Abstract
Dens invaginatus is a rare anatomic variation that is found primarily in maxillary lateral incisors. The management of dens invaginatus is challenging for clinicians; diagnosing the type of malformation, choosing the most appropriate treatment, and carrying out treatment are complicated by the intricate root system of these teeth. The following case report describes the diagnosis and treatment planning of dens invaginatus Type 3 after cone-beam computed tomography evaluation.
Keywords: Cone-beam computed tomography, C-shaped canal, dens invaginatus
INTRODUCTION
Dens invaginatus is an anatomic variation that has been described as a “tooth within a tooth” because it is a developmental defect resulting from the involution of the crown before calcification has occurred. Dens invaginatus is observed primarily in maxillary lateral incisors, and the prevalence ranges between 0.3% and 10%.[1]
Dens invaginatus is challenging to treat because of the complex root canal system.
The most commonly used classification of invaginated teeth was published by Oehlers in 1957.[2]
Several treatments have been suggested in literature, including endodontic treatment of the invagination alone or along with the main canal, surgical treatment, or removal of the entire tooth.[3,4,5,6,7,8,9,10,11,12]
Cone-beam computed tomography (CBCT) is a three-dimensional (3D) radiographic technique that is useful for various endodontic applications, such as the diagnosis and treatment of teeth with complex or abnormal root canal anatomy.[9,13,14]
The aim of this case report is to describe how CBCT was used for diagnosing, treatment planning, and successfully managing a complex dens invaginatus case with endodontic therapy.
CASE REPORT
A 22-year-old male was referred by his dentist to the Department of Endodontics at the Oral Maxillofacial Medical Center in Tel Hashomer due to the abnormal anatomy of tooth 12.
The patient reported a history of frequent episodes of pain (at the time, he was unable to chew or bite food, and the tooth was tender when touched).
The oral examination and the evaluation of the patient's periodontal status revealed a good oral hygiene. A composite filling was detected on the palatal aspect of the crown and an orthodontic splint retained teeth 13–23 [Figure 1]. Periodontal probing revealed pocket depths of less than 3 mm, and there was no excess mobility of the tooth. The tooth was sensitive to percussion and palpation and did not respond to a cold thermal test (Endo Ice, Coltene Whaldent Inc.; Cuyahoga Falls, OH, USA). The adjacent teeth responded positively to a cold test, and there was no excess mobility or sensitivity to palpation or percussion.
Figure 1.

Tooth 12-preoperative periapical radiograph
Radiographic examination revealed that tooth 12 presented with dens invaginatus and had an associated apical radiolucency extending from the distal aspect of tooth 12 to the mesial aspect of tooth 13. The size of the radiolucency was over 20 mm, and the apical border was not visible on the film [Figure 1].
Due to the irregular anatomy of the tooth, the patient was referred for a CBCT examination to visualize the exact morphology of the tooth and to clarify the size and the exact borders of the radiolucent area.
Cross-sectional and longitudinal CBCT (Carestream 9300, France) slices revealed that the invagination extended along the entire root length. The invagination was embedded into the mesial wall of the root canal on the coronal third, and the main canal partly surrounded the invagination in a C-shaped form. In the middle third, the invagination was detached from the root dentin, and the main canal surrounded the invagination. In the apical third, two separate canals were observed [Figure 2].
Figure 2.
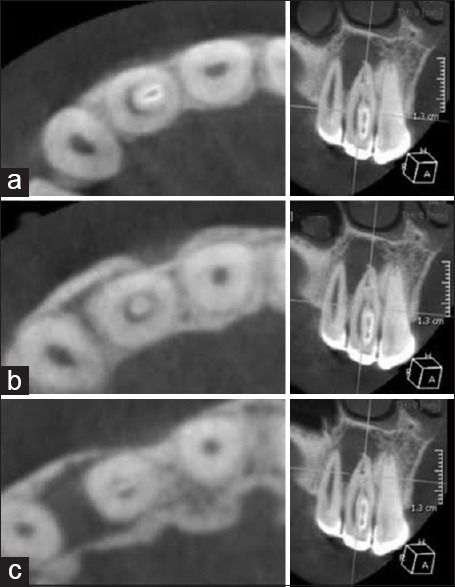
Cone-beam computed tomography. Sagittal and coronal sections: (a) coronal third, (b) middle third, and (c) apical third
The 3D lesion size was 9.73 mm × 9.49 mm × 13.9 mm [Figure 3]. The lesion bordered the floor of the nasal cavity and the mesial aspect of tooth 13, and the lesion penetrated into the cortical plates of the palatal and buccal bone.
Figure 3.
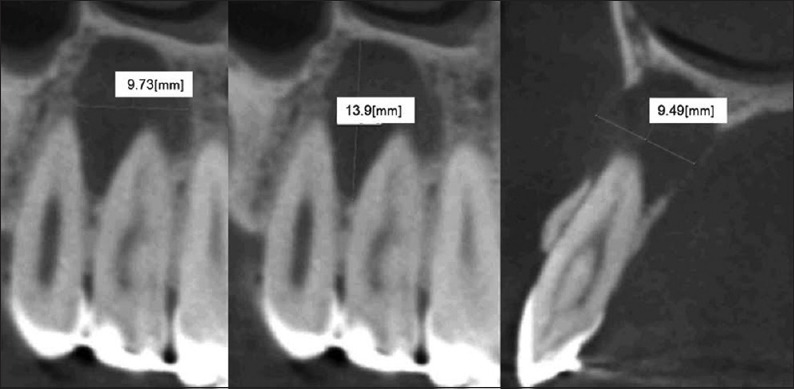
Cone-beam computed tomography for 3-dimentional measurement of the lesion
Based on the clinical and radiographic examination, the following diagnosis was made: Pulpal Necrosis, Symptomatic Apical Periodontitis, and Dens Invaginatus Type 3.[2]
During the first appointment, the tooth was isolated with a rubber dam, and a lingual access cavity was prepared under a surgical operating microscope (Carl Zeiss Surgical GmbH, Oberkochen, Germany) based on the CBCT evaluation as a guide. The first step was to gain access to the location of the invagination by carefully cleaning the lingual pit [Figure 4a]. The second step was to enter the main C-shaped canal with a buccodistal angular approach [Figure 4b]. Necrotic tissue was detected in both the invaginated canal and the main canal. The working length was predetermined by CBCT[15] and confirmed with an electronic apex locator (Dentaport ZX, Morita, Tokyo, Japan) and a radiograph [Figure 5].
Figure 4.
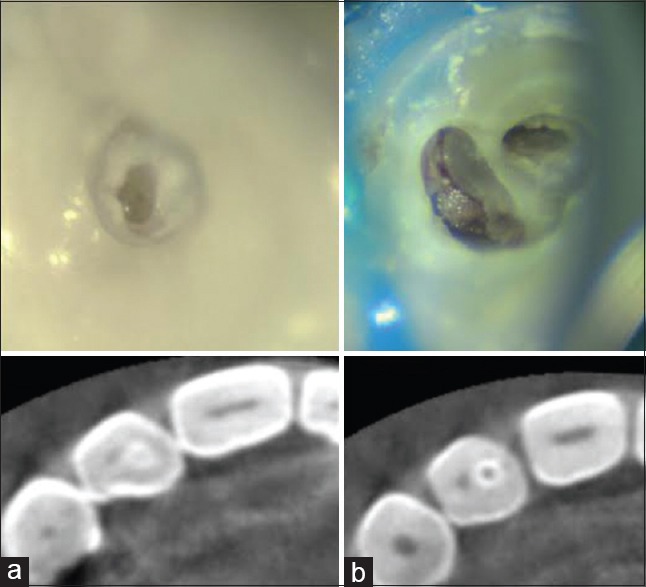
Clinical photographs and cone-beam computed tomography sagittal sections: (a) access to dens, (b) main C-shaped canal
Figure 5.
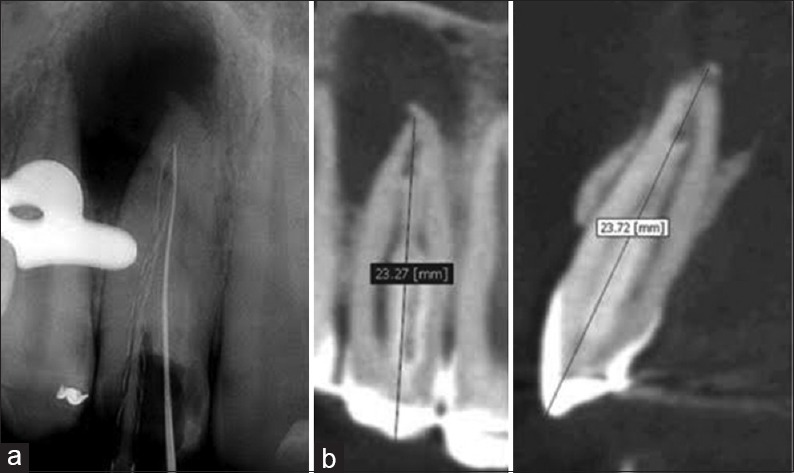
Working length determination: (a) periapical radiograph, (b) preliminary cone-beam computed tomography examination
Biomechanical preparation of the narrow, invaginated canal was performed with nickel-titanium (NiTi) rotary instruments, G-Files (G1, G2, Micro-Mega, Besançon, France), Revo-S files (Micro-Mega, Besançon, France), and irrigated with 3% sodium hypochlorite (NaOCl). The main C-shaped canal was prepared with a Self-Adjusting File (SAF) 1.5-mm file (ReDent-Nova, Ra'anana, Israel) and irrigated with 3% NaOCl using the special VATEA irrigation pump (ReDent-Nova, Ra'anana, Israel) with an irrigant flow of 4 ml/min.[16]
Final irrigation was performed with 17% ethylene diamine tetra-acetic acid (EDTA) and a creamy, aqueous calcium hydroxide dressing was placed in the canals with a spiral Lentulo. The access cavity was temporized with Cavit (ESPE, Seefeld, Germany) and IRM (Caulk, DeTrey Dentsply, Saint-Quentin-Yvelines, France).
At the second appointment (2 weeks later), clinical symptoms had disappeared. After removing the calcium hydroxide with copious irrigation of NaOCl using the SAF,[17] final irrigation with 17% EDTA was performed. Both canals were dried and obturated with a combination technique: Cold lateral compaction of Gutta-percha in the apical third using NiTi finger spreaders (Dentsply Maillefer, Ballaigues, Switzerland) and warm compaction in the middle and coronal thirds with B&;L Alpha (B&L Biotech, Gunpo, Korea) and Machtou pluggers (Dentsply Maillefer, Ballaigues, Switzerland). AH Plus (Dentsply Maillefer, Ballaigues, Switzerland) was used as a sealer. The access cavity was temporized with the EQUIA glass ionomer (GC America, Alsip, IL., USA) [Figure 6a].
Figure 6.
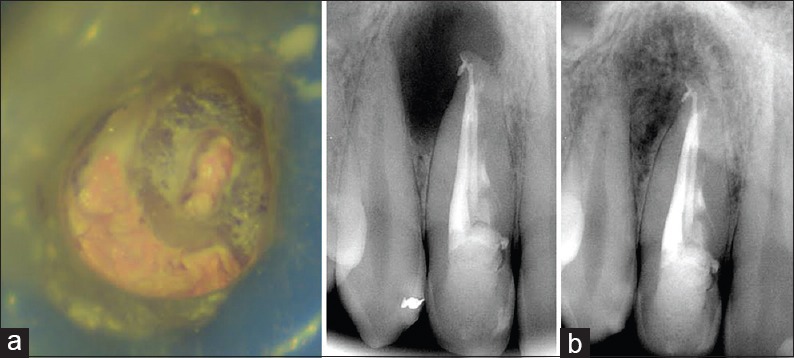
(a) postoperative clinical photograph and periapical radiograph, (b) 24-month follow-up
A follow-up examination at 24 months revealed that the tooth was clinically asymptomatic, lacked tenderness to percussion and palpation, had normal mobility, and lacked deep pockets on probing. Radiographic examination revealed a reduction in the size of the lesion [Figure 6b].
DISCUSSION
Dens invaginatus is challenging to treat because of the complex root canal system. Dens invaginatus creates abnormal anatomy in a tooth and primarily occurs in lateral maxillary incisors and occasionally in premolars.[18,19]
Treatment options for dens invaginatus include prophylactic treatments, endodontic treatment of the invaginated canal alone or along with the main canal, surgical treatment, or removal of the entire tooth.[3,4,5,6,7,8,9,10,11,12]
CBCT enables a 3D evaluation of teeth with complex or abnormal root canal anatomy.[9,13,14] Visualizing the exact anatomy of the root canal can influence treatment decisions and lead to more appropriate treatment plans. Follow-up examinations do not include CBCT because of the as low as reasonably achievable principle.
In this case report, CBCT enabled a 3D visualization of the abnormal anatomy and showed that the invagination occupied most of the canal. In the coronal third of the canal, the invagination was embedded into the mesial wall, while in the middle third, the invagination was detached from the root dentin and the main canal surrounded the entire invagination. Therefore, complete removal of the invagination was impossible. Moreover, removal of the invaginated portion might have biomechanical consequences, such as weakening the tooth structure because of the loss of healthy dentin.[20,21] The main canal of the tooth and the canal created by the invagination followed the entire length and varied in their cross-sectional outlines: The main canal was C-shaped and the invagination created a narrow, round canal. After reviewing all of the findings, we elected to perform conservative, orthograde endodontic therapy in both the invaginated portion and the main C-shaped canal with different instrumentation: The SAF for the C-shaped canal[16] and NiTi rotary instruments for the narrow, round pseudocanal.
The subsequent warm compaction technique forced the obturation material into the area surrounding the invaginated portion in the middle third of the main canal, which was observed in the final radiograph. Our assumption was that the necrotic tissue in this area was dissolved by the synergistic effect of NaOCl with the SAF, followed by a calcium hydroxide dressing.[22,23,24,25,26,27,28,29]
CONCLUSION
This report describes the management of dens invaginatus Type 3 with a 3D CBCT evaluation to guide the treatment planning and clinical decision-making process for this complex, anatomical variation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alani A, Bishop K. Dens invaginatus. Part 1: Classification, prevalence and aetiology. Int Endod J. 2008;41:1123–36. doi: 10.1111/j.1365-2591.2008.01468.x. [DOI] [PubMed] [Google Scholar]
- 2.Oehlers FA. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10:1204–18. doi: 10.1016/0030-4220(57)90077-4. [DOI] [PubMed] [Google Scholar]
- 3.Holtzman L. Conservative treatment of supernumerary maxillary incisor with dens invaginatus. J Endod. 1998;24:378–80. doi: 10.1016/S0099-2399(98)80139-8. [DOI] [PubMed] [Google Scholar]
- 4.De Sousa SM, Bramante CM. Dens invaginatus: Treatment choices. Endod Dent Traumatol. 1998;14:152–8. doi: 10.1111/j.1600-9657.1998.tb00830.x. [DOI] [PubMed] [Google Scholar]
- 5.Tsurumachi T, Hayashi M, Takeichi O. Non-surgical root canal treatment of dens invaginatus type 2 in a maxillary lateral incisor. Int Endod J. 2002;35:310–4. [PubMed] [Google Scholar]
- 6.Creaven J. Dens invaginatus-type malformation without pulpal involvement. J Endod. 1975;1:79–80. doi: 10.1016/S0099-2399(75)80087-2. [DOI] [PubMed] [Google Scholar]
- 7.Kulild JC, Weller RN. Treatment considerations in dens invaginatus. J Endod. 1989;15:381–4. doi: 10.1016/S0099-2399(89)80078-0. [DOI] [PubMed] [Google Scholar]
- 8.Skoner JR, Wallace JA. Dens invaginatus: Another use for the ultrasonic. J Endod. 1994;20:138–40. doi: 10.1016/S0099-2399(06)80060-9. [DOI] [PubMed] [Google Scholar]
- 9.Kfir A, Telishevsky-Strauss Y, Leitner A, Metzger Z. The diagnosis and conservative treatment of a complex type 3 dens invaginatus using cone beam computed tomography (CBCT) and 3D plastic models. Int Endod J. 2013;46:275–88. doi: 10.1111/iej.12013. [DOI] [PubMed] [Google Scholar]
- 10.Vier-Pelisser FV, Pelisser A, Recuero LC, Só MV, Borba MG, Figueiredo JA. Use of cone beam computed tomography in the diagnosis, planning and follow up of a type III dens invaginatus case. Int Endod J. 2012;45:198–208. doi: 10.1111/j.1365-2591.2011.01956.x. [DOI] [PubMed] [Google Scholar]
- 11.Munavalli A, Kambale S, Ramesh S, Ajgaonkar N. Mandibular first molar with single root and single root canal. J Conserv Dent. 2015;18:346–8. doi: 10.4103/0972-0707.159757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Da Silva Neto UX, Hirai VH, Papalexiou V, Gonçalves SB, Westphalen VP, Bramante CM, et al. Combined endodontic therapy and surgery in the treatment of dens invaginatus type 3: Case report. J Can Dent Assoc. 2005;71:855–8. [PubMed] [Google Scholar]
- 13.Durack C, Patel S. The use of cone beam computed tomography in the management of dens invaginatus affecting a strategic tooth in a patient affected by hypodontia: A case report. Int Endod J. 2011;44:474–83. doi: 10.1111/j.1365-2591.2011.01866.x. [DOI] [PubMed] [Google Scholar]
- 14.Patel S. The use of cone beam computed tomography in the conservative management of dens invaginatus: A case report. Int Endod J. 2010;43:707–13. doi: 10.1111/j.1365-2591.2010.01734.x. [DOI] [PubMed] [Google Scholar]
- 15.Jeger FB, Janner SF, Bornstein MM, Lussi A. Endodontic working length measurement with preexisting cone-beam computed tomography scanning: A prospective, controlled clinical study. J Endod. 2012;38:884–8. doi: 10.1016/j.joen.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 16.Solomonov M, Paqué F, Fan B, Eilat Y, Berman LH. The challenge of C-shaped canal systems: A comparative study of the self-adjusting file and ProTaper. J Endod. 2012;38:209–14. doi: 10.1016/j.joen.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 17.Topçuoglu HS, Düzgün S, Ceyhanli KT, Akti A, Pala K, Kesim B. Efficacy of different irrigation techniques in the removal of calcium hydroxide from a simulated internal root resorption cavity. Int Endod J. 2015;48:309–16. doi: 10.1111/iej.12316. [DOI] [PubMed] [Google Scholar]
- 18.Al Omari F, Al-Omari IK. Cleft lip and palate in Jordan: Birth prevalence rate. Cleft Palate Craniofac J. 2004;41:609–12. doi: 10.1597/03-034.1. [DOI] [PubMed] [Google Scholar]
- 19.Tagger M. Nonsurgical endodontic therapy of tooth invagination. Report of a case. Oral Surg Oral Med Oral Pathol. 1977;43:124–9. doi: 10.1016/0030-4220(77)90362-0. [DOI] [PubMed] [Google Scholar]
- 20.Sornkul E, Stannard JG. Strength of roots before and after endodontic treatment and restoration. J Endod. 1992;18:440–3. doi: 10.1016/S0099-2399(06)80845-9. [DOI] [PubMed] [Google Scholar]
- 21.Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J Endod. 2014;40:1160–6. doi: 10.1016/j.joen.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 22.Hasselgren G, Olsson B, Cvek M. Effects of calcium hydroxide and sodium hypochlorite on the dissolution of necrotic porcine muscle tissue. J Endod. 1988;14:125–7. doi: 10.1016/S0099-2399(88)80212-7. [DOI] [PubMed] [Google Scholar]
- 23.Türkün M, Cengiz T. The effects of sodium hypochlorite and calcium hydroxide on tissue dissolution and root canal cleanliness. Int Endod J. 1997;30:335–42. doi: 10.1046/j.1365-2591.1997.00085.x. [DOI] [PubMed] [Google Scholar]
- 24.Wadachi R, Araki K, Suda H. Effect of calcium hydroxide on the dissolution of soft tissue on the root canal wall. J Endod. 1998;24:326–30. doi: 10.1016/S0099-2399(98)80128-3. [DOI] [PubMed] [Google Scholar]
- 25.Andersen M, Lund A, Andreasen JO, Andreasen FM. In vitro solubility of human pulp tissue in calcium hydroxide and sodium hypochlorite. Endod Dent Traumatol. 1992;8:104–8. doi: 10.1111/j.1600-9657.1992.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 26.De-Deus G, Barino B, Marins J, Magalhães K, Thuanne E, Kfir A. Self-adjusting file cleaning-shaping-irrigation system optimizes the filling of oval-shaped canals with thermoplasticized gutta-percha. J Endod. 2012;38:846–9. doi: 10.1016/j.joen.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 27.Siqueira JF, Jr, Alves FR, Almeida BM, de Oliveira JC, Rôças IN. Ability of chemomechanical preparation with either rotary instruments or self-adjusting file to disinfect oval-shaped root canals. J Endod. 2010;36:1860–5. doi: 10.1016/j.joen.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 28.Wu MK, Kast’áková A, Wesselink PR. Quality of cold and warm gutta-percha fillings in oval canals in mandibular premolars. Int Endod J. 2001;34:485–91. doi: 10.1046/j.1365-2591.2001.00463.x. [DOI] [PubMed] [Google Scholar]
- 29.Metzger Z, Zary R, Cohen R, Teperovich E, Paqué F. The quality of root canal preparation and root canal obturation in canals treated with rotary versus self-adjusting files: A three-dimensional micro-computed tomographic study. J Endod. 2010;36:1569–73. doi: 10.1016/j.joen.2010.06.003. [DOI] [PubMed] [Google Scholar]


