eyes (95.5%) and did not change in 3 eyes (4.5%). In study group 2, the mean score decreased in 9 eyes (37.5%), did not change in one eye (4.2%) and increased in 14 eyes (58.3%).
Table 1. Comparison between the thermosensitive (study group 1) and silicone plug (study group 2) as regards mean scoring for symptoms of dry eye, mean Schirmer's I test values and mean TBUT values pre and post plug insertion along the period of follow up.
| Parameters | Group 1 (range) | Group 2 (range) | P |
| Symptoms score (points) | |||
| Pre-plug insertion | 81.24±10.3 (62.5-97.2) | 81.24±10.3 (62.5-97.2) | 1.0 (NS) |
| 1mo | 81.24±10.3 (62.5-97.2) | 81.24±10.3 (62.5-97.2) | 1.0 (NS) |
| 3mo | 78.08±11.59 (62.5-97.2) | 80.41±11.2 ( 62.5-97.2) | 0.7 (NS) |
| 6mo | 66.32±17.92 (46.9-93.8) | 73.83±15.7 ( 46.9-93.8) | 0.08 (NS) |
| Schirmer's I test values (mm) | |||
| Pre-plug insertion | 3.4±0.7 (2.0-5.0) | 3.4±0.7 (2.0-5.0) | 1.0 (NS) |
| 1mo | 3.4±0.7 (2.0-5.0) | 3.4±0.7 (2.0-5.0) | 1.0 (NS) |
| 3mo | 3.4±0.7 (2.0-5.0) | 3.51±0.7 (2.0-5.0) | 0.2 (NS) |
| 6mo | 5.24±1.8 (2.0-8.0) | 4.25±1.22 (3.0-7.0) | 0.008 (SS) |
| TBUT values (s) | |||
| Pre-plug insertion | 3.4±0.9 (2.0-5.0) | 3.4±0.9 (2.0-5.0) | 1.0 (NS) |
| 1mo | 3.4±0.9 (2.0-5.0) | 3.4±0.9 (2.0-5.0) | 1.0 (NS) |
| 3mo | 6.62±1.96 (2.0-9.0) | 6.3±2.0 (2.0-9.0) | 0.1(NS) |
| 6mo | 12.08±5.1 (2.0-18.0) | 5.8±4.8 (2.0-17.0) | <0.001 (SS) |
SD: Standard deviation; NS: Statistically non significant; SS: Statistically significant.
x±s
Before punctal plug placement, the mean Schirmer's I test values were 3.4±0.7 mm (range: 2.0-5.0) and after plug occlusion, these values were 5.24±1.8 mm (range: 2.0-8.0) in study group 1 and 4.25±1.22 mm (range: 3.0-7.0) in study group 2. A statistically significant (P<0.01 compared to baseline data) increase in mean Schirmer's I test values was found in both groups. The increase in the mean values was greater in study group 1 than in study group 2 with a statistically significant increase in study group 1 compared to study group 2 (P value was 0.008) at 6mo of follow up (Table 1). Following plug insertion at the end of follow up in study group 1, the mean Schirmer's I test values improved in 26 eyes (57.7%) and did not change in 19 eyes (42.3%). In study group 2, improvement in mean values were observed in 5 eyes (20.8%) and did not change in 19 eyes (79.2%).
Before punctal plug placement, the mean TBUT was 3.4±0.9s (range: 2.0-5.0) and after plug occlusion, these value was 12.08±5.1s (range: 2.0-18.0) in study group 1 and 5.8±4.8s (range: 2.0-17.0) in study group 2. A statistically significant increase in mean TBUT was reported in both groups, started 3mo following insertion and continued at 6mo of treatment (P<0.01 compared to baseline data). The increase in the mean values was greater in study group 1 than in study group 2 with a statistically significant difference in group 1 compared to group 2 (P<0.01) at 6mo of follow up (Table 1). Following plug insertion at the end of follow up in study group 1, the mean TBUT improved in 40 eyes (88.8%) and did not change in 2 eyes (4.4%) and reduced in 3 eyes (6.7%). In study group 2, improvement in mean values were observed in 11 eyes (45.8%) and did not change in 6 eyes (25.0%) and reduced in 7 eyes (29.1%).
The pattern of corneal fluorescein staining showed a statistically significant (P<0.01 compared to baseline data) improvement started 3mo following insertion in both groups. Both groups show decrease in the area of cornea stained with fluorescein with a statistically significant difference between both groups at each time of follow up (P<0.01). The number of patients who showed <1/3 of the corneal surface stained by fluorescein had greatly increased in study group 1 than in study group 2 while the patients who showed severe staining (more than 2/3 of the cornea) did not show much improvement in both groups (Table 2). Following plug insertion at the end of follow up in study group 1, the staining reduced in 35 eyes (77.8%) and did not change in 10 eyes (22.2%). In study group 2, reduction were observed in 6 eyes (25.0%) and did not change in 18 eyes (75.0%).
Table 2. Comparison between the thermosensitive (study group 1) and silicone plug (study group 2) as regards grading of corneal fluorescein staining pre and post plug insertion along the period of follow up.
| Corneal fluorescein staining | Group 1 | Group 2 | P |
| Baseline (pre-plug insertion) | |||
| Grade 1 | 14.0 (31.1) | 14.0 (31.1) | 1.0 (NS) |
| Grade 2 | 21.0 (46.7) | 21.0 (46.7) | 1.0 (NS) |
| Grade 3 | 10.0 (22.2) | 10.0 (22.2) | 1.0 (NS) |
| 1mo post-insertion | |||
| Grade 1 | 14.0 (31.1) | 20.0 (44.4) | 0.01 (SS) |
| Grade 2 | 21.0 (46.7) | 15.0 (33.3) | 0.02 (SS) |
| Grade 3 | 10.0 (22.2) | 10.0 (22.2) | 1.0 (NS) |
| 3mo post-insertion | |||
| Grade 0 | 11.0 (24.4) | 3.0 (7.7) | <0.001 (SS) |
| Grade 1 | 4.0 (8.9) | 5.0 (12.8) | <0.001 (SS) |
| Grade 2 | 20.0 (44.5) | 21.0 (53.8) | 0.45 (NS) |
| Grade 3 | 10.0 (22.2) | 10.0 (25.7) | 0.01 (SS) |
| 6mo post-insertion | |||
| Grade 0 | 35.0 (77.8) | 6.0 (25.0) | <0.001 (SS) |
| Grade 1 | 0.0 | 1.0 (4.2) | <0.001 (SS) |
| Grade 2 | 0.0 | 9.0 (37.5) | <0.001 (SS) |
| Grade 3 | 10.0 (22.2) | 8.0 (33.3) | <0.001 (SS) |
NS: Statistically non significant; SS: Statistically significant.
n (%)
Regarding the reduction in rose bengal staining, a statistically significant improvement in grading was evident in study group 1 (P<0.01), however there was no statistically significant improvement in study group 2 between the pre-insertion grading and each period of follow up (P value was 0.08) with a statistically significant difference between the two groups started 3mo after treatment (P<0.01) (Table 3). At the end of follow up in study group 1, the staining reduced in 15 eyes (33.3%) and did not change in 30 eyes (66.7%). In study group 2, reduction was observed in 5 eyes (20.8%) and did not change in 19 eyes (79.2%).
Table 3. Comparison between the thermosensitive (study group 1) and silicone plug (study group 2) as regards grading of rose bengal staining pre and post plug insertion along the period of follow up.
| Rose bengal staining | Group 1 | Group 2 | P |
| Baseline (pre-plug insertion) | |||
| Grade 2 | 23.0 (51.1) | 23.0 (51.1) | 1.0 (NS) |
| Grade 3 | 22.0 (48.9) | 22.0 (48.9) | 1.0 (NS) |
| 1mo post-insertion | |||
| Grade 2 | 23.0 (51.1) | 23.0 (51.1) | 1.0 (NS) |
| Grade 3 | 22.0 (48.9) | 22.0 (48.9) | 1.0 (NS) |
| 3mo post-insertion | |||
| Grade 1 | 6.0 (13.3) | 9.0 (23.1) | 0.001 (SS) |
| Grade 2 | 18.0 (40.0) | 10.0 (25.6) | 0.002 (SS) |
| Grade 3 | 21.0 (46.7) | 20.0 (51.3) | 0.87 (NS) |
| 6mo post-insertion | |||
| Grade 1 | 15.0 (33.3) | 5.0 (20.8) | 0.004 (SS) |
| Grade 2 | 10.0 (22.2) | 3.0 (12.5) | <0.001 (SS) |
| Grade 3 | 20.0 (44.5) | 16.0 (66.7) | 0.1 (NS) |
NS: Statistically non significant; SS: Statistically significant.
n (%)
There was a statistically significant improvement in mean corneal sensitivity in all regions of the cornea in both groups after plug insertion compared to pre-insertion values (P<0.01). The improvement was statistically higher in study group 1 compared to study group 2 (P<0.01) at 3mo of follow up with no statistically significant difference was found at 6mo of follow up (Table 4).
Table 4. Comparison between the thermosensitive (study group 1) and silicone plug (study group 2) as regards mean corneal sensation pre and post plug insertion along the period of follow up.
| Parameters | Group 1 (range) | Group 2 (range) | P |
| Baseline (pre-plug insertion) | |||
| Corneal centre | 4.02±0.75 (3.0-5.0) | 4.06±0.72 (3.0-5.0) | 0.16 (NS) |
| ST quadrant | 3.71±0.99 (2.0-6.0) | 3.67±0.95 (2.0-6.0) | 0.42 (NS) |
| SN quadrant | 2.35±0.95 (1.0-4.0) | 2.44±0.94 (1.0-4.0) | 0.16 (NS) |
| IT quadrant | 2.31±1.10 (1.0-5.0) | 2.35±1.02 (1.0-5.0) | 0.53 (NS) |
| IN quadrant | 2.13±0.86 (1.0-4.0) | 2.20±0.84 (1.0-4.0) | 0.18 (NS) |
| 3mo post-insertion | |||
| Corneal centre | 4.93±0.80 (4.0-6.0) | 3.58±0.78 (2.0-5.0) | <0.001 (SS) |
| ST quadrant | 4.31±0.79 (3.0-6.0) | 3.89±0.97 (2.0-6.0) | <0.001 (SS) |
| SN quadrant | 3.28±0.84 (2.0-5.0) | 2.82±0.85 (1.0-4.0) | <0.001 (SS) |
| IT quadrant | 3.37±0.96 (1.0-5.0) | 2.94±0.99 (1.0-5.0) | <0.001 (SS) |
| IN quadrant | 3.11±1.00 (1.0-5.0) | 2.79±0.89 (1.0-4.0) | 0.004 (SS) |
| 6mo post-insertion | |||
| Corneal centre | 5.40±0.65 (4.0-6.0) | 5.75±0.44 (5.0-6.0) | 0.11 (NS) |
| ST quadrant | 5.31±0.63 (4.0-6.0) | 5.46±0.51 (5.0-6.0) | 0.32 (NS) |
| SN quadrant | 5.26±0.64 (4.0-6.0) | 5.37±0.65 (4.0-6.0) | 0.27 (NS) |
| IT quadrant | 5.28±0.69 (4.0-6.0) | 5.37±0.57 (4.0-6.0) | 0.66 (NS) |
| IN quadrant | 5.31±0.72 (4.0-6.0) | 5.42±0.65 (4.0-6.0) | 0.40 (NS) |
NS: Statistically non significant; SS: Statistically significant; ST: Superotemporal; SN: Superonasal; IT: Inferotemporal; IN: Inferonasal.
x±s, cm
There was a decrease in the dependence on the artificial tears in both groups. This was noticed from the 3 rd month of follow up (Table 5). A statistically significant decrease in frequency of application of artificial tears was noticed in both groups along the period of follow up and between both groups (P<0.01). Following plug insertion at the end of follow up in study group 1, the need for frequent application of artificial tear supplements decreased in 30 eyes (66.7%) and no change in frequency of artificial tear application was found in 15 eyes (33.3%). In study group 2, the frequency decreased in 3 eyes (12.5%), did not change in 10 eyes (41.6%) and increased in 11 eyes (45.8%).
Table 5. Comparison between the thermosensitive (study group 1) and silicone plug (study group 2) as regards frequency of artificial tear application pre and post plug insertion along the period of follow up.
| Parameters | Group 1 | Group 2 | P |
| Baseline (pre-plug insertion) | |||
| 4-6 times | 19.0 (42.2) | 19.0 (42.2) | 1.0 (NS) |
| >6 times | 26.0 (57.8) | 26.0 (57.8) | 1.0 (NS) |
| 1mo post-insertion | |||
| 4-6 times | 19.0 (42.2) | 19.0 (42.2) | 1.0 (NS) |
| >6 times | 26.0 (57.8) | 26.0 (57.8) | 1.0 (NS) |
| 3mo post-insertion | |||
| 1-3 times | 6.0 (13.3) | 0.0 | <0.001(SS) |
| 4-6 times | 20.0 (44.5) | 18.0 (46.2) | 0.45 (NS) |
| >6 times | 19.0 (42.2) | 21.0 (53.8) | 0.29 (NS) |
| 6mo post-insertion | |||
| 1-3 times | 11.0 (24.4) | 0.0 | 0.001 (SS) |
| 4-6 times | 19.0 (42.2) | 3.0 (12.5) | <0.001 (SS) |
| >6 times | 15.0 (33.4) | 21.0 (87.5) | <0.001 (SS) |
NS: Statistically non significant; SS: Statistically significant.
n (%)
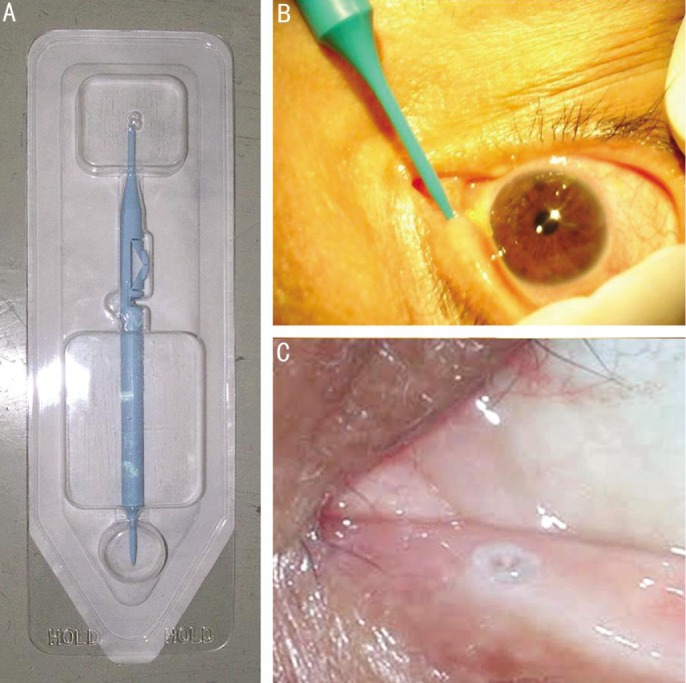
A statistically significant difference was found in conjunctival impression cytology features; cohesion power, cell size, goblet cell density, N/C and degree of keratinization started 6mo post insertion in both groups (P<0.01) from baseline data (Figure 3). There was a statistically significant improvement in cytological features in study group 1 compared to the study group 2 (Table 6).
Figure 3. Conjunctival impression cytology grading before and after plug insertion.
A: Grade 3 before plug insertion in which there is loss of goblet cells, N/C ratio is around 1:6, loss of cohesion of epithelial cells with marked enlargement of the size of epithelial cells with deeply stained cytoplasm; B: Grade 2 three months following punctal occlusion in which there are larger epithelial cells with N/C ratio is around 1:4-1:5 with marked reduction in goblet cell density; C: Grade 1 six months following punctal occlusion in which there is increased cohesion of cells, slightly larger epithelial cells with eosinophilic cytoplasm, N/C ratio is around 1:3, minimal in goblet cell density (white arrow) stained with Periodic acid schiff and Gill's modified papanicolau stain, microscopic magnification ×400.
Table 6. Comparison between the thermosensitive (study group 1) and silicone plug (study group 2) as regards microscopic features of conjunctival impression cytology before and after treatment.
| Grading | Group 1 |
Group 2 |
||||
| Baseline (n=45) | 3mo (n=45) | 6mo (n=45) | Baseline (n=45) | 3mo (n=39) | 6mo (n=24) | |
| Cohesion power | ||||||
| Grade 1 | 0.0 | 0.0 | 36.0 (80.0) | 0.0 | 0.0 | 7.0 (29.2) |
| Grade 2 | 35.0 (77.8) | 35.0 (77.8) | 0.0 | 35.0 (77.8) | 29.0 (74.4) | 9.0 (37.5) |
| Grade 3 | 10.0 (22.2) | 10.0 (22.2) | 9.0 (20.0) | 10.0 (22.2) | 10.0 (25.6) | 8.0 (33.3) |
| Cell size | ||||||
| -1 | 10.0 (22.2) | 10.0 (22.2) | 10.0 (22.2) | 10.0 (22.2) | 10.0 (25.6) | 8.0 (33.3) |
| 0 | 0.0 | 0.0 | 35.0 (77.8) | 0.0 | 0.0 | 5.0 (20.8) |
| 1 | 35.0 (77.8) | 35.0 (77.8) | 0.0 | 35.0 (77.8) | 29.0 (74.4) | 11.0 (45.9) |
| N/C ratio | ||||||
| 1:3 | 0.0 | 0.0 | 16.0 (35.6) | 0.0 | 0.0 | 3.0 (12.5) |
| 1:4 | 18.0 (40.0) | 18.0 (40.0) | 11.0 (24.4) | 18.0 (40.0) | 14.0 (35.9) | 6.0 (25.0) |
| 1:5 | 17.0 (37.8) | 17.0 (37.8) | 8.0 (17.8) | 17.0 (37.8) | 15.0 (38.5) | 7.0 (29.2) |
| 1:6 | 4.0 (8.9) | 4.0 (8.9) | 4.0 (8.9) | 4.0 (8.9) | 4.0 (10.3) | 2.0 (8.3) |
| 1:7 | 6.0 (13.3) | 6.0 (13.3) | 6.0 (13.3) | 6.0 (13.3) | 6.0 (15.3) | 6.0 (25.0) |
| Distribution of goblet cells (in 4 HPF) | ||||||
| Absent | 10.0 (22.2) | 10.0 (22.2) | 4.0 (8.9) | 10.0 (22.2) | 10.0 (25.6) | 8.0 (33.3) |
| Present | 35.0 (77.8) | 35.0 (77.8) | 41.0 (91.1) | 35.0 (77.8) | 29.0 (74.4) | 16.0 (66.7) |
| Degree of keratinization | ||||||
| Absent | 0.0 | 0.0 | 36.0 (80.0) | 0.0 | 0.0 | 7.0 (29.2) |
| Mild | 10.0 (22.2) | 10.0 (22.2) | 9.0 (20.0) | 10.0 (22.2) | 29.0 (74.4) | 0.0 |
| Moderate | 35.0 (77.8) | 35.0 (77.8) | 0.0 | 35.0 (77.8) | 10.0 (25.6) | 17.0 (70.8) |
| Overall conjunctival impression cytology grading | ||||||
| Grade 1 | 0.0 | 0.0 | 28.0 (62.2) | 0.0 | 0.0 | 14.0 (58.3) |
| Grade 2 | 28.0 (62.2) | 28.0 (62.2) | 0.0 (0.0) | 28.0 (62.2) | 22.0 (56.4) | 0.0 |
| Grade 3 | 17.0 (37.8) | 17.0 (37.8) | 17.0 (37.8) | 17.0 (37.8) | 17.0 (43.6) | 10.0 (41.7) |
HPF: High power field.
n (%)
Improvement of keratinization grading occurred in all eyes (100%) in study group 1. In study group 2, improvement of it occurred in 7 eyes (29.2%) with no change in grading in 8 eyes (33.3%) and worsening of it in 9 eyes (37.5%). Regarding goblet cell distribution in study group 1, specimens of 6 eyes (13.3%) showed appearance of goblet cells which was not present before plug occlusion with no change had occurred in specimens taken from study group 2.
There was a statistically significant difference (P=0.03) in both groups regarding the pre-insertion total grade of impression cytology and 6mo post-plug insertion, also there was a statistically significant difference (P=0.007) between both groups. The improvement was more observed in study group 1 more than study group 2 (Table 6). In study group 1, the overall conjunctival impression cytology grading was improved in 28 eyes (62.2%) and did not change in 17 eyes (37.8%). In study group 2, it was improved in 14 eyes (58.3%) and did not change in 10 eyes (41.7%).
The rate of spontaneous punctal plug loss in the silicone plug group (group 2) was: 6 eyes (13.0%) and another 15 eyes (33.0%) developed plug loss 3mo and 6mo respectively after insertion. Complications related to plug insertion were temporary foreign-body sensation which was experienced in all silicone-treated eyes. Two eyes (4.4%) in smart plug treated group (group 1) experienced canaliculitis developed 6mo post-insertion. Inflammation resolved completely with topical and systemic antibiotics.
DISCUSSION
Next to the medical therapy, blockage of the lacrimal drainage system is the most common form of treating dry eye. It helps to preserve any remaining natural tear fluid, which by far has the best wetting and nutrient capacity for the ocular surface[26]. Preserving natural tears by blocking the lacrimal drainage system can successfully maintain the integrity of the ocular surface, corneal transparency and visual acuity[3].
Punctal plugs are miniature medical implants that were initially developed for the treatment of moderate to severe dry eye syndrome. Since their introduction in 1975, many punctal plugs made from different materials and designs have been developed[27]. They are placed directly in the opening of the lacrimal punctum and extend into the lacrimal ampulla. In this position, they prevent the active and the passive drainage of the tear fluid[28]. Although insertion of punctal plugs is an effective therapy for treatment of dry eye syndrome, many complications are associated with their use. To overcome these issues intelligent designs of plugs were proposed[26].
The present study aimed to compare between two types of punctual plugs; one made of silicone and the other made of thermodynamic hydrophobic acrylic polymer (smart plug) for treatment of aqueous deficient dry eye syndrome as regards their effectiveness, tolerability and accompanied complications. The lower canaliculus was occluded because it is more accessible and it is also thought that most of the tear drainage is through the lower canaliculus[28].
Significant improvement in dry eye symptoms and ocular surface health occurred in both groups started 3mo following treatment. This was comparable to previous studies conducted on smart plug[14]–[15],[29], silicone plug[13],[30]–[32] or comparing the efficacy of both of them in management of dry eye[33]. Of 95.5% patients received smart plug had subjective improvements of symptoms compared to 37.5% following silicone plug insertion at the end of follow up. This was explained by several advantages of smart plug as stated by Chen and Lee[15] included that the smart plug material accommodates the canalicular anatomy, accurate punctal gauging is unnecessary before installation and there is no exposed portion to irritate the ocular surface, so the risk of spontaneous extrusion is reduced.
Significant improvements in mean Schirmer's I test values was reported 3mo after insertion of plugs. Kojima et al[14] inserted smart plug in 18 eyes of 10 dry eye patients who experienced problems with conventional punctal plugs. The plug was inserted in their study in both superior and inferior lacrimal punctal. They reported significant improvements in TBUT, fluorescein and rose bengal staining, Schirmer's I test and tear clearance tests 3mo after insertion with no statistical differences between pre-and post-treatment Schirmer test values. They assumed this result to that the smart plug might not block completely lacrimal canaliculi and it does not have disk shaped head that sit on the surface of punctal opening. Burgess et al[33] reported an increase in mean Schirmer score following insertion of both silicone and smart plugs although neither achieved statistical significance.
Sakamoto et al[13] reported that the mean Schirmer value did not increase significantly after two types of silicone plugs inserted for patients with or without Sjogren syndrome. Yen et al[23] showed a decrease in Schirmer test scores in healthy subjects after silicone plug occlusion. The decrease is believed to result from excessive negative feedback from the ocular surface, alterations of the tear drainage apparatus, or decreased lacrimal gland tear secretion after punctal occlusion.
In patients with dry eye, the thickness and the composition of the tear film are disturbed. Therefore, the possibility that the altered tear film changes the final intensity of the stimulus reaching the corneal nerve endings must be considered. In the case of mechanical stimuli, the normal tear film is expected to act as a limited filter for mechanical forces. Decreases in its thickness and/or elastoviscosity would at best reduce this filtering effect, enhancing the transmission of force to the nerve endings so that the same stimulus would be more intensely felt in dry eyes. Despite this, in patients with dry eye, mechanical sensitivity was significantly lower[34]. Hyposecretion of tears in dry eye may lead to pathologic changes in corneal epithelium and a decline in corneal sensitivity[35]–[36].
Mean corneal sensitivity study after punctal plug occlusion for treatment of dry eye was not previously reported. In the present study the mean corneal sensitivity significantly improved in both groups 3mo following treatment compared to pre-plug insertion.
Both silicone and smart plug treated eyes showed significant reduction in mean artificial tear drop use over the course of study however more significant reduction in dependency on the artificial tears in the smart plug group (66.7%) compared to silicone plug (12.5%). No one of our eyes in both groups completely stopped topical treatment.
Burgess et al[33] found that the overall use of tear supplements was decreased in 55.6% silicone and 61.1% smart plug treated eyes. At least one type of tear supplement was stopped in 38.8% silicone and 33.3% smart plug-treated eyes. Topical treatment was stopped in one 5.5% eye in each group. According to Chen and Lee[15] 60.4% reported a decreased use of lubricant eye drops after smart plug insertion including 15.4% who were free of supplementary lubricant eye drops after a mean 13.0mo of follow-up.
The effects of punctal occlusion on ocular surface have not studied well on a histological basis. There are few reports about ocular surface-punctal plug interactions in patients with dry eye syndrome[37]–[39].
Conjunctival impression cytology was used to investigate ocular surface changes following punctal occlusion. A statistically significant improvement in conjunctival impression cytology features; cohesion power, cell size, goblet cell density, N/C and degree of keratinization started 6mo post insertion in both groups compared to base line features. More significant improvement in ocular surface changes was found in the smart plug group compared to silicone group. Improvement of the degree of keratinization occurred in all smart plug treated eyes 100% versus 29 % in silicone plug treated eyes. Of 13.3% smart plug treated eyes show appearance of goblet cells which was not present before plug occlusion. Punctal plug occlusion provides improvement in tear film stability, ocular surface staining scores, conjunctival squamous metaplasia and goblet cell density in the present study which was comparable to Guzey et al[37], Dursun et al[38] and Li et al[39]. Increased ocular surface exposure to essential tear components with punctal occlusion may be important for the genesis of these changes.
Although punctal occlusion is an effective therapy for severe dry eye, there are complications related to punctal plug insertions[40]–[41]. Frequent spontaneous loss of silicone plugs has been reported. In the present study 46.6% of silicone plugs were spontaneously lost. The retention rates for the different kind of the plugs have been reported to be about 50% after 1y[14],[29],[32],[41], on the other hand, silicone plug is easily removed when causing discomfort or irritation[31],[42].
Different mechanisms explaining extrusion of plugs has been reported, including inadequate plug sizing, lid laxity in elderly, excessive dilation of the punctum with rupture of punctal ring, or spontaneous dissection of canalicular mucosa[41]. The intracanalicular position contributes to the lower rate of extrusion of smart plug. There is one previous case report of incomplete extrusion of smart plug at 1mo after plug insertion[43]. The extrusion rate of the smart plug is still not clear and should be investigated in further trials[14],[32].
In the US open-label trial by Medennium, 120 subjects were enrolled in a prospective, comparative study over a 90-day period. There were no reports of canaliculitis or dacryocystitis observed in that study. Kojima et al[14] reported no complications over 3mo after smart plug insertion.
Pyogenic granuloma formation[44] canaliculitis, dacryocystitis and epiphora[45] have been described after smart plug placement. Hill et al[46] found the prevalence of canaliculitis per patient was 7.23% and the prevalence of canaliculitis per smart plug inserted was 4.73%. The average time from smart plugs insertion to onset of symptoms was 3y. All affected patients required canaliculotomy and plug removal.
Klein-Theyer et al[47] reported the prevalence of canaliculitis per smart plug to be 16.6%. The median time from smart plug insertion to the onset of canaliculitis was 4.7y. They concluded that only long-term follow-up periods, such as those up to 10.5y as used in their study, can identify the majority of complications associated with smart plugs. Treatment of canaliculitis due to a lodged plug is ranging from simple topical/oral antibiotics to irrigation, retrograde plug expression, canaliculotomy or even dacryocystorhinostomy. Partial patency after smart plug insertion represents a site of entry for pathogens and constitutes at least one of the potential reasons for the high prevalence of canaliculitis[14]. The risk of canaliculitis might also be increased if the plug is inserted too deeply in the canaliculus or has migrated due to the formation of a sump, as assumed by Chen and Lee[15].
In conclusion improvement of subjective and objective manifestations of severe forms of aqueous deficient dry eye occurred after punctal occlusion by the thermosensitive and silicone plugs. The thermosensitive plug is more effective in its effects on corneal sensation, ocular surface health and tears film stability. It also has good patient's compliance with fewer complications and lower rates of loss compared to the silicone plugs.
Acknowledgments
Conflicts of Interest: Said AMA, None; Farag ME, None; Abdulla TM, None; Ziko OAO, None; Osman WM, None.
REFERENCES
- 1.Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int. 2015;112(5):71–82. doi: 10.3238/arztebl.2015.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vickers LA, Gupta PK. The future of dry eye treatment: a glance into the therapeutic pipeline. Ophthalmol Ther. 2015;4(2):69–78. doi: 10.1007/s40123-015-0038-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schaumberg DA, Dana R, Buring, Sullivan DA. Prevalence of dry eye disease among US men: estimates from the physicians' health studies. Arch Ophthalmol. 2009;127(6):763–768. doi: 10.1001/archophthalmol.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin H, Yiu SC. Dry eye disease: a review of diagnostic approaches and treatments. Saudi J Ophthalmol. 2014;28(3):173–181. doi: 10.1016/j.sjopt.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sy A, O'Brien KS, Liu MP, Cuddapah PA, Acharya NR, Lietman TM, Rose-Nussbaumer J. Expert opinion in the management of aqueous deficient dry eye disease (DED) BMC Ophthalmol. 2015;15:133. doi: 10.1186/s12886-015-0122-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chi SL, Acquah KF, Richard MJ, Lee PP, Sloan FA. Longitudinal evidence on punctal plug use in an elderly population. Ophthal Plast Reconstr Surg. 2012;28(4):289–293. doi: 10.1097/IOP.0b013e31825ca599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472–478. doi: 10.1097/ICO.0b013e318225415a. [DOI] [PubMed] [Google Scholar]
- 8.Stern ME, Schaumburg CS, Pflugfelder SC. Dry eye as a mucosal autoimmune disease. Int Rev Immunol. 2013;32(1):19–41. doi: 10.3109/08830185.2012.748052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stevenson W, Chauhan SK, Dana R. Dry eye disease: an immune-mediated ocular surface disorder. Arch Ophthalmol. 2012;130(1):90–100. doi: 10.1001/archophthalmol.2011.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yao W, Davidson RS, Durairai VD, Gelston CD. Dry eye syndrome: an update in office management. Am J Med. 2011;124(11):1016–1018. doi: 10.1016/j.amjmed.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 11.Dogru M, Tsubota K. Pharmacotherapy of dry eye. Expert Opin Pharmacother. 2011;12(3):325–334. doi: 10.1517/14656566.2010.518612. [DOI] [PubMed] [Google Scholar]
- 12.Murube J, Murube E. Treatment of dry eye by blocking the lacrimal canaliculi. Surv Ophthalmol. 1996;40(6):463–480. doi: 10.1016/s0039-6257(96)82013-3. [DOI] [PubMed] [Google Scholar]
- 13.Sakamoto A, Kitagawa K, Tatami A. Efficacy and retention rate of two types of silicone punctal plugs in patients with and without Sjogren syndrome. Cornea. 2004;23(3):249–254. doi: 10.1097/00003226-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Kojima T, Dogru M, Ishida R, Goto E, Matsumoto Y, Tsubota K. Clinical evaluation of the smart plug in the treatment of dry eyes. Am J Ophthalmol. 2006;141(2):386–388. doi: 10.1016/j.ajo.2005.08.032. [DOI] [PubMed] [Google Scholar]
- 15.Chen S, Lee G. SmartPlug in the management of severe dry eye syndrome. Cornea. 2007;26(5):534–538. doi: 10.1097/ICO.0b013e318038d2cd. [DOI] [PubMed] [Google Scholar]
- 16.Schiffman RM, Christianson MD, Jacobsen G, Hirsch JD, Reis BL. Reliability and validity of the ocular surface disease index. Arch Ophthalmol. 2000;118(5):615–621. doi: 10.1001/archopht.118.5.615. [DOI] [PubMed] [Google Scholar]
- 17.Aragona P, Cannavo SP, Borgia F, Guarneri F. Utility of studying the ocular surface study in patients with acne vulgaris treated with oral isotretinoin: a randomized controlled trial. Br J Dermatol. 2005;152(3):576–578. doi: 10.1111/j.1365-2133.2005.06389.x. [DOI] [PubMed] [Google Scholar]
- 18.Lemp MA. Report of the National Eye Institute/Industry workshop on clinical trials in dry eye. CLAO J. 1995;21(4):221–232. [PubMed] [Google Scholar]
- 19.Nichols KK, Nichols JJ, Lynn Mitchell G. The relation between tear film tests in patients with dry eye disease. Ophthalmic Physiol Opt. 2003;23(6):553–560. doi: 10.1046/j.1475-1313.2003.00153.x. [DOI] [PubMed] [Google Scholar]
- 20.Eliason JA, Maurice DM. Staining of the conjunctiva and conjunctival tear film. Br J Ophthalmol. 1990;74(9):519–522. doi: 10.1136/bjo.74.9.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea. 2004;23(3):272–285. doi: 10.1097/00003226-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22(7):640–650. doi: 10.1097/00003226-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Yen MT, Pflugfelder SC, Feuer WJ. The effect of punctal occlusion on tear production, tear clearance and ocular surface sensation in normal subjects. Am J Ophthalmol. 2001;131(3):314–323. doi: 10.1016/s0002-9394(00)00822-9. [DOI] [PubMed] [Google Scholar]
- 24.Tseng SC. Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology. 1985;92(6):728–733. doi: 10.1016/s0161-6420(85)33967-2. [DOI] [PubMed] [Google Scholar]
- 25.Nelson JD, Havener VR, Cameron JD. Cellulose acetate impressions of the ocular surface. Dry eye states. Arch Ophthalmol. 1983;101(12):1869–1872. doi: 10.1001/archopht.1983.01040020871007. [DOI] [PubMed] [Google Scholar]
- 26.Yellepeddi VK, Sheshala R, McMillan H, Gujral C, Jones D, Raghu Raj Singh T. Punctal plug: a medical device to treat dry eye syndrome and for sustained drug delivery to the eye. Drug Discov Today. 2015;20(7):884–889. doi: 10.1016/j.drudis.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 27.Miller KL, Walt JG, Mink DR, Satram-Hoang S, Wilson SE, Perry HD, Asbell PA, Pflugfelder SC. Minimal clinical important difference for the ocular surface disease index. Arch Ophthalmol. 2010;128(1):94–101. doi: 10.1001/archophthalmol.2009.356. [DOI] [PubMed] [Google Scholar]
- 28.Ogut MS, Bavbek T, Kazokoglu H. Assessment of tear drainage by fluorescein dye disappearance test after experimental canalicular obstruction. Acta Ophthalmol. 1993;71(1):69–72. doi: 10.1111/j.1755-3768.1993.tb04963.x. [DOI] [PubMed] [Google Scholar]
- 29.Guo L, Wu XY, Yuan F, Li B. Application of smart plug lacrimal plug in the treatment of dry eye. Nan Fang Yi Ke Da Xue Xue Bao. 2010;30(10):2370–2372. [PubMed] [Google Scholar]
- 30.Tai MC, Cosar CB, Cohen EJ, Ropauno CJ, Laibson PR. The clinical efficacy of silicone punctal plug therapy. Cornea. 2002;21(2):135–139. doi: 10.1097/00003226-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Balaram M, Schaumberg DA, Dana MR. Efficacy and tolerability outcomes after punctal occlusion with silicone plugs in dry eye syndrome. Am J Ophthalmol. 2001;131(1):30–36. doi: 10.1016/s0002-9394(00)00620-6. [DOI] [PubMed] [Google Scholar]
- 32.Nava-Castaneda A, Tovilla-Canales JL, Rodriguez L, Tovilla Y Pomar JL, Jones CE. Effects of lacrimal occlusion with collagen and silicone plugs on patients with conjunctivitis associated with dry eye. Cornea. 2003;22(1):10–14. doi: 10.1097/00003226-200301000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Burgess PI, Koay P, Clark P. Smart plug versus silicone punctal plug therapy for dry eye: a prospective randomized trial. Cornea. 2008;27(4):391–394. doi: 10.1097/ICO.0b013e318160d030. [DOI] [PubMed] [Google Scholar]
- 34.Bourcier T, Acosta MC, Borderie V, Borras F, Gallar J, Bury T, Laroche L, Belmonte C. Decreased corneal sensitivity in patients with dry eye. Invest Ophthalmol Vis Sci. 2005;46(7):2341–2345. doi: 10.1167/iovs.04-1426. [DOI] [PubMed] [Google Scholar]
- 35.Xu KP, Yagi Y, Tsubota K. Decrease in corneal sensitivity and change in tear function in dry eye. Cornea. 1996;15(3):235–239. doi: 10.1097/00003226-199605000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Adatia FA, Michaeli-Cohen A, Naor J, Caffery B, Bookman A, Slomovic A. Correlation between corneal sensitivity, subjective dry eye symptoms and corneal staining in Sjogren's syndrome. Can J Ophthalmol. 2004;39(7):767–771. doi: 10.1016/s0008-4182(04)80071-1. [DOI] [PubMed] [Google Scholar]
- 37.Guzey M, Ozardali I, Kilic A, Basar E, Dogan Z, Satici A, Karadede S. The treatment of severe trachomatous dry eye with canalicular silicone plugs. Eye (Lond) 2001;15(Pt 3):297–303. doi: 10.1038/eye.2001.98. [DOI] [PubMed] [Google Scholar]
- 38.Dursun D, Ertan A, Bilezikçi B, Akova YA, Pelit A. Ocular surface changes in keratoconjunctivitis sicca with silicone punctum plug occlusion. Curr Eye Res. 2003;26(5):263–269. doi: 10.1076/ceyr.26.4.263.15431. [DOI] [PubMed] [Google Scholar]
- 39.Li XM, Zhang J, Wang W. Application of lacrimal plug for dry eye patients. Zhonghua Yan Ke Za Zhi. 2005;41(12):1098–1102. [PubMed] [Google Scholar]
- 40.Paparizo SC, Edward DP, Osmanovic S. Plug surface defects as a late complication of silicone punctal plugs. Cornea. 2013;32(9):1224–1226. doi: 10.1097/ICO.0b013e31829a6881. [DOI] [PubMed] [Google Scholar]
- 41.Kaido M, Ishida R, Dogru M, Tsubota K. Comparison of retention rates and complications of 2 different types of silicone lacrimal punctal plugs in the treatment of dry eye disease. Am J Ophthalmol. 2013;155(4):648–653. doi: 10.1016/j.ajo.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 42.Bukhari AA. Botulinum neurotoxin type A versus punctal plug insertion in the management of dry eye disease. Oman J Ophthalmol. 2014;7(2):61–65. doi: 10.4103/0974-620X.137142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fasce F, Francato R. Incomplete extrusion of an acrylic punctum plug in a case of severe dry eye syndrome. Eur J Ophthalmol. 2005;15(1):132–134. doi: 10.1177/112067210501500122. [DOI] [PubMed] [Google Scholar]
- 44.Chou TY, Perry HD, Donnenfeld ED, Solomon R. Pyogenic granuloma formation following placement of the Medennium SmartPLUG punctum plug. Cornea. 2006;25(4):493–495. doi: 10.1097/01.ico.0000183489.78012.7a. [DOI] [PubMed] [Google Scholar]
- 45.SmartPlug Study Group Management of complications after insertion of the smart plug punctal plug: a study of 28 patients. Ophthalmology. 2006;113(10):1859. e1–6. doi: 10.1016/j.ophtha.2006.05.032. [DOI] [PubMed] [Google Scholar]
- 46.Hill RH, 3rd, Norton SW, Bersani TA. Prevalence of canaliculitis requiring removal of smart plugs. Ophthal Plast Reconstr Surg. 2009;25(6):437–439. doi: 10.1097/IOP.0b013e3181b80d63. [DOI] [PubMed] [Google Scholar]
- 47.Klein-Theyer A, Boldin I, Rabensteiner DF, Aminfar H, Horwath-Winter J. Prevalence of canaliculitis after smartplug insertion during long term follow-up. Br J Ophthalmol. 2015;99(8):1134–1136. doi: 10.1136/bjophthalmol-2014-306290. [DOI] [PubMed] [Google Scholar]