Abstract
Background
To examine the association between potentially modifiable risk factors with cardiovascular disease (CVD) and all-cause mortality and to quantify their population attributable fractions (PAFs) among a sample of Tehran residents.
Methods
Overall, 8108 participants (3686 men) aged≥30 years, were investigated. To examine the association between risk factors and outcomes, multivariate sex-adjusted Cox proportional hazard regression analysis were conducted, using age as time-scale in two models including general/central adiposity: 1)adjusted for different independent variables including smoking, education, family history of CVD and sex for both outcomes and additionally adjusted for prevalent CVD for all-cause mortality 2)further adjusted for obesity mediators (hypertension, diabetes, lipid profile and chronic kidney disease). Separate models were used including either general or central adiposity.
Results
During median follow-up of >10 years, 827 first CVD events and 551 deaths occurred. Both being overweight (hazard ratio (HR), 95%CI: 1.41, 1.18–1.66, PAF 13.66) and obese (1.51, 1.24–1.84, PAF 9.79) played significant roles for incident CVD in the absence of obesity mediators. Predicting CVD, in the presence of general adiposity and its mediators, significant positive associations were found for hypercholesterolemia (1.59, 1.36–1.85, PAF 16.69), low HDL-C (1.21, 1.03–1.41, PAF 12.32), diabetes (1.86, 1.57–2.27, PAF 13.87), hypertension (1.79, 1.46–2.19, PAF 21.62) and current smoking (1.61, 1.34–1.94, PAF 7.57). Central adiposity remained a significant positive predictor, even after controlling for mediators (1.17, 1.01–1.35, PAF 7.55). For all-cause mortality, general/central obesity did not have any risk even in the absence of obesity mediators. Predictors including diabetes (2.56, 2.08–3.16, PAF 24.37), hypertension (1.43, 1.11–1.84, PAF 17.13), current smoking (1.75, 1.38–2.22, PAF 7.71), and low education level (1.59, 1.01–2.51, PAF 27.08) were associated with higher risk, however, hypertriglyceridemia (0.83, 0.68–1.01) and being overweight (0.71, 0.58–0.87) were associated with lower risk.
Conclusions
Modifiable risk factors account for more than 70% risk for both CVD and mortality events.
Introduction
Cardiovascular diseases (CVD) are the leading cause of both mortality and disability worldwide [1]. Approximately, two-thirds (63%) of premature deaths in adults (aged 15–69 years), and three-out-of-four of all adult deaths are attributable to non-communicable diseases, which are mainly due to CVD [2]. It has been predicted that by 2030, over 23.3 million people will die annually from CVD [3], most of which will occur in low-and-middle income countries, such as those in Middle East, where rapid changes in lifestyle, ageing populations and transforming environments all contribute to the dramatic pace of the epidemic [4]. It has been shown that CVDs are becoming a major health problem in this region mostly due to the already high and fast increasing prevalence of cardiovascular risk factors [5–11]. In spite of having higher CVD morbidity and mortality; compared to Western countries, data in regards to the dynamics of CVD from Eastern population is limited [12].
Management of the multiple modifiable risk factors associated with incident CVD and all-cause mortality in the general populations is an ongoing challenge for primary health care decision makers. Population attributable fraction (PAF), a measure of potential global impact, is one of the most applicable indices in public health which can assist policymakers in prioritizing health strategies among the general population [13]. It is the hypothetical reduction in incidence that would be observed if the population were entirely unexposed, compared with its current (actual) exposure pattern [13].
The aim of the current study is to determine the associations of potentially modifiable cardiovascular risk factors including general or central obesity, smoking, educational level, blood pressure categories, glucose intolerance status, lipid profile and chronic kidney disease (CKD) with CVD and all-cause mortality and their PAF, using data from a long-term population–based prospective study, the Tehran Lipid-Glucose Study (TLGS), with over a decade long follow-up.
Methods and Materials
Study design and sample
The Tehran Lipid and Glucose Study (TLGS) is an ongoing prospective population-based study performed on a representative sample of the Tehran population, aimed at determining the prevalence and incidence of non-communicable diseases and their risk factors. Details of the TLGS have been reported elsewhere [14]. In brief, one baseline examination (1999–2001) and 3 follow-up phases at about 3-year intervals had been carried out until 2012.
Study population
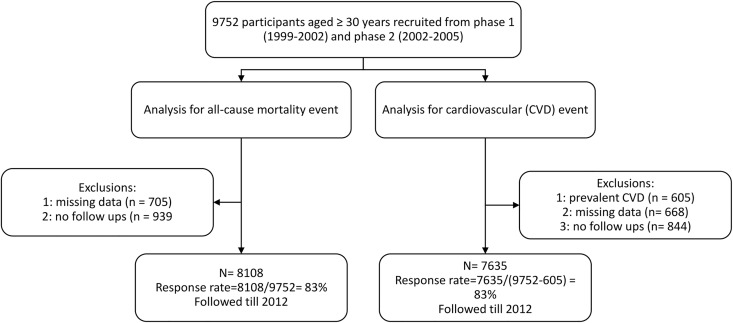
Exclusions were carried out at two separate lines for all-cause mortality and CVD event analysis. For all-cause mortality analysis, from among 9752 participants (5331 women and 4421 men) ≥30 years [7550 people from the baseline examination (1999–2001) and 1597 new participants were recruited from the second phase (2001–2005)], after exclusions of 705 cases with missing data on any examined baseline variables and 939 participants with no follow-up from baseline examination; finally 8108 participants (4422 women and 3686 men) remained to be followed till 2012, (mean follow-up of 10.67 years and 3.88 interquartile range, response rate 83%) (Fig 1).
Fig 1. Study population.
For CVD event analysis, among 9752 participants aged 30 years or more were selected. Subjects with prevalent CVD on baseline examination (N = 605), missing data (N = 668) or without any follow-up (N = 844) were excluded, leaving 7635 participants (4205 women and 3430 men) for the current study, who were followed up till 2012 (mean follow-up of 10.73 years and 3.65 interquartile range, response rate 83%) (Fig 1).
A written consent was obtained from all participants after being informed about the general aspects of the investigation and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in prior approval by the ethical committee of the Research Institute for Endocrine Sciences (RIES).
Clinical and laboratory measurements
Using a standard questionnaire, a trained interviewer collected information, which included demographic data, drug history and family history of type 2 diabetes (T2D) and CVD. Details of anthropometric measurements including weight, height and waist circumference (WC), systolic blood pressure (SBP) and diastolic blood pressure (DBP) measurements have been reported elsewhere (14).
A blood sample was taken between 7:00 and 9:00 AM from all study participants, after 12 to 14 hours overnight fasting. Details of laboratory measurement including fasting plasma glucose (FPG), total cholesterol (TC), triglyceride (TG) and high-density lipoprotein (HDL-C) were reported elsewhere (14).
Glomerular filtration rate (GFR) was estimated using the abbreviated prediction equation, provided by the Modification of Diet in Renal Disease (MDRD) study as follows:
In this equation, estimated GFR (eGFR) is expressed as mL/min per 1.73 m2 and serum creatinine (Scr) as mg/dL [15].
Definition of terms and outcomes measurement
Cardiovascular risk factors were categorized and defined as illustrated in Table 1. For a collection of cardiovascular outcomes, each participant has followed up annually for any medical event; a trained nurse asked them regarding any related medical condition, and a trained physician collected complementary data for that event, during a home visit, and also by the acquisition of data from medical files from hospitals and any medical encounters. In the current study, the events targeted were the first CVD event, including definite myocardial infarction (MI), probable MI, unstable angina, angiographic-proven CHD, and stroke (defined by a new neurological deficit that lasted more than 24 h). In case of mortality, data were collected by an authorized local physician from the hospital or the death certificate. Data collected were evaluated by an outcome committee (Cohort Outcome Panel) consisting of a principal investigator, an internist, an endocrinologist, a cardiologist, an epidemiologist, and the physician who collected the outcome data; other experts were invited as required for evaluation of non-communicable disorders. The final diagnosis was by consensus of the majority of committee members (i.e. by ≥3 members of the committee).
Table 1. Definition of different cardiovascular risk factors categories; Tehran Lipid and Glucose Study 1999–2012.
| CVD risk factor | Definition |
|---|---|
| Glucose intolerance | |
| Non-diabetic | FPG< 100mg/dl (5.55 mmol/l) and 2h-PCPG<140 mg/dl (7.77 mmol/l) and taking no anti-diabetic medications |
| Diabetic[16] | FPG ≥126 mg/dl (7 mmol/l) or 2 h-PCPG ≥200 mg/dl (11.1 mmol/l) or taking any medication for T2D |
| Pre-diabetic[17] | Individuals who were not characterized as non-diabetic or diabetic |
| General obesity | |
| Normal BMI | BMI<25 kg/m2 |
| Overweight | 25≤ BMI<30 kg/m2 |
| Obese | BMI ≥ 30 kg/m2 |
| Central obesity | Waist circumference ≥95 cm [18] |
| Blood pressure [19] | |
| Normotensive | SBP <120 mmHg and DBP <80 mmHg |
| Hypertension | SBP ≥140 mmHg or DBP ≥90 mmHg or taking any medication for hypertension |
| Pre-hypertensive | Individuals who were not characterized as normotensive or hypertensive |
| Dyslipidemia [20] | |
| Hypercholesterolemia | TC ≥ 6.21 mmol/L or using lipid lowering medications |
| Hypertriglyceridemia | TG ≥ 1.69 mmol/L |
| Low HDL-C | HDL-C< 1.06 mmol/L (men) or HDL-C<1.29 mmol/L (women) |
| Family history of CVD | History of myocardial infarction, stroke or sudden cardiac death in a male first degree relative <55 years or in a female first degree relative <65 |
| Current smoking | Participants who used any tobacco product (cigarette, pipe, and water pipe) at time of examination |
| Education | |
| <6 | Illiterate participant and those with primary school education or less (less than 6 years of education) |
| 6–12 | Those who had a diploma or did not complete the diploma but finished the primary school (6 years) |
| >12 | Those with higher than diploma education(more than 12 years of education) |
| CKD | Those with eGFR<60 mL/min/1.73 m2[21]. |
FPG, Fasting plasma glucose; 2h-PCPG, 2 hour-post-challenge plasma glucose; BMI, body mass index; T2D, type 2 diabetes; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; TG, triglycerides; HDL-C, high-density lipoprotein cholesterol; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate.
Statistical analysis
Baseline characteristics of the study population are presented as mean or frequency (percentage) for continuous and categorical variables, respectively.
All possible first-order interactions between sex and independent variables were checked in multivariable analysis (i.e. sex × BMI, sex × glucose intolerance status, sex × WC, sex × blood pressure categories, sex × TC, sex × HDL-C, sex× TG, sex × family history of CVD, sex × smoking, sex × education levels, sex × CKD, sex × prevalent CVD). Considering the Bonferroni correction as a multiple comparison correction, we found no P value ≤ 0.01 for interaction between different risk factors with sex for either CVD or mortality events [22]; hence, we adjusted for sex, to reach full statistical power, in the different models. Similarly, we also found no interaction between prevalent CVD and different risk factors for mortality events (all P-values for interactions >0.01). All of the interactions were tested by log-likelihood ratio test.
Cox proportional hazard models with age as the time scale [23], were used to estimate the hazard ratios (HRs) with 95% confidence intervals (95% CIs) of different risk factors for development of each outcome of interest in two models including general/central obesity adjusted for 1) different independent variables including smoking, education, family history of CVD and sex for both outcomes and additionally adjusted for prevalent CVD for all-cause mortality, 2) the above risk factors plus obesity mediators including blood pressure categories, glucose intolerance status, abnormal lipid profile (hypercholesterolemia, low HDL-C, and hypertriglyceridemia) [24] and chronic kidney disease (CKD) [25–28], applying the enter method. Non-modifiable risk factors including sex, family history of CVD and prevalent CVD were considered as confounder variables in our data analysis. To overcome the issue of collinearity, we conducted separate models for general and central adiposity.
The proportional hazard assumption was examined using Schoenfeld residuals test and plotting log [–log (survival)] versus log (time) to assess parallelism. Follow-up duration was defined as the period between entrance to study and the end point; end points were considered as the first CVD event or mortality, and censoring was defined as leaving the residence area, lost to follow-up or until the end of the study.
PAFs were calculated using the following formula [29]:
HRadj indicates multivariate-adjusted hazard ratio for a particular exposure factor and Pc represents the prevalence of that exposure among individuals with the outcome of interest. Stata (Stata Corp 12 SE) was used for data analysis and p values<0.05 were considered statistically significant. Additionally, to recover our missing data, we used multivariate imputation by chained equation, using a regression including all of the variables in the main models [30, 31].
Results
The study sample for analysis of all-cause mortality consisted of 8108 participants, aged ≥30 years, mean age 47.52 (range 30–88 years). Baseline characteristics of respondent and non-respondent participants (those with missing data at the baseline or with no follow-up data) in our sample are shown in Table 2. Compared to non-respondents, respondents were older, more educated and hypercholesterolemic and had higher WC; however, they had lower BMI, the rates of current smoking as well as prevalent CVD. Aforementioned results were similar in study sample for CVD events (n = 7635).
Table 2. Baseline characteristics* of respondent and non-respondent participants in both genders; Tehran Lipid and Glucose Study 1999–2005.
| Respondent (n = 8108) | Non-respondent (n = 1644) | P-value† | ||
|---|---|---|---|---|
| Continuous variables: | Mean (SD) | Mean (SD) | ||
| Age (years) ** | 47.52(12.44) | 48.30(13.96) | 0.025 | |
| BMI (kg/m2) | 27.52(4.56) | 27.18(4.74) | 0.012 | |
| Waist circumference (cm) | 90.87(11.53) | 89.87(11.52) | 0.004 | |
| Triglyceride levels (mmol/L) | 2.06(1.34) | 2.12(1.68) | 0.170 | |
| Total cholesterol (mmol/L) | 5.53(1.18) | 5.57(1.22) | 0.226 | |
| HDL-C (mmol/L) | 1.07(0.28) | 1.08(0.29) | 0.066 | |
| Systolic blood pressure (mmHg) | 121.69(19.96) | 122.37(21.13) | 0.239 | |
| Diastolic blood pressure (mmHg) | 78.64(11.03) | 78.68(11.06) | 0.900 | |
| Fasting plasma glucose (mmol/L) | 5.62(1.96) | 5.67(2.29) | 0.331 | |
| eGFR (mL/min/1.73 m2) | 68.89(11.54) | 68.03(12.55) | 0.018 | |
| Categorical variables††: | ||||
| Sex(men) | 3686(45.46) | 735(44.71) | 0.576 | |
| General obesity | ||||
| Normal BMI | 2424(29.90) | 437(26.58) | 0.076 | |
| Overweight | 3524(43.46) | 579(35.22) | ||
| Obese | 2160(26.64) | 326(19.83) | ||
| Central obesity | 3047(37.58) | 466(28.35) | 0.057 | |
| Hypertriglyceridemia | 4328(53.38) | 693(42.15) | 0.109 | |
| Hypercholesterolemia | 2248(27.73) | 423(25.73) | 0.015 | |
| Low HDL-C | 5701(70.31) | 958(58.27) | 0.442 | |
| Blood Pressure | ||||
| Normal | 3279(40.44) | 564(34.31) | 0.728 | |
| Pre hypertension | 2679(33.04) | 481(29.26) | ||
| Hypertension | 2150(26.52) | 389(23.66) | ||
| Blood Sugar Status | ||||
| Non-diabetic | 5096(62.85) | 680(41.4) | 0.003 | |
| Pre-diabetic | 1862(22.97) | 266(16.2) | ||
| Diabetic | 1150(14.18) | 205(12.5) | ||
| CKD** | 1698(20.94) | 327(19.89) | 0.09 | |
| Current smoking | 1356(16.72) | 299(18.18) | <0.0001 | |
| Education status | ||||
| >12 years | 988(12.19) | 186(11.31) | 0.022 | |
| 6–12 years | 3789(46.73) | 713(43.37) | ||
| <6 years | 3331(41.08) | 729(44.34) | ||
| Family history of CVD | 1358(16.75) | 255(15.51) | 0.618 | |
| Anti-hypertensive drug | 776(9.57) | 171(10.40) | 0.300 | |
| Anti-diabetic drugs | 447(5.51) | 90(5.47) | 0.950 | |
| Lipid lowering drugs | 327(4.03) | 82(4.99) | 0.078 | |
| Prevalent CVD | 472(5.82) | 133(8.09) | 0.001 | |
* Baseline characteristics were reported by frequency (percent) in each category and compared by Chi-square test otherwise indicated.
** Age was reported by mean (SD) in each group and compared by Student’s independent t-test.
† P-values were derived from comparison between respondent and non-respondent participants
††for categorical variables, numbers (percent), the definition of categorical variables is shown in Table 1.
eGFR, glomerular filtration rate; HDL-C, high-density lipoprotein cholesterol; CKD, chronic kidney disease.
During the follow-up period, 827 first CVD events and 551 deaths occurred. Underlying causes of mortality were CVD (n = 255), cancer (n = 89), sepsis and pneumonia (n = 48), accidents (n = 19), other heart diseases (n = 23), diabetes complications (n = 18), unknown (n = 53) and miscellaneous reasons (n = 46).
Multivariate-adjusted hazard ratios and 95% confidence intervals (CIs) of potential cardiovascular risk factors as well as their PAFs for incident CVD and all-cause mortality, controlled for BMI and in the absence of obesity mediators are shown in Table 3. Accordingly, both being overweight (HR, 95% CI: 1.41, 1.18–1.66) and obese (1.51, 1.24–1.84) played significant roles for in a higher risk of incident CVD. Furthermore, there were significant positive associations between family history of CVD, smoking and male gender with CVD events. Furthermore, smoking, less than 6 years of education, family history of CVD, male gender, and prevalent CVD remained significant predictors for higher risk of mortality. Our results showed that being overweight was associated with lower risk of mortality events (0.8, 0.66–0.97, P = 0.030).
Table 3. Multivariate-adjusted hazard ratios and 95% confidence intervals (CIs) of potential cardiovascular risk factors for incident CVD and all-cause mortality, without obesity mediators controlling for general adiposity status, Tehran lipid and Glucose study (1999–2012).
| CVD event | All-cause mortality | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% confidence interval | p-value | Prevalence* | 95% confidence interval | PAF** | 95% confidence interval | HR | 95% confidence interval | p-value | Prevalence* | 95% confidence interval | PAF** | 95% confidence | ||
| BMI | |||||||||||||||
| Normal | 1 | 0.24 | 0.21–0.27 | - | 1 | 0.36 | 0.31–0.39 | - | |||||||
| Overweight | 1.41 | 1.18–1.66 | <0.0001 | 0.47 | 0.43–0.50 | 13.66 | 6.55–19.87 | 0.80 | 0.66–0.97 | 0.030 | 0.39 | 0.35–0.43 | -9.75 | (-18.03)-(-1.32) | |
| Obesity | 1.51 | 1.24–1.84 | <0.0001 | 0.29 | 0.25–0.32 | 9.79 | 4.83–14.60 | 0.98 | 0.77–1.23 | 0.878 | 0.25 | 0.21–0.29 | - | ||
| Current Smoker | 1.53 | 1.27–1.83 | <0.0001 | 0.20 | 0.17–0.23 | 6.92 | 3.61–10.43 | 1.63 | 1.29–2.06 | <0.0001 | 0.18 | 0.14–0.21 | 6.95 | 3.14–10.80 | |
| Education | |||||||||||||||
| >12 years | 1 | 1 | 0.05 | 0.02–0.06 | - | ||||||||||
| 6–12 years | 1.22 | 0.92–1.62 | 0.159 | - | 1.49 | 0.94–2.38 | 0.088 | 0.22 | 0.19–0.26 | 7.23 | (-1.21)-15.07 | ||||
| <6 years | 1.16 | 0.87–1.55 | 0.295 | - | 1.67 | 1.06–2.63 | 0.027 | 0.73 | 0.69–0.77 | 29.28 | 3.90–47.72 | ||||
| Family history of CVD | 1.58 | 1.33–1.87 | <0.0001 | 0.21 | 0.17–0.23 | 7.70 | 4.21–10.70 | 1.33 | 1.06–1.66 | 0.011 | 0.18 | 0.14–0.21 | 4.46 | 0.79–8.34 | |
| Male gender (female as a reference) | 1.73 | 1.47–2.02 | <0.0001 | - | 1.42 | 1.17–1.73 | <0.0001 | - | |||||||
| Prevalent CVD | - | 2.01 | 1.62–2.47 | <0.0001 | 0.21 | 0.17–0.21 | 10.55 | 6.50–12.49 | |||||||
*Prevalence represents the prevalence of the exposure among individuals with outcome of interest
**The population attributed fractions were calculated using the following formula: Prevalence*((Hazard ratio-1)/Hazard ratio)
HR, hazard ratio; HDL-C, high-density lipoprotein cholesterol; CKD, chronic kidney disease
The definition of categorical variables is shown in Table 1.
Multivariate-adjusted hazard ratios and 95% confidence intervals (CIs) of potential cardiovascular risk factors as well as their PAFs for incident CVD and all-cause mortality, controlled for BMI and in the presence of obesity mediators are shown in Table 4. Accordingly, significant positive associations between hypercholesterolemia, low HDL-C level, hypertension, diabetes, current smoking, family history of CVD, male gender, and incident CVD were observed (all p values < 0.05). Predicting all-cause mortality, hypertension (1.43, 1.11–1.84), diabetes (2.56, 2.08–3.16) smoking (1.75, 1.38–2.22), less than 6 years of education (1.59, 1.01–2.51), male gender (1.48, 1.21–1.82), prevalent CVD (1.63, 1.32–2.02), family history of CVD (1.24, 0.99–1.55, P = 0.054) revealed positive associations with higher risk of death. However, general obesity (0.79, 0.62-.1.00, P = 0.058), being overweight (0.71, 0.58-.87, P = 0.001) and hypertriglyceridemia (0.83, 68–1.01; P = 0.066) were associated with lower risks of all-cause mortality.
Table 4. Multivariate-adjusted hazard ratios and 95% confidence intervals (CIs) of potential cardiovascular risk factors for incident CVD and all-cause mortality, with obesity mediators (diabetes, hypertension, lipid profile and CKD), controlling for general adiposity status, Tehran lipid and Glucose study (1999–2012).
| CVD event | All-cause mortality | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (event) | HR | 95% confidence interval | p-value | Prevalence* | 95% confidence interval | PAF** | 95% confidence interval | N (event) | HR | 95% confidence interval | p-value | Prevalence* | 95% confidence interval | PAF** | 95% confidence interval | ||
| BMI | |||||||||||||||||
| Normal | 202 | 1 | 196 | 1 | 0.36 | 0.31–0.39 | |||||||||||
| Overweight | 386 | 1.15 | 0.96–1.37 | 0.122 | 218 | 0.71 | 0.58–0.87 | 0.001 | 0.39 | 0.35–0.43 | -15.93 | (-25.34)-(-6.42) | |||||
| Obesity | 239 | 1.06 | 0.86–1.31 | 0.550 | 137 | 0.79 | 0.62–1.01 | 0.058 | 0.25 | 0.21–0.28 | -6.64 | (-12.87)-(0.27) | |||||
| High TG | 540 | 1.02 | 0.86–1.20 | 0.809 | 295 | 0.83 | 0.68–1.01 | 0.066 | 0.53 | 0.49–0.57 | -10.85 | (-0.23)-(0.56) | |||||
| High TC | 373 | 1.59 | 1.36–1.85 | <0.0001 | 0.45 | 0.41–0.48 | 16.69 | 10.85–22.05 | 210 | 1.03 | 0.85–1.25 | 0.735 | |||||
| low HDL-C | 584 | 1.21 | 1.03–1.41 | 0.020 | 0.71 | 0.67–0.73 | 12.32 | 1.95–21.22 | 336 | 0.94 | 0.78–1.13 | 0.560 | |||||
| Blood pressure status | |||||||||||||||||
| Normal | 174 | 1 | 0.21 | 0.18–0.23 | 105 | 1 | 0.20 | 0.15–0.22 | |||||||||
| prehypertension | 241 | 1.12 | 0.92–1.37 | 0.251 | 0.29 | 0.26–0.32 | 129 | 0.91 | 0.70–1.20 | 0.536 | 0.23 | 0.19–0.26 | |||||
| Hypertension | 412 | 1.79 | 1.46–2.19 | <0.0001 | 0.49 | 0.46–0.53 | 21.62 | 14.49–28.79 | 317 | 1.43 | 1.11–1.84 | 0.005 | 0.57 | 0.53–0.61 | 17.13 | 5.25–27.84 | |
| Blood sugar status | |||||||||||||||||
| Normal | 353 | 1 | 0.43 | 0.39–0.46 | 200 | 1 | 0.36 | 0.32–0.40 | |||||||||
| Pre diabetes | 223 | 1.11 | 0.94–1.32 | 0.214 | 0.27 | 0.23–0.29 | 130 | 1.13 | 0.90–1.42 | 0.267 | 0.23 | 0.20–0.27 | |||||
| Diabetes | 251 | 1.86 | 1.57–2.22 | <0.0001 | 0.30 | 0.27–0.33 | 13.87 | 9.80–18.13 | 221 | 2.56 | 2.08–3.16 | <0.0001 | 0.40 | 0.36–0.44 | 24.37 | 18.69–30.07 | |
| CKD | 276 | 1.02 | 0.86–1.19 | 0.84 | 233 | 1.02 | 0.84–1.23 | 0.809 | |||||||||
| Current Smoker | 168 | 1.61 | 1.34–1.94 | <0.0001 | 0.20 | 0.17–0.23 | 7.57 | 4.31–11.14 | 100 | 1.75 | 1.38–2.22 | <0.0001 | 0.18 | 0.14–0.21 | 7.71 | 3.85–11.54 | |
| Education | |||||||||||||||||
| >12 years | 59 | 1 | 21 | 1 | 0.05 | 0.02–0.06 | |||||||||||
| 6–12 years | 269 | 1.19 | 0.90–1.58 | 0.214 | 124 | 1.47 | 0.92–2.33 | 0.099 | 0.22 | 0.19–0.26 | 7.03 | -1.65–14.84 | |||||
| <6 years | 499 | 1.13 | 0.85–1.51 | 0.390 | 406 | 1.59 | 1.01–2.51 | 0.044 | 0.73 | 0.69–0.77 | 27.08 | 0.68–46.32 | |||||
| Family history of CVD | 171 | 1.52 | 1.28–1.80 | <0.0001 | 0.21 | 0.18–0.23 | 7.18 | 3.93–10.22 | 99 | 1.24 | 0.99–1.55 | 0.054 | 0.18 | 0.14–0.21 | 3.48 | (-0.14)-7.45 | |
| Male gender(female as a reference) | 490 | 2.02 | 1.71–2.39 | <0.0001 | 340 | 1.48 | 1.21–1.82 | <0.0001 | |||||||||
| Prevalent CVD | - | 117 | 1.63 | 1.32–2.02 | <0.0001 | 0.21 | 0.17–0.21 | 8.12 | 4.12–10.60 | ||||||||
*Prevalence represents the prevalence of the exposure among individuals with outcome of interest
**The population attributed fractions were calculated using the following formula: Prevalence*((Hazard ratio-1)/Hazard ratio)
HR, hazard ratio; HDL-C, high-density lipoprotein cholesterol; CKD, chronic kidney disease
The definition of categorical variables is shown in Table 1.
PAFs calculations, in CVD event analysis, showed that hypertension had the highest population attributed risk (21.62%) followed by hypercholesterolemia (16.69%), diabetes (13.87%), low HDL-C (12.32%) and smoking (7.57%). As for all-cause mortality, having less than 6 years of education had the highest attributed risk (27.08%), followed by diabetes (24.37%), hypertension (17.13%), prevalent CVD (8.12%) and smoking (7.71).
Multivariate-adjusted hazard ratios and 95% confidence intervals (95% CIs) of potential cardiovascular risk factors as well as their PAFs for incident CVD and all-cause mortality, controlled for central adiposity and in the absence and presence of obesity mediators are shown in Tables A and B in S1 File, respectively. Results were generally as same as those observed in the presence of general adiposity; however, in contrast to general adiposity, abdominal obesity had a significant association with CVD, in the presence of mediators (1.17, 1.01–1.35).
The results of imputation analysis were similar to our main results (Tables C-J in S1 File).
Discussion
Using data from a 10-year follow-up of an Iranian adult population, we estimated the association of potential cardiovascular risk factors as well as their PAFs for incident CVD and all-cause mortality rate. To the best of our knowledge, this is the first study conducted in the Middle East region, reporting the population attributable fraction of potential risk factors for incident CVD and all-cause mortality. Considering CVD event, in the absence of obesity mediators, general obesity, being overweight and high WC was associated with higher CVD incidence. Additionally, in the presence of mediators, hypercholesterolemia, low HDL-C, hypertension, diabetes, and smoking were attributed to higher CVD event rate. Central obesity, per se, in the presence of obesity mediators, had an independent positive association with CVD incidence. Considering all-cause mortality, although significant positive associations were observed for hypertension, diabetes, smoking and low education level; hypertriglyceridemia was inversely associated. Modifiable risk factors including hypertension, diabetes, smoking (for both CVD and mortality events), plus hypercholesteremia and low HDL-C (for CVD) and low education level (for mortality events) accounted for more than 70% of the PAF of both outcomes.
General and central obesity which are commonly assessed with BMI and WC respectively were associated with higher risk of incident CVD and all-cause mortality [32, 33]. In the current study, only in the absence of obesity mediators, being overweight and obesity showed significant risk for CVD events and whereas all together they showed a PAF of about 23%. However, in our data analysis, it has been indicated that the detrimental effect of general obesity on CVD event was mediated by hypertension, T2D and serum lipid profile. A pooled analysis of 97 prospective cohorts with 1.8 million participants, showed almost over 50% of the excess risk for CVD was mediated through three metabolic risk factors which can be explained as obesity mediators i.e. blood pressure categories, glucose intolerance status, abnormal lipid profile [24]. Furthermore, studies showed that obesity is associated with an increased incidence of CKD [25, 26] and CKD, per se, plays a role as an independent predictor of MI, stroke, and death [27, 28]. Hence, we added CKD as another obesity mediator.
In line with other studies [34–36], we showed that central adiposity was associated with higher risk of incident CVD. A finding which indicated that, in contrast to BMI, in the presence of obesity mediators, WC, per se, increased the risk of CVD incidence. In several large-scale studies, WC was found to be one of the most important predictors of CVD [37–39]. Cerhan.et al, also reported higher WC in both genders to be associated with higher mortality at all levels of BMI between 20–50 kg/m2 [34]; their finding supports the importance and major role of central obesity over general obesity in predicting incident CVD; which also was highlighted in other publications[40, 41]. On the other hand, for all-cause mortality, consistent with several studies, our results are supportive of the well-known “obesity paradox” [42–44]. We found that compared to normal BMI participants, overweight and obsess individuals had over 20% decreased risk for all-cause mortality. It has been shown that there is a U-shaped association between BMI and all-cause mortality with the concave regions sitting in the region of BMI 22–27 kg/m2[45]; this U-shaped relationship might be a result of the fact that BMI is composed of different components, i.e. fat mass, and fat-free mass, which have opposite effects on mortality, i.e. in contrast to fat mass, fat-free mass has an inverse association with mortality [46]. Furthermore, in a recent meta-analysis, overweight and moderately obese participants had lower mortality compared to normal BMI participants [33]. The authors concluded that use of predefined standard BMI groupings can facilitate between-study comparisons. Hence in the current study, we applied standard cutoffs for categorization of general adiposity. It should also be considered that over half of obese subjects in our population had grade 1 obesity (30–35 kg/m2) (Data not shown). Possible explanations include the earlier presentation of illness in overweight/obese population, greater likelihood of receiving optimal medical treatment, the cardio-protective metabolic effects of increased body fat, having better nutrition status and benefits of higher metabolic reserves [47]. It also should be considered in our study, following CVD, cancer and sepsis were the most common causes of death and weight loss is one of the most well-known poor prognostic factors in patients with both malignant and inflammatory diseases [48–50].
In line with previous studies, we observed both incident CVD and all-cause mortality to be increased among participants with diabetes [51–53]. Generally, diabetes is a prevalent metabolic disorder among Iranians [54] and is known as a coronary heart disease equivalent [55]. In the light of the high incidence and PAF of diabetes in this population [56], greater fraction of CVD and mortality event rates are expected to be attributable to diabetes in the future.
Similar to previous studies, we showed that hypertension is an independent, putative risk factor for incident CVD and all-cause mortality [57] and reduction in hypertension incidence remarkably reduces the risk of incident CVD and all-cause. In fact, hypertension is known as the most important modifiable risk factor for CVD and all-cause mortality worldwide [58, 59]. Therefore, more aggressive efforts may help decrease CVD risk and mortality among those already affected by inadequately treated or untreated hypertension.
More than 7% of incident CVD and of all-cause mortality were attributable to smoking in our study sample. Compared to current literature which reported smoking to be responsible for approximately 12% and 6% of male and female deaths respectively, worldwide [60, 61]. Recent studies also show that smoking in Iranian populations has an experiencing increasing trend [10, 62, 63]; this coupled with the fact that in Iran, unlike developed countries, smoking cessation counseling services are infrequently available or actively offered by health professionals.
It has been reported that even smoking a few cigarettes during childhood are associated with significantly higher odds of daily smoking in adolescence [64]. The prevalence of 15% was reported for current smoking in a study conducted among Iranian male high school adolescents [65]. However, unfortunately, we have no data in our study sample about the initiation trend of smoking and amount of tobacco use during childhood. Our findings showed that prioritization of smoking controlling programs at national levels to be effective strategies for the prevention of CVD and premature death.
Considering dyslipidemia, in the current study, hypercholesterolemia and low HDL-C, all together, account for about 30% of PAF of incident CVD. The significant roles of hypercholesterolemia and low HDL-C as well-established risk factors for incident CVD have been highlighted before[66]. Treatment of elevated cholesterol and mixed lipid disorders using statins may relieve some of the burden, as recently noted for patients with diabetes and stroke[66]. Despite the fact that the lipid-lowering drugs consumption in our population has increased remarkably (1.59 vs. 6% within a decade)[10], almost one-third of our population with dyslipidemia have not achieved the target levels of lipid measures may be due to poor compliance [10]. We also observed a favorable time trends in the population levels of lipid profile including HDL-C during 10 years follow-up [11].
One intriguing result reached through our study was that high serum TG was inversely associated with all-cause mortality among participants. Recently, we showed that 1 SD increment in log-transformed TGs was accompanied with 19% lower risk of non-CVD mortality [67]. A contention in contrast with previous studies, which highlighted the linear relation between hypertriglyceridemia and mortality [68, 69]; one explanation would be that low TG could be a marker of malnutrition and weight loss which, in turn, may increase mortality risk in the population [70]. In our study, after CVD, cancer was the most common cause of death and it has been shown that the low TG and weight loss are poor prognostic signs in cancerous patients and are associated with poor survival [48–50, 71]. Recently, we showed that hypertriglyceridemic waist circumference increased the age-adjusted risk of incident CVD, among both men and women [72]. Noticeably, in previous studies, we detected favorable time trends in the population levels of TG in the TLGS population (from 2.11 to 1.94 mmol/L in men and from 1.88 to 1.74 mmol/L in women) [11]; this significant decrease in TG levels could be the other plausible justification to this intriguing result.
Importantly, lower education level potentially increased the risk of all-cause mortality by about 60% and showed the highest PAF of 27% among other risk factors. A steady relationship documented between mortality and educational inequalities indicated that higher education status is associated with better adaptation to preventive lifestyles, lower prevalence of risk factors, early diagnosis and management of chronic disease risk factors, better quality treatment of acute diseases and lower risk of malnutrition and infection [73]. In line with our findings, Yusuf et al. found that nine easily measured and potentially modifiable risk factors such as education level account for an overwhelmingly large (over 90%) proportion of the risk of an initial acute myocardial infarction [74].
The strengths of our study include the prospective nature, the use of a large population-based-cohort of both sexes, accurate and valid data on risk factors at baseline and continuous surveillance of mortality, based on standard criteria. Our findings, however, need to be interpreted in the light of our study limitations. First, the population studied was of Persian ancestry, because of which, our results might not be directly extrapolated to other populations. Second, we only considered the status of risk factors at baseline and did not consider changes during the long-term follow-up. Third, we did not have enough statistical power to investigate the impact of risk factors for cause-specific mortality events. Fourth, we also used PAF as an epidemiologic tool to quantify the burden of CVD and mortality attributable to modifiable risk factors. This guides policymakers in prioritizing health strategies and interventions. In fact, PAF is a theoretical concept, and total elimination of certain risk factors by conducting intervention programs at the population level is generally almost impossible. In this regard, PAF is a better tool for prioritization than attributable risk. In most epidemiological studies, PAF measures only the excess fraction (the proportion of cases developing over some period of time among the exposed population, i.e. “excess” in comparison with the unexposed), rather than etiologic fraction (the proportion of cases in which the exposure has a causal role in disease occurrence) [75]. Last but not least, in a population-based observational cohort study of TLGS, the extent and importance of the risk factors are highlighted and the effect of treatment, interventions and the impact of different methods for accomplishing the changes shall be tested in clinical trial settings.
Conclusion
Among modifiable risk factors, we found positive associations between diabetes, hypertension, current smoking and both outcomes; hypercholesterolemia, low HDL-C and CVD incidence; low education level and all-cause mortality events. These potentially modifiable risk factors which account for over 70% risk for both CVD and mortality events, indicating that modification of derived risk factors has the potential to prevent most CVD/all-cause mortality events among Tehranian adults.
Supporting Information
Multivariate-adjusted hazard ratios and 95% confidence intervals (CIs) of potential cardiovascular risk factors as well as their PAFs for incident CVD and all-cause mortality, controlled for central adiposity and in the absence and present of obesity mediators (table A and B). Results from multivariate imputation by chained equation, using a regression including all of the variables in the main models (table C-J)
(PDF)
(DTA)
(DTA)
Acknowledgments
We express our appreciation to the participants of district–13 of Tehran for their enthusiastic support in this study and would like to acknowledge Mrs. Niloofar Shiva for critical language editing of English grammar and syntax of the manuscript, Dr. Davood Khalili for valuable comments and Dr. Golnaz Babaei and Miss Marzieh Montazeri. This manuscript is the result of the thesis of Dr. Mahsa Sardarinia.
Data Availability
Data underlying the findings described is fully available, without restriction as attached in S2 File and S3 File. In order to protect sensitive patient data and upon the journal request, any column including dates was removed.
Funding Statement
This study was supported by Grant No.121 from the National Research Council of the Islamic Republic of Iran. Funding source had no role in design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
References
- 1.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet. 2013;380(9859):2197–223. [DOI] [PubMed] [Google Scholar]
- 2.Organization WH. Mortality and burden of disease estimates for WHO member states in 2008 Geneva: World Health Organization; 2010. [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. Plos med. 2006;3(11):e442 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alwan A. Global status report on noncommunicable diseases 2010: World Health Organization; 2011. [Google Scholar]
- 5.Moghaddam MM, Mohebi R, Hosseini F, Lotfaliany M, Azizi F, Saadat N, et al. Distribution of ideal cardiovascular health in a community-based cohort of Middle East population. Annals of Saudi medicine. 2014;34(2):134–42. Epub 2014/06/05. 10.5144/0256-4947.2014.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lotfaliany M, Akbarpour S, Mozafary A, Boloukat RR, Azizi F, Hadaegh F. Hypertension phenotypes and incident cardiovascular disease and mortality events in a decade follow-up of a Middle East cohort. Journal of hypertension. 2015;33(6):1153–61. 10.1097/HJH.0000000000000540 [DOI] [PubMed] [Google Scholar]
- 7.Hadaegh F, Hasheminia M, Lotfaliany M, Mohebi R, Azizi F, Tohidi M. Incidence of metabolic syndrome over 9 years follow-up; the importance of sex differences in the role of insulin resistance and other risk factors. PloS one. 2013;8(9):e76304 10.1371/journal.pone.0076304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hadaegh F, Derakhshan A, Zafari N, Khalili D, Mirbolouk M, Saadat N, et al. Pre‐diabetes tsunami: incidence rates and risk factors of pre‐diabetes and its different phenotypes over 9 years of follow‐up. Diabetic Medicine. 2015. [DOI] [PubMed] [Google Scholar]
- 9.Hadaegh F, Hasheminia M, Abdi H, Khalili D, Bozorgmanesh M, Arshi B, et al. Prehypertension Tsunami: A Decade Follow-Up of an Iranian Adult Population. PloS one. 2015;10(10):e0139412 10.1371/journal.pone.0139412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jahangiri-Noudeh Y, Akbarpour S, Lotfaliany M, Zafari N, Khalili D, Tohidi M, et al. Trends in Cardiovascular Disease Risk Factors in People with and without Diabetes Mellitus: A Middle Eastern Cohort Study. PloS one. 2014;9(12):e112639 10.1371/journal.pone.0112639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kheirandish M, Asgari S, Lotfaliany M, Bozorgmanesh M, Saadat N, Tohidi M, et al. Secular trends in serum lipid levels of a Middle Eastern adult population; 10 years follow up in Tehran lipid and glucose study. Lipids in health and disease. 2014;13:20 Epub 2014/01/25. PubMed Central PMCID: PMC3912503. 10.1186/1476-511X-13-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong Y. Burden of cardiovascular disease in Asia: big challenges and ample opportunities for action and making a difference. Clinical chemistry. 2009;55(8):1450–2. 10.1373/clinchem.2009.125369 [DOI] [PubMed] [Google Scholar]
- 13.Rothman KJ, Greenland S, Lash TL. Modern epidemiology: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 14.Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials. 2009;10(1):5. PubMed Central PMCID: PMC2656492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levey A, Bosch J, Lewis J, ROGERS N, ROTH D. A simplified equation to predict glomerular filtration rate from serum creatinine. 2000. [DOI] [PubMed]
- 16.American Diabetes A. Standards of medical care in diabetes-2015 abridged for primary care providers. Clinical diabetes: a publication of the American Diabetes Association. 2015;33(2):97–111. Epub 2015/04/22. PubMed Central PMCID: PMC4398006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bozorgmanesh M, Hadaegh F, Saadat N, Azizi F. Fasting glucose cutoff point: where does the risk terminate? Tehran lipid and glucose study. Acta diabetologica. 2012;49(5):341–8. Epub 2011/05/28. 10.1007/s00592-011-0298-5 [DOI] [PubMed] [Google Scholar]
- 18.Hadaegh F, Zabetian A, Sarbakhsh P, Khalili D, James WP, Azizi F. Appropriate cutoff values of anthropometric variables to predict cardiovascular outcomes: 7.6 years follow-up in an Iranian population. International journal of obesity. 2009;33(12):1437–45. Epub 2009/09/16. 10.1038/ijo.2009.180 [DOI] [PubMed] [Google Scholar]
- 19.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Jama. 2014;311(5):507–20. Epub 2013/12/20. 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 20.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. Epub 2002/12/18. [PubMed] [Google Scholar]
- 21.Levey A, Bosch J, Lewis J, SHAHRIARI AR, Rogers N, Roth D. A simplified equation to predict glomerular filtration rate from serum creatinine. 2000.
- 22.Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied linear statistical models: McGraw-Hill Irwin; New York; 2005. [Google Scholar]
- 23.Pencina MJ, Larson MG, D'Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Statistics in medicine. 2007;26(6):1343–59. Epub 2006/09/07. 10.1002/sim.2699 [DOI] [PubMed] [Google Scholar]
- 24.Huxley R. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1· 8 million participants. The Lancet. 2014;383(9921):970–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang Y, Ryu S, Choi Y, Zhang Y, Cho J, Kwon M-J, et al. Metabolically healthy obesity and development of chronic kidney disease: a cohort study. Annals of internal medicine. 2016;164(5):305–12. 10.7326/M15-1323 [DOI] [PubMed] [Google Scholar]
- 26.Foster MC, Hwang S-J, Larson MG, Lichtman JH, Parikh NI, Vasan RS, et al. Overweight, obesity, and the development of stage 3 CKD: the Framingham Heart Study. American Journal of Kidney Diseases. 2008;52(1):39–48. 10.1053/j.ajkd.2008.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parikh NI, Hwang S-J, Larson MG, Levy D, Fox CS. Chronic kidney disease as a predictor of cardiovascular disease (from the Framingham Heart Study). The American journal of cardiology. 2008;102(1):47–53. 10.1016/j.amjcard.2008.02.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weiner DE, Tighiouart H, Amin MG, Stark PC, MacLeod B, Griffith JL, et al. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. Journal of the American Society of Nephrology. 2004;15(5):1307–15. [DOI] [PubMed] [Google Scholar]
- 29.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. American journal of public health. 1998;88(1):15–9. Epub 1998/05/16. PubMed Central PMCID: PMC1508384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. Journal of statistical software. 2011;45(3). [Google Scholar]
- 31.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Statistics in medicine. 2011;30(4):377–99. 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- 32.Lu Y, Hajifathalian K, Rimm EB, Ezzati M, Danaei G. Mediators of the effect of body mass index on coronary heart disease: decomposing direct and indirect effects. Epidemiology (Cambridge, Mass). 2015;26(2):153–62. Epub 2015/02/03. [DOI] [PubMed] [Google Scholar]
- 33.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Jama. 2013;309(1):71–82. 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cerhan JR, Moore SC, Jacobs EJ, Kitahara CM, Rosenberg PS, Adami HO, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clinic proceedings. 2014;89(3):335–45. Epub 2014/03/04. PubMed Central PMCID: PMC4104704. 10.1016/j.mayocp.2013.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam study. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 2001;25(11):1730–5. Epub 2001/12/26. [DOI] [PubMed] [Google Scholar]
- 36.Staiano AE, Reeder BA, Elliott S, Joffres MR, Pahwa P, Kirkland SA, et al. Body mass index versus waist circumference as predictors of mortality in Canadian adults. International journal of obesity. 2012;36(11):1450–4. Epub 2012/01/18. PubMed Central PMCID: PMC4120111. 10.1038/ijo.2011.268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27 000 participants from 52 countries: a case-control study. The Lancet. 2005;366(9497):1640–9. [DOI] [PubMed] [Google Scholar]
- 38.Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet. 2004;364(9438):937–52. [DOI] [PubMed] [Google Scholar]
- 39.Balkau B, Deanfield JE, Després J-P, Bassand J-P, Fox KA, Smith SC, et al. International Day for the Evaluation of Abdominal Obesity (IDEA) a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168 000 primary care patients in 63 countries. Circulation. 2007;116(17):1942–51. 10.1161/CIRCULATIONAHA.106.676379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schulze MB, Heidemann C, Schienkiewitz A, Bergmann MM, Hoffmann K, Boeing H. Comparison of anthropometric characteristics in predicting the incidence of type 2 diabetes in the EPIC-Potsdam study. Diabetes Care. 2006;29(8):1921–3. 10.2337/dc06-0895 [DOI] [PubMed] [Google Scholar]
- 41.McKeigue P, Shah B, Marmot M. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. The Lancet. 1991;337(8738):382–6. [DOI] [PubMed] [Google Scholar]
- 42.Bucholz EM, Rathore SS, Reid KJ, Jones PG, Chan PS, Rich MW, et al. Body mass index and mortality in acute myocardial infarction patients. The American journal of medicine. 2012;125(8):796–803. PubMed Central PMCID: PMC3408565. 10.1016/j.amjmed.2012.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carl J. New insights into the “obesity paradox” and cardiovascular outcomes. Journal of Glycomics & Lipidomics. 2012. [Google Scholar]
- 44.Hainer V, Aldhoon-Hainerová I. Obesity paradox does exist. Diabetes Care. 2013;36(Supplement 2):S276–S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in a prospective cohort of US adults. New England Journal of Medicine. 1999;341(15):1097–105. 10.1056/NEJM199910073411501 [DOI] [PubMed] [Google Scholar]
- 46.Thorogood M, Appleby P, Key T, Mann J. Relation between body mass index and mortality in an unusually slim cohort. Journal of epidemiology and community health. 2003;57(2):130–3. 10.1136/jech.57.2.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hastie CE, Padmanabhan S, Slack R, Pell AC, Oldroyd KG, Flapan AD, et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. European heart journal. 2010;31(2):222–6. Epub 2009/08/19. 10.1093/eurheartj/ehp317 [DOI] [PubMed] [Google Scholar]
- 48.Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clinical nutrition. 2008;27(1):5–15. 10.1016/j.clnu.2007.10.007 [DOI] [PubMed] [Google Scholar]
- 49.Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino JR, et al. Prognostic effect of weight loss prior tochemotherapy in cancer patients. The American journal of medicine. 1980;69(4):491–7. [DOI] [PubMed] [Google Scholar]
- 50.McMahon K, Decker G, Ottery F, editors. Integrating proactive nutritional assessment in clinical practices to prevent complications and cost. Seminars in oncology; 1998. [PubMed] [Google Scholar]
- 51.Morgan CL, Currie CJ, Peters JR. Relationship between diabetes and mortality: a population study using record linkage. Diabetes Care. 2000;23(8):1103–7. [DOI] [PubMed] [Google Scholar]
- 52.Barr EL, Zimmet PZ, Welborn TA, Jolley D, Magliano DJ, Dunstan DW, et al. Risk of cardiovascular and all-cause mortality in individuals with diabetes mellitus, impaired fasting glucose, and impaired glucose tolerance: the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Circulation. 2007;116(2):151–7. 10.1161/CIRCULATIONAHA.106.685628 [DOI] [PubMed] [Google Scholar]
- 53.Taylor KS, Heneghan CJ, Farmer AJ, Fuller AM, Adler AI, Aronson JK, et al. All-cause and cardiovascular mortality in middle-aged people with type 2 diabetes compared with people without diabetes in a large UK primary care database. Diabetes Care. 2013;36(8):2366–71. 10.2337/dc12-1513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hadaegh F, Bozorgmanesh MR, Ghasemi A, Harati H, Saadat N, Azizi F. High prevalence of undiagnosed diabetes and abnormal glucose tolerance in the Iranian urban population: Tehran Lipid and Glucose Study. BMC public health. 2008;8:176 PubMed Central PMCID: PMC2413226. 10.1186/1471-2458-8-176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hadaegh F, Fahimfar N, Khalili D, Sheikholeslami F, Azizi F. New and known type 2 diabetes as coronary heart disease equivalent: results from 7.6 year follow up in a Middle East population. Cardiovascular diabetology. 2010;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Derakhshan A, Sardarinia M, Khalili D, Momenan AA, Azizi F, Hadaegh F. Sex specific incidence rates of type 2 diabetes and its risk factors over 9 years of follow-up: Tehran Lipid and Glucose Study. PloS one. 2014;9(7):e102563 PubMed Central PMCID: PMC4100911. 10.1371/journal.pone.0102563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gray L, Lee IM, Sesso HD, Batty GD. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study). Journal of the American College of Cardiology. 2011;58(23):2396–403. PubMed Central PMCID: PMC3253414. 10.1016/j.jacc.2011.07.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. The Lancet. 2006;367(9524):1747–57. [DOI] [PubMed] [Google Scholar]
- 59.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. The lancet. 2005;365(9455):217–23. [DOI] [PubMed] [Google Scholar]
- 60.Organization WH. Global health risks: mortality and burden of disease attributable to selected major risks: World Health Organization; 2009. [Google Scholar]
- 61.Gellert C, Schottker B, Brenner H. Smoking and all-cause mortality in older people: systematic review and meta-analysis. Archives of internal medicine. 2012;172(11):837–44. 10.1001/archinternmed.2012.1397 [DOI] [PubMed] [Google Scholar]
- 62.Boshtam M, Sarraf Zadegan N, Rafiei M, Tafazoli F. Smoking habits among an Iranian population. Pak J Cardiol January 2005;16(1):23–8. [Google Scholar]
- 63.Akbarpour S, Jahangiri-Noudeh Y, Lotfaliany M, Zafari N, Khalili D, Tohidi M, et al. Trends in Anthropometric Indexes, Blood Pressure, Smoking and Lipids Over a Decade in Diabetic and Non-Diabetic Populations: Tehran Lipid and Glucose Study. Iranian Journal of Epidemiology. 2015;11(2):23–36. [Google Scholar]
- 64.Jackson C, Dickinson D. Cigarette consumption during childhood and persistence of smoking through adolescence. Archives of pediatrics & adolescent medicine. 2004;158(11):1050–6. Epub 2004/11/03. [DOI] [PubMed] [Google Scholar]
- 65.Karimy M, Niknami S, Heidarnia AR, Hajizadeh I, Montazeri A. Prevalence and determinants of male adolescents' smoking in iran: an explanation based on the theory of planned behavior. Iranian Red Crescent medical journal. 2013;15(3):187–93. Epub 2013/08/29. PubMed Central PMCID: PMCPMC3745745. 10.5812/ircmj.3378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smith DG. Epidemiology of dyslipidemia and economic burden on the healthcare system. The American journal of managed care. 2007;13:S68–71. [PubMed] [Google Scholar]
- 67.Ghasemzadeh Z, Abdi H, Asgari S, Tohidi M, Khalili D, Valizadeh M, et al. Divergent pathway of lipid profile components for cardiovascular disease and mortality events: Results of over a decade follow-up among Iranian population. Nutrition & Metabolism. 2016;13(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shankar A, Mitchell P, Rochtchina E, Wang JJ. The association between circulating white blood cell count, triglyceride level and cardiovascular and all-cause mortality: population-based cohort study. Atherosclerosis. 2007;192(1):177–83. 10.1016/j.atherosclerosis.2006.04.029 [DOI] [PubMed] [Google Scholar]
- 69.Liu J, Zeng FF, Liu ZM, Zhang CX, Ling WH, Chen YM. Effects of blood triglycerides on cardiovascular and all-cause mortality: a systematic review and meta-analysis of 61 prospective studies. Lipids in health and disease. 2013;12:159 Epub 2013/10/30. PubMed Central PMCID: PMC4231478. 10.1186/1476-511X-12-159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–57. 10.1016/S0140-6736(06)68770-9 [DOI] [PubMed] [Google Scholar]
- 71.Cvetkovic Z, Cvetkovic B, Petrovic M, Ranic M, Debeljak-Martarcic J, Vucic V, et al. Lipid profile as a prognostic factor in cancer patients. J BUON. 2009;14(3):501–6. [PubMed] [Google Scholar]
- 72.Samadi S, Bozorgmanesh M, Khalili D, Momenan A, Sheikholeslami F, Azizi F, et al. Hypertriglyceridemic waist: the point of divergence for prediction of CVD vs. mortality: Tehran Lipid and Glucose Study. International journal of cardiology. 2013;165(2):260–5. 10.1016/j.ijcard.2011.08.049 [DOI] [PubMed] [Google Scholar]
- 73.Pednekar MS, Gupta R, Gupta PC. Illiteracy, low educational status, and cardiovascular mortality in India. BMC public health. 2011;11(1):567. PubMed Central PMCID: PMC3160988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet (London, England). 2004;364(9438):937–52. Epub 2004/09/15. [DOI] [PubMed] [Google Scholar]
- 75.Greenland S, Robins JM. Conceptual problems in the definition and interpretation of attributable fractions. American journal of epidemiology. 1988;128(6):1185–97. Epub 1988/12/01. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multivariate-adjusted hazard ratios and 95% confidence intervals (CIs) of potential cardiovascular risk factors as well as their PAFs for incident CVD and all-cause mortality, controlled for central adiposity and in the absence and present of obesity mediators (table A and B). Results from multivariate imputation by chained equation, using a regression including all of the variables in the main models (table C-J)
(PDF)
(DTA)
(DTA)
Data Availability Statement
Data underlying the findings described is fully available, without restriction as attached in S2 File and S3 File. In order to protect sensitive patient data and upon the journal request, any column including dates was removed.