Abstract
Diagnostic testing is an integral component of patient evaluation in the emergency department (ED). Emergency clinicians frequently use diagnostic testing to more confidently exclude “worst case” diagnoses rather than to determine the most likely etiology for a presenting complaint. Increased utilization of diagnostic testing has not been associated with reductions in disease-related mortality but has led to increased overall healthcare costs and other unintended consequences (e.g., incidental findings requiring further work-up, unnecessary exposure to ionizing radiation or potentially nephrotoxic contrast). Shared decision making (SDM) presents an opportunity for clinicians to discuss the benefits and harms associated with diagnostic testing with patients to more closely tailor testing to patient risk. This article introduces the challenges and opportunities associated with incorporating SDM into emergency care by summarizing the conclusions of the diagnostic testing group at the 2016 Academic Emergency Medicine Consensus Conference on SDM. Three primary domains emerged: 1) characteristics of a condition or test appropriate for SDM; 2) critical elements of and potential barriers to SDM discussions on diagnostic testing; and 3) financial aspects of SDM applied to diagnostic testing. The most critical research questions to improve engagement of patients in their acute care diagnostic decisions were determined by consensus.
INTRODUCTION
Diagnostic testing has classically been perceived as definitively establishing the presence or absence of a discrete disease state. In the emergency department (ED), diagnostic tests are often aimed at “ruling out” rather than “ruling in” disease, and therefore ED diagnostic testing often favors sensitivity over specificity.1,2 The focus on a worst-case scenario, rather than the most likely scenario, has led to increasing rates of diagnostic test utilization in emergency medicine (EM).3 For many conditions,4,5 this increase has not been associated with improved patient outcomes, but may have contributed to higher overall ED treatment costs and other unintended consequences (e.g., incidental findings requiring further work-up, unnecessary exposure to ionizing radiation or potentially nephrotoxic contrast).6
The potential implications of shared decision making (SDM) applied to the use of diagnostic testing in the ED are profound. Reducing inappropriate utilization of advanced imaging is a research and public policy priority. The SDM model provides an alternative to standard diagnostic testing approaches and offers a potential avenue for initiating discussions about when tests should be completed. The SDM mode, as described by Charles et al7 includes four essential components:
At least two participants - clinician and patient (or caregiver)
Both parties share information
Both parties take steps to build a consensus about the preferred approach
An agreement is reached on the approach to implement
The SDM model has been proposed for use within the context of the ED.8–11 While conceptually logical, several unique challenges exist. In a recent survey of emergency physicians, only 56% reported using SDM with their patients. The survey highlighted a number of potential barriers to the effectiveness of SDM in the ED, including: perceptions that patients prefer a unilateral directive approach; concern that patients may opt for overly aggressive approaches; fear of legal liability; time constraints needed to engage patients; and concern for gaps in patient knowledge.12
In this manuscript, we present challenges and opportunities regarding incorporating SDM for diagnostic testing in the ED. We summarize the findings from the consensus conference breakout sessions that focused on the following three domains: 1) characteristics of a condition or test appropriate for SDM; 2) critical elements of and potential barriers to SDM discussions on diagnostic testing; and 3) financial aspects of SDM applied to diagnostic testing. Critically important research questions that must be answered to help advance SDM for acute care diagnostic testing are also described.
These consensus recommendations for future research and policy directives emphasize the critical aspects of the SDM approach that will ultimately empower patients to more actively participate in decisions regarding their own care.
I. WHAT CHARACTERISTICS OF A CONDITION OR TEST MAKE IT APPROPRIATE FOR SDM?
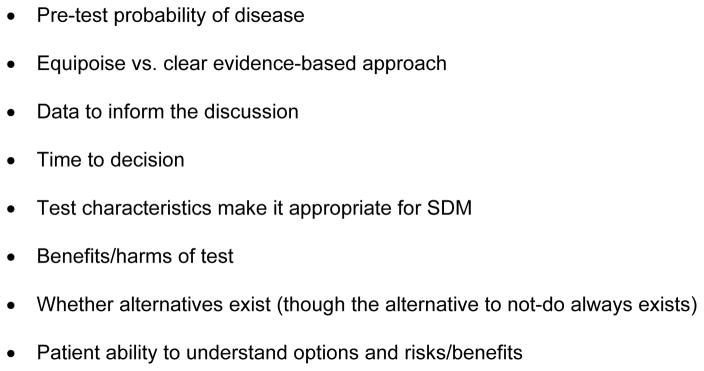
It would be simplistic to think that every decision that a clinician makes can be shared with the patient, and a variety of factors affect whether or not SDM is appropriate. Factors related to the condition or test that can help determine when SDM may or may not be medically reasonable can be summarized in a conceptual approach (Figure 1) based upon the following:
Figure 1.
Conceptual Approach to Determine Appropriateness of SDM for Diagnostic Testing
Pre-test probability of disease
In order to evaluate the appropriateness of SDM for diagnostic testing, one needs to understand the probability that the patient might have the clinical condition being evaluated. Patients at intermediate probability of having the condition being considered are most likely to benefit. Patients at low or high risk are less likely to benefit, unless the test itself is associated with a likelihood ratio that strongly indicates the presence or absence of disease. Of note, there are situations in which the use of a clinical decision rule itself may appropriately involve SDM, and thus the following discussion of “tests” includes the use of decision rules. Discussions below assume that the pre-test probability will be altered by the diagnostic test result. Tests that will not meaningfully alter the pretest probability should not be performed and therefore should not be considered for SDM.
Equipoise
The situation when there is clear-cut evidence suggesting an optimal diagnostic approach is different from the situation when there is equipoise between two or more different diagnostic approaches. As an example, for a 55-year-old patient presenting to the ED with potential acute coronary syndrome, data show no clear difference in patient outcome whether they receive a coronary computed tomography angiogram or observation and subsequent stress test. On the other hand, obtaining an electrocardiogram and troponin in this same patient is standard of care and not a situation where SDM is appropriate. Although the patient may refuse the electrocardiogram and troponin, this would not represent SDM as the physician made a clear evidence-based recommendation.
Data available
The availability of data regarding test performance should probably not affect whether or not SDM is appropriate, but is very important to inform the approach to the SDM conversation. Ideally, patients could be presented with best options based on the performance characteristics of the tests being considered to help inform their decision. When data regarding test performance characteristics are not well known, the SDM conversation may be more difficult, but these situations may have the greatest degree of equipoise.
Time to decision
Some of the most critical decisions in EM need to be made in a time sensitive manner, but this should not be an excuse to avoid SDM. It is well-established that patients can complete a full informed consent process to determine whether or not they want to enroll in a clinical trial that requires medication administration within minutes of arrival in the ED (i.e., stroke, acute myocardial infarction).13 The depth of the SDM conversation may need to be modified based upon the time sensitivity of the decision, but we should not lose sight of the fact that patients should still be engaged as able.
Benefits and harms of testing
The benefits and harms of tests should be considered prior to engaging in SDM. One could argue that if the test had 100% sensitivity and specificity, took 1 minute to complete, was free, would alter outcomes or management, and was not associated with any harms, there would be no reason to engage in SDM. But such a test does not exist. The potential harms of testing can include those specific to the patient (e.g., exposure to ionizing radiation, financial cost to the patient, potential insignificant incidental findings that lead to harmful downstream testing) as well as the potential harms to other patients (e.g., delay in other patients’ access to care) or to the healthcare system at large (e.g., expensive, low-yield tests that contribute to the high-cost of healthcare). The assessment of harms for each patient may vary based on patient characteristics (such as age or pregnancy status as it relates to radiation exposure) and other priorities. Furthermore, if a test has significant potential benefit, SDM may not be necessary.
Existence of alternatives
SDM conversations are designed to take place at times when a decision is needed, often between two or more testing or treatment approaches. Clinicians may not consider SDM an option for situations where there is only one testing option, but in these situations there is still a decision to be made: test or not test.
Patient understanding
A patient’s ability to engage in conversation and to understand the risks and benefits of testing options is essential to effective SDM. The provider must elicit a patient’s clear understanding of risks and benefits during the conversation to ensure patient comprehension. While involvement of a healthcare proxy is appropriate, SDM should not be pursued when a patient (or their proxy) cannot fully comprehend the discussion.
Patient fear
Patients come to the ED because they are concerned about their injury or illness. Research shows that one of their priorities is alleviation of fear and reassurance, which all too often involves some form of diagnostic testing.14,15 Campaigns (e.g., Choosing Wisely16) have identified a number of low value tests to avoid but they do not address the collateral impact of such testing on patient fear. Excessive use of diagnostic testing cannot be effectively addressed until we understand each patient’s motivation for seeking care and develop systems to alleviate their concerns in the absence of diagnostic testing.
Consensus-Derived Highest Priority Research Topics Related to Characteristics of a Condition or Test Make It Appropriate for SDM
Determine how to incorporate new practices or emerging testing/treatments in the setting of an old practice standard.
Define the role of SDM when there is overwhelming evidence that one approach is diagnostically superior to other approaches yet other test characteristics (e.g., invasiveness, cost) affect patient decision-making.
Examine how patient fear and symptom uncertainty impact SDM discussions in the acute care setting.
Explore if there is utility in SDM discussions for situations when there is not enough evidence to have an evidence-based discussion.
Identify the types of diagnostic tests for which patients are most interested in SDM.
II. CRITICAL ELEMENTS OF A SDM DISCUSSION ON DIAGNOSTIC TESTING IN THE ED AND POTENTIAL BARRIERS
Effective communication between patients and physicians involves the bilateral sharing of information, thoughts, and feelings in a manner that is effectively received by both parties.17 Three essential elements must be present for SDM to occur:
Both the health care provider and the patient must recognize and acknowledge that a decision is required;
The patient and clinician must know and understand the best available evidence concerning the risks and benefits of each option; and
Decisions must take into account both the provider’s guidance and the patient’s values and preferences.18
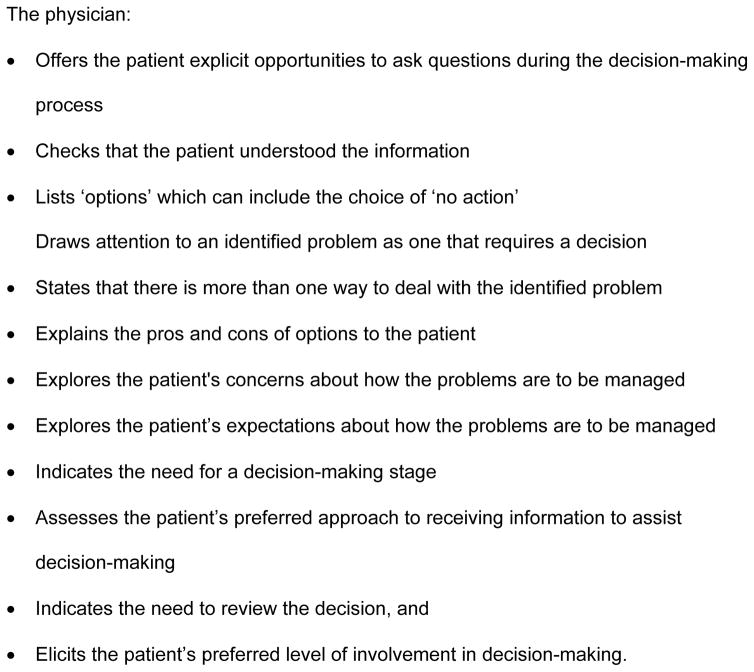
It is critical within a SDM discussion to assess each patient’s desired role and to have effective communication of the relevant information. Potential barriers to effective communication in SDM discussions on diagnostic testing in the ED and suggested approaches to overcome these barriers are discussed below and summarized in Table 1. Understanding the best evidence available requires comprehension of potentially complex information, which may be impacted by patient literacy and numeracy,19,20 as well as by the acuity of the presentation and ED environment. Similarly, incorporation of patient preferences may involve efforts to understand the role of other cultures or languages of patients.21 The most commonly used scale to measure the extent to which clinicians involve patients in decision-making is the “Observing patient involvement in decision-making” (OPTION) scale (Figure 2).22 Clinicians are judged on how well they inform patients about options and consequences; whether they ensure that patients have understood the information; whether they discuss concerns, expectations, and preferences; and how well they guide patients through the decision making process.
Table 1.
Barriers and facilitators of effective communication in SDM discussion on diagnostic testing in the ED
|
|
||
|---|---|---|
| Barriers | Facilitators | |
|
|
||
| Patient characteristics | Being in poor health Cognitive impairments (e.g., dementia, intoxication) |
Limited debility and intact cognition Prior exposure to a similar process |
|
| ||
| Decision characteristics | Significant decisions are a barrier and facilitator Timing relative to the disease course (e.g., will the diagnostic test change management) |
Significant decisions are a barrier and facilitator |
|
| ||
| Interaction Characteristics | Power imbalance in the patient– clinician relationship The desire to be a ‘‘good’’ patient and perceived benefits that might arise (e.g., lack of conflict in the encounter) Perception that there are ‘‘right’’ and ‘‘wrong’’ decisions Perceived unacceptability of asking the physician questions and raising options These barriers are affected by the patient’s cultural background and health literacy. |
Physicians who effectively listen to patients, respect their concerns, and seek to understand individual needs The presence of an advocate or caregiver |
Patient-reported barriers and facilitators to SDM relate to how the healthcare system is organized (i.e., time available, continuity of care, organization of workflow and the setting itself) and to what happens in the ED visit (i.e., predisposing factors such as patient characteristics, interactional influences including the power imbalance between patient and clinician, and SDM encounter and the process itself, including knowledge gain). Most patient-reported barriers and facilitators are potentially modifiable.
Clinician-reported barriers are time, lack of agreement with the applicability of SDM to the patient, and lack of agreement with the applicability of SDM to the clinical situation, suggesting clinicians presume that many patients will not benefit from SDM, or do not wish to take part.
Figure 2.
Observing patient involvement in decision-making (OPTION) scale
Role of literacy and numeracy
Patients need to understand concepts of risk and probability to make informed choices about diagnostic tests and treatment.23–30 Low health literacy and poor comprehension are common and unlikely to be acknowledged by patients. Low literacy is more common in people over age 65, without a high school education, in minority population groups or immigrants, and in patients with chronic diseases.31,32 Patients with lower education, limited health literacy, lower trust in physicians and limited English language proficiency are more likely to report suboptimal SDM.19,20
Compared to those with higher literacy levels, patient with lower literacy ask fewer questions during a medical encounter and are less likely to request additional services or more information.33 Recommendations to improve health communications so that patients can participate in SDM include: assessing literacy (through standardized assessment and clues indicating skills); use of plain language; use of concrete and specific phrases; use of multiple forms of communication, including written, oral, and visual; encouragement of questions from patients; and confirmation of patient comprehension (e.g., teach back). In addition, when providing numeric information, best practices include: expressing probabilities in terms of numbers rather than percentages (e.g., 1 in 20 rather than 5%); keeping the denominator consistent (e.g., do not change between 1 in 10 and 1 in 1000); and avoiding relative risk.
Interventions to improve care and outcomes for patients with limited health literacy include those at the clinician-patient level (e.g., patient-centered communication, clear communication techniques, teach-to-goal methods, and reinforcement), at the system-patient level (e.g., clear health education materials, visual aids, clear medication labeling, self-management support programs, and shame-free clinical environments), and at the community-patient level (e.g., adult education referrals, lay health educators, and harnessing the mass media).34
Role of other cultures and languages
Incorporating a patient’s values and preferences should include an exploration of how the community’s and individual patient's cultural traditions might shape preferences for care. Different tools have been adapted to be applicable to different cultures.35,36 When treating non-English-speaking patients in the absence of a bilingual physician or professional interpreter, the increased potential for miscommunication often leads to conservative decision making and increased use of expensive diagnostic testing.37 Simple, non-medical or layman terms phrases facilitate involvement in the decision-making process.
Role of decision aids
Decision aids can help patients understand and remember the evidence presented in a SDM conversation as well as communicate their personal preferences. Decision aids provide information about the nature of options and their attributes.8,38 Decision aids have been found to increase patient knowledge and engagement in decision making and decrease healthcare utilization when used for SDM conversations in the ED.8 Validated clinical decision rules present emergency physicians with a simplified schematic to engage in SDM about diagnostic testing and several are already routinely used in practice (e.g., NEXUS for cervical spine imaging, PERC rule for pulmonary embolism).1,2
Role of technology
Health technology has been used to implement SDM.39 Computerized aids have the advantage of tailoring information to individual user characteristics, with interactive and advanced visual features to facilitate participant involvement.40 Use of computer-based aids has been found to achieve similar improvement on knowledge of options and outcomes when compared to non-computerized aids. The interactive components, such as self-assessment and feedback modules, significantly improved knowledge and accuracy of risk expectations.40
Consensus-Derived Highest Priority Research Topics Related to Critical Elements of a SDM Discussion on Diagnostic Testing in the ED
Determine what information patients and clinicians should communicate in SDM discussions.
Investigate how patient acuity impacts the assessment of whether SDM is appropriate.
Define the patient's desired role for SDM regarding diagnostic testing in the acute care setting.
Explore methods to assess each patient’s desired level of participation in the SDM process.
Develop approaches to modify SDM discussions in the setting of varying patient health literacy and cultural beliefs.
III. FINANCIAL ASPECTS OF SDM AND DIAGNOSTIC TESTING
Financial considerations and SDM
Previous research suggests that SDM can substantially decrease overall healthcare costs, particularly for conditions with multiple clinically-appropriate treatment options and high practice variability.41,42 For example, one study found that use of SDM in elective orthopedic surgery reduced surgical costs by 12–21%.42
Research on healthcare costs and SDM in the ED has been sparse. In a recent survey of ED patients, 63% had never discussed the cost of ED care with a provider and 17% had concerns about their ability to pay for care.43 None of the patients with a concern about their ability to pay discussed this with their provider. The most common reasons that patients did not initiate a conversation about costs included lack of face-to-face time with the provider, belief that the provider should focus on treatment without considering costs, and a belief that the provider was not the appropriate person at the hospital with whom to discuss costs. Additionally, 27% of patients reported that they did not fill a prescription or did not attend a follow-up appointment due to cost. Among the 24 resident physicians practicing in this ED, 63% considered the cost of care they were delivering at least once per shift, but only 21% discussed costs with patients.44 These findings highlight tremendous opportunity to improve communication about healthcare costs between ED providers and patients. Advanced diagnostic imaging, which includes computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound, accounts for perhaps the greatest costs in the ED other than the costs associated with hospital admission. In fact, advanced diagnostic imaging comprises the bulk of the cost burden of all testing in the ED.45 Moreover, considerable practice variation and overuse of certain advanced imaging modalities make diagnostic testing a prime target for research on SDM in the ED.46 Promising topics for study include methods to safely reduce CT use for minor head trauma, evaluation for pulmonary embolism, and kidney stones.47–49
A SDM approach that includes a clinician-patient discussion about both the medical appropriateness of a test as well as the cost to the patient has the potential to decrease unnecessary testing and improve patient satisfaction with the decision-making process. However, a major barrier to this approach is a lack of knowledge among providers about the cost of specific diagnostic tests to specific patients. Informed discussions about the cost of diagnostic testing would require accessible and accurate information about both total and out-of-pocket costs based on a patient’s healthcare insurance plan. While significant investment would be required to generate and maintain logbooks of the cost for commonly ordered diagnostic tests in the ED, these records could be essential for meaningful discussions with patients about what diagnostic tests to pursue.
Potential financial stakeholders
Financial stakeholders in ED-based SDM may include the following (when applicable): the patient, the insured (parent, spouse, etc.), the insurance carrier, the insured’s employer, the treating physician, other physicians who interpret the test (e.g., radiologist for plain films, CT, MRI; cardiologists for stress imaging studies) and the hospital providing care. In addition to reducing overall healthcare costs, use of SDM to drive down testing may improve ED throughput and increase the overall number of ED patients that a clinician may treat in their shift thus improving efficiency. However, in the current United States (US) health care system, decreasing testing may lower revenue for hospitals and physicians by reducing medical complexity with lower Evaluation and Management codes leading to a reduction in Relative Value Units, and less billing for interpretation of diagnostic tests. This concern will likely be mitigated as we move toward a more value-based health care system.
Role of the payer and influence on decisions
Several other major knowledge and research gaps exist regarding the impact of patient characteristics, patient- clinician relationships, and insurance coverage. For example, a preliminary simulation study suggests that clinician counseling in a neonatal setting varies depending on the race and insurance status of the expectant patient.50 As the number of US patients with high-deductible health plans continues to grow as a result of the Affordable Care Act, there is concern that enrollees with low socioeconomic status may forgo emergency care due to burdensome out-of-pocket costs.51,52 It is possible that patients subject to different insurance with varying copays, deductibles, or bundled-payment plans may make very different choices; the impact of similar factors in the ED setting have not yet been elucidated.
Medicolegal Considerations
The issue of medicolegal concerns related specifically to decisions that are made with SDM arose as an issue of critical importance to the Work Group. It is currently unknown whether decisions made with SDM will be seen as adhering to best clinical practices by the court system. It was also acknowledged, however, that medicolegal concerns are provider-centered, while SDM is patient-centered, and thus medicolegal concerns should not be prioritized in the development and implementation of SDM processes.
Consensus-Derived Highest Priority Research Topics Related to Financial Aspects of SDM and Diagnostic Testing
Identify the primary barriers that limit clinicians’ ability to provide patients with accurate, real-time costs for common diagnostic tests.
Explore potential financial incentives that payers could offer to optimize the use of SDM and decision aids in the acute care setting.
Determine what medicolegal concerns about performing/not performing a diagnostic test impact whether an EM clinician deems SDM appropriate.
Conclusions
SDM presents an opportunity for the provider and patient to discuss the benefits and harms associated with diagnostic testing with a goal of more appropriate test utilization. Three primary domains emerged from the 2016 Academic Emergency Medicine consensus conference diagnostic testing work group: 1) characteristics of a condition or test appropriate for SDM; 2) critical elements and potential barriers of SDM discussions on diagnostic testing; and 3) financial aspects of SDM applied to diagnostic testing. The most critical research questions to improve engagement of patients in their acute care management were determined by consensus and presented.
Acknowledgments
Funding Sources: Drs. Rising and Hollander are supported in part by award ME-1503-28476 from the Patient Centered Outcomes Research Institute (PCORI). Dr. Self is supported in part by NIH K23GM110469. Dr. Brody is supported in part by NIH R01HL127215-01A. Dr. Levy is supported in part by PCORI award FC14-1409-21656, NIH R01MD005849-05, and NIH R01HL127215-01A. Dr. Hess is supported in part by PCORI contracts 952, 12-11-4435, and 0867. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or PCORI. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Appendix
List of Attendees at the May 10, 2016 Diagnostic Testing Breakout Session
| Name and Degree | Institution | |
|---|---|---|
| Lynette Krebs | University of Alberta | lkrebs@valberta.ca |
| Julie Leonard | Nationwide Children's | julie.leonard@nationwidechildrens.org |
| Prashant Mahajan | Childrens Hospital of Michigan | pmahajun@dmi.org |
| Jim Homme | Mayo Clinic | homme.james@mayo.edu |
| Erika Newton | Stony Brook | erika.newton@stonybrookmedicine.edu |
| Sangil Lee | Mayo Clinic | lee.sangil@mayo.edu |
| Wes Self | Vanderbilt | wesley.self@vanderbilt.edu |
| Danielle McCarthy | Northwestern | |
| Iris Reyes | University of Pennsylvania | iris.reyes@uphs.upenn.edu |
| Mira Grieser | PCORI | mgrieser@picori.org |
| Patrick Archambault | University Laval | patrick.m.archambault@gmail.com |
| Melanie Hogg | Carolina Med Center | mhogg@carolinas.org |
| Brent Ruoff | Washington University | ruoffb@wustl.edu |
| Bjorn Westgard | Regions Hospital, St. Paul,Minnesota. | bjorn.westgard@gmail.com |
| Paul Musey | Indiana University | pmusey@iu.edu |
| Joe Miller | Henry Ford | jmiller6@lfhs.org |
| Mike Mouw | University Medical Center Brackenridge, Austin, TX | mmouw@aol.com |
| Jana Anderson | Mayo Clinic | anderson.jana@mayo.edu |
| Elizabeth Schoenfeld | Baystate Med Center | ElizSchoen@gmail.com |
| Errel Uhondpourdo | Baystate Med Center | |
| Toby Magurney | Boston | Tmagurney@partners.org |
| Gail Weingarten | Patient Advocate,Philadelphia, PA | gweig333@comcast.net |
| Kristin Rising | Jefferson | Kristin.Rising@jefferson.edu |
| Philip Levy | Wayne State | apozza@wayne.edu |
| Laura Melville | NYP-Methodist Hosp. | lmelville@mac.com |
| Jefferey Hom | Stony Brook University | jhommdmph@yahoo.com |
| Sean Collins | Vanderbilt | sean.collins@vanderbilt.edu |
| Aaron Brody | Wayne State University | abrody@med.wayne.edu |
| Mike Radeos | NY Presbyterian/Queens | MSR9007@nyp.org |
| Timothy Jang | UCLA | tbj@g.ucla.edu |
| Jennifer Marin | Univ. of Pittsburgh | jennifer.marin@uhp.edu |
| Kenneth Dodd | Hennepin | Kenneth.dodd@gmail.com |
| Tyler Barrett | Vanderbilt | tyler.barrett@vanderbilt.edu |
| M,Fernanda Bellolio, MD, MS | Mayo Clinic | Bellolio.Fernanda@mayo.edu |
| Bjug Borgundvaag, MD | Toronto, Canada | |
Footnotes
Conflicts of Interests/Disclosures: There are no conflicts of interest in connection with this submission nor are there any copyright constraints. No industry financial support or compensation has been or will be received for conducting this study. Barrett: Consultant, Red Bull GmbH, Fuschl am See, Salzburg and Boehringer Ingelheim Pharmaceuticals, Inc. Ridgefield, Connecticut; Research Support as Site Principal Investigator: Janssen Pharmaceuticals, Raritan, NJ; Alere, San Diego, CA; Others: None
Role of the Sponsors: The funding organizations had no role in the design and conduct of the study; the collection, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
References
- 1.Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. NEJM. 2000;343:94–9. doi: 10.1056/NEJM200007133430203. [DOI] [PubMed] [Google Scholar]
- 2.Kline Ja, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772–780. doi: 10.1111/j.1538-7836.2008.02944.x. [DOI] [PubMed] [Google Scholar]
- 3.Kocher KE, Meurer WJ, Fazel R, Scott PA, Krumholz HM, Nallamothu BK. National trends in use of computed tomography in the emergency department. Ann Emerg Med. 2011;58(5):452–462. e3. doi: 10.1016/j.annemergmed.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Korley FK, Pham JC, Kirsch TD. Use of Advanced Radiology During Visits to US Emergency Departments for Injury-Related Conditions, 1998–2007. JAMA. 2010;304(13):1465–1471. doi: 10.1001/jama.2010.1408. [DOI] [PubMed] [Google Scholar]
- 5.Wiener RS, Schwartz LM, Woloshin S. Time Trends in Pulmonary Embolism in the United States: Evidence of Overdiagnosis. Arch Intern Med. 2011;171(9):831–837. doi: 10.1001/archinternmed.2011.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell AM, Jones AE, Tumlin JA, Kline JA. Prospective study of the incidence of contrast-induced nephropathy among patients evaluated for pulmonary embolism by contrast-enhanced computed tomography. Acad Emerg Med. 2012;19(6):618–625. doi: 10.1111/j.1553-2712.2012.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (Or it takes, at least two to tango) Soc Sci Med. 1997;44(5):681–692. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 8.Hess EP, Knoedler MA, Shah ND, et al. The chest pain choice decision aid: a randomized trial. Circ Cardiovasc Qual Outcomes. 2012;5(3):251–9. doi: 10.1161/CIRCOUTCOMES.111.964791. [DOI] [PubMed] [Google Scholar]
- 9.Geyer BC, Xu M, Kabrhel C. Patient preferences for testing for pulmonary embolism in the ED using a shared decision-making model. Am J Emerg Med. 2014;32(3):233–6. doi: 10.1016/j.ajem.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 10.Flynn D, Knoedler Ma, Hess EP, et al. Engaging Patients in Health Care Decisions in the Emergency Department Through Shared Decision-making: A Systematic Review. Acad Emerg Med. 2012;19(8):959–67. doi: 10.1111/j.1553-2712.2012.01414.x. [DOI] [PubMed] [Google Scholar]
- 11.Hess EP, Wyatt KD, Kharbanda AB, et al. Effectiveness of the head CT choice decision aid in parents of children with minor head trauma: study protocol for a multicenter randomized trial. Trials. 2014;15(1):253. doi: 10.1186/1745-6215-15-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanzaria HK, Brook RH, Probst MA, Harris D, Berry SH, Hoffman JR. Emergency physician perceptions of shared decision-making. Acad Emerg Med. 2015;22(4):399–405. doi: 10.1111/acem.12627. [DOI] [PubMed] [Google Scholar]
- 13.Larkin GL, Marco CA, Abbott JT. Emergency determination of decision-making capacity: balancing autonomy and beneficence in the emergency department. Acad Emerg Med. 2001;8(3):282–284. doi: 10.1111/j.1553-2712.2001.tb01307.x. [DOI] [PubMed] [Google Scholar]
- 14.Rising KL, Padrez KA, O’Brien M, et al. Return Visits to the Emergency Department_: The Patient Perspective. Ann Emerg Med. 2015;65(4):377–386. doi: 10.1016/j.annemergmed.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Rising KL, Hudgins A, Reigle M, Hollander JE, Carr BG. “I’m Just a Patient”: Fear and Uncertainty as Drivers of Emergency Department Use in Patients With Chronic Disease. Ann Emerg Med. 2016 doi: 10.1016/j.annemergmed.2016.03.053. In Press. [DOI] [PubMed] [Google Scholar]
- 16.American College of Emergency Physicians. [Accessed May 18, 2016];Choosing Wisely. 2013 Available at: http://www.choosingwisely.org/societies/american-college-of-emergency-physicians/
- 17.Hess EP, Grudzen CR, Thomson R, Raja AS, Carpenter CR. Shared Decision-making in the Emergency Department: Respecting Patient Autonomy When Seconds Count. Acad Emerg Med. 2015;22(7):856–864. doi: 10.1111/acem.12703. [DOI] [PubMed] [Google Scholar]
- 18.Legare F, Witteman HO. Shared decision making: Examining key elements and barriers to adoption into routine clinical practice. Health Aff. 2013;32(2):276–284. doi: 10.1377/hlthaff.2012.1078. [DOI] [PubMed] [Google Scholar]
- 19.Barton JL, Koenig CJ, Evans-Young G, et al. The design of a low literacy decision aid about rheumatoid arthritis medications developed in three languages for use during the clinical encounter. BMC Med Inform Decis Mak. 2014;14(1):104. doi: 10.1186/s12911-014-0104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barton JL, Trupin L, Tonner C, et al. English language proficiency, health literacy, and trust in physician are associated with shared decision making in rheumatoid arthritis. J Rheumatol. 2014;41(7):1290–1297. doi: 10.3899/jrheum.131350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: A systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 22.Elwyn G, Edwards A, Wensing M, Hood K, Atwell C, Grol R. Shared decision making: developing the OPTION scale for measuring patient involvement. Qual Saf Heal Care. 2003;12(2):93–99. doi: 10.1136/qhc.12.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Health literacy: Report of the Council on Scientific Affairs. JAMA. 1999;281(6):552–557. [PubMed] [Google Scholar]
- 24.Kripalani S, Paasche-Orlow MK, Parker RM, Saha S. Advancing the field of health literacy. JGIM. 2006;21(8):804–805. [Google Scholar]
- 25.Weiss BD, Coyne C. Communicating with patients who cannot read. NEJM. 1997;337(4):272–273. doi: 10.1056/NEJM199707243370411. [DOI] [PubMed] [Google Scholar]
- 26.Schillinger D, Grumbach K, Piette J, et al. Association of Health Literacy With Diabetes Outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 27.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165(17):1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 28.Peterson PN, Shetterly SM, Clarke CL, et al. Health Literacy and Outcomes Among Patients With Heart Failure. JAMA. 2011;305(16):1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low Health Literacy and Health Outcomes_: An Updated Systemic Review. Ann Intern Med. 2014;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 30.Weiss B, Blanchard J, McGee D, et al. Illiteracy among Medicaid recipients and its relationship to health care costs. J Heal Care Poor Underserved. 1994;5(2):99–111. doi: 10.1353/hpu.2010.0272. [DOI] [PubMed] [Google Scholar]
- 31.Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy. Washington, DC: 2006. [Google Scholar]
- 32.Institute of Medicine Committee on Health Literacy. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004. [Accessed May 15, 2016]. Available at: http://www.nap.edu/download.php?record_id=10883. [Google Scholar]
- 33.Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior during the medical encounter: A mixed-methods analysis. J Gen Intern Med. 2007;22(6):782–786. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sudore RL, Schillinger D. Interventions to Improve Care for Patients with Limited Health Literacy. J Clin Outcomes Manag. 2009;16(1):20–29. [PMC free article] [PubMed] [Google Scholar]
- 35.Jull J, Giles A, Minwaashin Lodge TAWSC, Boyer Y, Stacey D. Cultural adaptation of a shared decision making tool with Aboriginal women: a qualitative study. BMC Med Inform Decis Mak. 2015;15:10. doi: 10.1186/s12911-015-0129-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jull J, Stacey D, Giles A, Boyer Y. Shared decision-making and health for First Nations, Métis and Inuit women: a study protocol. BMC Med Inform Decis Mak. 2012;12(1):146–155. doi: 10.1186/1472-6947-12-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hampers LC, McNulty JE. Professional Interpreters and Bilingual Physicians in a Pediatric Emergency Department. Arch Pediatr Adolesc Med. 2002;156(11):1108–1113. doi: 10.1001/archpedi.156.11.1108. [DOI] [PubMed] [Google Scholar]
- 38.Stacey D, Légaré F, Nf C, et al. Decision aids for people facing health treatment or screening decisions (Review) Cochrane Database Syst Rev 2014. 2014;(1) doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 39.Elwyn G, Légaré F, van der Weijden T, Edwards A, May C. Arduous implementation: does the Normalisation Process Model explain why it’s so difficult to embed decision support technologies for patients in routine clinical practice. Implement Sci. 2008;3(57) doi: 10.1186/1748-5908-3-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheehan J, Sherman KA. Computerised decision aids: A systematic review of their effectiveness in facilitating high-quality decision-making in various health-related contexts. Patient Educ Couns. 2012;88(1):69–86. doi: 10.1016/j.pec.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 41.O’Connor AM, Wennberg JE, Legare F, et al. Toward The “Tipping Point”: Decision Aids And Informed Patient Choice. Health Aff. 2007;26(3):716–725. doi: 10.1377/hlthaff.26.3.716. [DOI] [PubMed] [Google Scholar]
- 42.Arterburn D, Wellman R, Westbrook E, et al. Introducing decision aids at group health was linked to sharply lower hip and knee surgery rates and costs. Health Aff. 2012;31(9):2094–2104. doi: 10.1377/hlthaff.2011.0686. [DOI] [PubMed] [Google Scholar]
- 43.Gilbert S, Wen L. Qualitative Study: Cost of Emergency Care From the Patients’ Perspective. Ann Emerg Med. 2015;66(4):S131. [Google Scholar]
- 44.Gilbert SK, Wen L. Qualitative Study: Cost of Emergency Care From the Providers’ Perspective. Ann Emerg Med. 2015;66(4):S97–S98. [Google Scholar]
- 45.Venkatesh AK, Schuur JD. A “Top Five” list for emergency medicine: A policy and research agenda for stewardship to improve the value of emergency care. Am J Emerg Med. 2013;31(10):1520–1524. doi: 10.1016/j.ajem.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 46.Kanzaria HK, Hall MK, Moore CL, Burstin H. Emergency Department Diagnostic Imaging: The Journey to Quality. Acad Emerg Med. 2015;22(12):1380–1384. doi: 10.1111/acem.12817. [DOI] [PubMed] [Google Scholar]
- 47.Marin JR, Weaver MD, Barnato AE, Yabes JG, Yealy DM, Roberts MS. Variation in emergency department head computed tomography use for pediatric head trauma. Acad Emerg Med. 2014;21(9):987–995. doi: 10.1111/acem.12458. [DOI] [PubMed] [Google Scholar]
- 48.Kindermann DR, McCarthy ML, Ding R, et al. Emergency department variation in utilization and diagnostic yield of advanced radiography in diagnosis of pulmonary embolus. J Emerg Med. 2014;46(6):791–799. doi: 10.1016/j.jemermed.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 49.Wong HJ, Sistrom CL, Benzer TI, et al. Use of Imaging in the Emergency Department: Physicians Have Limited Effect on Variation. Radiology. 2013;268(3):779–789. doi: 10.1148/radiol.13130972. [DOI] [PubMed] [Google Scholar]
- 50.Edmonds BT, McKenzie F, Fadel WF, et al. Using Simulation to Assess the Influence of Race and Insurer on Shared Decision-making in Periviable Counseling. Simul Heal. 2014;9(6):353–359. doi: 10.1097/SIH.0000000000000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wharam JF, Zhang F, Landon BE, Soumerai SB, Ross-Degnan D. Enrollees in high-deductible plans reduced high-severity emergency care. Health Aff. 2013;32(8):1398–1406. doi: 10.1377/hlthaff.2012.1426. [DOI] [PubMed] [Google Scholar]
- 52.Lee EO, Ezekiel, Emanuel J. Shared Decision-Making to Improve Care and Reduce Costs. N Engl J Med. 2013;368(1):6–8. doi: 10.1056/NEJMp1209500. [DOI] [PubMed] [Google Scholar]