Abstract
The purpose of this research is to determine the effects of implementing an electronic health record on medical-surgical registered nurses' time spent in direct professional patient-centered nursing activities, attitudes and beliefs related to implementation, and changes in level of nursing engagement after deployment of the electronic health record. Patient-centered activities were categorized using Watson's Caritas Processes and the Relationship-Based Care Delivery System. Methods included use of an Attitudes and Beliefs Assessment Questionnaire, Nursing Engagement Questionnaire, and Rapid Modeling Corporation's personal digital assistants for time and motion data collection. There was a significant difference in normative belief between nurses with less than 15 years' experience and nurses with more than 15 years' experience (t21 = 2.7, P = .01). While nurses spent less time at the nurses' station, less time charting, significantly more time in patients' rooms and in purposeful interactions, time spent in relationship-based caring behavior categories actually decreased in most categories. Nurses' engagement scores did not significantly increase. These results serve to inform healthcare organizations about potential factors related to electronic health record deployment which create shifts in nursing time spent across care categories and can be used to explore further patient centered care practices.
KEY WORDS: Caritas Processes, Electronic health record, Nursing, Patient-centered care, Relationship-based care, Time and motion study
The federal government, through the Office of the National Coordinator, mandated the use of electronic health records (EHRs) in order to improve patient safety and satisfaction while lowering the cost of care for all Americans. However, more information is needed on the influence the implementation has on the provision of patient-centered nursing care by registered nurses practicing at the bedside.
BACKGROUND AND SIGNIFICANCE
Utilization of the EHR in a meaningful way has been internationally adopted as a method to increase continuity of care by increasing access to health information, improve care quality, provide care coordination, and increase patient and provider satisfaction while lowering the cost of care.1–3 However, various studies have demonstrated mixed reviews due to potential disruptions in ease of communication and workflow, difficulty with computerized equipment, lack of clinical decision support capabilities, increased inefficiencies and an overall resistance to change in practice.4–9 As of 2013, approximately 40% of hospitals in the United States had not adopted a basic electronic health system.10 While in many cases, the EHR has increased patient and provider communication, decreased the incidence of errors, and streamlined workflow processes, use of EHRs has not been without its share of challenges and resistance from providers and registered nurses.11–14 The inability of health systems to quickly implement comprehensive health information technology, including widespread use of EHRs across care settings, is likely due to many factors. These factors include initial high cost, lack of interoperability between software systems, and the variability of barriers and facilitating factors between and within user groups.15–19 Further, challenges to successful adoption include learning how to navigate use of EHRs in the midst of a continuously changing healthcare environment where the need for standardization of care, ease of use of clinical decision-making tools, and care coordination is vital for the delivery of patient-centered and value-based care. There is a paucity of research on the effects of EHRs on the practice of nurses and how these changes in practice affect the nurse-patient relationship in acute care settings.
TIME AND MOTION STUDIES
The most widely cited time and motion study of medical-surgical nurses is by Hendrich and colleagues20; baseline data were collected in 36 hospital medical-surgical units within 17 health systems across 15 states about how nurses spend their time before EHR implementation. Paper documentation and care coordination systems were found to be full of inefficiencies, required duplicative charting between data collection systems, and forced nurses to spend a majority of their time outside of patient rooms at the nurses' station, resulting in significant time lost from patient care activities. A full 35% of nurses' time was spent on documentation, while 20.6% was spent on care coordination and 17.2% was spent on medication administration. A second time and motion study categorized nursing behavior at baseline and 1 year following EHR implementation in a progressive cardiac inpatient unit in a community-based hospital.21 Although nurses increased their time documenting from 23% to 35% after EHR implementation, they were able to spend 6% (P < .05) more time in direct patient care activities and 3% (P < .008) less time in indirect patient care activities. In addition, nurses spent 12% (P = .773) less time in administrative tasks.21 This finding may be explained by Kossman and Scheidenhelm's22 qualitative work, which showed that the implementation of an EHR enabled nursing staff to have much faster and easier access to patient health information and that they used the EHR system to gather data and communicate more efficiently with other medical departments. The EHR system was not used solely for documenting patient conditions or care given but was also used to access health data and coordinate care with other departments while the patient was hospitalized. This streamlined indirect nursing care work and freed up nurses for more direct nursing work.
HEALTH SYSTEM CULTURAL CONTEXT
The commitment of a multistate, faith-based, nonprofit, integrated health system on the East Coast of the United States to Meaningful Use and to installation of an EPIC-based EHR system in all of its hospitals created a rich opportunity to explore its impact on the nurse-patient relationship in acute medical-surgical settings. While studies show that nurses save an average of about 25% of their time documenting post-EHR implementation, none have documented the effects of EHR implementation on patient-centered care and on the nurse-patient relationship.23,24 These studies infer that if nurses have more time available, they will spend it with their patient in direct care in patient-centered nursing activities.
Patient-centered care is defined by the Institute of Medicine's Crossing the Quality Chasm, quoting Gerteis's work, as including “(1) respect for patients' values, preferences, and expressed needs; (2) coordination and integration of care; (3) information, communication and education; (4) physical comfort; (5) emotional support—relieving fear and anxiety; and (6) involvement of family and friends.”25 This health system strongly values the delivery of patient-centered care as described by Gerteis and has embraced Jean Watson's Theory of Human Caring (THC), which is an inclusive, humanitarian approach to patient-centered care delineated in the Caritas Processes.26,27 Table 1 outlines the 10 Caritas Processes. The health system also subscribes to the Relationship-Based Care Model, which embodies Watson's Caritas Processes and also defines the patient and family in the center of all healthcare processes.28 Figure 1 lists the components of a Relationship-Based Care Delivery System.
Table 1.
Watson's 10 Caritas Processes
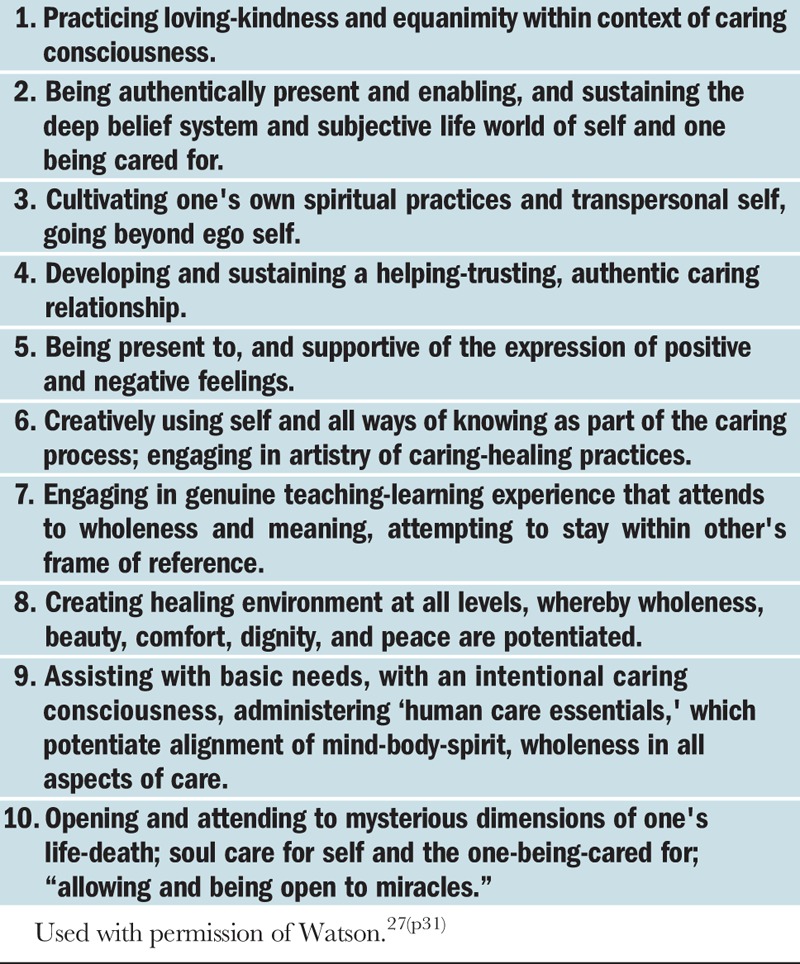
FIGURE 1.
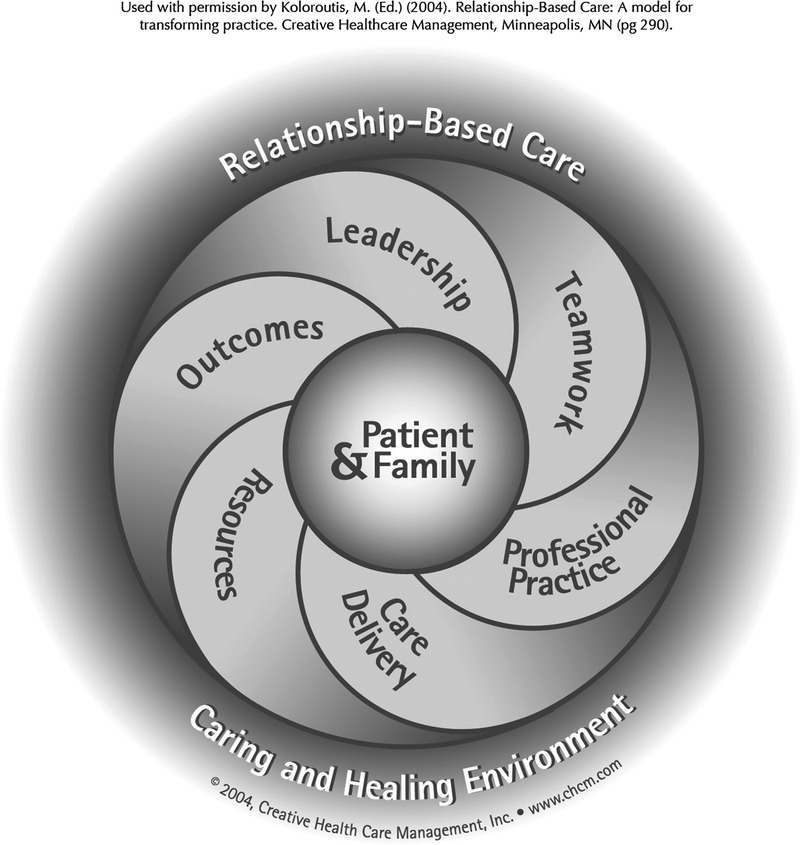
Components of a relationship-based care delivery system for a relationship-based care model.
STUDY AIM
It was with the Caritas Processes and the Relationship-Based Care Model in mind that the health system wished to understand the impact of EHR deployment on registered nurses' time spent in direct professional patient-centered nursing activities on medical-surgical units. Our study aims were to
Identify the attitudes and beliefs of nurses practicing at the bedside related to the implementation of the EHR and their subsequent ability to integrate professional nursing activities in their practice;
Examine the relationship between amounts of time spent in the patient's room and professional nursing activities; and
Explore whether change had occurred in professional nursing activities and nursing engagement pre- and post-implementation of the EHR.
THEORETICAL FRAMEWORK
Watson's THC capitalizes on nursing's deep-rooted establishment as a profession of caring, healing art, and science.26,27 It centers on the human-to-human caring practices, called Caritas Processes, which are built upon relationships designed to facilitate wellness achievement. The use of the THC's 10 Caritas Processes helps to foster communication and interactions between the nurse and the patient, which, in turn, promotes authentic emotional support, decreases anxiety, and facilitates healing.26,27 Applying the Caritas Processes creates space for nurses to cocreate a plan for care and healing and constructs a new nursing identity around the delivery of personhood-centered care.29 Implementing Watson's THC and the Relationship-Based Care Model so that patients and their families are central to nurses leading, engaging in collaborative interprofessional teamwork, in the achievement of high-quality outcomes, and in the delivery of compassionate competent care results in patient-centered care.26–28
In addition to Watson's THC and the Relationship-Based Care model, the Theory of Planned Behavior (TPB) was used to guide this study.26,27,30 The TPB examines the impact of attitudes and beliefs that could serve as facilitators or barriers to performance or adoption of a specific behavior. The TPB has been used by other healthcare providers and researchers as a model to predict behavior, especially toward acceptance of EHRs.12,15,30,31 In previous research, clinician predictors of strong belief that EHR implementation would increase productivity and performance were based upon perceptions that there was interoperability between systems, enough knowledge to operate the system, and the availability of technical support.32 Providers' positive beliefs toward and previous experience using information technology increased their readiness for using EHRs in their practice.12
SAMPLE
A purposive sample of nurses (n = 81) working 12-hour dayshifts from eight medical-surgical units across four hospitals in two states was included at baseline and about half of those nurses (n = 40) 6 months post EHR implementation from October 2010 through April 2011. Researchers attempted to include all participating nurses at T2 who had participated at T1. All nurses had to complete EHR training before obtaining a sign-on code. This training consisted of online modules, in-person classroom, practice in a nonlive environment, and passing basic proficiency tests. Flyers advertising the study were placed in staff locker rooms and bathrooms. In addition, announcements explaining the study requirements were made at all staff meetings in the month prior to starting the study. Managers were asked to leave these meetings to protect the privacy of potential participants. Participants were also recruited from coworker recommendations. Qualifications for being a medical-surgical unit included operation as a unit that provides 24-hour care for a diverse population, one that operated less than a step-down unit and intensive care unit, and was not identified as a specialty unit (ie, OB/GYN). Units were chosen based upon identification of medical-surgical units from the chief nursing officer of each facility. Inclusion criteria for participants were as follows: (1) licensed registered nurse, (2) a minimum of 32 work hours per week, (3) completed mandatory training for all nurse employees in relationship-based caring principles based on the THC, the Relationship-Based Care Model, and on the health system's Nursing Professional Practice Model, and (4) English as a primary language.
METHOD
All participants filled out a standardized institutional review board–approved 5-page consent form that included the title, purpose, procedures, time, and duration of the study. The consent form stipulated potential risks and discomforts as well as possible benefits. The consent form emphasized privacy and confidentiality, human subjects protection, and right to withdraw consent to participate at any time. All participants filled out a demographic survey and an Attitude and Beliefs Assessment on EHR Use Questionnaire. The Attitudes and Beliefs Assessment measures were devised by the researchers based upon the TPB.30 The assessment is based upon principles of the TPB and assesses intention, attitude, subjective norm, self-efficacy, behavioral beliefs, normative beliefs, and control beliefs regarding the nurse's ability to use the EHR and the ability to incorporate professional practice activities with the implementation of the EHR. The survey includes questions rated on a 5-point Likert scale, ranging from very bad to very good. An example of some of the questions were, “How easy or hard would it be for you to use an electronic health record in your professional nursing activities?” and “I am sure that I would be able to incorporate more professional nursing activities in my care with the implementation of the electronic health record.”
Participants were educated on the health system's Nursing Professional Practice Model grounded in Watson's THC Caritas Processes and in the Relationship-Based Care Model to ensure that they had received consistent on-boarding education, even if they were not new to the health system.26–28 These 30-minute in-services were face-to-face on study units and took place before and during work hours. All nurses participating in the study were in-serviced in small groups or one-on-one using PowerPoint (Microsoft, Redmond, WA) and handouts.
The initial PDA prompt inquired whether the nurse was engaged in a purposeful interaction with the patient. Purposeful interactions are a major component of having a caring relationship that facilitates healing, supports Caritas Processes 1 to 4 and 8 to 10, supports principles in the Relationship-Based Care Model, and is embedded in the health system's Nursing Professional Practice Model.26,27,33 How to conduct a 5-minute purposeful interaction with patients was included in the in-service. The health system defined purposeful interactions as dedicating 5 minutes of uninterrupted personal interaction time with a patient, sitting down and being at eye level with the patient, and letting the interaction be patient guided to identify patient-preferred goals. The goal of a purposeful interaction is for the intentional presence of nurses to create a healing and trusting relationship where they authentically listen to the patient and hold their concern in their practice by individualizing care toward the patient's unique needs. During this 5-minute interaction, the nurse is not doing any other task and may engage in contextual and culturally appropriate comforting touch. For nonverbal patients, the nurse may simply sit next to the patient and be a caring presence.
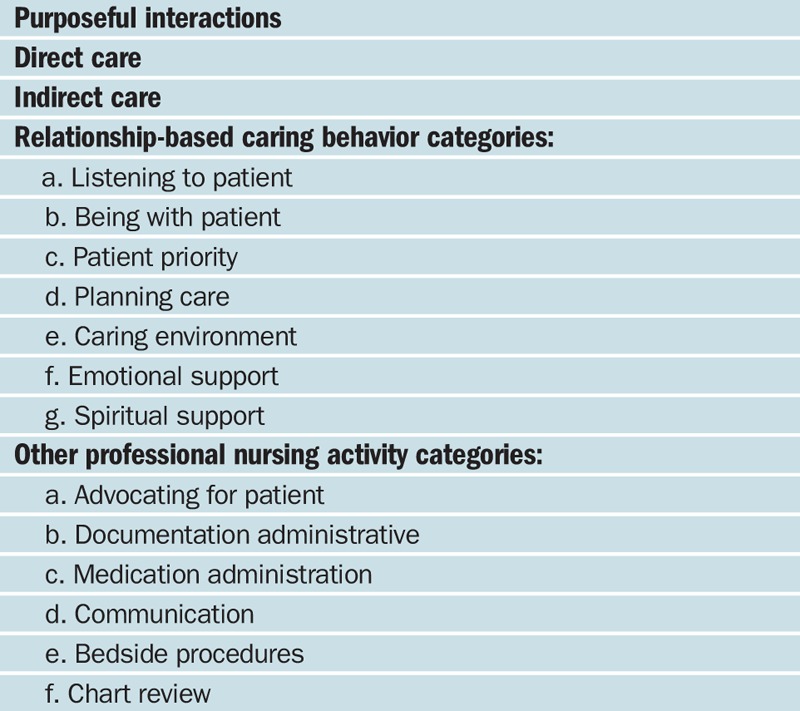
Rapid Modeling Corporation's (Batavia, OH) personal digital assistants (PDAs) were used to assess professional practice activities pre EHR and 6 months post EHR implementation. The PDAs were programmed with activity categories based on the first four essentials of practice of the American Nurses Association (ANA) standards of professional practice, Watson's THC, the Relationship-Based Care Model, and the health system's Nursing Professional Practice Model.26–28,33 Table 2 lists ANA standards of practice, while Table 3 lists PDA categories. Personal digital assistants were also used for location assessment because not all hospitals in the study had Wi-Fi installed to enable radiofrequency identification (RFID) technology. How to respond to the electronic prompts of the PDA designed to assess professional activities was included in the in-service. The PDA device signaled randomly throughout 12-hour shifts for three consecutive scheduled shifts, prompting the nurse to select the appropriate activity being conducted at the time of the prompt. Nurses were instructed to not interrupt a direct patient care activity if the PDA signaled during a critical moment, such as a dressing change, and instead were asked to document their activity as soon as they completed it. When an activity was assessed, an affirmative response received a value of 1 and a negative response received a value of 0. All nursing activities were clustered into categories. To identify a total score for professional nursing activities, responses were combined to reveal an overall activity score per activity category, with higher scores reflecting more time spent in the nursing activity category. Frequencies and percentages were also scored to determine the amount of time spent in and out of the patient's room before and after the EHR implementation.
Table 2.
ANA's Essentials of Contemporary Professional Nursing Practice
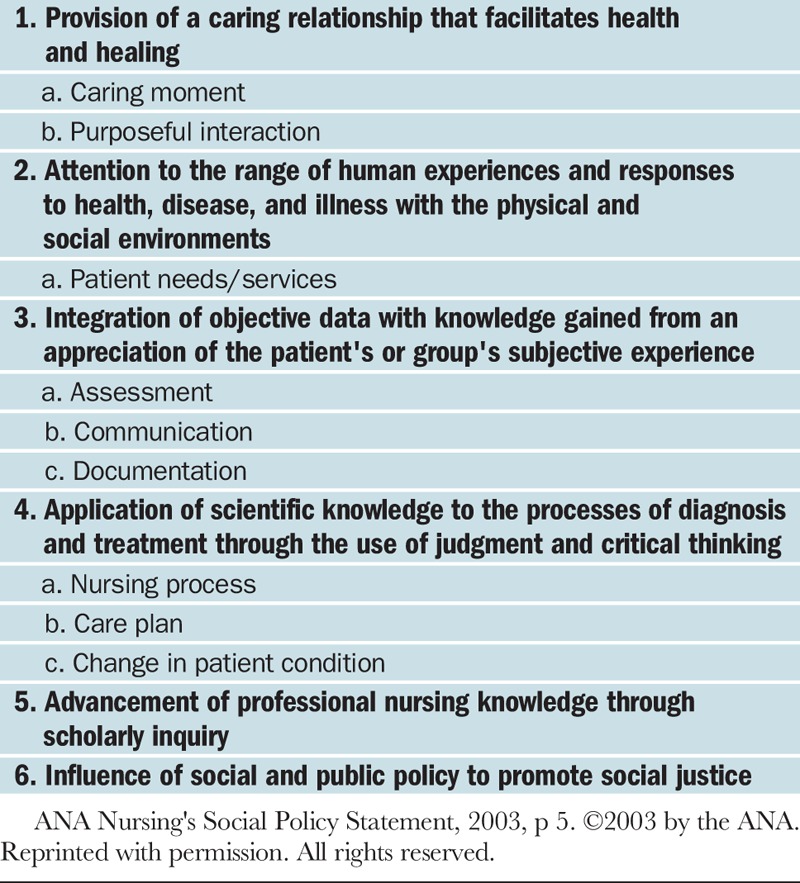
Table 3.
PDA Categories
Nursing engagement was assessed using the Nursing Engagement Gallup poll data obtained during the previous fiscal year prior to implementation of the EHR and repeated annually (post implementation of the EHR). Since engagement data are assessed in aggregate at the unit level, overall registered nurse engagement level was assessed at the unit level. The researchers did not conduct a power analysis but simply strove to enroll as close to 100 participants as possible.
FINDINGS
Demographics
The demographics of the sample population revealed that 78% identified as white, 14% identified as black, 4% identified as Asian, 2% identified as mixed, and 2% did not disclose ethnic origin. Forty-one percent had an associate's degree; 38%, a bachelor's degree; and 20%, a nursing diploma; only 2% identified as having a master's degree as the highest educational level attained.
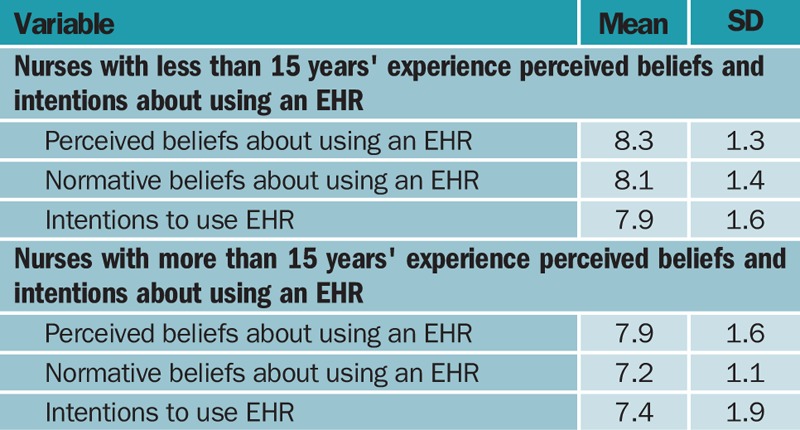
Attitudes and Beliefs
Attitudes and beliefs about using an EHR were favorable. An independent-samples t test was conducted to evaluate whether attitudes and beliefs of using an EHR would differ based upon educational level of the nurse. The only significant difference was between diploma graduate nurses' and associates degree nurses' intent to use an EHR (t23 = 2.56, P = .01). Both diploma- and associate-prepared nurses were less positive than baccalaureate-prepared nurses about EHR use. All other tests were not significant, and the mean values were similar across groups. Table 4 lists the mean values. Findings indicate that when looking at experience level, there was a significant difference in normative belief between nurses with less than 15 years' experience and nurses with more than 15 years' experience (t21 = 2.7, P = .01), possibly indicating that nurses with less experience were more favorable with the use of the technology because it was more of a normative behavior for them. Nurses with less experience had overall more perceived beliefs that they could use an EHR (mean [SD], 8.3 [1.3]), more normative beliefs (mean [SD], 8.1 [1.4]), and more intentions to use an EHR (mean [SD], 7.9 [1.6]) than did nurses who had more experience and reported lower perceived beliefs (mean [SD], 7.9 [1.6]), lower normative beliefs (mean [SD], 7.2 [1.1]), and less intentions (mean [SD], 7.4 [1.9]).
Table 4.
Mean Values Across Groups for EHR Values and Beliefs
Time Spent in Professional Activities
Descriptive analysis of PDA data (Figures 2 and 3) revealed that nurses spent 27% of their time in the patient room during T1, before EHR deployment, and 42% of their time in patient room T2, 6 months after EHR implementation. Nurses also spent less time at the nurses' station in T2 (38%) compared to in T1 (43%). The overall percentage of other professional activities did not largely increase, which was 14% at T1 and 15% at T2. Time spent in purposeful interaction at T1 was 37% and increased to 46% during T2.
FIGURE 2.
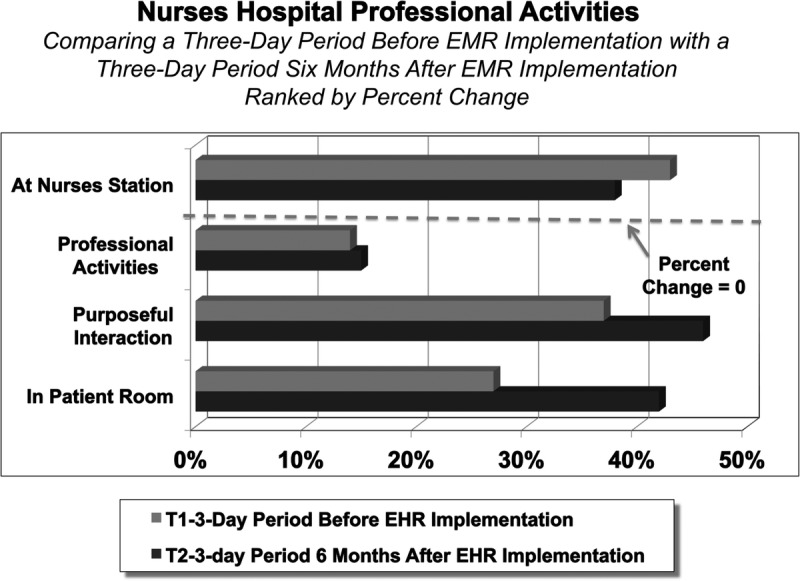
Comparing time spent in a 3-day period before EMR implementation with a 3-day period 6 months after EMR implementation ranked by percentage change.
FIGURE 3.
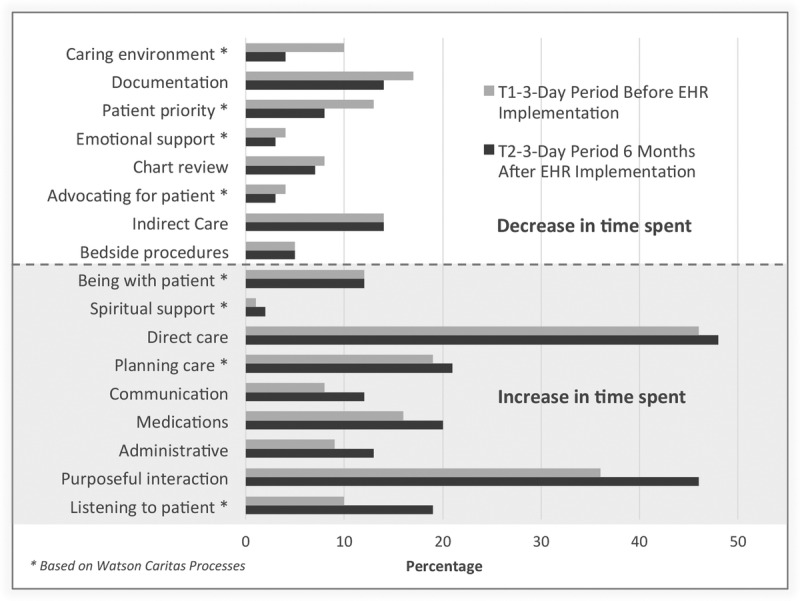
Comparing time spent in a 3-day period before EMR implementation with a 3-day period 6 months after EMR implementation ranked by percentage change in all activities.
Analysis of the relationship-based caring behavior categories indicate that during T1, nurses spent the most amount of time planning care for the patient (19%) and equal amounts of time being with the patient (12%) and making the patient a priority (12%). Listening to the patient (10%) and providing a caring environment (10%) were evenly matched. Nurses spent the least amount of time providing emotional support (4%), advocating for the patient (4%), and providing spiritual support (1%). Other professional nursing activities revealed that nurses spent most of their time in documentation (18%), followed by giving meds (16%), in chart review (8%), administrative tasks (9%), communication (8%), and conducting bedside procedures (5%).
During T2, 6 months after EHR implementation, nurses spent the majority of their time in the relationship-based caring behavior categories of listening to the patient (19%), being with the patient (12%), and making the patient a priority (9%), with the least amount of time spent providing a caring environment (4%), providing emotional support and advocating for the patient (3%), and providing spiritual support (2%). Other professional nursing activity category results in T2 include planning care for the patient and medication administration (21%), time spent in administrative tasks (14%), documentation (14%), communication (12%), chart review (7%), and conducting bedside procedures (5%).
Nursing Engagement
An investigation was conducted to determine if there was a significant increase in the Registered Nurse Engagement Survey administered in 2010 and again in 2011 (preimplementation and postimplementation survey). There was a concern regarding the sampling unit of the department that resulted in a small sample of 11. However, research has shown that these small samples could be analyzed using the paired-sample t test with samples as small as five if the within-pair correlation is high.34
A paired-samples t test was conducted to evaluate whether registered nurses rated the Registered Nurse Engagement Survey higher after EHR deployment (intervention) was conducted. The sample consisted of 11 departments' mean scores on the administration of the Registered Nurse Engagement Survey in 2010 and these departments' mean scores in 2011. The paired sample correlations was relatively high and significant (r11 = 0.783, P = .004). The results indicated that the mean (SD) score on the preimplementation survey (4.42 [0.226]) was slightly greater than on the postimplementation survey (4.39 [0.302]) (t10 = 0.593, P = .278). The standardized effect size index, Cohen d, was 0.178, reflecting a small effect size. Plausible explanation for the lack of significance is the range of mean scores from the departments. On the pre–Registered Nurse Engagement Survey, the range was 0.65 (4.07 minimum to 4.72 maximum), and on the post–Registered Nurse Engagement Survey, the range was 0.84 (3.94 minimum to 4.78 maximum).
DISCUSSION
The researchers did not collect date of birth information from participants so they cannot conclude that nurses with diploma or ADN degrees and nurses with more experience were older and therefore less likely to be comfortable with computers and EHR use than younger, less experienced, and more educated nurses. However, the researchers believe that it was more likely the age and level of familiarity with computers than the degree level that was associated with attitudes and beliefs about EHR use. As increasing percentages of younger nurses enter the workforce, more nurses are likely to feel more normative toward using an EHR.
While nurses spent less time at the nurses' station and significantly more time in patients' rooms and in purposeful interactions 6 months post EHR implementation, time spent in relationship-based caring behavior categories actually decreased except for the categories of listening to the patient, being with the patient, and providing spiritual support. Other professional nursing activity categories of documentation decreased by 4%, while chart review decreased by only 1% post EHR implementation. Administrative behaviors increased from 9% to 14%, medication administration increased from 16% to 21%, and communication increased from 8% to 12%. It is likely that 6 months post EHR implementation, nurses adapted to using the EHR for documentation and for chart review, which freed up their time to engage in other activity category types. While it is likely that significant increases in time listening to the patient accounted for the largest rise in purposeful interaction, it is disappointing that increased time to focus on patients' concerns did not lead to increases in more time in relationship-based caring behavior categories. Also surprising was the lack of time spent by registered nurses in a faith-based health system giving spiritual support or providing emotional support. While all participants completed education sessions on the health system's Nursing Professional Practice Model, the THC, and the Relationship-Based Care Model, researchers did not determine how nurses defined giving spiritual support. Definitions of spiritual support may have been narrow and defined as only praying with the patient; nurses may have felt it was solely the chaplains' job to give spiritual support.
Although researchers were able to determine percentage of time nurses spent in the patient's room, they were not able to determine what nurses were doing in the room unless it involved activities that included the patient, such as listening to the patient and being with the patient. Medication administration required nurses to be both outside as well as inside the patient's room. Either computer workstations-on-wheels were in use or every patient room had a laptop computer mounted on a wall so nurses may have been documenting or performing chart review while they were in the room. This does not explain all the increase in time spent in patient rooms since overall time in documentation and chart review decreased after EHR implementation. Nurses being in the room with a patient does not necessarily equate to higher quality care if interactions are not patient centered.
Nursing staffing on all medical-surgical units was adequate. The health system participates in the Premier OperationsAdvisor database and benchmarks all medical-surgical nursing departments. Based on internal comparisons across hospitals and external in the National Database for Nurse Quality Indicators, the health system found the best outcomes when staffed between the 25th and 33rd percentile ranking. They did not find a substantial improvement in nurse-sensitive outcomes when staffed above the 50th percentile. Confirming that staffing was adequate ensured that nurses could choose to spend time in purposeful interactions and in the Caritas Processes.
While some units showed a slight increase in Gallop nursing engagement scores, overall scores slightly decreased after EHR implementation. While there are no direct questions on level of satisfaction with EHR use, questions solicited whether the nurse had enough materials and equipment to do their work right, had the opportunity to do their best every day, and had opportunities to learn and grow. Satisfaction scores were very high pre EHR implementation, which could explain for the lack of overall significant findings since the score range between pretest and posttest was narrow. Other issues besides EHR use may have been the cause of lower post-engagement scores on some units, especially units who were in-between managers.
LIMITATIONS
Limitations for this study include the lack of consistent Wi-Fi capability across all hospitals at the time of this study so the researchers could not use RFID technology, which led to solely self-reported time nurses spent in activities. Although staff nurses' identities were carefully protected, nursing managers knew which of their units were participating in the study and it may have been obvious which nurses were participating due to the presence of PDAs in their hands. Nurses' knowledge that their managers knew about their participation may have biased their self-reports. In one of the four participating hospitals, none of the nurses participating during T1 data collection pre EHR deployment participated during T2 data collection 6 months post EHR deployment. While this may have skewed the results, there was only a 1% variation at T1 when data from the fourth hospital was removed from analysis. Because of this small variation, all data from all four hospitals were left in the final analysis of findings. In addition, not all nurses who participated in the study from the rest of the hospitals participated in T2 data collection; only about 50% of nurses participated in T2 overall. Asking nurses to self-report on PDAs for three consecutive scheduled shifts was burdensome as about 10% of the nurses were compliant with PDA responses only 2 out of the 3 days in T1 so the researchers averaged the data between consistent PDA responders and nonconsistent PDA responders. This may have biased results toward nurses who had more time or organizational skills to more consistently respond to PDA prompts.
While TPB has been used extensively to examine the impact of attitudes and beliefs and the primary investigator had extensive experience using TPB, the Attitudes and Beliefs Assessment was not independently tested for reliability or validity. Researchers relied on expert knowledge and experience for tool development. This may have biased survey findings.
IMPLICATIONS FOR FUTURE RESEARCH
Mixed-method studies are needed to determine factors related to EHR deployment, which creates shifts in nursing time spent across care categories. Simply capturing time spent in categories is not enough to determine which factors influenced time spent in activities across categories pre and post EHR deployment. While nurses may spend more time in the patient's room post EHR deployment, this does not guarantee that it is time well spent in individualizing care and in improving the overall patient care experience. More data are needed to determine what health systems can do to ensure that extra nursing time is well spent for the good of the patient. Reporting burden must be decreased to ensure that nurses who participated in baseline assessment data collection participate in end point data collection. Sample size should be increased to reduce chance of bias.
CONCLUSION
As health systems move toward data-driven systems and meaningful use, it is critical to not lose sight of the human beings we care for. Technology is a tool that should help frontline nurses deliver the highest-quality, safe, and patient-centered care achievable. It should never get in the way of treating patients as vulnerable human beings who need their healthcare givers to address their concerns as competently and as humanely as possible. To this end, further research needs to be conducted to determine factors that prevent nurses from spending enough time in relationship-based caring behaviors and technological processes that are likely to increase their time individualizing care.
Acknowledgments
The authors thank Diane Stager, Director, Marketing and Communications, Planning, Marketing and Communications, who helped with all the figures.
Footnotes
Bon Secours Health System, Inc, fully funded this research study.
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
References
- 1.Dahm MF, Wadenten B. Nurses' experiences of and opinions about using standardized care plans in electronic health records: a questionnaire study. J Clin Nurs. 2008: 2137–2145. doi:10.1111/j.1365-2702.2008.02377.x [DOI] [PubMed] [Google Scholar]
- 2.Milstein A, Darling H. Better U.S. health care at lower cost. Issues Sci Technol. 2013;26(2): 31–40. [Google Scholar]
- 3.Murphy J. The journey to meaningful use of electronic health records. Nurs Econ. 2010;28(4): 282–286. [PubMed] [Google Scholar]
- 4.Collins SA, Fred M, Wilcox L, Vawdrey DK. Workarounds used by nurses to overcome design constraints of electronic health records. Nurs Inform. 2012;93 [PMC free article] [PubMed] [Google Scholar]
- 5.Embi PJ, Weir C, Efthimiadis EN, Thielke SM, Hedeen AN, Hammond KW. Computerized provider documentation: findings and implications of a multisite study of clinicians and administrators. J Am Med Inform Assoc. 2013;20: 718–726. doi:10.1136/amiajnl-2012-000946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furukawa M, Raghu T, Shao B. Electronic medical records and cost efficiency in hospital medical-surgical units. Inquiry. 2010;47(2):110–123. doi:10.5034/inquiryjrnl_47.02.110 [DOI] [PubMed] [Google Scholar]
- 7.Furukawa M, Raghu T, Shao B. Electronic medical records, nurse staffing, and nurse-sensitive patient outcomes: evidence from California hospitals, 1998-2007. Health Serv Res. 2010;45(4): 941–962. doi:10.1111/j.I475-6773.2010.01110.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haughom J, Kriz S, McMillan D. Overcoming barriers to EHR adaption. Healthc Financ Manage. 2011;65(7): 96–100. [PubMed] [Google Scholar]
- 9.Stewart R, Kroth P, Schuyler M, Bailey R. Do electronic health records affect the patient-psychiatrist relationship? A before & after study of psychiatric outpatients. BMC Psychiatry. 2010;10(3). http://www.biomedcentral.com/1471-244X/10/3. Accessed April 19, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charles D, Gabriel M, Furukawa M. Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008–2013. The Office of the National Coordinator for Health Information Technology Data Brief, May 2014. http://www.healthit.gov/sites/default/files/oncdatabrief16.pdf. Accessed April 19, 2016.
- 11.Emani S, Ting DY, Healey M, et al. Physician beliefs about the impact of meaningful use of the EHR: a cross-sectional study. Appl Clin Inform. 2014;5(3): 789–801. doi:10.4338/ACI-2014-05-RA-0050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holden RJ. Physicians' beliefs about using EMR and CPOE: in pursuit of a contextualized understanding of health IT use behavior. Int J Med Inform. 2010;79(2): 71–80. doi:10.1016/j.ijmedinf.2009.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy J. Nursing and technology: a love/hate relationship. Nurs Econ. 2010;28(6): 405–408. [PubMed] [Google Scholar]
- 14.Whittaker A, Aufdenkamp M, Tinely S. Barriers and facilitators to electronic documentation in a rural hospital. J Nurs Scholarsh. 2009;41(3): 293–300. doi:10.1111/j.1547-5069.2009.01278.x [DOI] [PubMed] [Google Scholar]
- 15.Gagnon MP, Ouimet M, Godin G, et al. Multi-level analysis of electronic health record adoption by health care professionals: a study protocol. Implement Sci. 2010;5: 30 doi:10.1186/1748-5908-5-30. http://www.implementationscience.com/content/5/1/30. Accessed April 19, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grove DH, Patel V. Physician motivations for adoption of electronic health records. The Office of the National Coordinator for Health Information Technology Data Brief, December 2014. http://healthit.gov/sites/default/files/oncdatabrief-physician-ehr-adoption-motivators-2014.pdf. Accessed April 19, 2016.
- 17.Janols R, Lind T, Goransson B, Sandblad B. Evaluation of user adoption during three module deployments of region-wide electronic patient record systems. Int J Med Inform. 2014;83: 438–449. doi:10.1016j.ijmedinf.2014.02.003. http://www.biomedcentral.com/content/pdf/1471-244X-10-3.pdf. Accessed April 19, 2016. [DOI] [PubMed] [Google Scholar]
- 18.McGinn C A, Gagnon M P, Shaw N, et al. Users' perspectives of key factors to implementing electronic health records in Canada: a Delphi study. BMC Med Inform Decis Mak. 2012;12: 105 doi:10.1186/1472-6947-12-105. http://www.biomedcentral.com/1472-6947/12/105. Accessed April 19, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Struik M, Koster F, Schuit A, Nugteren R, Veldwijk J, Lambooij M. The preferences of users of electronic medical records in hospitals: quantifying the relative importance of barriers and facilitators of an innovation. Implement Sci. 2014;9(69). doi:10.1186/1748-5908-9-69. http://www.implementationscience.com/content/9/1/69. Accessed April 19, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hendrich A, Chow M, Skierczynski B, Lu Z. A 36-hospital time and motion study: how do medical surgical nurses spend their time? Perm J. 2008;12(3): 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Banner L, Olney C. Automated clinical documentation: does it allow nurses more time for patient care? Comput Inform Nurs. 2009;27(2): 75–81. doi:10.1097/NCN.0b013e318197287d [DOI] [PubMed] [Google Scholar]
- 22.Kossman S, Scheidenhelm S. Nurses' perceptions of the impact of electronic health records on work and patient outcomes. Comput Inform Nurs. 2008;26(2): 69–77. doi:10.1097/01.NCN.0000304775.40531.67 [DOI] [PubMed] [Google Scholar]
- 23.Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12(5): 505–516. doi:10.1197/jamia.M1700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson D, Johnston P, Spurr C. The impact of electronic medical records on nursing efficiency. J Nurs Adm. 2009;39(10): 444–451. doi:10.1097/NNA.0b013e3181b9209c [DOI] [PubMed] [Google Scholar]
- 25.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century Committee on Quality of Health Care in America. Washington DC: National Academy of Sciences National Academy Press; 2001. http://iom.edu/Reports/2001/Crossing-the-Quality-Chasm-A-New-Health-System-for-the-21st-Century.aspx. Accessed April 19, 2016. [Google Scholar]
- 26.Watson J. Nursing: The Philosophy and Science of Caring. Boulder, CO: University Press of Colorado; 1979. [Google Scholar]
- 27.Watson J. Nursing: The Philosophy and Science of Caring. Rev ed Boulder, CO: University Press of Colorado; 2008. [Google Scholar]
- 28.Koloroutis M. (Ed). Relationship-Based Care: A Model for Transforming Practice. Minneapolis, MN: Creative Healthcare Management; 2004. [Google Scholar]
- 29.Watson J, Foster R. The Attending Nurse Caring Model: integrating theory, evidence and advanced caring-healing therapeutics for transforming professional practice. J Clin Nurs. 2003;12(3): 360–365. doi:10.1046/j.1365-2702.2003.00774.x [DOI] [PubMed] [Google Scholar]
- 30.Ajzen I. Organizational behavior and human decision processes. Theory Planned Behav. 1991;50(2): 179–211. doi:10.1016/0749-5978(91)90020-T [Google Scholar]
- 31.LeBlanc G, Gagnon MP, Sanderson D. Determinants of primary care nurses' intention to adopt an electronic health record in their clinical practice. Comput Inform Nurs. 2012;30(9): 496–502. doi:10.1097/NXN.0b013e318257db17 [DOI] [PubMed] [Google Scholar]
- 32.Chisolm DJ, Purnell TS, Cohen DM, McAlearney AS. Clinician perceptions of an electronic medical record during the first year of implementation in emergency services. Pediatr Emerg Care. 2010;26(2): 107–110. doi:10.1097/PEC.0b013e3181ce2f99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American Nurses Association. Nursing's Social Policy Statement. 2nd ed Washington, DC: ANA Press; 2003. [Google Scholar]
- 34.De Winter JCF. Using the Student's t-test with extremely small sizes. Pract Assess Res Eval. 2013;18(10). http://pareonline.net/getvn.asp?v=18&n=10. Accessed April 19, 2016. [Google Scholar]


