Abstract
Background:
The prognostic values of the coronary computed tomography angiography (CCTA) score for predicting future cardiovascular events have been previously demonstrated in numerous studies. However, few studies have used the rich information available from CCTA to detect functionally significant coronary lesions. We sought to compare the prognostic values of Gai's plaque score and the coronary artery calcium score (CACS) of CCTA for predicting functionally significant coronary lesions, using fractional flow reserve (FFR) as the gold standard.
Methods:
We retrospectively analyzed 107 visually assessed significant coronary lesions in 88 patients (mean age, 59.6 ± 10.2 years; 76.14% of males) who underwent CCTA, invasive coronary angiography, and invasive FFR measurement. An FFR <0.80 indicated hemodynamically significant coronary stenosis. Lesions were divided into two groups using an FFR cutoff value of 0.80. We compared Gai's plaque scores and CACS between the two groups and evaluated the correlations of these scores with FFR. The statistical methods included unpaired t-test, Mann-Whitney U-test, and Spearman's correlation coefficients.
Results:
Coronary lesions with FFR <0.80 had higher Gai's scores than those with FFR ≥0.80. Gai's score had the strongest correlation with FFR (r = −0.48, P < 0.01) and had a greater area under the curve = 0.72 (95% confidence interval: 0.61–0.82; P < 0.01) than the CACS of whole arteries and a single artery.
Conclusions:
Both CACS in a single artery and Gai's plaque score demonstrated a good capacity to assess functionally significant coronary artery stenosis when compared to the gold standard FFR. However, Gai's plaque score was more predictive of FFR <0.80. Gai's score can be easily calculated in daily clinical practice and could be used when considering revascularization.
Keywords: Computed Tomography Coronary Angiography, Coronary Calcification, Coronary Stenosis, Fractional Flow Reserve
Introduction
Coronary computed tomography angiography (CCTA) is now a mainstream, well-established cardiac diagnostic imaging modality with widespread acceptance and applications, predicting cardiovascular adverse events.[1,2,3,4,5] In clinical practice, lesions with a stenosis diameter of ≥50% on CCTA are generally considered for referral to invasive coronary angiography (ICA) examination. However, a lesion's severity judged with either CCTA or ICA is often inaccurate for identifying functionally significant coronary lesions that can cause ischemia, which should be further assessed by fractional flow reserve (FFR).[6,7] Stress myocardial computed tomography (CT) perfusion imaging and FFR-CT are new noninvasive methods that may overcome the mismatch between anatomy and function in cardiac imaging, but their use is currently limited because of increased costs and radiation exposure.[8,9,10]
Several scores that can be estimated based on routine evaluation with coronary CT, such as the coronary artery calcium score (CACS) and Gai's CCTA plaque score, have been developed for clinical use,[1,11,12,13] but few studies have evaluated whether these scores are associated with FFR. The present study sought to compare the ability of these CCTA scores to evaluate functional ischemia in patients with significant stenosis, using FFR as the gold standard.
Methods
Study population
We retrospectively evaluated data from patients who underwent both CCTA and ICA and a subsequent measurement of FFR at People's Liberation Army General Hospital from June 2012 to June 2016. Both sexes were included. The sample included 88 patients. The decision to measure FFR was based on the visual assessment of ICA results and was made at the discretion of the interventional cardiologist. Exclusion criteria were poor image quality and patients with prior coronary bypass surgery, acute ST elevation myocardial infarction, previous percutaneous coronary intervention, unstable hemodynamics, left ventricular ejection fraction <30%, and/or atrial fibrillation. Poor image quality was defined as severe motion artifacts or poor contrast opacification. The study protocol was approved by the Ethics Committee of the People's Liberation Army General Hospital. All patients gave written informed consent for both CCTA and ICA.
Coronary computed tomography angiography scanning protocol and image analysis
All patients were examined using a second-generation dual-source CCTA scanner (Somatom Definition Flash, Siemens Medical Solutions, Forchheim, Germany). If the heart rate of a patient was higher than 65 beats/min, up to 50 mg of esmolol was administered intravenously immediately before scanning. If systolic blood pressure was >100 mmHg (1 mmHg = 0.133 kPa), nitroglycerin was administered sublingually just before image acquisition. The patients underwent image acquisition in the electrocardiogram (ECG)-triggered sequential scan mode, retrospective ECG-gated spiral scan mode, or high-pitch spiral scan mode, as appropriate. The CT angiographic scan parameters were 64.0 mm × 2.0 mm × 0.6 mm collimation with a Z-flying focal spot for both detectors, gantry rotation time of 280 milliseconds, tube current of 370 mA, and tube voltage of 100 or 120 kV. A 60–90 ml bolus of high-concentration contrast (370 mg/ml, Ultravist; Bayer Schering Pharma AG, Germany) was administered intravenously at 5 ml/s, followed by a 50 ml injection of saline at the same injection rate. The bolus-tracking technique was used to initiate the scan.
Coronary calcium was quantified by the CACS based on a noncontrast-enhanced sequential scan and evaluated with a commercially available software package (Siemens Calcium Score, Siemens, Erlangen, Germany).
Two experienced observers, a radiologist and a cardiologist who were blinded to ICA and FFR findings, evaluated CCTA data on a Syngo Multimodality Workstation (Siemens Medical Solutions, Forchheim, Germany) using volume rendering, multiplanar reformation, and maximum intensity projection. In image analyses, all patients’ vessels were identified and analyzed using a modified classification. Each segment was assessed for diameter, location, presence of atherosclerotic changes (calcified, noncalcified, or mixed), and concomitant coronary artery stenosis. Coronary stenosis was classified as significant if it had a diameter stenosis (DS) over 50% on the longitudinal images.[1]
Gai's coronary computed tomography angiography plaque score
Gai's CCTA plaque score was calculated using the methods described in a previous study.[12,13] The calculations were as follows: (1) minor plaque, 1 point: plaque was definitely visible as a thin layer with a low-density shadow and the estimated stenosis was <30%; (2) moderate plaque, 2 points: a thick layer of low-density plaque was visible and the estimated stenosis was 30–75%; (3) severe localized stenosis, 3 points: plaque was highly stenotic (>75%) and was of low density; (4) erosive plaque, 5 points: plaque was of low or ultra-low density and showed multiple features, including calcification, severe localized stenosis, long lesions of 20 mm or more and involving more than two segments, ulceration, and craters; (5) calcification, 1 point: irrespective of its extensiveness; (6) drug-eluting stent, 5 points; (7) plaque with positive remodeling, 3 points; (8) complete occlusion, 3 points; and (9) diffuse moderate lesions, 2 points. Unlike other CCTA scores, Gai's plaque score can calculate individual vessels, but we only assessed the vessel that had also been assessed by FFR.
Fractional flow reserves measurement protocol
A PressureWire Certus (St. Jude Medical, MN, USA) pressure wire was used to measure FFR. The pressure sensor was placed distal to the stenosis, an adequate hyperemic stimulus was given, and maximal myocardial hyperemia was induced by continuous intravenous infusion of adenosine triphosphate at an infusion rate of 140 μg·kg−1·min−1 for at least 2 min. FFR was calculated as the ratio of the mean distal pressure measured by the pressure wire divided by the mean proximal pressure measured by the guiding catheter. FFR <0.80 indicated hemodynamically significant coronary stenosis.[14,15]
Statistical analysis
All data analyses were performed using SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were expressed as frequencies and percentages and compared using Chi-squared test, and continuous variables were expressed as mean ± standard deviation (SD) or as medians (interquartile ranges) in time intervals and compared using the unpaired t-test or Mann-Whitney U-test. Spearman's correlation coefficients were used to correlate the score data with FFR. The population was further divided into two groups using an FFR cutoff value of 0.80. Receiver operating characteristic (ROC) curves and the derived area under the curves (AUC; C-statistic) were then generated to evaluate the ability of the CCTA-derived scoring systems to detect functional ischemia (FFR <0.80). Two-sided P < 0.05 was considered statistically significant.
Results
Study population
In total, we retrospectively analyzed 107 significant coronary lesions from 88 patients (mean age, 59.6 ± 10.2 years; 76.14% of males) who underwent CCTA, ICA, and invasive FFR measurement. Baseline characteristics are shown in Table 1.
Table 1.
Baseline characteristics of all patients who underwent both CCTA and ICA (n = 88)
| Characteristics | Data |
|---|---|
| Male sex | 67 (76.14) |
| Age (years) | 59.6 ± 10.2 |
| Diabetes mellitus | 34 (38.64) |
| Hypertension | 59 (67.05) |
| Dyslipidemia | 34 (38.64) |
| Current smoking | 37 (42.01) |
| Prior myocardial infarction | 5 (5.68) |
| CACS of whole arteries | 281.70 ± 464.56 |
| Total cholesterol (mmol/L) | 4.24 ± 1.36 |
| LDL cholesterol (mmol/L) | 2.12 ± 0.82 |
| Fasting blood glucose (mmol/L) | 5.38 ± 0.52 |
| Coronary lesions measured by FFR | |
| One | 67 (76.14) |
| Two | 20 (22.73) |
| Three | 1 (1.14) |
Data are presented as n (%) or mean ± SD. CCTA: Coronary computed tomography angiography; ICA: Invasive coronary angiography; CACS: Coronary artery calcium score; LDL: Low-density lipoprotein; FFR: Fractional flow reserve; SD: Standard deviation.
Lesion characteristics and coronary computed tomography angiography scores
The 107 significant coronary lesions were divided into two groups according to the FFR value. The FFR was <0.80 in 31 coronary lesions (28.97%). Coronary lesions with FFR <0.80 had higher Gai's scores than did those with FFR ≥0.80, while the CACS for single artery and plaque characteristics was not significantly different between the two groups [Table 2].
Table 2.
CCTA scores and lesion characteristics stratified by FFR value
| Items | All patients (n = 107) | FFR ≥0.80 (n = 76) | FFR <0.80 (n = 31) | Statistics | P |
|---|---|---|---|---|---|
| FFR | 0.82 ± 0.09 | 0.86 ± 0.05 | 0.71 ± 0.08 | 11.71* | <0.01 |
| Gai’s score | 4.84 ± 2.36 | 4.32 ± 2.12 | 6.13 ± 2.43 | −3.84* | <0.01 |
| Calcium score (single artery) | 134.72 ± 218.41 | 114.07 ± 203.47 | 185.35 ± 247.64 | −1.54* | 0.13 |
| Calcified plaque | 8 (7.48) | 6 (7.89) | 2 (6.45) | 0.02† | 0.88 |
| Noncalcified plaque | 29 (27.10) | 23 (30.26) | 6 (19.35) | 1.79† | 0.18 |
| Mixed plaque | 70 (65.42) | 47 (61.84) | 23 (74.19) | 0.00† | 0.95 |
Data are presented as n (%) or mean ± SD. *t value; †χ2 value. P values are from comparisons between patients with FFR ≥0.80 and <0.80. CCTA: Coronary computed tomography angiography; FFR: Fractional flow reserve; SD: Standard deviation.
Correlation between coronary computed tomography angiography scores and fractional flow reserve
The correlation of CCTA scores with FFR was evaluated. Of these scores, the correlation between Gai's score and FFR was stronger than that between FFR and CACS of whole arteries and a single artery (r = −0.48, P < 0.01) [Figure 1]. The FFR was modestly correlated with CACS of a single artery (r = −0.23, P = 0.02) [Figure 2]. In contrast, there was no correlation between FFR value and CACS of whole arteries (r = −0.19, P = 0.10).
Figure 1.
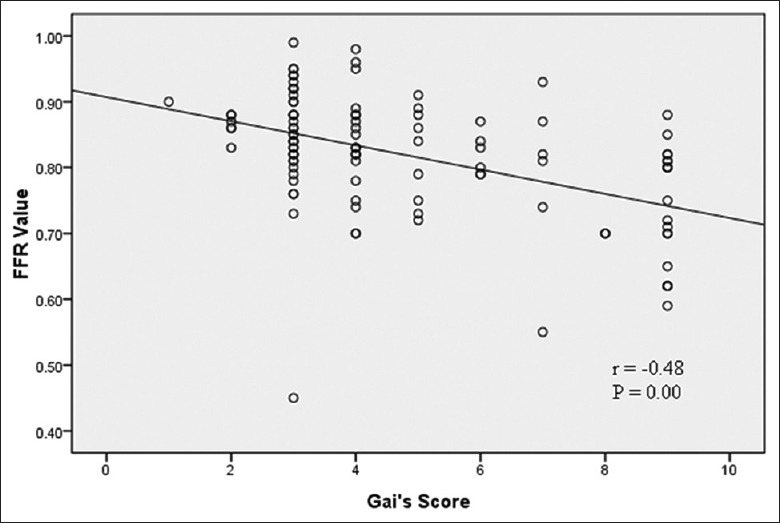
Correlation between the fractional flow reserve value and Gai's score (n = 107). FFR: Fractional flow reserve.
Figure 2.
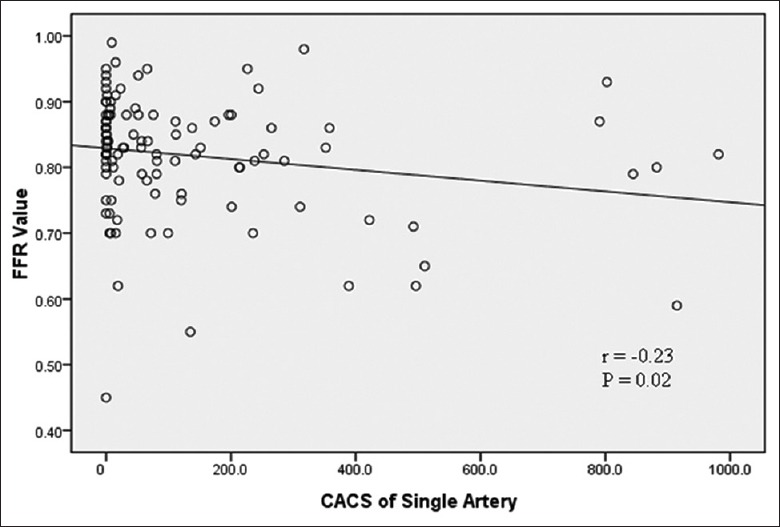
Correlation between the fractional flow reserve value and the coronary artery calcium score of a single artery (n = 107). FFR: Fractional flow reserve, CACS: Coronary artery calcium score.
To evaluate further the association between Gai's score, CACS of a single artery, and the FFR value, ROC curve analyses were performed to assess the ability of these scores to predict FFR <0.80 [Figure 3]. Gai's score showed a greater AUC (0.72; 95% confidence interval [CI]: 0.61–0.82; P < 0.01) than did CACS of a single artery (AUC, 0.62; 95% CI, 0.51–0.74; P = 0.05). The optimal cutoff values for predicting FFR <0.80 were as follows: 4.5 for Gai's score (64.5% sensitivity, 71.1% specificity, and 45.5% positive predictive value [PPV], and 83.1% negative predictive value [NPV]) and 4.85 for CACS of a single artery (87.1% sensitivity, 36.8% specificity, 36% PPV, and 12.5% NPV).
Figure 3.
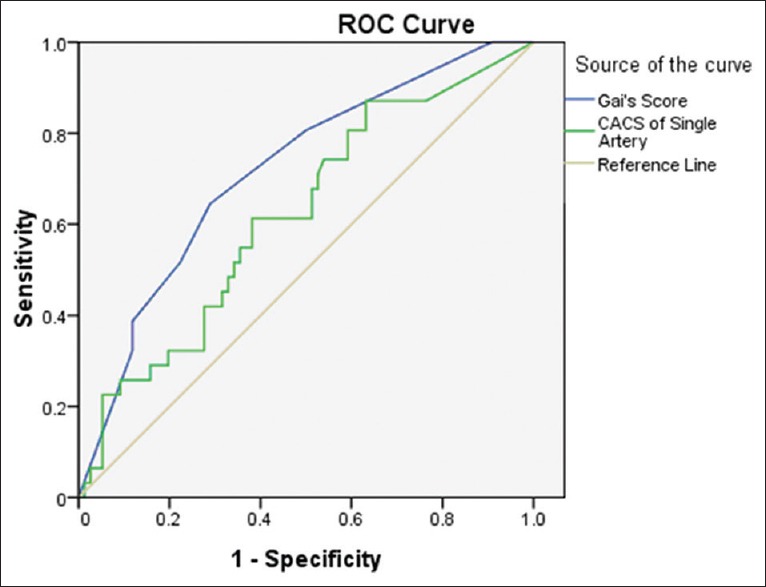
Receiver operating characteristic curves for detection of a fractional flow reserve value <0.80 (n = 107). ROC: Receiver operating characteristic, CACS: Coronary artery calcium score.
Discussion
FFR is an accurate and reliable method for assessing the physiological significance of coronary artery stenosis.[6,14,15] Consequently, using FFR to assess the potential of coronary artery stenosis to induce myocardial ischemia has been incorporated into coronary revascularization guidelines.[16,17] Several studies have shown promising results for noninvasive methods of evaluating the physiological significance of coronary artery stenosis that are comparable to those for FFR,[8,9,10] but these modalities are limited in their widespread use due to the requirement of increased irradiation, contrast use, cost, and time-consuming natures.
Some CCTA scores have already been developed as long-term predictors of serious cardiac events such as the segment involvement score (SIS) and the segment stenosis score (SSS). These scores use some of the same information obtained with CCTA, such as the number of lesions (similar as SIS) and the number of lesions plus the degree of stenosis (similar as SSS).[18] Our previous studies[12,13] described the development of a CT-derived plaque score (Gai's plaque score) that is similar to SIS and SSS. We have demonstrated its capability to predict major adverse cardiac events, such as acute myocardial infarction and cardiac death. Both SIS and SSS focus on long-term prognostic effects and are not able to predict functionally significant coronary lesions. In contrast, Gai's plaque score is related to atherosclerosis, lesion length, and plaque burden, which correlate with FFR,[19,20] and it can assess vessels individually. For this reason, we used Gai's plaque score to predict functionally significant coronary lesions in this study. Our results showed that Gai's score was moderately correlated with FFR (r = −0.48, P < 0.01).
We also assessed the association between the CACS and the FFR. CT is the only noninvasive imaging modality capable of accurately detecting and quantifying coronary calcium. Previous investigations suggested associations among coronary calcium and abnormal coronary vascular function, abnormal myocardial perfusion, and the process of atherosclerosis.[21,22,23,24] A greater calcium burden might predict advanced atherosclerotic processes in coronary arteries. A recent study evaluated the relationship between the FFR and CACS and reported that more extensive coronary artery calcification indicated a greater likelihood of physiological ischemia in angiographic intermediate stenosis, and the FFR correlated with CACS in individual arteries with intermediate stenosis rather than the total CACS.[25] Our data showed a similar tendency between FFR and CACS.
In the present study, compared with the CACS for a single artery, Gai's score showed a stronger correlation and better diagnostic accuracy with respect to significant coronary stenosis. It is known that several important factors can affect coronary flow: the degree of DS, lesion length, plaque burden, vessel size, lesion morphology, plaque characteristics, blood viscosity, collateral circulation, and supplied myocardium.[19] Gai's score includes more information about these factors than the CACS does and shows a larger AUC of a single artery than the CACS does. Furthermore, we did not combine Gai's score with the CACS to improve the diagnostic accuracy of the calcium burden, as that individual item was already assessed by Gai's score. Regarding the rich information that can be obtained from CCTA, the interest in effectively using this information for clinical purposes has resulted in intense research. Gai's score can be easily calculated using the CCTA reports used in daily clinical practice without additional costs, time, irradiation, contrast use, or drug administration. Thus, Gai's score appears to offer a feasible way to indicate physiological ischemia in significant coronary artery stenosis.
There were some limitations with this study. First, it was a single-center, retrospective study performed in a small number of patients referred for ICA because of moderately to severely diseased coronary arteries. Future prospective studies are required to evaluate the diagnostic accuracy of Gai's score and the CACS for selecting patients who will benefit most from revascularization. Second, because of the relatively small number of positive observations, we could not perform a multivariate logistic regression analysis to identify independent predictors of a positive FFR. Third, the scores rely on the actual CCTA reports, which vary in clinical practice. Finally, we excluded vessels with poor image quality on CCTA.
Both the CACS in a single artery and Gai's plaque score demonstrated a good capacity to assess functionally significant coronary artery stenosis with respect to the gold standard FFR. However, Gai's plaque score showed better performance in predicting FFR <0.80. This score can be easily calculated in daily clinical practice and could be used when considering revascularization.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
References
- 1.Hou ZH, Lu B, Gao Y, Jiang SL, Wang Y, Li W, et al. Prognostic value of coronary CT angiography and calcium score for major adverse cardiac events in outpatients. JACC Cardiovasc Imaging. 2012;5:990–9. doi: 10.1016/j.jcmg.2012.06.006. doi: 10.1016/j.jcmg.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Gai JJ, Gai LY, Yan JJ, Jin QH. Calculation of coronary angiographic total blush in patients with coronary artery disease and its prognostic implication. Chin Med J. 2015;128:2485–90. doi: 10.4103/0366-6999.164934. doi: 10.4103/0366-6999.164934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chi LQ, Zhang JQ, Kong QY, Xiao W, Liang L, Chen XL. Early results of coronary endarterectomy combined with coronary artery bypass grafting in patients with diffused coronary artery disease. Chin Med J. 2015;128:1460–4. doi: 10.4103/0366-6999.157652. doi: 10.4103/0366-6999.157652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mowatt G, Cook JA, Hillis GS, Walker S, Fraser C, Jia X, et al. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: Systematic review and meta-analysis. Heart. 2008;94:1386–93. doi: 10.1136/hrt.2008.145292. doi: 10.1136/hrt.2008.145292. [DOI] [PubMed] [Google Scholar]
- 5.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–32. doi: 10.1016/j.jacc.2008.07.031. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 6.Pijls NH. Fractional flow reserve to guide coronary revascularization. Circ J. 2013;77:561–9. doi: 10.1253/circj.cj-13-0161. doi: 10.1253/circj.CJ-13-0161. [DOI] [PubMed] [Google Scholar]
- 7.Sarno G, Decraemer I, Vanhoenacker PK, De Bruyne B, Hamilos M, Cuisset T, et al. On the inappropriateness of noninvasive multidetector computed tomography coronary angiography to trigger coronary revascularization: A comparison with invasive angiography. JACC Cardiovasc Interv. 2009;2:550–7. doi: 10.1016/j.jcin.2009.03.009. doi: 10.1016/j.jcin.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Ko BS, Cameron JD, Meredith IT, Leung M, Antonis PR, Nasis A, et al. Computed tomography stress myocardial perfusion imaging in patients considered for revascularization: A comparison with fractional flow reserve. Eur Heart J. 2012;33:67–77. doi: 10.1093/eurheartj/ehr268. doi: 10.1093/eurheartj/ehr268. [DOI] [PubMed] [Google Scholar]
- 9.Ho KT, Chua KC, Klotz E, Panknin C. Stress and rest dynamic myocardial perfusion imaging by evaluation of complete time-attenuation curves with dual-source CT. JACC Cardiovasc Imaging. 2010;3:811–20. doi: 10.1016/j.jcmg.2010.05.009. doi: 10.1016/j.jcmg.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989–97. doi: 10.1016/j.jacc.2011.06.066. doi: 10.1016/j.jacc.2011.06.066. [DOI] [PubMed] [Google Scholar]
- 11.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. doi: 10.1016/0735-1097(90)90282-T. [DOI] [PubMed] [Google Scholar]
- 12.He B, Gai LY, Gai JJ, Qiao HY, Zhang SY, Guan ZW. Coronary plaques identified by coronary computed tomography angiography and the risk factors for major adverse cardiac events: A correlation analysis (In Chinese) J South Med Univ. 2012;32:1400–6. doi: 10.3969/j.issn.1673-4254.2012.10.004. [PubMed] [Google Scholar]
- 13.Zhang KY, Gai LY, Gai JJ, He B, Guan ZW. Four-year clinical outcome in asymptomatic patients undergoing coronary computed tomography angiography. Chin Med J. 2013;126:1630–5. [PubMed] [Google Scholar]
- 14.Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, Bornschein B, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol. 2010;56:177–84. doi: 10.1016/j.jacc.2010.04.012. doi: 10.1016/j.jacc.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 15.De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991–1001. doi: 10.1056/NEJMoa1205361. doi: 10.1056/NEJMoa1205361. [DOI] [PubMed] [Google Scholar]
- 16.Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J. 2014;35:2541–619. doi: 10.1093/eurheartj/ehu278. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 17.Patel MR, Dehmer GJ, Hirshfeld JW, Smith PK, Spertus JA. ACCF/SCAI/STS/AATS/AHA/ASNC/HFSA/SCCT 2012 Appropriate use criteria for coronary revascularization focused update: A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2012;59:857–81. doi: 10.1016/j.jacc.2011.12.001. doi: 10.1016/j.jacc.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Hulten E, Bittencourt MS, Singh A, O'Leary D, Christman MP, Osmani W, et al. Coronary artery disease detected by coronary computed tomographic angiography is associated with intensification of preventive medical therapy and lower low-density lipoprotein cholesterol. Circ Cardiovasc Imaging. 2014;7:629–38. doi: 10.1161/CIRCIMAGING.113.001564. doi: 10.1161/CIRCIMAGING.113.001564. [DOI] [PubMed] [Google Scholar]
- 19.Rossi A, Papadopoulou SL, Pugliese F, Russo B, Dharampal AS, Dedic A, et al. Quantitative computed tomographic coronary angiography: Does it predict functionally significant coronary stenoses? Circ Cardiovasc Imaging. 2014;7:43–51. doi: 10.1161/CIRCIMAGING.112.000277. doi: 10.1161/CIRCIMAGING.112.000277. [DOI] [PubMed] [Google Scholar]
- 20.Wang L, Jerosch-Herold M, Jacobs DR, Jr, Shahar E, Detrano R, Folsom AR. MESA Study Investigators Coronary artery calcification and myocardial perfusion in asymptomatic adults: The MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2006;48:1018–26. doi: 10.1016/j.jacc.2006.04.089. doi: 10.1016/j.jacc.2006.04.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalra SS, Shanahan CM. Vascular calcification and hypertension: Cause and effect. Ann Med. 2012;44(Suppl 1):S85–92. doi: 10.3109/07853890.2012.660498. doi: 10.3109/07853890.2012.660498. [DOI] [PubMed] [Google Scholar]
- 22.Ross R. The pathogenesis of atherosclerosis: A perspective for the 1990s. Nature. 1993;362:801–9. doi: 10.1038/362801a0. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 23.Stary HC. Composition and classification of human atherosclerotic lesions. Virchows Arch A Pathol Anat Histopathol. 1992;421:277–90. doi: 10.1007/BF01660974. doi: 10.1007/BF01660974. [DOI] [PubMed] [Google Scholar]
- 24.Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W., Jr A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation. 1995;92:1355–74. doi: 10.1161/01.cir.92.5.1355. doi: 10.1161/01.CIR.92.5.1355. [DOI] [PubMed] [Google Scholar]
- 25.Horie K, Kikuchi Y, Takizawa K, Inoue N. Role of coronary calcium scoring in the assessment of physiological ischemia in patients with intermediate stenosis. Int J Angiol. 2015;24:283–91. doi: 10.1055/s-0035-1554943. doi: 10.1055/s-0035-1554943. [DOI] [PMC free article] [PubMed] [Google Scholar]


