Abstract
A case is described of motor neurone disease presenting with an ocular motor disorder characterised by saccadic intrusions, impaired horizontal and vertical saccades, and apraxia of eyelid opening. The occurrence of eye movement abnormalities in motor neurone disease is discussed.
KEYWORDS: motor neurone disease, saccadic intrusions, supranuclear gaze palsy
CASE REPORT
A 71-year-old man presented with difficulty opening and moving his eyes. He described a feeling as if his ‘eyes were locked straight ahead’. His visual acuity was 6/9 bilaterally. He had apraxia of lid opening, saccadic intrusions, and difficulty generating horizontal and vertical saccades. However, oculocephalic testing revealed a full range of movement.
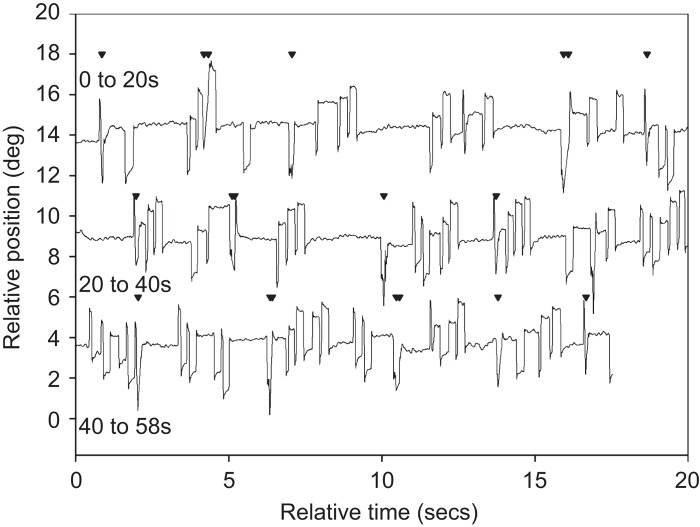
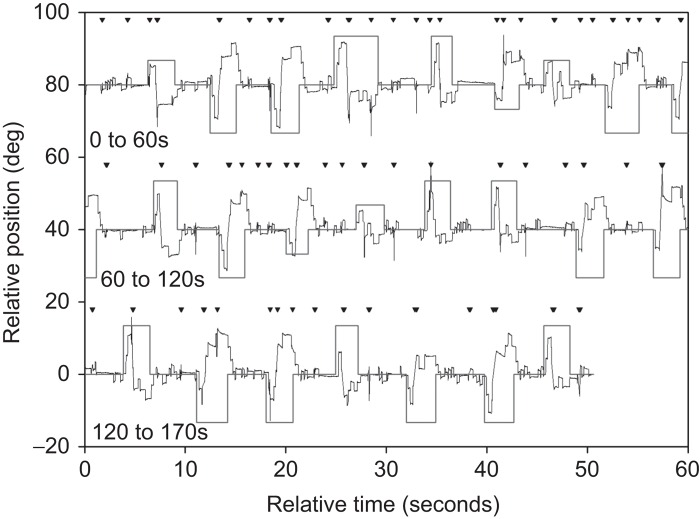
Eye movement recordings (EyelinkII) confirmed frequent square wave saccadic intrusions of 2 degrees amplitude at a frequency of 60 per minute (Figure 1). Vertical and horizontal saccades were hypometric with reduced peak velocity. There was 100% error rate on the anti-saccade test (Figure 2). Smooth pursuit had reduced gain. The vestibulo-ocular reflex (VOR) gain was good at 0.75, but VOR suppression was abnormal at 0.47. The findings were consistent with a supranuclear disorder of ocular motility.
FIGURE 1 .
Central fixation showing frequent saccadic intrusions (triangles represent blinks).
FIGURE 2 .
Anti-saccade test showing 100% error rate and self-correction of anti-saccadic errors.
Over the next 4 months, he developed progressive muscle weakness and wasting. He was noted to have extensive fasciculations of his limbs and trunk muscles at rest. He developed a spastic gait and his reflexes were noted to be exaggerated. He became progressively dysarthric and dysphagic.
Computerised tomographic imaging of the head showed mild generalised cortical atrophy. Electromyography study revealed spontaneous activity and fasciculation potentials in a widespread distribution. Motor units showed only mild re-modelling, sensory nerves were intact, and no conduction block was seen on motor nerve conduction studies.
Our patient had a final clinical diagnosis of motor neurone disease (MND). He did not have fronto-temporal dementia and had an Addenbrooke’s Cognitive Examination score of 93/100. His condition deteriorated and he died of end-stage MND about 6 months after his initial presentation. Consent for autopsy was not given.
COMMENT
This case report illustrates an atypical initial presentation of MND. Eye movements are typically spared in MND until very late in the disease course.1 Significant eye movement abnormalities are generally seen only if survival is artificially prolonged.2 What is unusual in the described case is that a supranuclear gaze palsy was the presenting feature of the illness, pre-dating the typical motor features of MND by several months.
Supranuclear vertical saccadic impairment has been observed in fronto-temporal dementia with MND3; however, our patient had a high Addenbrooke’s Cognitive Examination score and did not meet the criteria for fronto-temporal dementia.
Other disorders, such as Kennedy disease, can mimic MND and abnormal eye movements have been described in Kennedy disease.4 However, our patient had neither the characteristic signs of androgen insufficiency, such as gynaecomastia, nor any tremor and there was no X-linked family history.
The eye movement recordings clearly demonstrate a supranuclear gaze palsy, in particular frequent saccadic intrusions, impaired smooth pursuit, impaired suppression of VOR, and difficulty generating vertical saccades. All of these findings have been previously reported in MND, but not as the presenting features of the disease.5,6
Post-mortem examinations of MND patients with supranuclear vertical gaze palsy have revealed extensive neuronal cell loss in the rostral interstitial nucleus of the medial longitudinal fasciculus (riMLF).7 The riMLF controls the generation of vertical saccade, and the slow vertical saccades could be explained by the pathological changes in the riMLF. Our patient had 100% error rate on the anti-saccade test and the high rate of anti-saccadic errors could also be a hallmark of prefrontal dysfunction.8
Supranuclear gaze palsy has been described in patients with amyotrophic lateral sclerosis.9 However, this is the first report of a supranuclear disorder of ocular motility as a rare initial presentation of MND.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- [1].Kaminski HJ, Richmonds CR, Kusner LL, Mitsumoto H.. Differential susceptibility of the ocular motor system to disease. Ann N Y Acad Sci 2002;956:42–54. [DOI] [PubMed] [Google Scholar]
- [2].Hayashi H, Kato S, Kawada T.. Amyotrophic lateral sclerosis: oculomotor function in patients on respirators. Neurology 1987;37:1431–1432. [DOI] [PubMed] [Google Scholar]
- [3].Moon SY, Lee BH, Seo SW, Kang SJ, Na DI.. Slow vertical saccades in frontotemporal dementia with motor neurone disease. J Neurol 2008;255:1337–1343. [DOI] [PubMed] [Google Scholar]
- [4].Thurtell MJ, Pioro EP, Leigh RJ.. Abnormal eye movements in Kennedy disease. Neurology 2009;72:1528–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Marti-Fàbregas J, Roig C.. Oculomotor abnormalities in motor neuron disease. J Neurol 1993;240:475–478. [DOI] [PubMed] [Google Scholar]
- [6].Shaunak S, Orrell RW, O’Sullivan E, Hawken MB, Lane RJ, Henderson L, Kennard C.. Oculomotor function in amyotrophic lateral sclerosis: evidence for frontal impairment. Ann Neurol 1995;38:38–44. [DOI] [PubMed] [Google Scholar]
- [7].Averbuch-Heller L, Helmchen C, Horn AK, Leigh RJ, Buttner-Ennever JA.. Slow vertical saccades in motor neuron disease: correlation of structure and function. Ann Neurol 1998;44:641–648. [DOI] [PubMed] [Google Scholar]
- [8].Garbutt S, Matlin A, Hellmuth J, Schenk AK, Johnson JK, Rosen H, Dean D, Kramer J, Neuhaus J, Miller BL, Lisberger SG, Boxer AL.. Oculomotor function in frontotemporal lobar degeneration, related disorders and Alzheimer’s disease. Brain 2008;131:1268–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].McCluskey L, Elman L, Martinez-Lage M.. Amyotrophic lateral sclerosis-plus syndrome with TAR DNA-binding protein-43 pathology. Arch Neurol 2009;66:121–124. [DOI] [PMC free article] [PubMed] [Google Scholar]