Abstract
AIM
To determine the main visual symptoms in a Brazilian population sample, associated to refractive errors (REs) and spectacle need to suggest priorities in preventive programs.
METHODS
A cross-sectional study was conducted in nine counties of the southeast region of Brazil, using a systematic sampling of households, between March 2004 and July 2005. The population was defined as individuals aged between 1 and 96y, inhabitants of 3600 residences to be evaluated and 3012 households were included, corresponding to 8010 subjects considered for participation in the survey, of whom 7654 underwent ophthalmic examinations. The individuals were evaluated according their demographic data, eye complaints and eye examination including the RE and the need to prescribe spectacles according to age. Statistical analysis was performed using SPSS software package and descriptive analysis using 95% confidence intervals (P<0.05).
RESULTS
The main symptom detected was asthenopia, most frequent in the 2nd and 3rd decades of life, with a significant decline after the 4th decade. Astigmatism was the RE most associated with asthenopia. Reduced near vision sight was more frequent in those ≥40y with a progressive decline thereafter. Spectacles were most frequently required in subjects of ≥40 years of age.
CONCLUSION
The main symptom related to the vision was asthenopia and was associated to astigmatism. The greatest need for spectacles prescription occurred after 40's, mainly to correct near vision. Subjects of ≥40 years old were determined to be at high risk of uncorrected REs. These observations can guide intervention programs for the Brazilian population.
Keywords: population study, visual symptoms, refractive error, spectacle need
INTRODUCTION
Visual symptoms are related to the individual's age and depend on the studied population. Asthenopia is the most frequent complaints in urban children, most likely due to school activities and referred as a large number of symptoms as blurred vision, difficulty in focusing at different distances, ocular pain or discomfort, brow ache, photophobia, watery, burning or itching eyes, dry eye sensation, double vision, headache on prolonged use of eyes that got relieved with the correction of refractive errors (REs)[1]–[2].
Ocular symptoms are subjective and do not always reflect the most important eye problem that the individual has, hence the importance of a complete eye examination to determine causes related to the complaint. Investigating elderly subjects indicated a high frequency of presbyopia (92.5%) and cataract (85.6%). However, the complaints of the participants were ocular hyperemia and more related to dry eye than to the detected visual condition[3].
Dry eye symptoms are associated to many other eye conditions as REs and can be related to disruptions in daily function, ocular discomfort or pain, have shown an association with vision and quality of life with an inverse association with the physical and mental component[4].
Nearly half of who have normal visual acuity (VA) complained about their quality of vision, and 25% believed that their vision is not good; on the other hand, 32% of the individuals with poor vision believe they had normal vision and 13% consider themselves to have good vision[5]. These disparities show that the assessments made by means of VA charts do not include all the factors that influence individual vision.
However, glasses prescription can only solve some of the visual symptoms in the REs carriers. In Africa, REs were identified in just 6.4% of the population between 15 and 50 years of age. Of these, only 22% had spectacles prescription; presbyopia was identified in over 32% of the sample, but very few were spectacle wearers, although almost 95% of these individuals could have benefitted from them[6]. Therefore, uncorrected REs remain the leading cause of visual impairment (VI) worldwide, and by far, spectacles remain the most common and cost-effective intervention for those REs and for presbyopia[7].
Population surveys involving systematic and randomized sampling to investigate visual problems have been rare in Brazil[8] and they are very important because could be used to the development of blindness prevention programs.
The present study was done with the goal of establishing the distribution of visual complaints present in a Brazilian sample, the association of those with REs and the need for spectacles.
SUBJECTS AND METHODS
A population-based cross-sectional ophthalmic survey of households was conducted in the southeast region of Brazil. The eligible population consisted of permanent, non-institutionalized residents, between March 2004 and July 2005. The exclusion criteria included prior cataract or refractive surgery. The study protocol was reviewed and approved by the Institutional Review Board of the Botucatu Medical School, Sao Paulo State, Brazil and the study was conducted in accordance with the tenets of the Declaration of Helsinki. Informed written consent was obtained in the presence of other family members, and each individual was free to decide whether to participate in the study. All examinations were carried out using a mobile eye unit. The participants were selected using a random, stratified, household cluster sampling technique. The selection of households to be evaluated was done systematically according to local census data: the first house was selected randomly; the next house was the sixth house on the even numbered side of the street and so on, successively. The randomly selected household received a letter of invitation to participate in the study and those who agreed to participate were contacted by telephone to schedule an appointment. All persons of the household were eligible to participate in the study. If there was no answer when the examiners contacted the household or if people refused to participate in the research, the first house to the right side was selected. If the next household refused to participate, the first house to the left side of the initial house was selected, and so on, successively. All study personnel underwent training as well all procedures were standardized prior to commencement. A single survey team composed by six ophthalmologists, two technicians and trained eye health care workers pointed by the municipality which conducted the study to filled out a detailed questionnaire investigating identification data (sex, ethnicity referred, age), on wearing and availability of glasses, family history of eye diseases or presence of any eye abnormalities and complains related to vision, considering near or far vision acuity reduced, asthenopia complaints such as lack of interest or loss of lines for reading, red eye, eye pain or headache after visual effort. Ocular symptoms were surveyed directly with the subjects and in the small children, with those in charge. Specific qualitative observations were performed by one or two members of the team in order to minimize inter-observer variability. Each participant then received a vision and eye examination. The first procedure was evaluation of presenting VA in the right eye followed by the left with a tumbling E Snellen chart. The VA was then retested with the spectacles in use when it exists. Autorefraction (Topcon KR-7000, Tokyo, Japan) was performed for all subjects over 3 years old independent of the VA. Objective refraction testing of children ≤3 years of age was performed using retinoscopy. Subjective refraction was performed only for those with VA worse than Snellen 6/12. For individual ≤40 years of age the refractive examination was performed under cycloplegia, obtained using two drops of cyclopentolate 1% in each eye with the refractive examination performed 30min after instillation of the drops. Only the objective refraction under cyclopegia (when necessary) was considered for the RE definitions and also for the best corrected visual acuity (BCVA) record. Slit lamp biomicroscopy (Shin Nippon SL101, http://www.shin-nippon.jp) and fundus examination (at the slit lamp using 90 D Volk lens under mydriasis-tropicamide 1%, 3 drops in those who had not received instillation of cyclopentolate eye drops) were performed. Intraocular pressure was evaluated with a non-contact tonometer (Canon TX-F, http://www.canon-europe.com/Medical/Eye_Care/TX-F/) and if intraocular pressure was higher than 21 mm Hg, the measurement was repeated using a Goldman tonometer.
Definitions for the Study
The symptoms were categorized into three segments: asthenopia (all symptoms related to eye strain as eye pain, headache, redness, burning to read were included), poor near sighted VA (referring inability to read usual books, newspaper and magazines) and poor far sighted VA (inability to read or recognize objects further than six meters). VI was considered when VA was worse than Snellen 6/18 (WHO definition). We adopted the definitions of RE from the Baltimore Eye Study[9] as follows: myopia was defined as an spherical equivalent (SE) ≤-0.5 D, high myopia as ≤-3.0 D, hyperopia as an SE≥+0.5 D, high hyperopia as ≥+3.0 D and astigmatism as a DC≤-0.5 D. Anisometropia was defined as a difference in the SE between the right and left eyes of ≥1.0 D.
The treatments considered for RE were no need of spectacles prescription, optical correction with improvement of the VA, VI despite adequate optical correction, and blindness even with spectacles.
Statistical Analysis
There was a high correlation between the right and left eye RE data (Spearman R=0.88). The analysis of the right eye RE and the demographic associations produced similar results to those in persons in whom the left eye RE was associated with demographic variables; hence, the results from the better eye were reported. The statistical software package used was SPSS version 15.0 (SPSS for Windows Inc., Chicago, IL, USA).
A descriptive analysis was performed using the mean, median and respective measures of dispersion (standard deviation and interquartile range). The proportion and prevalence data are presented in graphs, using 95% confidence intervals (CIs) and P values (significant at the P<0.05 level).
RESULTS
A total of 3012 households were included in the study, and 8010 subjects were considered for participation in the survey, of whom 7654 underwent ophthalmic examinations. Near 5% were not included in the sample and the primary reasons for non-participation were work commitments, not meeting the inclusion criteria, or refusal to participate. The municipalities were homogeneous for their frequency of participation, ranging from 9.0% to 13.3%. Of the study participants, 62.73% were female, 92.1% considered themselves to be white and 6.5% black. The mean age of the participants was 36.9±21.1y, ranging from 1 to 96 years old. The frequency of participation was higher in the 2nd and 5th decade of life, with 15.48% and 17.13% of participation, respectively, with participation falling progressively in the oldest groups (Table 1). The predominance of females was evident in all the age groups, reaching nearly 50% in the 3rd and 4th age groups (Table 1).
Table 1. Distribution and frequency of the studied population according to gender and age.
| Age (a) | Male | Female | Total |
| 1 to 9 | 422 (5.51) | 457 (5.97) | 879 (11.48) |
| 10 to 19 | 471 (6.15) | 714 (9.33) | 1185 (15.48) |
| 20 to 29 | 284 (3.71) | 696 (9.09) | 980 (12.80) |
| 30 to 39 | 278 (3.63) | 706 (9.22) | 984 (12.85) |
| 40 to 49 | 473 (6.18) | 838 (10.95) | 1311 (17.13) |
| 50 to 59 | 424 (5.54) | 651 (8.51) | 1075 (14.05) |
| 60 to 69 | 286 (3.74) | 439 (5.74) | 725 (9.48) |
| 70 + | 215 (2.81) | 300 (3.92) | 515 (6.73) |
| Total | 2853 (37.27) | 4801 (62.73) | 7654 (100) |
n (%)
According to VI distribution, 13.82% were considered VI at the first exam without RE correction and reducing to 7.32% when considering with the best RE correction. Instead the adequate RE correction, 2.31% remained as blind condition.
The main ocular symptom was asthenopia, present in 59.6% (95%CI: 58.5-60.7) of the participants, followed by poor near sighted VA, reported by 39.6% (95%CI: 38.5-40.7), and poor far sighted VA, found in 23.8% (95%CI: 22.8-24.8) of the subjects.
Considering the frequency of symptoms by gender, asthenopia was mentioned by 61.8% (95%CI: 60.5-63.2) of female and by 55.8% (95%CI: 54-57.7) of male, poor far sighted VA by 25.3% (95%CI: 24.1-26.6) of female and 21.2% (95%CI: 19.7-22.2) of male and poor near sighted VA by 39% (95%CI: 37.6-40.4) of female and 40.7% of male (95%CI: 38.9-42.5).
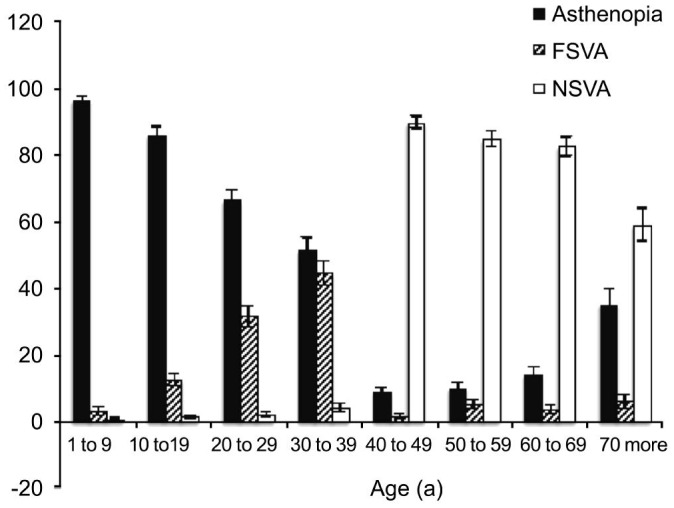
Regarding age, there was a higher frequency of asthenopia in younger age decades, with 96.1% (95%CI: 94.8-97.3) in the first decade and 85.9% (95%CI: 83.9-87.9) in the 2nd decade of life. There was a significant decline in asthenopia after 40 years of age. The poor far sighted VA occurred more often in the 3rd and 4th decades of life, with 23.1% (95%CI: 20.4-25.7) and 31.0% (95%CI: 27.2-33) of the subjects reporting this complaint. Poor near sighted VA was rare until the 4th decade, from 4.1% (95%CI: 3.5-4.7) to 89.4% (95%CI: 87.7-91.1) between 40 and 49y with a progressive decrease, reaching 58.8% (95%CI: 54.5-63.1) after 70 years of age (Figure 1).
Figure 1. Frequency and confidence interval (95%) of ocular symptoms, according to age (in years) of inhabitants of the southeast region of Brazil.
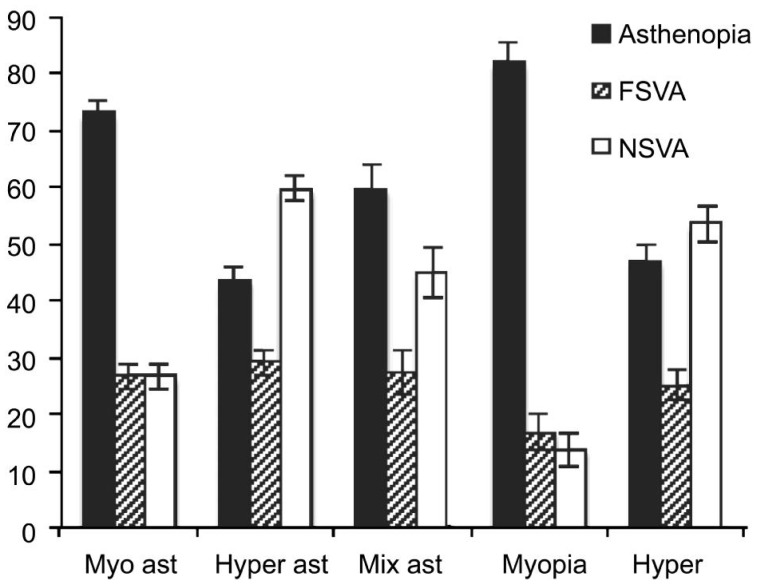
Assessment of the association between the complaints and RE showed that asthenopia was the main symptom for myopic (73.1%) or mixed astigmatism (60%) and for myopia (82.1%). Poor near sighted VA was most frequently observed in hyperopic (59.8%) and mixed astigmatism (45%) and simple hyperopia (53.7%). Poor far sighted VA was less frequent in all categories, reaching a maximum of 29.2% in the hyperopic astigmatism (Figure 2).
Figure 2. Frequency (%) and confidence interval (95% CI) of ocular symptoms in relation to refractive error in inhabitants of the southeast region of Brazil.
Myo ast: Myopic astigmatism; Hyper ast: Hyperopic astigmatism; Mix ast: Mixed astigmatism; Hyper: Hyperopia; FSVA: Far-sighted visual acuity; NSVA: Near sighted visual acuity.
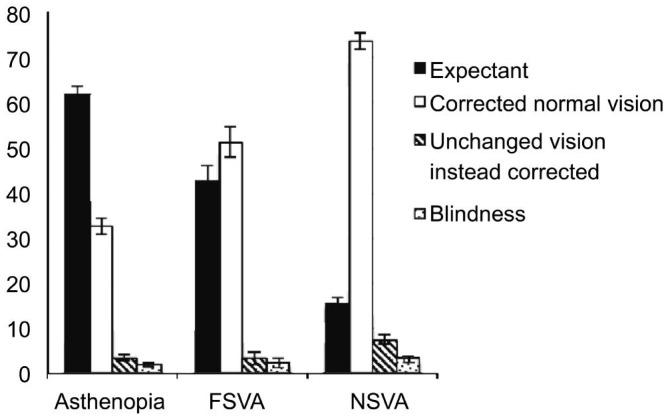
Regarding the need for treatment, the majority (62.0%) of the subjects with asthenopia had no need of corrective lenses or had VA improved with eyeglass prescription (32.0%). For those with poor far sighted VA, a new optical prescription resulted in normal vision for 51% of patients and 42% had no need of a spectacles prescription. The need for spectacles resulting in normal VA was more common for those who had poor near sighted VA (73.6%). Therefore, the need for spectacles was especially important for those individuals who showed poor near sighted VA (Figure 3).
Figure 3. Distribution and confidence interval (95% CI) according to ophthalmologic symptoms and treatment performed in inhabitants of the southeast region of Brazil.
FSVA: Far-sighted visual acuity; NSVA: Near sighted visual acuity.
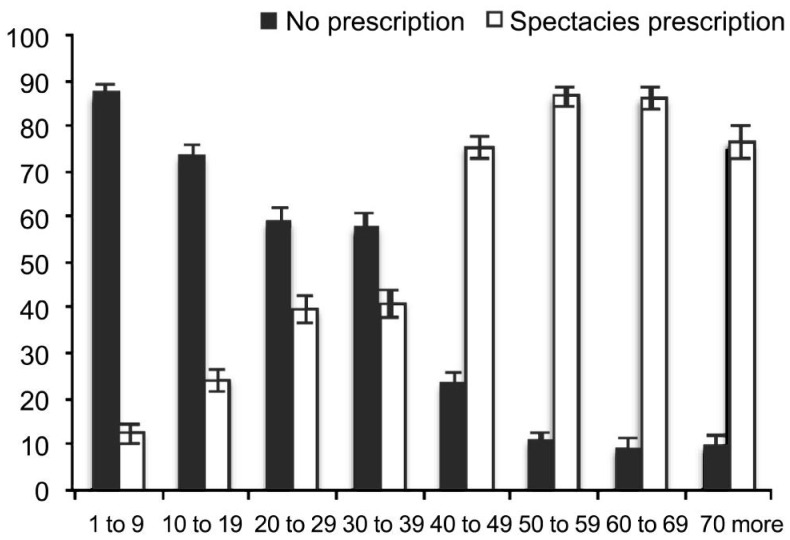
The need for an optical prescription was segmented according to age because the symptoms also showed an age dependent distribution. Thus, we observed that individuals over 40 years old were most likely to need spectacles, with a frequency of prescription reaching 86.4% (95% CI: 84.4-88.5) between 50 and 59. However, 79.2% (95% CI: 77.4-80.9) of those aged below 20y had no need of spectacles (Figure 4).
Figure 4. Relative frequency and confidence interval (95% CI) of prescribing need spectacles according to age group in the southeast region of Brazil.
DISCUSSION
The present study followed a cross section model, visiting and examining the population at the same day. This condition leave around 5% of the inhabitants not included in the sample mainly due to activities as work, school or another reason and this can be a bias in sampling. Furthermore, any participant was free for not participate.
Concerning the characteristics of the studied population, it was noted that almost all of the participants self-reported as white, although miscegenation is very common in Brazil. An analysis of the demographic data of the the study stratified by age and gender shows that there was a predominance of female in almost all the age groups and a reduction in the numbers of male in the 3rd and 4th decades, most likely because of the time of data collection coincided with work activities, reflecting the predominance of females whom work just at home as another possible bias in sampling.
Ocular Symptoms Associated with Refractive Errors
Evaluating the ocular symptoms in this population that was chosen at random, i.e. a population that resembles the general population, asthenopia was the most common ocular complaint, present mainly in subjects of ≤40 years of age, followed by the complaint of poor far sighted VA. Expressive prevalence of asthenopia was detected in children and adolescents, probably related to the amount of learning activities, time spent concentrating, and cognitive maturity[1]. According to another study, asthenopia symptom appears to be common in Chinese students and it is strongly associated with computer use, psychosocial state, environment conditions and dietary habits[10].
After 40y, the most frequent complaint was poor near sighted VA coinciding with the age of onset of presbyopia.
Eyestrain is defined as the set of symptoms related to asthenopia, including eye fatigue, eye pain, lid “weight”, difficulty focusing on objects, blurred vision, double vision, headaches, eyelid tremors, dry eye, photophobia, burning eyes, and vague symptoms, often related to the maintained effort to see clearly. This wide range of symptoms helps to understand the high variability found in asthenopia. A large number of individuals who complained of asthenopia was considered normal after the exams, which may reflect the intersection of disorders with similar signs and symptoms such as external eye diseases, sinusitis, headaches of varying causes, inflammation of the cranial nerves, or related symptoms in other organs and systems[11] and it is very difficult to separate symptoms related just to REs than others. Asthenopia symptoms might be associated with the activity performed. Notably, more than four hours daily in computer activity can cause symptoms of dry eye, redness, headache, blurred vision, eye pain and eyestrain, known as computer vision syndrome. According to others, with 30h per week over 10y, computer vision syndrome can trigger psychosomatic, depressive and obsessive behavior[12]. Unexpectedly, a large amount of children referred asthenopia instead other complaints. Commonly between infants, any type of symptoms can be misunderstood as asthenopia. Those complaints are frequently associated with uncorrected REs, generally secondarily to accommodative or vergence difficulties, heterophoria, inadequate merger and aniseikonia. So, uncorrected REs contaminates the symptoms of visual dysfunction, fundamentally when an accommodative dysfunction is present and is important to correct the RE before initiating a specific treatment to alleviate the symptoms of accommodative or vergence dysfunction[13].
The present study showed that asthenopia was more frequently associated with astigmatism (myopic, mixed or hyperopic) and hyperopia. The difficulty in positioning the circle of lower confusion on the retina and the associated visual aberrations corroborated these findings.
Complaints related to asthenopia were more frequent than poor far sighted VA for the individuals with myopic astigmatism, most likely in the large number of subjects with low degrees of myopia that could achieve reasonable distance VA with accommodative effort. Additionally, the overcorrection of myopia can cause symptoms of fatigue and the effort to produce a pinhole slit mechanism is adopted unconsciously to improve visual sharpness in those cases not properly corrected. When high myopia or hyperopia were presented, the complaint was of poor far sighted VA. Interestingly, the complaint of the myopic astigmatism carriers was poor near sighted VA, most likely reflecting the combination of this RE with presbyopia.
A similar distribution between asthenopia and poor far sighted VA reveals an association between the symptoms found mainly in subjects with astigmatism and hyperopia. Astigmatism, amblyopia, strabismus and anisometropia are more common in preschoolers with hyperopia >3.25 D and the likelihood increases as hyperopia increases[14]. Hyperopic astigmatism was related to asthenopia, but at a lower intensity. The most frequent association for hyperopic astigmatism and hyperopia was with poor near sighted VA. The large presence of presbyopia in the sample may be responsible for this increased frequency.
There was an inverse relationship between asthenopia and advancing age. Besides the pathophysiology of presbyopia still remains poorly understood, restoration of accommodation remains a challenge[15]. The weakening of the accommodative system coincides with the reduction of the frequency of asthenopia and reduction of near sighted VA, occurring in an inverse relationship with the increase prevalence of presbyopia which confirm the relation between asthenopia and endeavor of accommodation.
Complaints and the Need for Spectacles in the Studied Population
Approximately half of the group with poor far sighted VA needed spectacles prescription, most likely due to the large number of low-grade myopic that could achieve normal VA, even with an uncorrected RE. Also, it must be considered the amount of examined population who had already spectacles and did not need a new prescription.
A large need for spectacles was observed especially among the elderly, reaching 86.41% between 50 and 59 years of age. Similar results were observed in a province of China where the spectacle coverage was 44.12%, and also spectacle coverage decreased as age increased[16].
Elderly people with VI and not corrected VA are more likely to report difficulties associated with their near daily activities, activity limitations, lower quality of life, poor social participation, increased risk for falling and increased mortality[17], another reason to give special attention to the elders in the public health programs.
The greatest demand for spectacles was to correct poor near sighted VA, coinciding with the onset of presbyopia and strengthens the greatest need for spectacles to correct near vision, placing in evidence this theme as a public health problem to be solved. The same was observed in Nepal, where over 90% of people in need of near correction do not have spectacles in this setting and related with ageing and poor education[18]. Also in Timor Leste, presbyopia remains underdiagnosed and poorly corrected in the population; of the 1414 individuals of ≥40 years of age, only 11.5% were using appropriate corrections and 32.3% would benefit from wearing spectacles for near vision[19]. That sampling was performed in rural areas, where limited access to health services and literacy were cited as the causes for these findings[19]. Similarly, in a region of India, presbyopia was present in 63.7% of the subjects aged over 35y and spectacle coverage for the RE was 29% and for presbyopia it was 19%, although 63% of the individuals of ≥40y had this condition[20].
The lack of spectacles to correct presbyopia can lead to limited accurate near vision, useful for all work activities, among those individuals of ≥40y. Considering the impact a simple prescription of corrective lenses can have on quality of life, the importance of providing spectacles to correct presbyopia has been emphasized.
We did not study the social conditions of our population, but it is very well known that the older subjects, the literate and the highest level of education were more likely to wear spectacles[18],[21]. Presbyopia is highly prevalent in rural China, and nearly half of affected persons have no access to correction[22], making spectacle coverage a large unmet issue need.
In addition, given that people with presbyopia are at higher risk for permanent VI from conditions such as glaucoma and diabetic eye disease, primary eye care should include refraction services as well as the detection and appropriate referral for these and other such conditions[23]. Other suggestions to improve the spectacle coverage in developing countries are dispensing ready-made and a greater understanding of the barriers and benefits to correcting near vision will inform the design and execution of a sustainable program to correct presbyopia[24].
In summary, the most common visual complaint within a representative sample of a Brazilian population, reported by more than half of the participants, was asthenopia, which is strongly influenced by age, occurring particularly in the 2nd and 3rd decades of life. A significant association between asthenopia and astigmatism was observed, present in almost half the cases. Poor near sighted VA was more common in patients after their 40's, with a decrease in subsequent age decades, the opposite of asthenopia, which declined significantly after the 4th decade of life. Our study identified subjects of ≥40 years old as a high risk group for uncorrected RE; this observation can guide intervention programs for our population, directing governmental strategies and intending suitable resources to attend those in needing population extracts.
Acknowledgments
The ophthalmic equipment used to evaluate patients in this research were acquired by FAPESP (Fundacao de Amparo a Pesquisa do Estado de Sao Paulo)-Brazil.
Conflicts of Interest: Schellini S, None; Ferraz F, None; Opromolla P, None; Oliveira L, None; Padovani C, None.
REFERENCES
- 1.García-Muñoz Á, Carbonell-Bonete S, Cacho-Martínez P. Symptomatology associated with accommodative and binocular vision anomalies. J Optom. 2014;7(4):178–192. doi: 10.1016/j.optom.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayanniyi AA, Folorunso FN, Adepoju FG. Refractive ocular conditions and reasons for spectacles renewal in a resource-limited economy. BMC Ophthalmol. 2010;10:12. doi: 10.1186/1471-2415-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romani FA. Prevalence of ocular diseases in a population of elderly residents of the city of Veranópolis, Brazil. Arq Bras Oftalmol. 2005;68(5):649–655. doi: 10.1590/s0004-27492005000500015. [DOI] [PubMed] [Google Scholar]
- 4.Paulsen AJ, Cruickshanks KJ, Fischer ME, Huang GH, Klein BEK, Klein R, Dalton DS. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014;157(4):799–806. doi: 10.1016/j.ajo.2013.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cinoto RW, Berezovsky A, Belfort R, Jr, Salomão SR. Comparison between self-reported quality of vision and visual acuity in a low-income elderly population in the city of São Paulo. Arq Bras Oftalmol. 2006;69(1):17–22. doi: 10.1590/s0004-27492006000100004. [DOI] [PubMed] [Google Scholar]
- 6.Chan VF, Mebrahtu G, Ramson P, Wepo M, Naidoo KS. Prevalence of refractive error and spectacle coverage in Zoba Ma'ekel Eritrea: a rapid assessment of refractive error. Ophthalmic Epidemiol. 2013;20(3):131–137. doi: 10.3109/09286586.2013.783082. [DOI] [PubMed] [Google Scholar]
- 7.Marmamula S, Ravuri LV, Boon MY, Khanna RC. Spectacle coverage and spectacles use among elderly population in residential care in the south Indian state of Andhra Pradesh. Biomed Res Int. 2013;2013:183502. doi: 10.1155/2013/183502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferraz FH, Corrente JE, Opromolla P, Schellini SA. Influence of uncorrected refractive error and unmet refractive error on visual impairment in a Brazilian population. BMC Ophthalmol. 2014;14:84. doi: 10.1186/1471-2415-14-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Katz J, Tielsch JM, Sommey A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci. 1997;38(2):334–340. [PubMed] [Google Scholar]
- 10.Han CC, Liu R, Liu RR, Zhu ZH, Yu RB, Ma L. Prevalence of asthenopia and its risk factors in Chinese college students. Int J Ophthalmol. 2013;6(5):718–722. doi: 10.3980/j.issn.2222-3959.2013.05.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aynur Özge A, Termine C, Antonaci F, Natriashvili S, Guidetti V, Wöber-Bingöl C. Overview of diagnosis and management of paediatric headache. Part I: diagnosis. J Headache Pain. 2011;12(1):13–23. doi: 10.1007/s10194-011-0297-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ranasinghe P, Wathurapatha WS, Perera YS, Lamabadusuriya DA, Kulatunga S, Jayawardana N, Katulanda P. Computer vision syndrome among computer office workers in a developing country: an evaluation of prevalence and risk factors. BMC Res Notes. 2016;9:150. doi: 10.1186/s13104-016-1962-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cacho-Martínez P, Cantó-Cerdán M, Carbonell-Bonete S, García-Muñoz Á. Characterization of Visual Symptomatology Associated with Refractive, Accommodative, and Binocular Anomalies. J Ophthalmol. 2015;2015:895803. doi: 10.1155/2015/895803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kulp MT, Ying GS, Huang J, Maguire M, Quinn G, Ciner EB, Cyert LA, Orel-Bixler DA, Moore BD, VIP Study Group Associations between hyperopia and other vision and refractive error characteristics. Optom Vis Sci. 2014;91(4):383–389. doi: 10.1097/OPX.0000000000000223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Papadopoulos PA, Papadopoulos AP. Current management of presbyopia. Middle East Afr J Ophthalmol. 2014;21(1):10–17. doi: 10.4103/0974-9233.124080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu M, Tong X, Zhao R, He X, Zhao H, Liu M, Zhu J. Visual impairment and spectacle coverage rate in Baoshan district, China: population-based study. BMC Public Health. 2013;13:311. doi: 10.1186/1471-2458-13-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garin N, Olaya B, Lara E, Moneta MV, Miret M, Ayuso-Mateos JL, Haro JL. Visual impairment and multimorbidity in a representative sample of the Spanish population. BMC Public Health. 2014;14:815. doi: 10.1186/1471-2458-14-815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sapkota YD, Dulal S, Pokharel GP, Pant P, Ellwein LB. Prevalence and correction of near vision impairment at Kaski, Nepal. Nepal J Ophthalmol. 2012;4(1):17–22. doi: 10.3126/nepjoph.v4i1.5845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ramke J, du Toil R, Palagyi A, Brian G, Naduvilath T. Correction of refractive error and presbyopia in Timor-Leste. Br J Ophthalmol. 2007;91(7):860–866. doi: 10.1136/bjo.2006.110502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marmamula S, Keeffe JE, Rao GN. Uncorrected refractive errors, presbyopia and spectacle coverage: results from a rapid assessment of refractive error survey. Ophthalmic Epidemiol. 2009;16(5):269–274. [PubMed] [Google Scholar]
- 21.Bourne RR. Uncorrected refractive error and presbyopia: accommodating the unmet need. Br J Ophthalmol. 2007;91(7):848–850. doi: 10.1136/bjo.2006.112862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lu Q, He W, Murthy GV, He X, Congdon N, Zhang L, Li L, Yang J. Presbyopia and near-vision impairment in rural northern China. Invest Ophthalmol Vis Sci. 2011;52(5):2300–2305. doi: 10.1167/iovs.10-6569. [DOI] [PubMed] [Google Scholar]
- 23.Holden BA, Fricke TR, Ho SM, Wong R, Schlenther G, Cronjé S, Burnett A, Papas E, Naidoo KS, Frick KD. Global vision impairment due to uncorrected presbyopia. Arch Ophthalmol. 2008;126(12):1731–1739. doi: 10.1001/archopht.126.12.1731. [DOI] [PubMed] [Google Scholar]
- 24.Wubben TJ, Guerrero CM, Salum M, Wolfe GS, Giovannelli GP, Ramsey DJ. Presbyopia: a pilot investigation of the barriers and benefits of near visual acuity correction among a rural Filipino population. BMC Ophthalmol. 2014;14:9. doi: 10.1186/1471-2415-14-9. [DOI] [PMC free article] [PubMed] [Google Scholar]