Abstract
Background:
Nowadays, social media tools such as short message service, Twitter, video, and web-based systems are more and more used in clinical follow-up, making clinical follow-up much more time- and cost-effective than ever before. However, as the most popular social media in China, little is known about the utility of smartphone WeChat application in follow-up. In this study, we aimed to investigate the feasibility and superiority of WeChat application in clinical follow-up.
Methods:
A total of 108 patients diagnosed with head and neck tumor were randomized to WeChat follow-up (WFU) group or telephone follow-up (TFU) group for 6-month follow-up. The follow-ups were delivered by WeChat or telephone at 2 weeks, 1, 2, 3, and 6 months to the patients after being discharged. The study measurements were time consumption for follow-up delivery, total economic cost, lost-to-follow-up rate, and overall satisfaction for the follow-up method.
Results:
Time consumption in WFU group for each patient (23.36 ± 6.16 min) was significantly shorter than that in TFU group (42.89 ± 7.15 min) (P < 0.001); total economic cost in WFU group (RMB 90 Yuan) was much lower than that in TFU group (RMB 196 Yuan). Lost-to-follow-up rate in the WFU group was 7.02% (4/57) compared with TFU group, 9.80% (5/51), while no significance was observed (95% confidence interval [CI]: 0.176–2.740; P = 0.732). The overall satisfaction rate in WFU group was 94.34% (50/53) compared with 80.43% (37/46) in TFU group (95% CI: 0.057–0.067; P = 0.034).
Conclusions:
The smartphone WeChat application was found to be a viable option for follow-up in discharged patients with head and neck tumors. WFU was time-effective, cost-effective, and convenient in communication. This doctor-led follow-up model has the potential to establish a good physician-patient relationship by enhancing dynamic communications and providing individual health instructions.
Trial Registration:
Chinese Clinical Trial Registry, ChiCTR-IOR-15007498; http://www.chictr.org.cn/ showproj.aspx?proj=12613.
Keywords: Communication, Lost-to-follow-up, Head and Neck Neoplasms, Physician-patient Relationship, Social Media
Introduction
The main purposes of routine long-term follow-up for head and neck tumor patients are as follows: (1) early detection and prompt treatment of locoregional recurrences; (2) detection of distant metastases or second primary tumors; (3) provide psychological and emotional support; (4) assessment of treatment-related complications; and (5) evaluation of treatment outcomes and posttreatment quality of life.[1,2,3,4] Even though there are many researchers focusing on standard follow-up strategy,[5,6] we found that the follow-up strategy has not fully been implemented in practice. The follow-up schedules might not be well delivered to patients due to various factors including the increasing number of cancer patients compared with a relative lack of medical resource and the poor traffic hindering cancer patients living in some of the remote areas from on-spot visiting.[7,8] Unlike most advanced countries, such as America or Germany, we do not have the interconnected or shared internetworking system in different hospitals among the whole country or even in different areas. It means that the doctors cannot get message from any other hospital, and hence it is pretty difficult to implement continuous follow-up strategy or postdischarge health surveillance in China. Besides, barriers regarding either the cost or the overburdening work were also considered to have led to the difficulty of follow-up delivery.[9]
The booming of information technology has brought up a great diversity of methods of medical consultation. Much evidence shows that the rapidly developing eHealth has a great impact on medical practice.[10,11] In addition, more and more investigators believe that the big data tools and technologies have the potential to create significant value for health care.[12] Telemedicine, characterized by the communication technology and medical information transmission ability based on the internet, has been used to conduct follow-up in orthopedic trauma.[13] Similarly, Marsh et al.[14] have performed the web-based assessment in follow-up after total joint arthroplasty. An interactive voice response system has been used to provide follow-up and feedback message in health-care settings.[15]
As smartphones have a wide usage in people's life, mobile health applications (apps) such as “Apple Health” is changing our way of medical consultation.[16,17] Therefore, these apps might have the potential to improve the follow-up strategy of head and neck cancer patients. In recent years, WeChat, a social media app, has become the most popular of its kind in China. According to Xinhua, the number of WeChat users reached over 600 million in October 2014. Yang et al.[18] have applied WeChat in providing guidance for pediatric intestinal colostomy. There are other researchers focusing on applying WeChat in library service, financial service, and other fields. However, to our knowledge, evidence of WeChat implemented for follow-up is limited at present. Given the huge potential, we are trying to apply mobile WeChat to the follow-up of head and neck tumor patients.
In this study, we reported the results of a randomized controlled trial (RCT) to investigate the feasibility and superiority of using WeChat as a wonderful assistant to clinical track and follow-up of patients with head and neck tumors. By comparing WeChat with the typical telephone follow-up (TFU) model, we hypothesized that the efficiency of follow-up would be improved due to the less time and money spent using WeChat. We will also assess the overall satisfaction rates and lost-to-follow-up rates of WFU method. Furthermore, the impact on the physician-patient relationship reconstruction based on doctor-led WeChat follow-up (WFU) model and the advantages of WeChat were discussed.
Methods
Patients
A total of 108 participants (100 males and 8 females, aged 20 to 77 years) were recruited to the RCT study. All the patients were pathologically diagnosed with head and neck tumors (benign or malignant) and underwent curative surgery therapy in our Hospital. All the participants were also required to own a smartphone and to be able to correctly complete the follow-up consultations either on WeChat or on phone calls. The patients who did not own a smartphone or could not correctly complete their consultations were also included if they had a family member who had a smartphone and could help them to complete the follow-up on WeChat. The patients under psychosis or other medical or psychological condition that would interfere with the ability to consent and/or participate in the program were excluded from this study. The patients’ diseases included laryngeal papilloma, laryngeal carcinoma, hypopharyngeal carcinoma, oropharyngeal carcinoma, and vocal leukoplakia. All the eligible patients had been enrolled into the study before discharging from the hospital.
This study protocol was approved by the Ethics Committee of The First Affiliated Hospital, Sun Yat-Sen University, and all the eligible patients provided informed consent to take part in the study.
Study design and randomization
The study was conducted from April 2015 to October 2015. Eligible patients were randomized to WFU group (followed-up on WeChat) or TFU group (followed-up on telephone) for clinical tracking according to the predesigned random allocation envelopes which they chose. (inside the envelopes were allocation cards either written 0 or 1: 0 represents WFU group and 1 represents TFU group). A laboratory technician, who was not directly involved in the study, blinded the investigators to the study grouping so that the investigators would not know how were patients randomized. In addition, the patients would not know which group other patients would be divided into. The patients who could not speak due to loss of phonation function were excluded from the TFU group. All the participants were informed the purpose of our study and the fact that they might be classified into either the WFU group or the TFU group. All the patients and their families were required to attend the pre-follow-up training regarding how to use WeChat on a smartphone. The only doctor involved in this study had registered a specific WeChat account exclusively for the follow-up work. For the WFU group, all the patients or relatives were added to the WeChat list of the doctor in charge, and the follow-up was conducted by delivering the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire, Head and Neck Module (EORTC QLQ-H&N35, in PDF format file), to the patients one by one on WeChat at 2 weeks, 1, 2, 3, and 6 months after they were discharged from the hospital. The patients were required to fill in the QLQ-H&N35 scale on a piece of paper after receiving it, take a picture of the completed form, and send it back in an image format to the doctor on WeChat. For the TFU group, the follow-up was conducted on telephone referring to the EORTC QLQ-H&N35 scale.[19] Then, the distributor recorded the data of both the WFU and TFU groups. All the participants were required to keep their mobile phones on or WeChat online. Patients suffering from malignant tumor or precancerous lesions were asked to make subsequent visit for computed tomography (CT), magnetic resonance imaging (MRI), or laryngoscope according to the NCCN Clinical Practice Guideline of Head and Neck Cancers at 3 and 6 months after discharging from the hospital.
Measurements
Time consumption
Time consumption of each follow-up delivery was recorded only from the physician's perspective to assess the doctor's workload. The time spent on delivering scales to participants, recording the scales, and answering the questions, all accounted for the time consumption of WFU, while the time spent when the patients were sending back the answers was not included for WFU. As for the TFU method, time consumption referred to the time spent on the telephone call to the patients.
Total economic cost
In general, the cost involved in the follow-up might happen to both the providers and the participants. In our study, the cost was calculated only on the physician's perspective, which included the telephone charge and mobile traffic cost (when WIFI is unavailable). As for WFU group, cost mainly depended on the internet traffic, which was calculated according to the traffic charging criterion of China Mobile. Cost for TFU group was calculated based on the charging criterion of China Telecom. We would only evaluate the total cost for WFU during the whole study since it is hard to calculate internet traffic for each patient or each follow-up consultation.
Lost-to-follow-up rate
Lost-to-follow-up is generally considered to be associated with the poor outcome and it should be seriously considered when making a follow-up regimen.[20] In our study, the patients who were out of contact or who refused any further follow-up were considered lost-to-follow-up. Moreover, the patients who did not reply to the distributor in 3 days were reminded by WeChat message and would be considered lost-to-follow-up if they still did not reply.
Satisfaction rate
Besides, satisfaction rates of each group were assessed by asking the patients whether they were satisfied with their follow-up methods at the end of the study, and the self-reported satisfaction data were calculated, through which the impact of WFU on the physician-patient relationship was discussed.
We hypothesized that (1) WFU would cost the doctors significantly less time and money to complete the follow-up than TFU would, (2) WFU would have a higher overall satisfaction rate than TFU would for its convenience, acceptability, and multimedia character, and (3) the doctor-led WFU model would have a significant impact on rebuilding the current physician-patient relationship situation in China.
Statistical analysis
All the statistical analyses were conducted with SPSS software version 22.0 (SPSS Inc., Chicago, IL, USA). Continuous data were analyzed by t-test, and the results were described as mean ± standard deviation (SD). Categorical data were compared by Chi-square or Fisher's exact tests, and the results were described as n (%). Mann-Whitney U-test was used to compare nonnormal distribution continuous data, and the results were expressed as median (quartile). A value of P < 0.05 was considered to be statistically significant.
Results
Of all the patients (n = 122) recruited to this study, 108 were deemed eligible to participate, with a randomized allocation to either WFU group (n = 57) or TFU group (n = 51). A total of 99 patients (n = 53 in WFU group and n = 46 in TFU group) completed the study, with four (4/57, 7.02%) dropped out from WFU group (of whom two could not continue the WFU due to the relative's absence, one due to poor compliance, and one patient due to WeChat account change) and five (5/51, 9.80%) dropped out from TFU (three due to poor compliance, one due to the relatives’ absence, and one probably due to phone number change). A flow diagram of this study is presented in Figure 1. Although baseline characteristic varies, there was no significant difference concerning the selected demographic and clinical characteristics in both groups [Table 1].
Figure 1.
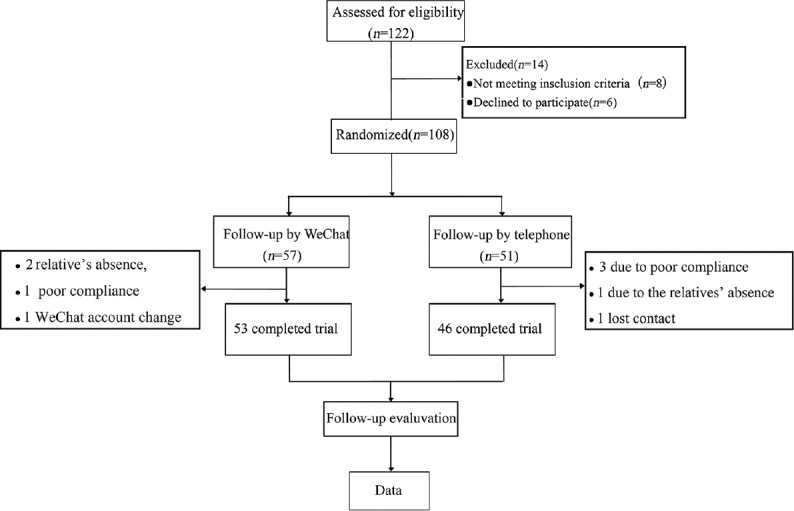
Trial procedure of the follow-up design.
Table 1.
Selected baseline characteristics of the randomized study groups
| Characteristics | TFU (n = 46) | WFU (n = 53) | Statistics | P |
|---|---|---|---|---|
| Age (years) | 61.5 (9.3) | 61.0 (13.0) | −0.660* | 0.509 |
| Male | 45 (97.8) | 50 (94.3) | 0.772† | 0.621 |
| Education level | ||||
| Less than high school | 35 (76.1) | 38 (71.7) | 0.245† | 0.621 |
| High school and above | 11 (23.9) | 15 (28.3) | – | – |
| Residence | ||||
| Rural | 14 (30.4) | 14 (26.4) | 0.169† | 0.658 |
| City | 32 (69.6) | 39 (73.6) | – | – |
| Diagnosis | ||||
| Laryngeal cancer | 29 (63.0) | 34 (64.2) | – | 0.589 |
| Hypopharyngeal cancer | 6 (13.0) | 5 (9.4) | 2.816† | – |
| Laryngeal papilloma | 6 (13.0) | 6 (11.3) | – | – |
| Oropharyngeal cancer | 4 (8.7) | 3 (5.7) | – | – |
| Vocal leukoplakia | 1 (2.3) | 5 (9.4) | – | – |
| Duration of disease (years) | 1.0 (1.5) | 1.0 (1.0) | −0.032* | 0.974 |
Data are medians (IQR) or n (%), *Z value, †χ2 value. –: No data; TFU: Telephone follow-up; WFU: WeChat follow-up; IQR: Interquartile range.
Time consumption
Time consumption in WFU group for each patient (23.36 ± 6.16 min) was significantly shorter than that in TFU group (42.89 ± 7.15 min, P < 0.001, Figure 2).
Figure 2.
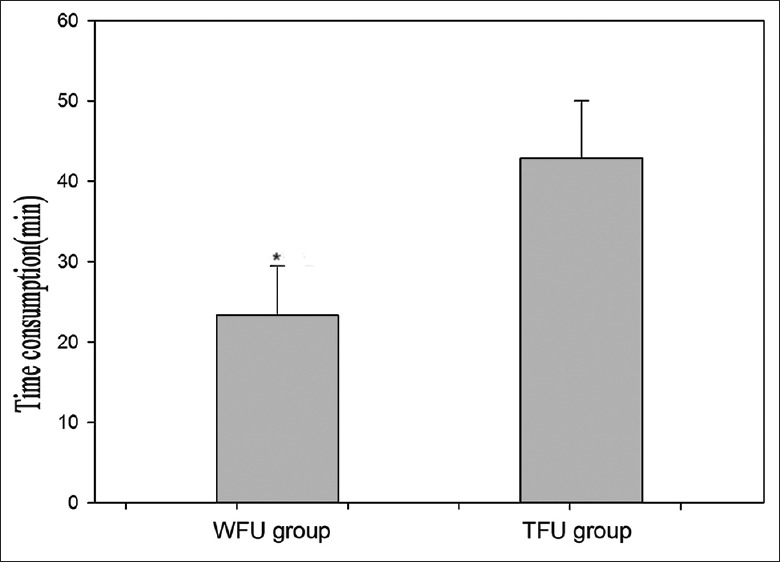
Time consumption of clinical follow-up. WFU: WeChat follow-up; TFU: Telephone follow-up; *P < 0.05 was considered to be statistically significant.
Total economic cost
At the end of this study, the total cost of WFU was RMB 90 Yuan compared with RMB 196 Yuan that of TFU, while the difference is not statistically significant.
Lost-to-follow-up rate
The lost-to-follow-up rate was lower in the WFU group (7.02%, 4/57) than that in the TFU group (9.80%, 5/51), but there was no significant difference between the two groups (95% confidence interval [CI]: 0.176–2.740; P = 0.732).
Satisfaction rate
We further calculated the overall satisfaction rates of the two delivery methods concerning the convenience, acceptability, and practicability. WFU group (94.34%, 50/53) had statistically significant higher satisfaction rates compared with TFU group (80.43%, 37/46) (95% CI: 0.057–0.067; P = 0.034). In addition, we focused on the impact of the WeChat on rebuilding the patient-doctor relationship based on this doctor-led follow-up model and gathered a lot of questions asked by the patients [Table 2].
Table 2.
Partial questions gathered from patients during WFU period
| Inquire |
|---|
| 1. I feel weak after the surgery. What drug should I take? |
| 2. I still feel great pain in my incision since the surgery last year. Is it normal and what should I do? |
| 3. I often cough when I eat and sometimes with food flow out of the incision. What is wrong with me? |
| 4. I underwent surgery 2 years ago and now I feel good. Do I still need to visit the outpatient department regularly? |
| 5. My voice has not improved since my throat surgery 2 months ago. Would it be any problem with me? |
| 6. This is the report of my CT scan and laryngoscope in the local hospital. It is inconvenient for me to visit your clinic. Could you check it for me? |
| 7. My voice got worse after chemotherapy. What is wrong with me and what drug should I take? |
| 8. I have been coughing for about 3 months and I have taken some medicine prescribed in the local clinic but it did not work. What should I do? |
CT: Computed tomography; WFU: WeChat follow-up.
Discussion
Our study demonstrated that the smartphone WeChat application could be a wonderful assistant to follow-up due to its better convenience, less time and money consumption, and higher degree of satisfaction than those of TFU. In general, patients who have gone through therapeutic approach are more likely to consult with the doctor, and hence it will be greatly helpful to set up a continuous communication platform for discharged patients.[11] In our study, patients in WFU group, compared with patients in TFU group, kept closer contact with their doctors and gave more feedback information to their doctors during the follow-up. This indicates that WeChat might have the potential to enhance the doctor-patient communication and thus help rebuild physician-patient relationship in China.
It cannot be denied that routine long-term follow-up plays a more and more important role in clinical work, especially in the practice of oncologic disciplines.[1] However, in many hospitals in China, the follow-up regimens have not been widely built and the total follow-up rate is low, the reasons of which could be described as follows: (1) the lack of follow-up department or full-time staff for follow-up work and (2) the lack of follow-up software. These resulted in high lost-to-follow-up rates of tumor patients, leaving a barrier to further developing the quality of follow-up work.[21,22] Furthermore, when follow-ups are conducted by other health-care providers than the doctors who were in charge of the patients in hospital, nonindividualized guidance, nonconsistent disease surveillance, or even wrong instructions might be given, contributing to the low total follow-up rate.[23] Unlike most advanced countries in the world, most hospitals in China do not have an interconnected or shared internetworking system. Hence, it is critical to set up a platform to integrate all the resources of different hospitals. In our study, we investigated the feasibility and superiority of a new follow-up model by combining the WeChat application with the clinical follow-up. By WeChat application, the doctor can keep contact with the patients, remind the patients when they do not attend routine clinical follow-up, and collect the clinical data of CT scan or laryngoscopy in picture format, no matter which hospital the patients attend the follow-up.
As information technology improves, more and more evidence was observed that the internet has the potential to rebuild health-care patterns.[24] Interestingly, the interest in using technology to deliver cancer follow-up is increasing worldwide.[25] In contrast to some of the investigators, we are devoting to applying a new doctor-led follow-up model, a one-to-one connection strategy to investigate the feasibility of follow-up using the smartphone application WeChat [Figure 3]. By making specific remarks to each patient and regular backup of WeChat communication information, we can easily manage the WFU [Figure 4a]. For example, we can search for specific patient, check his/her personal information or clinical histories through communication records, and make comparisons among different patients. Notably, as a convenient internet tool, the app WeChat is flexible with respect to the freedom of location and time for communication so that this follow-up model will not significantly increase the doctors’ workload or time consumption. Our finding that WFU costs the doctors less spare time to conduct follow-ups suggested that WeChat application might be an option for follow-up delivery that does not add too much to the clinical workload.[7] However, with the increasing number of the patients, appropriate management strategies such as team management are important to handle this follow-up. In the team management strategy, the senior doctor is in charge of the overall management of the guidance for the discharged patient with the help of the intermediate doctors, along with the data management by the resident. Although the fact that WeChat had an economic advantage over the traditional TFU as observed in our study, the difference in total economic cost between WFU and TFU groups was not statistically significant. However, other investigators concluded that WeChat application could save the patients’ time and money by avoiding unnecessary physical presence in the hospital, which was, however, not investigated in our study.[18] Remarkably, our WFU would not increase cost for the patients.
Figure 3.
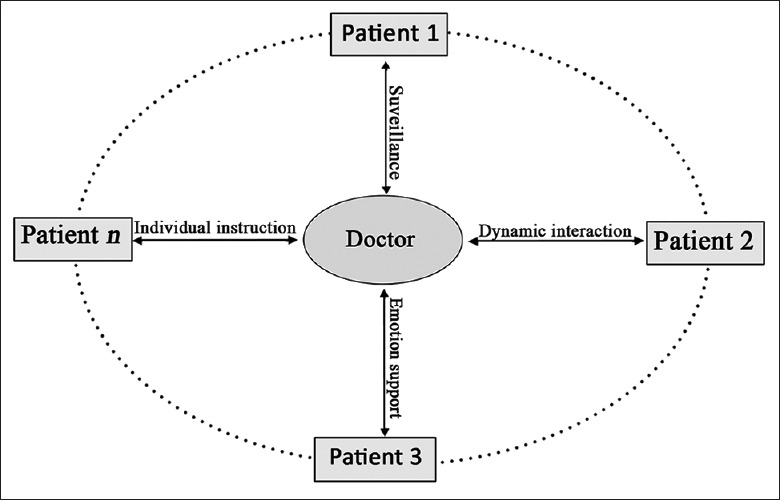
The doctor-led physician-patient relationship.
Figure 4.
Management strategy of WeChat follow-up method (WeChat user interface): Representative pictures chosen from our WeChat follow-up method to show our management strategies. (a) WeChat list of patients (translated into English); (b) Laryngoscopy sent by patients; (c) Health consultation of a discharged laryngectomized.
Our results showed low lost-to-follow-up rates in both WFU and TFU groups without a statistical difference. As for the overall satisfaction, WeChat group has showed a higher satisfaction than telephone group, which indicated that patients would rather like to keep a close relationship with the attendance doctor. Obviously, WeChat could provide the doctors and patients with media which not only include voice communication, but also include text reading, image sharing, and video consultation. It indicates that WeChat might have the potential to build a stronger tie between patients and doctors than telephone. This demonstrates that WeChat could be used for follow-up instead of telephone under many circumstances, especially for delivering health-care education to discharged head and neck cancer patients. A previous research reported that the patients who received multimedia information about head and neck cancer would show higher levels of satisfaction compared with those who did not.[26] Above all, WeChat application can be an augmentation to follow-up, of which the long-term feasibility and effectiveness still need to be further observed.
In addition to the advantages mentioned above, we concluded that WeChat application might have a profound positive impact on the physician-patient relationship based on postdischarge follow-up. Under the circumstance of big data, subtle changes were observed with respect to the physician-patient relationship, which meant a shift in the role of the patient from passive recipient to active seeker of health information from the internet and the doctor would be requested to provide more health information.[11,27,28] Using the media technology, the clinical outcome of the patients was found to be improved.[29] In addition, with the increasing implementation of the internet in health care, web-based health information was considered to be a viable way through which the physician-patient relationship was enhanced.[30] Nonetheless, the web-based health information model also has many disadvantages. For instance, the quality of the information can be highly variable, which might include misleading or misinterpreted information, thus leading to incorrect instructions and impaired outcomes, or result in inappropriate requests in the clinical interventions.[30,31,32] Unlike the website-based eHealth model, the WFU strategy requires that the follow-up should be conducted by the doctor who was in charge of the patients when they were in hospital so that the doctor can have a comprehensive understanding of the patients’ conditions and give the patients individual-specified instructions. Other researches also reported that the physician-patient relationship itself other than the internet was more valuable in patient education.[33] Therefore, setting up a more direct physician-patient relationship is crucial to the improvement of the current medical circumstance in China.
In our study, we initially investigated the impact of the smartphone WeChat application on the physician-patient relationship. By long-term monitoring and tracing of a discharged patient, the person-to-person connection between the doctor and the patient was established. Compared with a website-based tool, WeChat is more available, more convenient, and more widely used, especially in China, providing a more direct, rapid, dynamic, and “friendly” interaction between doctors and patients. In addition, the WFU appears to be able to fill in the gaps between doctors and patients by facilitating communication and collaboration.
The flexibility and convenience might also make WeChat more feasible than websites or telephone. As shown in Table 2, the WFU established a portable direct platform for doctor-patient interaction, thereby increasing the time of communication between doctors and patients. Obviously, this WFU model will benefit both patients and doctors. As for the patients, the continuous health instruction and education from the health professionals will help them make healthful decisions, provide them a psychological assistance and a comprehensive understanding of diseases, thus improving their satisfaction and final outcomes. As for the doctors, this on-hand traceable model can provide them real-time information of the patients in the form of text, voice, image, and video. This provides a flexible feedback mechanism for the doctors, which might help to know about the rehabilitation condition and detect the recurrence or the complication [Figure 4b and 4c]. Besides, an early study conducted by Angie Hart et al.[32] found that patients had quite a high degree of trust in their health-care practitioners. Similarly, our study of implementing WeChat in follow-up has shown a strong tie between doctors and patients, where patients had good compliance and a great deal of trust in their doctors. This indicated that WeChat might greatly help rebuild the physician-patient relationship, although further studies focusing on this issue are still in need.
Here, we are illustrating the mobile WeChat, a novel internet tool, as a useful assistant rather than a replacement for clinical follow-up in China. As we all know, the poor follow-up regimens in China were caused not only by technological problem but also by policy defect. Under this circumstance, more efficient methods should be investigated and practically appropriate strategies should be flexibly applied to enhance clinical follow-up. Notably, there are no assistant methods that could never replace traditional clinical follow-up because we could not diagnose without clinical examination or medical equipment. However, we could get rough message by continuous dynamic surveillance through Internet device, which would be valuable for clinical follow-up. Besides, under any ambiguous feedback or suspicious condition, we would recall the patients for clinical or medical equipment examination to avoid misdiagnosis or missed diagnosis.
Despite the positive findings, our study also had some limitations. First, the average age of the studied population is relatively older because of the epidemiological characteristics of head and neck tumors. The patients might have a relatively low literacy condition and a poor ability of using the smartphone or some of them even do not own a smartphone, which was also observed in a study held in Japan.[16] In this condition, the follow-up or communication would need the assistance of their families or relatives. This might create bias and uncertainties of the results. This limitation might be avoided when applied to other diseases. Second, sample size should be strictly determined by the primary end point of RCT. However, we indeed did not strictly determine the sample size and the reasons are as follows: (1) powerful conclusion could be preliminarily drawn based on the current sample size in our research. Our future study with a larger sample size will further confirm this conclusion and (2) we are now trying to investigate a novel internet tool for clinical follow-up. We do think that novelty and speed are important for the clinical research, especially in the internet era. Third, excluding participants after randomization in our research might lead to bias. However, it is hard to avoid this situation concerning the characteristic of the TFU. A more appropriate design should be considered for our further research. In addition, the abundant patients from our hospital contribute to the conclusion. Moreover, we do think that this follow-up has inclusive valuable when applied to most hospitals of different sizes. Besides, it is yet unknown that whether WFU will improve the clinical outcome through individual guidance and more specialized education. What is more, the study has a limited sample size and a short follow-up period, thus no conclusion regarding clinical outcome has been appropriately drawn. Our future studies with a larger cohort and longer follow-up will continue to confirm the conclusions and further investigate whether the WFU model would bring a positive clinical outcome.
Financial support and sponsorship
This work was partially supported by a grant from the National Natural Science Foundation of China (No. 81072224).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng lyu
References
- 1.Boysen M, Lovedale O, Tausjo J, Winther F. The value of follow-up in patients treated for squamous cell carcinoma of the head and neck. Eur J Cancer (Oxford England 1990) 1992;28:426–30. doi: 10.1016/s0959-8049(05)80068-1. doi: 10.1016/S0959-8049(05)80068-1. [DOI] [PubMed] [Google Scholar]
- 2.de Visscher AV, Manni JJ. Routine long-term follow-up in patients treated with curative intent for squamous cell carcinoma of the larynx, pharynx, and oral cavity. Does it make sense? Arch Otolaryngol Head Neck Surg. 1994;120:934–9. doi: 10.1001/archotol.1994.01880330022005. doi: 10.1001/archotol.1994.01880330022005. [DOI] [PubMed] [Google Scholar]
- 3.Guibert M, Lepage B, Woisard V, Rives M, Serrano E, Vergez S. Quality of life in patients treated for advanced hypopharyngeal or laryngeal cancer. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:218–23. doi: 10.1016/j.anorl.2011.02.010. doi: 10.1016/j.anorl.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Kilbourn KM, Anderson D, Costenaro A, Lusczakoski K, Borrayo E, Raben D. Feasibility of EASE: A psychosocial program to improve symptom management in head and neck cancer patients. Support Care Cancer. 2013;21:191–200. doi: 10.1007/s00520-012-1510-z. doi: 10.1007/s00520-012-1510-z. [DOI] [PubMed] [Google Scholar]
- 5.Jung YH, Song CM, Park JH, Kim H, Cha W, Hah JH, et al. Efficacy of current regular follow-up policy after treatment for head and neck cancer: Need for individualized and obligatory follow-up strategy. Head Neck. 2014;36:715–21. doi: 10.1002/hed.23364. doi: 10.1002/hed.23364. [DOI] [PubMed] [Google Scholar]
- 6.Kothari P, Trinidade A, Hewitt RJ, Singh A, O'Flynn P. The follow-up of patients with head and neck cancer: An analysis of 1,039 patients. Eur Arch Otorhinolaryngol. 2011;268:1191–200. doi: 10.1007/s00405-010-1461-2. doi: 10.1007/s00405-010-1461-2. [DOI] [PubMed] [Google Scholar]
- 7.Okera M, Baker NA, Hayward AM, Selva-Nayagam S. Oncology workforce issues: The challenge of the outpatient clinic. Intern Med J. 2011;41:499–503. doi: 10.1111/j.1445-5994.2011.02506.x. doi: 10.1111/j.1445-5994.2011.02506.x. [DOI] [PubMed] [Google Scholar]
- 8.Hall SJ, Samuel LM, Murchie P. Toward shared care for people with cancer: Developing the model with patients and GPs. Fam Pract. 2011;28:554–64. doi: 10.1093/fampra/cmr012. doi: 10.1093/fampra/cmr012. [DOI] [PubMed] [Google Scholar]
- 9.Wu Q, Zhao Q, Xiao M, Reng G, Xiao S. Follow-up status and strategy for discharged patients in our country (in Chinese) Chinese Nursing Management. 2012;12:88–91. doi: 10.3969/j.issn.1672-1756.2012.04.029. [Google Scholar]
- 10.Kummervold PE, Chronaki CE, Lausen B, Prokosch HU, Rasmussen J, Santana S, et al. eHealth trends in Europe 2005-2007: A population-based survey. J Med Internet Res. 2008;10:e42. doi: 10.2196/jmir.1023. doi: 10.2196/jmir.1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiegand S, Marggraf J, Wilhelm T, Eivazi B, Werner JA. Internet-mediated physician-patient interaction focusing on extracranial hemangiomas and vascular malformations. Head Neck. 2014;36:187–90. doi: 10.1002/hed.23282. doi: 10.1002/hed.23282. [DOI] [PubMed] [Google Scholar]
- 12.Panahiazar M, Taslimitehrani V, Jadhav A, Pathak J. Empowering personalized medicine with big data and semantic web technology: Promises, challenges, and use cases. Proc IEEE Int Conf Big Data 2014. 2014:790–5. doi: 10.1109/BigData.2014.7004307. doi: 10.1109/BigData.2014.7004307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: A pilot study. J Orthop Trauma. 2015;29:e139–45. doi: 10.1097/BOT.0000000000000189. doi: 10.1097/BOT.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 14.Marsh J, Hoch JS, Bryant D, MacDonald SJ, Naudie D, McCalden R, et al. Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am. 2014;96:1910–6. doi: 10.2106/JBJS.M.01558. doi: 10.2106/JBJS.M.01558. [DOI] [PubMed] [Google Scholar]
- 15.Willig JH, Krawitz M, Panjamapirom A, Ray MN, Nevin CR, English TM, et al. Closing the feedback loop: An interactive voice response system to provide follow-up and feedback in primary care settings. J Med Syst. 2013;37:9905. doi: 10.1007/s10916-012-9905-4. doi: 10.1007/s10916-012-9905-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takahashi Y, Ohura T, Ishizaki T, Okamoto S, Miki K, Naito M, et al. Internet use for health-related information via personal computers and cell phones in Japan: A cross-sectional population-based survey. J Med Internet Res. 2011;13:e110. doi: 10.2196/jmir.1796. doi: 10.2196/jmir.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flores Mateo G, Granado-Font E, Ferré-Grau C, Montaña-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: A systematic review and meta-analysis. J Med Internet Res. 2015;17:e253. doi: 10.2196/jmir.4836. doi: 10.2196/jmir.4836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang QL, Wei Q, Huang Y, Jiang YX, Chen DZ, Huang P, et al. The application of multimedia messaging services via mobile phones to support outpatients: Home nursing guidance for pediatric intestinal colostomy complications. Chin Nurs Res. 2015;2:9–11. doi: 10.1016/j.cnre.2015.01.001. [Google Scholar]
- 19.Singer S, Wollbrück D, Wulke C, Dietz A, Klemm E, Oeken J, et al. Validation of the EORTC QLQ-C30 and EORTC QLQ-H&N35 in patients with laryngeal cancer after surgery. Head Neck. 2009;31:64–76. doi: 10.1002/hed.20938. doi: 10.1002/hed.20938. [DOI] [PubMed] [Google Scholar]
- 20.Murray DW, Britton AR, Bulstrode CJ. Loss to follow-up matters. J Bone Joint Surg Br. 1997;79:254–7. doi: 10.1302/0301-620x.79b2.6975. doi: 10.1002/hed.20938. [DOI] [PubMed] [Google Scholar]
- 21.Luo X, Hu X. To strengthen the management and construction for patient follow-up system (in Chinese) The Science Education Article Cultures. 2014;29:224–6. doi: 10.3969/j.issn.1672-7894.2014.29.110. [Google Scholar]
- 22.Xu X, Zhang J, Zhao M. To strengthen the management and construction for patient follow-up system (in Chinese) Soft science of health. 2011;25:75–7. doi: 10.3969/j.issn.1003-2800.2011.02.002. [Google Scholar]
- 23.Wang R. Problems and countermeasures in the follow-up of patients for large public hospitals (in Chinese) Mod Med Health. 2010;26:1227–9. [Google Scholar]
- 24.Hawn C. Take two aspirin and tweet me in the morning: How Twitter, Facebook, and other social media are reshaping health care. Health Aff (Millwood) 2009;28:361–8. doi: 10.1377/hlthaff.28.2.361. doi: 10.1377/hlthaff.28.2.361. [DOI] [PubMed] [Google Scholar]
- 25.Dickinson R, Hall S, Sinclair JE, Bond C, Murchie P. Using technology to deliver cancer follow-up: A systematic review. BMC Cancer. 2014;14:311. doi: 10.1186/1471-2407-14-311. doi: 10.1186/1471-2407-14-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D'Souza V, Blouin E, Zeitouni A, Muller K, Allison PJ. Do multimedia based information services increase knowledge and satisfaction in head and neck cancer patients? Oral Oncol. 2013;49:943–9. doi: 10.1016/j.oraloncology.2013.06.005. doi: 10.1016/j.oraloncology.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 27.McMullan M. Patients using the Internet to obtain health information: How this affects the patient-health professional relationship. Patient Educ Couns. 2006;63:24–8. doi: 10.1016/j.pec.2005.10.006. doi: 10.1016/j.pec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 28.Kassirer JP. Patients, physicians, and the Internet. Health Aff (Millwood) 2000;19:115–23. doi: 10.1377/hlthaff.19.6.115. doi: 10.1377/hlthaff.19.6.115. [DOI] [PubMed] [Google Scholar]
- 29.Bacigalupe G. Is there a role for social technologies in collaborative healthcare? Fam Syst Health. 2011;29:1–14. doi: 10.1037/a0022093. doi: 10.1037/a0022093. [DOI] [PubMed] [Google Scholar]
- 30.Wald HS, Dube CE, Anthony DC. Untangling the Web –The impact of internet use on health care and the physician-patient relationship. Patient Educ Couns. 2007;68:218–24. doi: 10.1016/j.pec.2007.05.016. doi: 10.1016/j.pec.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 31.Bao H, Zhu F, Wang F, Liu Z, Bao MH, He S, et al. Scoliosis related information on the internet in China: Can patients benefit from this information? PLoS One. 2015;10:e0118289. doi: 10.1371/journal.pone.0118289. doi: 10.1371/journal.pone.0118289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hart A, Henwood F, Wyatt S. The role of the Internet in patient-practitioner relationships: Findings from a qualitative research study. J Med Internet Res. 2004;6:e36. doi: 10.2196/jmir.6.3.e36. doi: 10.2196/jmir.6.3e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Aung KK, Wu WK, Tokumi A, Kuo P, Day CS. Does a directive to an internet site enhance the doctor-patient interaction? A prospective randomized study for patients with carpal tunnel syndrome. J Bone Joint Surg Am. 2015;97:1112–8. doi: 10.2106/JBJS.N.00741. doi: 10.2106/JBJS.N.00741. [DOI] [PubMed] [Google Scholar]



