Abstract
Introduction:
Recently, Salmonella enterica serovar Poona caused a multistate outbreak, with 245 out of 907 cases occurring in California. We report a comparison of pulsed-field gel electrophoresis (PFGE) results with whole genome sequencing (WGS) for genotyping of Salmonella Poona isolates.
Methods:
CA Salmonella Poona isolates, collected from July to August 2015, were genotyped by PFGE using XbaI restriction enzyme. WGS was done using Nextera XT library kit with 2x300 bp or 2x250 bp sequencing chemistry on the Illumina MiSeq Sequencer. Reads were mapped to the de novo assembled serovar Poona draft genome (48 contigs, N50= 223,917) from the outbreak using CLCbio GW 8.0.2. The phylogenetic tree was generated based on hqSNPs calling. Genomes were annotated with CGE and PHAST online tools. In silico MLST was performed using the CGE online tool.
Results:
Human (14) and cucumber (2) Salmonella Poona isolates exhibited 3 possibly related PFGE patterns (JL6X01.0018 [predominant], JL6X01.0375, JL6X01.0778). All isolates that were related by PFGE also clustered together according to the WGS. One isolate with a divergent PFGE pattern (JL6X01.0776) served as an outlier in the phylogenetic analysis and substantially differed from the outbreak clade by WGS. All outbreak isolates were assigned to MLST sequence type 447. The majority of the outbreak-related isolates possessed the same set of Salmonella Pathogenicity Islands with few variations. One outbreak isolate was sequenced and analyzed independently by CDC and CDPH laboratories; there was 0 SNP difference in results. Additional two isolates were sequenced by CDC and the raw data was processed through CDPH and CDC analysis pipelines. Both data analysis pipelines also generated concordant results.
Discussion:
PFGE and WGS results for the recent CA Salmonella enterica serovar Poona outbreak provided concordant assignment of the isolates to the outbreak cluster. WGS allowed more robust determination of genetic relatedness, provided information regarding MLST-type, pathogenicity genes, and bacteriophage content. WGS data obtained independently at two laboratories showed complete agreement.
Keywords: Outbreak, phylogenetic analysis, pulsed-field gel electrophoresis, Salmonella serovar Poona, whole-genome sequencing
The Study
Salmonella enterica serotype Poona is a relatively rare serotype in the United States, responsible for about 1% of reported human Salmonella cases1. Salmonella Poona outbreaks are commonly attributed to farm-produced crops and goods2. Serotype Poona has also caused outbreaks associated with pet reptile exposure3. Recently, Salmonella Poona caused a multistate outbreak, with 245 out of 907 cases occurring in California. A multistate investigation identified imported cucumbers distributed by Company A as the likely source of the outbreak4. We report results of a real-time comparison of pulsed-field gel electrophoresis (PFGE) and whole genome sequencing (WGS) for this Salmonella Poona outbreak investigation.
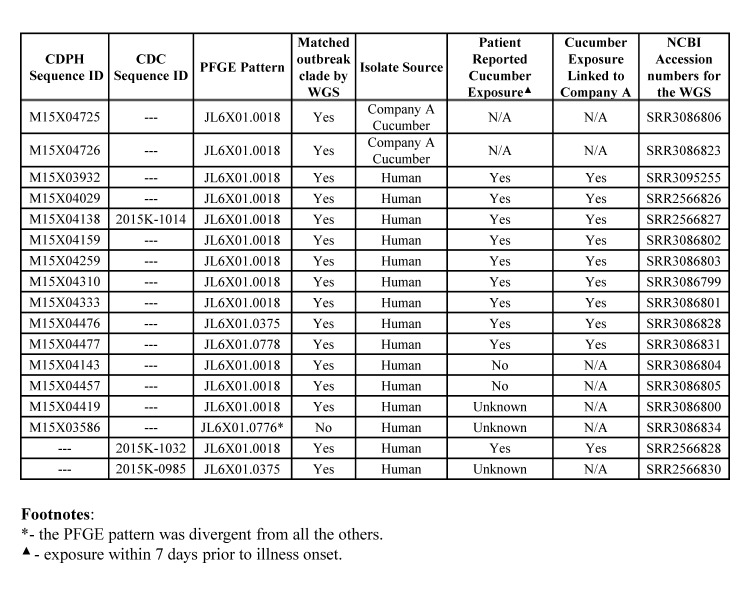
The Salmonella Poona isolates from California analyzed in this study are listed in Table 1. At the California Department of Public Health (CDPH), PFGE was performed using XbaI macrorestriction per PulseNet USA protocol5. For WGS, DNA libraries were prepared using Nextera XT kit (Illumina Inc., San Diego, CA) and sequenced with 2x300 bp or 2x250 bp chemistry on the Illumina MiSeq at 49-124x sequencing coverage (see NCBI accession numbers for the corresponding sequences in Table 1). Time-to-results was 4 days for PFGE and 7 days for WGS. The analysis of sequencing data at CDPH was performed as follows:
Table 1.Salmonella enterica serotype Poona isolates, California (N=17): pulsed-field gel electrophoresis (PFGE) profiles, whole genome sequencing (WGS)-based clustering, and patient-reported cucumber exposure.
Genomes were annotated with prokka v1.1 tool6, the Center for Genomic Epidemiology (CGE), and Phage Search Tool (PHAST) online resources7,8. In silico multi-locus sequence typing (MLST) was performed using the CGE online tool9 against the 7-gene MLST database of University of Warwick (http://mlst.warwick.ac.uk/mlst/dbs/Senterica). The Salmonella Pathogenicity Islands (SPI) were characterized using SPIFinder 1.0 CGE tool (https://cge.cbs.dtu.dk/services/SPIFinder/).
Paired-end reads were mapped to the de novo assembled outbreak Salmonella Poona M15X04725 draft genome (48 contigs, N50= 223,917) using CLCbio Genomic Workbench 8.0.2 (Qiagen, Aarhus, Denmark). Genes of mobile and prophage elements in the reference Salmonella Poona M15X04725 genome were annotated using prokka v1.1 and PHAST tools and consequently masked from mapping in CLCbio Genomic Workbench 8.0.2. SNPs were then called in coding and non-coding genome areas using SAMtools mpileup (v.1.2;10) and converted into VCF matrix using bcftools (v0.1.19; http://samtools.github.io/bcftools/). Variants were parsed using vcftools (v.0.1.12b;11) to include only high-quality SNPs (hqSNPs) with minimum position coverage ≥30x and minimum quality of the base > 200 (--min-meanDP 30; --minQ 200), with InDels and the heterozygote calls excluded. The Maximum Likelihood phylogenetic tree was generated based on hqSNPs calls under the Jukes-Cantor nucleotide substitution model; with 100 bootstrap replicates.
At the US Centers for Disease Control and Prevention (CDC) LyveSET 1.1.4 SNP calling pipeline (http://www.github.com/lskatz/lyve-SET) was applied with reads trimmed using fastx_trimmer 5 bases from 5’ ends before mapping single-end by SMALT. SNPs were called using Varscan at > 20x coverage, > 95% read support, and ≥5 bp apart. The draft assembly of FDA00009409 from the outbreak (38 contigs) was used as a reference without prophage masking.
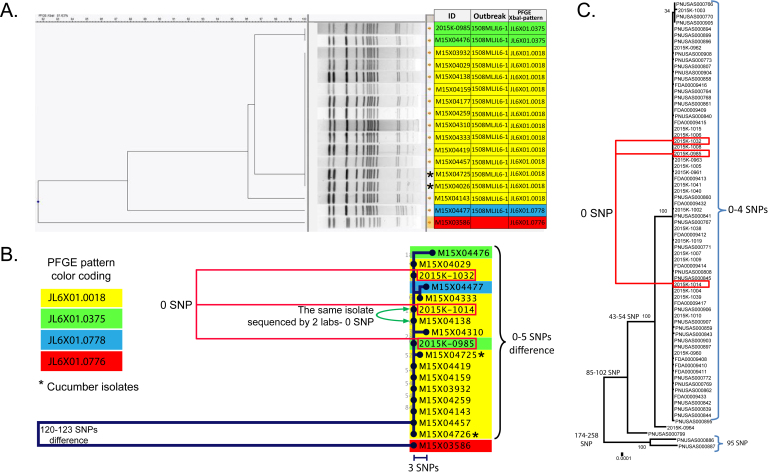
Fourteen human and two cucumber Salmonella Poona isolates analyzed in this study exhibited 3 possibly related PFGE patterns (JL6X01.0018 [predominant], JL6X01.0375, JL6X01.0778). The isolates were selected to include representatives of the three above mentioned PFGE patterns and epidemiologically representative isolates with and without links to the cucumber source. In the interest of the cost effectiveness, the WGS was limited to 16 isolates since the detected PFGE patterns were rare in California and only few SNP differences were found among the sampled isolates. Of the 14 case-patients whose isolates were analyzed, 10 (71%) reported consuming cucumbers during the week preceding their illness onsets, 2 case-patients denied consuming any cucumbers, and cucumber exposure was unknown for 2 case-patients (Table 1. The cucumber exposures reported by the 10 case-patients were all linked to Company A. One isolate (M15X03586) with a divergent PFGE pattern (JL6X01.0776) served as an outlier in the phylogenetic analysis (Table 1, Figure 1A). Cucumber exposure for the patient was unknown; the patient was not considered part of the outbreak cluster based on PFGE.
Phylogeny of Salmonella enterica serovar Poona based on single nucleotide polymorphism (SNP) differences discovered between the isolates by whole genome sequencing (WGS) vs. phylogeny based on PFGE profiles clustering.
A- Pulsed-field gel electrophoresis (PFGE) dendrogram of the California isolates; B- Maximum likelihood tree generated by California Department of Public Health (CDPH) for California outbreak isolates. Background coloring designates PFGE pattern. Red boxes designate sequences generated by CDC; C- Maximum likelihood tree generated by Centers for Disease Control and Prevention (CDC) for multistate investigation, including California. Red boxes designate selected isolates from California.
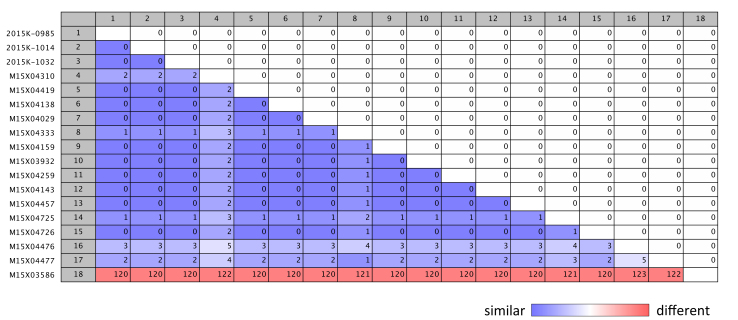
Pairwise comparison of single nucleotide polymorphism (SNP) differences between Salmonella Poona isolates from California.
All 16 isolates that were highly similar by PFGE also clustered together according to WGS. WGS of cucumber isolates showed close relatedness to the genomes of human isolates, with only 0-3 SNPs difference (Figure 1B, 2). The isolate with the divergent PFGE pattern JL6X01.0776 was substantially different (120-123 hqSNPs) from the outbreak clade by WGS (Figure 1A vs. 1B). One outbreak isolate M15X04138 was sequenced and analyzed independently by CDC and CDPH laboratories; no SNP differences in sequences were detected. Two additional isolates were sequenced by CDC, and the raw data was processed through CDPH and CDC analysis pipelines. Both data analysis pipelines generated the same results (Figure 1B vs. 1C).
All outbreak isolates were assigned to the MLST sequence type 447 (ST447). The divergent outgroup strain had a single mutation in hemD gene locus, which did not correspond to any known allele in the MLST database. There was only one entry of ST447 in MLST database; Salmonella strain 3854/83 isolated in 1982 from a wild rodent in India.
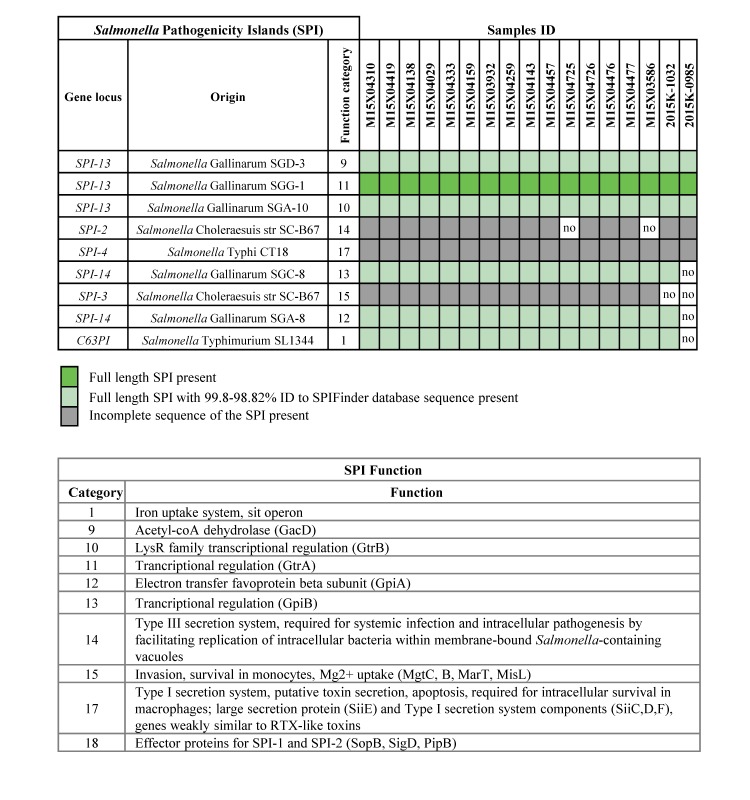
The majority of the outbreak-related isolates possessed the same set of Salmonella Pathogenicity Islands (SPI), with variability mostly caused by the absence of SPI-2 or SPI-3, which encode Type III secretion system and invasion functions, respectively (Table 2).
Table 2.Salmonella Pathogenicity Islands in outbreak-related Salmonella Poona isolates.
All isolates possessed phage elements homologous to Salmonella phage Fels-1 (NC_010391) and partial Enterobacteria phage P4 (NC_001609). Four isolates harbored the genes homologous to an additional bacteriophage of either of the following types: Synechococcus phage S-SKS1 (NC_020851), Ectocarpus siliculosus virus 1 (NC_002687), Enterobacteria phage ES18 (NC_006949), or Enterobacteria phage P1 (NC_005856). Interestingly, phage genes found in one of the isolates were homologous to S-SKS1 bacteriophage, which was described as a virus infecting Synechococcus, a genus of Cyanobacteria known to be one of the predominant prokaryotic components of the oceans’ picophytoplankton12. Another isolate possessed genes homologous to EsV-1 bacteriophage, characterized previously as a bacteriophage of the marine filamentous brown algae Ectocarpus siliculosus13. The sequences identified as incomplete S-SKS1 or EsV-1 phages were integrated into the larger contigs with clear Salmonella identity according to BLAST search. The marine phage-like sequences were also common in other Salmonella enterica serotypes found in NCBI database and seem to represent a part of the Salmonella accessory genome.
WGS has proven to be a powerful tool for the investigation of outbreaks caused by Salmonella enterica, providing great epidemiological concordance and higher resolution than PFGE, the traditional method for Salmonella strain subtyping14,15,16. In our study, WGS confirmed the genetic relatedness of strains with similar PFGE patterns. Outbreak-related isolates exhibited 3 PFGE patterns which complicated assignment of the isolates to a single outbreak source. Particularly, isolate M15X04477 with the pattern JL6X01.0778 differed by 3 bands from the predominant outbreak PFGE-type, thus introducing a higher degree of uncertainty regarding the inclusion of this isolate in the outbreak cluster even though the epidemiologic information supported a possible link to the outbreak. WGS, on the other hand, showed unambiguous clustering of all epidemiologically-related isolates together and clarified genetic relatedness of M15X04477 to the other outbreak isolates. Two case-patients denying cucumber consumption also clustered with the outbreak, which could be explained by possible secondary transmission, cross-contamination of other foods, poor food history recall, or case-patients’ not noticing cucumbers as part of a multi-ingredient meal such as a salad or a sandwich. In support of the high reproducibility of the method, the results of WGS performed by two different laboratories were identical. Additionally, WGS provided information about the MLST sequence type and acquired components of the genome, allowing for more comprehensive characterization of the isolates. Though MLST usually provides poor resolution between Salmonella strains, it is helpful for understanding the global epidemiology of infectious clones17. Diversity in accessory genes of the studied isolates demonstrates the plasticity of the Salmonella Poona genome which is potentially responsible for variations in PFGE patterns that do not necessarily reflect the phylogenetic distance between the isolates18. Since the loss/acquisition of mobile elements does not affect genome-wide SNPs calling, it explains higher evolutionary congruence of WGS-inferred phylogeny compared with PFGE. Noteworthy, WGS results were acquired in 7 working days from the time of pure culture reception by the laboratory. Our experience suggests that WGS can be used for routine epidemiological subtyping.
Conclusions
Real-time PFGE and WGS genotyping results from this Salmonella Poona outbreak provided concordant assignment of isolates to the outbreak cluster by both methods. However, the WGS allowed for a more unequivocal determination of the genetic relatedness of the isolates than PFGE. WGS provided additional information regarding MLST type, pathogenicity genes, and bacteriophage content of the isolates. WGS data obtained independently at two laboratories showed complete agreement.
Data Availability Statement
The raw reads for sequenced here samples were submitted to NCBI SRA archive under accession numbers SRR2566826- SRR2566828, SRR2566830, SRR3086799- SRR3086806, SRR3086823, SRR3086828, SRR3086831, SRR3086834, SRR3095255 (see Table 1 for details).
Competing Interest Statement
The authors have declared that no competing interests exist.
Corresponding Authors
Vishnu Chaturvedi: Vishnu.Chaturvedi@cdph.ca.gov
Varvara K. Kozyreva: Varvara.Kozyreva@cdph.ca.gov
Acknowledgments
We acknowledge colleagues in Food & Waterborne Diseases and Immunodiagnostics & Parasitic Sections of CDPH Microbial Disease Laboratory Branch, particularly Francine Arroyo, Katherine Trinh, Frank Ni, and Greg Inami for processing and identification of bacterial cultures. We thank the CDPH Infectious Diseases Branch, and particularly Dr. Duc Vugia for the critical review of this work. We acknowledge valuable assistance from the CDPH Food and Drug Branch (Michael Needham, Amber Barnes, Samantha Mauldin, Brandon Adcock), and the California local health departments, particularly County of San Diego Health and Human Services Agency (Azarnoush Maroufi, Eric C. McDonald, Jessica Healy, Brian Murphy, Loreto N. Negado) and County of San Diego Department of Environmental Health (Heather Buonomo, Cory Neiss).
Biographies
Dr. Varvara Kozyreva is a research scientist at the Microbial Disease Laboratory Branch of the California Department of Public Health. She serves as a scientific lead for the whole-genome sequencing laboratory involved in outbreak investigations.
Dr. Jeniffer Concepción-Acevedo is the PulseNet International coordinator at CDC, Atlanta, GA, USA. She completed a PhD in Microbiology from the University of Massachusetts, Amherst where she studied the mechanisms of mitochondrial DNA replication in African trypanosomes as a potential target for new antitrypanosomal drugs. During her postdoctoral training at Emory University, she investigated the impact of bacterial antibiotic resistance on antimicrobial pharmacodynamics and treatment outcomes. At CDC, she works collaboratively with international partners towards laboratory systems strengthening and implementation of molecular subtyping tools. Dr. Concepción-Acevedo is interested in supporting national and international initiatives to build laboratory capacity for the investigation and detection of foodborne disease outbreaks.
Funding Statement
The authors received no specific funding for this work.
Contributor Information
Varvara K. Kozyreva, California Department of Public Health, Richmond, CA, USA
John Crandall, California Department of Public Health, Richmond, CA, USA.
Ashley Sabol, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Alyssa Poe, California Department of Public Health, Richmond, CA, USA.
Peng Zhang, California Department of Public Health, Richmond, CA, USA.
Jeniffer Concepción-Acevedo, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Morgan N. Schroeder, Centers for Disease Control and Prevention, Atlanta, GA, USA
Darlene Wagner, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Jeffrey Higa, California Department of Public Health, Los Angeles, CA, USA.
Eija Trees, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Vishnu Chaturvedi, California Department of Public Health, Richmond, CA, USA.
References
- 1.Centers for Disease Control and Prevention. Multistate outbreaks of Salmonella serotype Poona infections associated with eating cantaloupe from Mexico—United States and Canada, 2000–2002. MMWR Morb Mortal Wkly Rep. 2002;51:1044–7. [PubMed]
- 2.Jackson BR, Griffin PM, Cole D, Walsh KA, Chai SJ: Outbreak-associated Salmonella enterica serotypes and food Commodities, United States, 1998-2008. Emerging infectious diseases 2013, 19(8):1239-1244. [DOI] [PMC free article] [PubMed]
- 3.Walters MS, Simmons L, Anderson TC, DeMent J, Van Zile K, Matthias LP, Etheridge S, Baker R, Healan C, Bagby R et al: Outbreaks of Salmonellosis From Small Turtles. Pediatrics 2016, 137(1). [DOI] [PubMed]
- 4.Multistate Outbreak of Salmonella Poona Infections Linked to Imported Cucumbers (Final Update) [http://www.cdc.gov/salmonella/poona-09-15/index.html] [DOI] [PMC free article] [PubMed]
- 5.Ribot EM, Fair MA, Gautom R, Cameron DN, Hunter SB, Swaminathan B, Barrett TJ: Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne pathogens and disease 2006, 3(1):59-67. [DOI] [PubMed]
- 6.Seemann T (2014) Prokka: rapid prokaryotic genome annotation. Bioinformatics 30: 2068-2069. [DOI] [PubMed]
- 7.Joensen KG, Scheutz F, Lund O, Hasman H, Kaas RS, et al. (2014) Real-time whole-genome sequencing for routine typing, surveillance, and outbreak detection of verotoxigenic Escherichia coli. J Clin Microbiol 52: 1501-1510. [DOI] [PMC free article] [PubMed]
- 8.Zhou Y, Liang Y, Lynch KH, Dennis JJ, Wishart DS (2011) PHAST: a fast phage search tool. Nucleic Acids Res 39: W347-352. [DOI] [PMC free article] [PubMed]
- 9.Larsen MV, Cosentino S, Rasmussen S, Friis C, Hasman H, et al. (2012) Multilocus sequence typing of total-genome-sequenced bacteria. J Clin Microbiol 50: 1355-1361. [DOI] [PMC free article] [PubMed]
- 10.Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, et al. (2009) The Sequence Alignment/Map format and SAMtools. Bioinformatics 25: 2078-2079. [DOI] [PMC free article] [PubMed]
- 11.Danecek P, Auton A, Abecasis G, Albers CA, Banks E, et al. (2011) The variant call format and VCFtools. Bioinformatics 27: 2156-2158. [DOI] [PMC free article] [PubMed]
- 12.Mann NH (2003) Phages of the marine cyanobacterial picophytoplankton. FEMS Microbiol Rev 27: 17-34. [DOI] [PubMed]
- 13.Delaroque N, Muller DG, Bothe G, Pohl T, Knippers R, et al. (2001) The complete DNA sequence of the Ectocarpus siliculosus Virus EsV-1 genome. Virology 287: 112-132. [DOI] [PubMed]
- 14.Deng X, Shariat N, Driebe EM, Roe CC, Tolar B, et al. (2015) Comparative analysis of subtyping methods against a whole-genome-sequencing standard for Salmonella enterica serotype Enteritidis. J Clin Microbiol 53: 212-218. [DOI] [PMC free article] [PubMed]
- 15.Scaltriti E, Sassera D, Comandatore F, Morganti M, Mandalari C, et al. (2015) Differential single nucleotide polymorphism-based analysis of an outbreak caused by Salmonella enterica serovar Manhattan reveals epidemiological details missed by standard pulsed-field gel electrophoresis. J Clin Microbiol 53: 1227-1238. [DOI] [PMC free article] [PubMed]
- 16.Taylor AJ, Lappi V, Wolfgang WJ, Lapierre P, Palumbo MJ, et al. (2015) Characterization of Foodborne Outbreaks of Salmonella enterica Serovar Enteritidis with Whole-Genome Sequencing Single Nucleotide Polymorphism-Based Analysis for Surveillance and Outbreak Detection. J Clin Microbiol 53: 3334-3340. [DOI] [PMC free article] [PubMed]
- 17.Sabat AJ, Budimir A, Nashev D, Sa-Leao R, van Dijl J, et al. (2013) Overview of molecular typing methods for outbreak detection and epidemiological surveillance. Euro Surveill 18: 20380. [DOI] [PubMed]
- 18.Gurtler V, Mayall BC (2001) Genomic approaches to typing, taxonomy and evolution of bacterial isolates. Int J Syst Evol Microbiol 51: 3-16. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw reads for sequenced here samples were submitted to NCBI SRA archive under accession numbers SRR2566826- SRR2566828, SRR2566830, SRR3086799- SRR3086806, SRR3086823, SRR3086828, SRR3086831, SRR3086834, SRR3095255 (see Table 1 for details).