Abstract
Randomized clinical trials (RCTs) with first- and second-generation drug-eluting stents (DESs) confirmed the superiority of coronary artery bypass surgery (CABG) in patients with multiple vessel disease. In spite of different DES designs, investigators in these trials used similar percutaneous coronary intervention (PCI) strategies hoping to achieve complete revascularization, meaning that all intermediate lesions would be stented. One of these studies also included small vessels in the revascularization policy. On this revision, authors searched for a potential explanation of these intriguing findings and also for solutions to this problem, not seen years ago when other RCTs compared CABG with PCI in the previous DES era. After they revised old and new scientific data, they concluded that improved DES design is not itself enough to narrow the gap between PCI and CABG and that in the future RCTs we should institute more conservative strategies avoiding unnecessary multiple DES implantation.
Keywords: drug-eluting stents, coronary artery bypass surgery, multiple vessel disease, randomized clinical trials, completeness of revascularization
It has almost been 25 years since the first randomized clinical trials (RCTs) comparing coronary artery bypass surgery (CABG) with coronary balloon angioplasty (POBA) in multiple vessel disease were published.1–5
During those years, several RCTs between percutaneous coronary intervention (PCI) – with either POBA or bare metal stents (BMS) – versus CABG in patients with a clinical indication for myocardial revascularization were conducted, and they consistently showed a similar comparative long-term incidence of death and myocardial infarction (MI), in spite of a greater number of repeat revascularization procedures with PCI. In these trials, the extent of coronary artery disease (CAD) was not associated with a better survival with CABG, and only diabetic patients had an inferior survival after percutaneous procedures.3,5–10 In addition, results from merged data of RCTs between BMS versus CABG in multiple vessel disease population (ARTS,11 ERACI II,12 MASS,13 and SoS9), published in 2008 by the investigators of these trials,14 did not show any differences between both revascularization strategies in either death (91.8% and 91.5%, respectively, P = 0.78) or death/MI/stroke (83.3% and 83.1%, respectively, P = 0.64).
Furthermore, with the composite end point of death/MI/stroke, there was no interaction between diabetics and nondiabetics with either of the revascularization strategies (P = 0.65).
With the introduction of drug-eluting stents (DESs) in clinical practice, the superiority of effectiveness of DESs over BMS has been largely demonstrated in head-to-head comparison in several RCTs as well as in observational studies and meta-analysis.15–19 Therefore, we would expect a substantial improvement in PCI results over CABG, narrowing the gap of recurrences in favor of CABG.
However, that was not the case and, on the contrary, all RCTs and observational studies between DESs and CABG showed that the gap in the rate of recurrences remained and there is an unexpected increased rate of cardiac death and MI in patients treated with DESs in both diabetic and nondiabetic patients.20–23
One of the explanations for this phenomenon was that, with no doubt, first-generation DESs were associated with an unacceptable high rate of stent thrombosis (SET); overall SET incidence was 15.4% at five years in the SYNTAX trial, which was related to an increased incidence of cardiac death and MI.24 In recent years, however, new-generation DESs significantly improved safety compared to the original ones, in terms of stent malapposition and stent strut coverage, which was reflected in a significant lower incidence of late and very late SET as well as the requirement for long-term dual antiplatelet therapy,25–27 although neoatherosclerosis was present.28
New randomized trials with these new-generation DESs29,30 were conducted, and one of them recently published the long-term outcome.
The BEST trial randomized patients with two- and three-vessel disease to either PCI with everolimus-eluting stents (EESs) or CABG.30 In spite of better DES design compared to the previous ones, PCI patients had again a significant greater incidence of spontaneous MI (P = 0.004) and new revascularization procedures (P < 0.001) than CABG patients. In addition, although death rate was not significantly different, it was indeed greater with PCI. In this trial, completeness of revascularization required all intermediate lesions to be stented; therefore, stent length was 85.3 mm. Stent length in this study suggested that they used a similar PCI strategy that the SYNTAX trial did (86.1 mm), although, in SYNTAX, 33.3% of patients had more than 100 mm of stent deployed;20 contrary to SYNTAX, the BEST trial included patients with two-vessel disease and excluded patients with left main stenosis.
Even more recently, authors of the SYNTAX and BEST trials published a pooled data from an individual patient level of these two RCTs comparing CABG versus DESs in patients with multiple vessel disease in the subgroup of non-diabetic patients.31 The BEST trial, which excluded diabetics, provided all patients for the analysis, whereas in SYNTAX only patients with three-vessel disease and no diabetics were included. Needless to say, nondiabetic patients have been largely considered the most favorable patients to be treated with PCI.10
The pooled data advantages of CABG over PCI went across major subgroups including DES design and, most important and surprising, showed no trial interaction (P = 0.913) for the primary outcome of death and death/MI/stroke all in favor of CABG (P = 0.037 and P = 0.011, respectively). Furthermore, a remarkable lower rate of MI in CABG was seen (P < 0.001) mostly driven by the occurrence of spontaneous MI after 30 days in the PCI group (P < 0.004).
Many interventional cardiologists, including us, are deeply concerned and disappointed with these intriguing findings. So what would then be the potential message for the cardiology community? Maybe, even in the new DES era, the superiority of CABG over PCI in multiple vessel disease is still undisputable across all subgroups of patients.
Is That the True and Simple Answer?
What was different in PCI between the two merged analysis described above?14,31 We may argue that patients treated with DESs had more three-vessel disease (87.3% vs. 36.1% with BMS) and perhaps a higher SYNTAX score than those treated with BMS (in fact, we will never know which was the SYNTAX score for them). However, on the other hand, BMS pooled data also included diabetic population (18.1% vs. 0% with DESs) and more frequently compromise of proximal LAD stenosis (90% vs. 59% with DESs).14,31
The fact that first-generation DESs were used in SYNTAX trial could be one of the most attractive explanations; in fact, SYNTAX patients with definitive SET (6.8%) had 35.4% occurrences of cardiac death.24 However, that was not the case with EES used in the BEST trial, which significantly improved safety compared to the first designs. Therefore, perhaps, stent design itself is not solely the reason for the poorer long-term outcome data of these two RCTs.
If we analyze the trial methods,21,30 in spite of different DES designs, both studies share similar PCI strategies, meaning that the goal was to achieve complete anatomic revascularization defined by authors “as not any residual stenosis 50% in any major coronary artery or their large branches”30; consequently, we can assume that many intermediate lesions were stented and that concurs with the similarity of stent length in both studies.
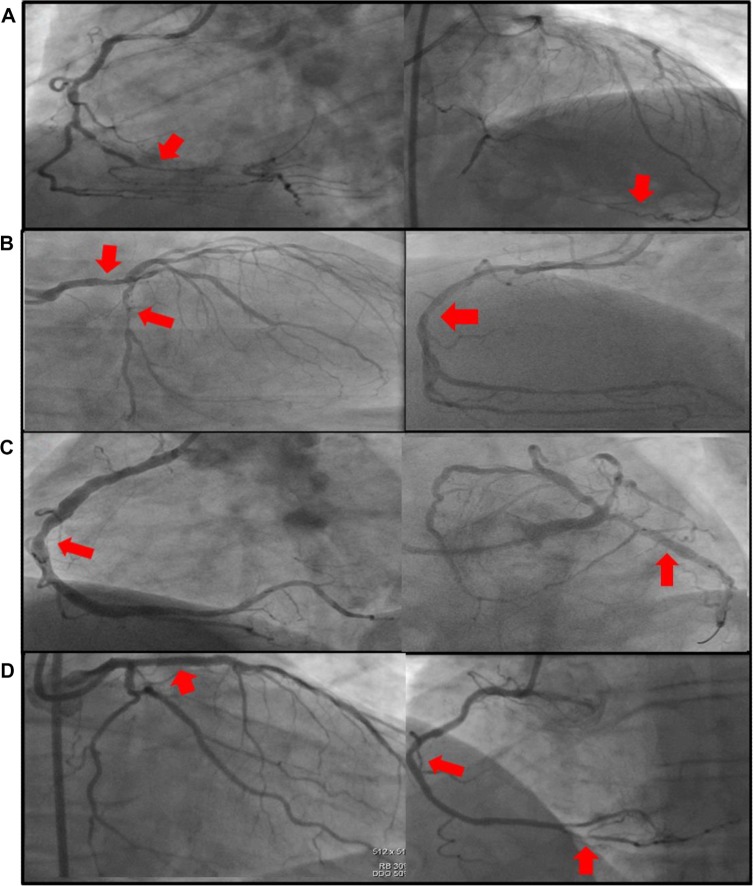
When we analyze completeness of revascularization with PCI,1 we should take into account several different situations such as the amount of myocardium at risk or stenosis severity of the lesions not included in the revascularization strategy. Prognosis in patients with incomplete revascularization should be different if the not-attempted vessels had a complete chronic closure with collateral circulation (Fig. 1A), high-degree steno-sis in a large vessel (Fig. 1B), intermediate stenosis in a large vessel (Fig. 1C), or severe stenosis in a small branch (Fig. 1D). Differences in the amount of completeness of revascularization with both, PCI and CABG, was present in all RCTs since the first study was performed; however, in the past, such differences were not associated with poorer outcome4,14 (53.2% with PCI vs. 82.7% with CABG, P = 0.0003, see Table 1). Furthermore, the fact that only 56.7% and 50.9% of SYNTAX and BEST patients, respectively, in the PCI arm achieved the goal of complete revascularization demonstrated how difficult it is for PCI to achieve such aim.31
Figure 1.
PCI STRATEGY: (A) Chronic closure in RCA with collateral circulation from LAD. (B) Intermediate stenosis in LMA and severe stenosis in LCX not treated and intermediate stenosis in mid portion of a large RCA after PCI. (C) Intermediate stenosis in a large RCA not treated and intermediate stenosis in LCX after DES deployment in LCX. (D) Proximal LAD after DES deployment and severe stenosis in a small PDA plus intermediate lesion in RCA not treated.
Abbreviations: LAD, Left Anterior Descending artery; RCA, Right Coronary Artery; LCX, Left Circumflex artery; LMA, Left Main Artery; PDA, Posterior Descending Artery; PCI, Percutaneous Coronary Intervention.
Table 1.
Completeness of revascularization of randomized clinical trials and registries between percutaneous coronary interventions (PCI) and coronary artery bypass surgery (CABG).
| STUDY | COMPLETE ANATOMIC REVASCULARIZATION (%) | P | |
|---|---|---|---|
| CABG | PCI | ||
| ERACI* | 88 | 51 | 0.001 |
| ERACI II** | 85 | 50.2 | 0.002 |
| ERACI III*** | 85 | 48 | 0.001 |
| ARTS** | 84.1 | 70.5 | 0.001 |
| MASS II** | 74 | 41 | 0.001 |
| SYNTAX*** | 63.2 | 56.7 | 0.005 |
| BEST*** | 71.5 | 50.9 | 0.004 |
| Mean | 74% | 55.3% | 0.001 |
Notes:
POBA.
BMS.
DES. ERACI, reference 1. ERACI II, reference 6. ERACI III, reference 15. ARTS, reference 7. MASS II, reference 8. SYNTAX, reference 22. BEST, reference 30.
Abbreviations: POBA, Plenty optimal balloon angioplasty; BMS, bare metal stents; DES, drug eluting stents.
Therefore, improved DES design is only one face of the problem, while changing PCI strategies using a more conservative policy during DES implantation would be the other.
If We Combined Both, We May Improve the Long-Term PCI Outcome
The ERACI IV study,32,33 with a patient population of multiple vessel disease and left main stenosis, used a second-generation DES and a conservative PCI strategy, defined as stenting only severe lesions (visually ≥70%) in large vessels. Intermediate (>50 to <70) lesions in small or large vessels or severe lesions in small vessels (<2.0 mm) were not included. The results coincide with the stent length of the study: 41.7 mm. This PCI strategy of not scoring lesions not included in the revascularization strategy allowed to build a new scoring system where low SYNTAX score was found in 54% of patients and only 17.2% of patients persisted with high SYNTAX score.34
Investigators of ERACI IV, at more than two years of follow-up, reported remarkable low rates of adverse events including death/MI/stroke of 3.9%, unplanned new revascularization of only 4%, and death/MI/stroke/target vessel revascularization (TVR) of 6.7%. It is important to note that there was no major penalty for this conservative policy as it was reflected by the low TVR rate in the not-stented intermediate lesions (1.3%).
We do not know whether these results will remain at a five-year follow-up, although at the present time, the low rate of events in the not-stented lesions supports the PCI strategy of this study. In agreement, FAME investigators largely demonstrated that nonischemic lesions had better outcome when they were not treated with DESs.35,36
We have to take into account that, even in the era of safer DESs, neoatherosclerosis as a consequence of DES implantation has not disappeared.28
To recap, interventional cardiologists have been doing a lot of work during this 25-year journey trying to close the safety/efficacy gap between PCI and CABG in patients with multiple vessel disease and, looking at long-term results from RCTs with the old and new DESs, we may conclude that improved stent design alone is not enough to narrow the gap between PCI and CABG.37
New revascularization strategies during PCI and the search for a more functional revascularization avoiding unnecessary DES implantation should be the new goal for future randomized comparisons between PCI and CABG.
The game between PCI and CABG is not over.
Footnotes
ACADEMIC EDITOR: Thomas E. Vanhecke, Editor in Chief
PEER REVIEW: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 329 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: AER. Analyzed the data: AER, HP, JDP. Wrote the first draft of the manuscript: AER. Contributed to the writing of the manuscript: HP, JDP. Agree with manuscript results and conclusions: AER, HP, JDP. Jointly developed the structure and arguments for the paper: AER, HP, JDP. Made critical revisions and approved final version: AER. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Rodríguez A, Boullón F, Perez Baliño N, et al. Argentine randomized trial of percutaneous transluminal coronary angioplasty versus coronary artery bypass surgery in multi-vessel disease (ERACI): in-hospital results and 1-year follow-up. J Am Coll Cardiol. 1993;22:1060–7. doi: 10.1016/0735-1097(93)90416-x. [DOI] [PubMed] [Google Scholar]
- 2.Hamm CW, Reimers J, Ischinger T, et al. A randomized study of coronary angioplasty compared with bypass surgery in patients with symptomatic multi-vessel coronary disease. German Angioplasty Bypass Surgery Investigation. N Engl J Med. 1994;331:1037–43. doi: 10.1056/NEJM199410203311601. [DOI] [PubMed] [Google Scholar]
- 3.On behalf of The Bypass Angioplasty Revascularization Investigation (BARI) Investigators Comparison of coronary bypass surgery with angioplasty in patients with multi-vessel disease. N Engl J Med. 1996;335:217–25. [Google Scholar]
- 4.Bourassa MG. Clinical trials of coronary revascularization: coronary angioplasty vs. coronary bypass grafting. Curr Opin Cardiol. 2000;15(4):281–6. doi: 10.1097/00001573-200007000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Pocock SJ, Henderson RA, Rickards AF, et al. Meta-analysis of randomized trials comparing angioplasty with bypass surgery. Lancet. 1995;346:1184–9. doi: 10.1016/s0140-6736(95)92897-9. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez AE, Bernardi V, Navia J, et al. Argentine randomized study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multiple vessel disease (ERACI II): 30-day results and one-year follow-up results. J Am Coll Cardiol. 2001;3:51–8. doi: 10.1016/s0735-1097(00)01052-4. [DOI] [PubMed] [Google Scholar]
- 7.Serruys PW, Unger F, Sousa JE, et al. Comparison of coronary artery bypass surgery and stenting for the treatment of multi-vessel disease. N Engl J Med. 2001;344:1117–24. doi: 10.1056/NEJM200104123441502. [DOI] [PubMed] [Google Scholar]
- 8.Hueb W, Soares P, Gersh B, et al. The medicine, angioplasty, or surgery study (MASS II trial): a randomized controlled clinical trial of three therapeutic strategies for multi-vessel coronary artery disease. J Am Coll Cardiol. 2004;43:1743–51. doi: 10.1016/j.jacc.2003.08.065. [DOI] [PubMed] [Google Scholar]
- 9.On behalf of SoS Investigators Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multi-vessel coronary artery disease (the stent or surgery trial): a randomized controlled trial. Lancet. 2002;360:965–70. doi: 10.1016/S0140-6736(02)11078-6. [DOI] [PubMed] [Google Scholar]
- 10.Hlatky MA, Boothroyd DB, Bravata DM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomized trials. Lancet. 2009;373(9670):1190–7. doi: 10.1016/S0140-6736(09)60552-3. [DOI] [PubMed] [Google Scholar]
- 11.Serruys PW, Ong AT, Van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the arterial revascularization therapies study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46(4):575–81. doi: 10.1016/j.jacc.2004.12.082. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez AE, Baldi J, Fernández Pereira C, et al. Five-year follow-up of the Argentine randomized trial of coronary angioplasty with stenting versus coronary bypass surgery in patients with multiple vessel disease (ERACI II) J Am Coll Cardiol. 2005;46(4):582–8. doi: 10.1016/j.jacc.2004.12.081. [DOI] [PubMed] [Google Scholar]
- 13.Hueb W, Lopes NH, Gersh BH, et al. Five-year follow-up of the medicine, angioplasty, or surgery study (MASS II). A randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2007;115(9):1082–9. doi: 10.1161/CIRCULATIONAHA.106.625475. [DOI] [PubMed] [Google Scholar]
- 14.Daemen J, Boersma E, Flather M, et al. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: a meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation. 2008;118(11):1146–54. doi: 10.1161/CIRCULATIONAHA.107.752147. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez AE, Grinfeld L, Fernandez-Pereira C, et al. Revascularization strategies of coronary multiple vessel disease in the drug eluting stent era: one-year follow-up results of the ERACI III Trial. EuroIntervention. 2005;294(10):1215–23. [PubMed] [Google Scholar]
- 16.Stone GW, Ellis SG, Cannon L, et al. Comparison of a polymer-based paclitaxel-eluting stent with a bare metal stent in patients with complex coronary artery disease: a randomized controlled trial. JAMA. 2005;294(10):1215–23. doi: 10.1001/jama.294.10.1215. [DOI] [PubMed] [Google Scholar]
- 17.McKeage K, Murdoch D, Goa KL. The sirolimuseluting stent: a review of its use in the treatment of coronary artery disease. Am J Cardiovasc Drugs. 2003;3(3):211–30. doi: 10.2165/00129784-200303030-00007. [DOI] [PubMed] [Google Scholar]
- 18.Kirtane AJ, Gupta A, Iyengar S, et al. Safety and efficacy of drug-eluting and bare metal stents: comprehensive meta-analysis of randomized trials and observational studies. Circulation. 2009;119(25):3198–206. doi: 10.1161/CIRCULATIONAHA.108.826479. [DOI] [PubMed] [Google Scholar]
- 19.Wallace EL, Abdel-Latif A, Charnigo R, et al. Meta-analysis of long-term outcomes for drug-eluting stents versus bare-metal stents in primary percutaneous coronary interventions for ST-segment elevation myocardial infarction. Am J Cardiol. 2012;109(7):932–4. doi: 10.1016/j.amjcard.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 20.Farkouh ME, Domanski M, Sleeper LA, et al. FREEDOM Trial Investigators Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367(25):2375–84. doi: 10.1056/NEJMoa1211585. [DOI] [PubMed] [Google Scholar]
- 21.Serruys PW, Morice MC, Mohr F, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–72. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 22.Head SJ, Davierwala PM, Serruys PW, et al. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J. 2014;35(40):2821–30. doi: 10.1093/eurheartj/ehu213. [DOI] [PubMed] [Google Scholar]
- 23.Verma S, Farkouh ME, Yanagawa B, et al. Comparison of coronary artery bypass surgery and percutaneous coronary intervention in patients with diabetes: a meta-analysis of randomised controlled trials. Lancet Diabetes Endocrinol. 2013;1(4):317–28. doi: 10.1016/S2213-8587(13)70089-5. [DOI] [PubMed] [Google Scholar]
- 24.Farooq V, Serruys PW, Zhang Y, et al. Short-term and long-term clinical impact of stent thrombosis and graft occlusion in the SYNTAX trial at 5 years. J Am Coll Cardiol. 2013;62(25):2360–9. doi: 10.1016/j.jacc.2013.07.106. [DOI] [PubMed] [Google Scholar]
- 25.Gao RL, Xu B, Lansky AJ, et al. Randomised comparison of a novel abluminal groove-filled biodegradable polymer sirolimus-eluting stent with a durable polymer everolimus-eluting stent: clinical and angiographic follow-up of the TARGET I trial. EuroIntervention. 2013;9(1):75–83. doi: 10.4244/EIJV9I1A12. [DOI] [PubMed] [Google Scholar]
- 26.Grube E, Chevalier B, Smits P, et al. The SPIRIT V study: a clinical evaluation of the XIENCE V everolimus-eluting coronary stent system in the treatment of patients with de novo coronary artery lesions. JACC Cardiovasc Interv. 2011;4(2):168–75. doi: 10.1016/j.jcin.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 27.Stone GW, Midei M, Newman W, et al. Randomized comparison of everolimus-eluting and paclitaxel-eluting stents: two-year clinical follow-up from the clinical evaluation of the Xience V everolimus eluting coronary stent system in the treatment of patients with de novo native coronary artery lesions (SPIRIT) III trial. Circulation. 2009;119:680–6. doi: 10.1161/CIRCULATIONAHA.108.803528. [DOI] [PubMed] [Google Scholar]
- 28.Otsuka F, Finn AV, Kolodgie FD, et al. Pathology of second-generation everolimus-eluting stents versus first-generation sirolimus- and paclitaxel-eluting stents in humans. Circulation. 2014;129(2):211–23. doi: 10.1161/CIRCULATIONAHA.113.001790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campos CM, Christiansen EH, Stone GW, Serruys PW. The EXCEL and NOBLE trials: similarities, contrasts and future perspectives for left main revascularization. EuroIntervention. 2015;11(suppl V):V115–9. doi: 10.4244/EIJV11SVA26. [DOI] [PubMed] [Google Scholar]
- 30.Park SJ, Ahn JM, Kim YH, et al. BEST Trial Investigators Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med. 2015;372(13):1204–12. doi: 10.1056/NEJMoa1415447. [DOI] [PubMed] [Google Scholar]
- 31.Chang M, Ahn JM, Lee CW, et al. Long-term mortality after coronary revascularization in nondiabetic patients with multivessel disease. J Am Coll Cardiol. 2016;68(1):29–36. doi: 10.1016/j.jacc.2016.04.034. [DOI] [PubMed] [Google Scholar]
- 32.Fernández-Pereira C, Santaera O, Larribau M, et al. Revascularization strategies for patients with multiple vessel coronary disease and unprotected left main. A prospective, multicenter and controlled Argentina registry with a cobalt-chromium rapamycin eluting stent, FIREBIRD 2™: protocol design and methods of the ERACI IV Registry. Revista Argentina de Cardioangiología Interv. 2014;5(01):0019–25. [Google Scholar]
- 33.Haiek C, Fernández-Pereira C, Santaera O, et al. Second vs. First generation drug eluting stents in multiple vessel disease and left main stenosis: two-year follow-up of the observational, prospective, controlled, and multicenter ERACI IV registry. Catheter Cardiovasc Interv. 2016 Mar 7; doi: 10.1002/ccd.26468. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez AE, Fernandez-Pereira C, Mieres J, Santaera O, Antoniucci D, ERACI IV Investigators Modifying angiographic syntax score according to PCI strategy: lessons learnt from ERACI IV Study. Cardiovasc Revasc Med. 2015;16(7):418–20. doi: 10.1016/j.carrev.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 35.Tonino PA, De Bruyne B, Pijls NH, et al. FAME Study Investigators Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213–24. doi: 10.1056/NEJMoa0807611. [DOI] [PubMed] [Google Scholar]
- 36.De Bruyne B, Fearon WF, FAME 2 Trial Investigators Fractional flow reserve–guided PCI for stable coronary artery disease. N Engl J Med. 2014;371:1208–17. doi: 10.1056/NEJMoa1408758. [DOI] [PubMed] [Google Scholar]
- 37.Fernandez-Pereira C, Mieres J, Rodriguez AE. Long-term mortality after coronary revascularization in nondiabetic patients with multivessel disease: Letter to Editor. J Am CollCardiol. 2016 doi: 10.1016/j.jacc.2016.07.792. In press. [DOI] [Google Scholar]