Abstract
A growing body of research shows that cognitive remediation (Cog Rem), consisting of drill- and-practice and/or strategy training in neurocognitive functions, produces moderate improvements in neurocognition. These improvements generalize to functioning when Cog Rem is provided with other rehabilitation interventions (Wykes et al., 2011) The number of studies using Cog Rem as an adjunct to other behavioral-based rehabilitation interventions however remains small and consists of widely varying interventions with few active control conditions. This study compared the effects of an extended (6-month), standardized, computer-assisted cognitive remediation intervention, administered along with a standardized program of social skills-training (SST), with those of an active control condition that included participation in the same SST program and a computer skills training program (Computer Skills). Sixty-four individuals with schizophrenia recruited from two treatment sites were randomly assigned to one of two conditions and were assessed by blinded raters on neurocognitive measures, performance-based measures of social skill, and ratings of psychosocial function before and after treatment. Results revealed that the Cog Rem group improved significantly more in attention, working memory, and empathy than the Computer Skills group, but there were no differences between groups on other measures of psychosocial functioning or skills. Taken together, these findings suggest that Cog Rem used in the context of other evidence-based psychosocial interventions (SST) improves working memory in schizophrenia and suggests that this effect may generalize to improved empathy.
Cognitive deficits in schizophrenia are evident across virtually every measured aspect of cognition (e.g., Heinrichs & Zakzanis, 1998; but see Gold et al., 2009), and are present by the first episode of the illness (Mesholam-Gately et al., 2009), persist over time (Irani et al., 2011), and are largely unaffected by contemporary pharmacologic approaches to symptom management. Cognitive impairment in schizophrenia has been linked at moderate levels to a variety of dimensions of outcome, explaining anywhere from 20-60% of the variance in these studies (Green et al., 2000). Dimensions of outcome linked to cognitive skill including social skill (Dickinson et al., 2007), community functioning (Green et al., 2004), vocational status and work quality (Bell & Bryson, 2001; McGurk & Mueser, 2003), and benefit from psychosocial rehabilitation (Kurtz, 2011). Thus, improving cognition has become a central focus of treatment development in the field.
Over the past 10 years a growing number of randomized, controlled studies have supported the efficacy of a range of cognitive remediation (Cog Rem) interventions for cognitive deficits in schizophrenia. These programs have differed according to training emphasis. Some train elementary sensory processing (e.g., tone frequency discrimination) as a method for increasing the fidelity of sensory representations in the mind (e.g., Fisher et al., 2009), others train discrete neuropsychological areas sequentially and hierarchically (attention, then memory then problem-solving; e.g., Bell et al., 2001), while still others focus on the acquisition of strategies to facilitate the learning of information (e.g., Wykes et al., 2007). Cog Rem programs also vary widely in terms of duration, intensity, training stimuli used, and the degree to which generalization is explicitly targeted (McGurk et al., 2013). Despite these differences, Cog Rem programs share a common intent, as summarized by a recent statement of the Experts in Cognitive Remediation Workshop (Florence, Italy, 2010): “a behavioral training based intervention that aims to improve cognitive processes (attention, memory, executive function, social cognition or metacognition) with the goals of durability and generalization.”
A comprehensive meta-analysis of 40 controlled studies and 2,104 participants revealed that Cog Rem programs produced mild to moderate and durable improvements across summary or global cognition measures (d=.45) as well as in a range of specific cognitive domains (e.g., attention/vigilance, speed of processing), and functioning (Wykes et al., 2011). There was also clear evidence that the impact of these treatments on functioning was boosted by participation in other rehabilitation interventions as compared to stand-alone Cog Rem interventions (d=.59 vs. d=.28). Thus, given the efficacy of Cog Rem studies based on this meta-analysis, and the importance of providing other rehabilitation interventions alongside Cog Rem in order to improve functional outcomes, understanding how Cog Rem interacts with psychosocial interventions is a crucial next step in this area of research.
The Wykes et al. (2011) meta-analysis identified ten studies that provided Cog Rem in addition to other rehabilitation services. These interventions ranged widely from vocational rehabilitation (e.g., Bell et al., 2005; Lindenmayer et al., 2008; McGurk et al., 2005, 2007), to social cognitive training groups (Hogarty et al., 2004), with only two studies combining Cog Rem with social skills training (SST) (Spaulding et al., 1999; Silverstein et al., 2009). Neither of these studies used an active control condition for the Cog Rem program.
SST, which includes modelling, behavioral rehearsal through role-plays, and positive and corrective feedback aimed at teaching more effective interpersonal skills, is an evidence-based intervention that has been recommended as a key treatment for schizophrenia by the Patient Outcomes Research Team (PORT) guidelines in the US (Dixon et al., 2010). A meta-analysis of 22 controlled studies of SST demonstrated large effect-size improvements for SST on tests of content mastery of skills taught directly in treatment sessions (d=1.20), moderate size effects on role-play measures of social and daily living skills (d=.52), other-rated measures of psychosocial function (d=.52) and negative symptoms (d=.40), and a small size effects for other symptoms (d=.15) and relapses (d=.23; Kurtz & Mueser, 2008).
However, not all individuals with schizophrenia benefit equally from SST. One major impediment to the acquisition of social skills is neurocognitive deficits. A recent review found that in seven out of eight studies impaired neurocognitive functioning was a rate-limiting factor for the acquisition of skills taught in SST (Kurtz, 2011). Several studies have also reported that impairments in neurocognition adversely influence treatment process variables such as treatment attendance, attention, and other indices of group engagement (Kern et al., 1992; McKee et al., 1997; Granholm et al., 2008). These findings support the hypothesis that improving cognitive skills may facilitate benefit for more people from SST.
We report the results of a randomized controlled trial evaluating the effects of computer-assisted Cog Rem targeting specific domains of cognitive functioning compared to an active control condition of instruction in computer skills (Computer Skills), with participants in both programs also receiving standardized social skills training (SST). This is the first study, to our knowledge, to assess the specificity of effects of Cog Rem for facilitating response to SST by including a comparison group that controls for non-specific treatment factors related to learning skills on a computer with an active control condition. Previous work from our laboratory revealed that our approach to Cog Rem produced improvements in attention and working memory that were greater than those produced by the Computer Skills program employed in the current study (see Kurtz et al., 2007).
Our primary hypotheses were: (1) individuals in the SST + Cog Rem condition would improve more in attention and working memory than those in SST + Computer Skills, consistent with our previous work (Kurtz et al., 2007); and (2) Cog Rem treatment effects would augment the effects of SST on performance-based measures of social skills, as well as ratings of psychosocial function.
Methods
Design
Study procedures were approved by appropriate institutional review boards and all participants provided written, informed consent. Participants were entered into a standardized program of social-skills training and were randomly assigned to one of the two treatment groups (Cog Rem or Computer Skills) after baseline assessments by a member of the unit clinical team who was not involved in pre- or post-training assessment, scoring or data analysis. This team member was instructed not to disclose group assignments to members of the assessment team.
Participants
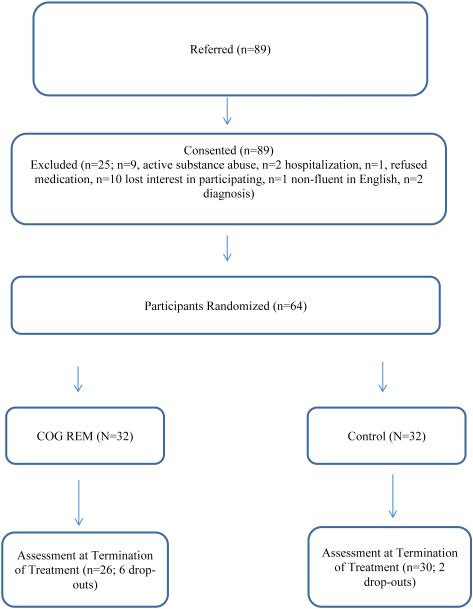
Sixty-four outpatients participated (see Table 1 for a summary of demographic, clinical, and treatment characteristics). Inclusion criteria included meeting DSM-IV (APA, 1994) criteria for schizophrenia or schizoaffective disorder, as confirmed by the Structured Clinical Interview for DSM-IV (First et al., 1995), and expressed desire to improve work or social functioning. Exclusion criteria were uncorrected auditory or visual impairment, intellectual disability as evidenced by a documented history of services, traumatic brain injury with a sustained loss of consciousness, presence or history of any neurologic illness, lack of proficiency in English, or current substance abuse or dependence. Recruitment for the study occurred over a period of six years (2007-2013) at two sites. The majority of the study participants were recruited from an intensive outpatient program for patients with schizophrenia at The Institute of Living in Hartford, CT (n=43; 77%), with the remainder recruited from a community mental health center in East Hartford, CT (n=13; 23%). See Figure 1 for the CONSORT diagram detailing the flow of participants through the study.
Table 1.
Cognitive remediation and social skills training curricula.
| Cognitive Remediation | Social-Skills Training | |
|---|---|---|
| Treatment Schedule | Fifty minutes per day, three days per week for target of 23 weeks or 69 sessions (50 hours). |
Fifty minutes per day, two days per week for target of 23 weeks or 46 sessions. |
| Treatment Curriculum |
Visual and Auditory Attention
Tone Discrimination I (Bracy, 2008), Simple Visual Reaction Time (Bracy, 1995), Simple Auditory Reaction Time (Bracy, 1995), Simple Choice Reaction Time Visual (Bracy, 1995), Simple Choice Reaction Time Auditory (Bracy, 1995). Progressive Attention Training-Respond to a Selected Color (Loong, 1988). Set Switching and Inhibition Stroop Effects I and II (Bracy, 2008) Progressive Attention Training- Alternate Black and Red by a Signal (Loong, 1988) Working Memory Sequenced Recall Digits Auditory (Bracy, 1995), Sequenced Recall Digits Visual (Bracy, 1995), Sequenced Recall Words Visual (Bracy, 1995), Sequenced Recall Graphics (Bracy. 1995). Verbal and Non-Verbal Learning and Memory Verbal Memory Categorizing (Bracy, 1995), Objects and Locations (Bracy, 2008), Colormatch (Bracy, 2008). Problem Solving Pyramids (Bracy, 2008), Simply Logical (Bracy, 2008), Matrix Deduction (Bracy, 2008), Nines All Around (Bracy, 2008). |
Basic Communication Skills
Expressing positive feelings Listening to others Expressing upset feelings constructively Conversation skills Starting a conversation with a new person Maintaining conversations by asking questions Maintain conversations by expressing feelings Staying on the topic set by another person Deciding how much to disclose Ending conversations Assertiveness Skills Asking for information Asking for help Refusing requests Getting your point across without arguing Making complaints Responding to complaints Understanding the other person’s perspective Compromise and Negotiation Leaving stressful situations. Friendship Skills Giving compliments Accepting compliments Finding common interests Asking someone to do something Making someone happy (Bellack, Mueser, Gingerich, & Agresta, 2004) |
Figure1.
CONSORT diagram.
Measures
Participants were assessed before and after SST on a brief neurocognitive test battery, a performance-based measure of social skill, and a measure of psychosocial function administered by trained research assistants who were blind to the intervention condition of the participants. All assessment and scoring was supervised by a doctoral-level psychologist.
Neurocognitive Assessment
Participants were administered a neuropsychological test battery including the Vocabulary, and the Digit Span subtests from the Wechsler Adult Intelligence Scale-III or IV (WAIS-III and IV; Wechsler, 1997; 2008), the Penn Continuous Performance Test (PCPT; Rosvold et al., 1956; Kurtz et al., 2001); the California Verbal Learning Test-II (Delis et al., 2000), and the Penn Conditional Exclusion Test (PCET; Kurtz et al., 2004). For the PCPT, the mean total true positives was selected as a dependent measure. For the CVLT-II, performance on trials 1 through 5 was selected as the dependent measures. For the PCET, the total number of errors was selected for analysis. Raw scores were converted to z-scores using published (CVLT-II, WAIS-III or WAIS-IV) or local (PCPT) normative data. Normative data were not available for the PCET so scores were transformed into z-scores using the mean and SD of scores obtained from study participants. Measures were selected based on their relationships with functional status in previous studies of schizophrenia (e.g., Green et al., 2000; 2004) and are a representative subgroup of the five separable factors underlying cognition in schizophrenia and consistent with the domains of MATRICS (e.g., Nuechterlein et al., 2008).
Social Skills Performance Assessment (SSPA; Patterson et al., 2001)
The SSPA is a standardized, brief assessment of social skill consisting of two 3-minute social role-plays in which the participant plays the role of: (1) a tenant meeting a new neighbor, and (2) a tenant reporting a leak in their household for a second time to a landlord. Interactions were audiotaped and rated on a variety of dimensions of social skill, including interest/disinterest, fluency, clarity, focus and affect, and social appropriateness. Training on the measure was conducted in consultation with the Department of Psychiatry at UCSD and blind scoring was conducted at UCSD or by trained local raters (ICC=.7).
Quality of Life Scale-Brief (QLS-B; Bilker et al., 2003)
The QLS-B is an abbreviated version of the QLS (Heinrichs et al., 1984), a semi-structured interview-based assessment that evaluates the quality of the individual’s psychosocial adjustment in areas such as role functioning and social relationships. The 7-item QLS-B is highly correlated with the total scores on full QLS in schizophrenia samples (r=.98; Bilker et al., 2003). Through ratings of practice videotapes all raters in the study maintained an ICC of .7 on the QLS-B. We analyzed total scores as well as the three QLS-B item ratings that most closely reflected the content of the SST curriculum selected for the current study: empathy, number of active social acquaintances, and social initiation.
The success of the blinding procedures for these outcome measures was evaluated by asking research assistants to guess the condition of participants at the time of their follow-up in half of the participants in the study (n=28). Accurate assessment of group membership was at exact chance levels (50%) for these participants.
Treatments
All participants received SST and were randomly assigned to concurrently receive either Cog Rem or Computer Skills training.
Social Skills Training
Group SST was provided in twice per week in 50-minute sessions (total: 46 sessions) over 4-6 months. The curriculum focused on conversation, assertiveness, and friendship skills (Bellack et al., 2004; see Table 1). The second co-author (KTM) lead an introductory training session in SST and day-to-day supervision of groups was conducted by the lead author (MMK). All sessions were audiotaped and tapes were periodically selected randomly and mailed to KTM for fidelity review. Review of tapes revealed high levels of treatment fidelity. Exposure to the SST program was defined as attending at least one training session.
Cognitive Remediation
The intervention was a 4-6-month, standardized course of cognitive remediation (a target of 50 hours) consisting of a sequence of computerized cognitive exercises designed to improve attention, working memory, verbal and non-verbal episodic memory, executive-function and language processing through repeated drill-and-practice (Bracy, 1995, 1998; Seltzer et al., 1997; Bell et al., 2001; Kurtz et al., 2007). Exercises and goals were started at a level of difficulty at which all participants were successful. Goals were modified as performance improved. Components of the intervention have produced performance gains on practiced tasks (e.g., Wexler et al., 1997), generalization of improvement to other tasks (Seltzer et al., 1997; Bell et al., 2001), normalization of task-related frontal lobe activation in fMRI studies (Wexler et al., 2000), and improved work functioning when offered in combination with vocational rehabilitation (Bell et al., 2005; Bell et al., 2007). The list of exercises is presented in Table 2.
Table 2.
Mean (SD) Demographic, clinical and treatment measures for participants in the cognitive-remediation (n=26) and control (n=30) conditions.
| COG REM | Control | Test Statistic | P-value | |
|---|---|---|---|---|
| Age | 36.1 (12.8) | 37.1 (12.1) | 1.33 | .19 |
| Gender (%male) | 73% | 73% | ||
| Education | 12.5 (2.2) | 11.7 (2.2) | 1.36 | .18 |
| Duration of illness (yrs.) |
12.8 (11.8) | 12.4 (10.7) | .11 | .91 |
| Number of Hospitalizations |
5.4 (5.7) | 4.4 (3.5) | .77 | .44 |
| Positive Symptoms | 16.7 (4.5) | 18.0 (6.4) | −.86 | .39 |
| Negative Symptoms |
17.2 (5.1) | 19.8 (5.2) | −1.74 | .09 |
| General Symptoms |
36.4 (8.1) | 37.2 (6.4) | −.38 | .71 |
| Vocabulary Scaled Score (WAIS-III or IV) |
7.5 (3.7) | 7.6 (3.6) | −.10 | .92 |
| Percent on atypical antipsychotic |
86 | 81 | .70 | .42 |
Control Computer Skills Condition
Control participants received an active control intervention that consisted of a 4-6-month course of computerized tutorials in general computer literacy and specific skills in using Microsoft Office (Computer Skills). Participants in this group received a similar duration of treatment (target of 50 hours) and equivalent interaction with a clinician as those in the Cog Rem condition. These tutorials did not involve practice of exercises specifically targeting basic neurocognitive skills (e.g., attention, memory and problem-solving).
Statistical Analysis
We used an intent-to-treat analysis which included all enrolled clients, regardless of level of participation in either the SST or computer interventions. The distribution of scores for each variable in each group was inspected for normality and compared to relevant comparison groups for homogeneity of variance. First, the two groups were compared at baseline on neurocognition, social skills, and psychosocial function, and exposure to the SST and the computer interventions (Cog Rem vs. Computer Skills) using independent sample t-tests. Second, to assess changes over time in the overall sample we compared pre- vs. post-training scores of all clients using matched-pairs t-tests on measures of neurocognition, social skill, and functioning. Third, to assess differences in change between the groups on the neurocognitive, social skills performance and functioning measures we performed a series of one-way analyses of covariance (ANCOVAs) with group (Cog Rem vs. Computer Skills) as the between-subjects variable, post-training scores as the dependent measure, and pre-training assessment scores as a covariate. Lastly, to assess change in individual items from the QLS-B we ran a series of one-way ANCOVAs with group (Cog Rem vs. Computer Skills) as the between-subjects variable, post-training ratings as the dependent measure, and pre-training ratings as a covariate. All statistical tests were two-tailed and alpha was set at .05.
Results
There were no significant differences between the Cog Rem and Computer Skills groups on any variables at baseline (see Table 2). All individuals in the study received at least 1 session of SST (mean number of SST sessions=32.30; SD=12.55) and there was no difference in the number of SST sessions attended between the two groups (Cog Rem mean=31.96, SD=12.60; Computer Skills mean=32.20, SD=12.55; NS). In the Cog Rem group all individuals participated in at least one training session (Cog Rem mean number of hours=23.14, SD=12.36); whereas in the Computer Skills group 77% of individuals received at least one session of Computer Skills training (Computer Skills training mean number of hours=21.17, SD=15.62). However, the difference in number of hours of cognitive training between the two groups was not significant.
Across the entire sample there was no evidence of improvement on the cognitive measures. With respect to differences in changes between the groups, the ANCOVAs for the four neurocognitive tests showed significant improvements for participants in Cog Rem compared to Computer Skills on attention and working memory (Digit Span) (F [1, 53]=4.22, p<.05; d=.46), but not sustained visual vigilance (PCPT), verbal learning and memory (CVLT-II), or problem-solving (PCET; ds<.19; see Table 3). In terms of individual participant response in each of the two groups for the attention and working memory measure, 58% of the participants in the Cog Rem group showed at least a small-moderate (≥ .33 SD) z-score improvement, compared to 37% of those in the Computer Skills group, a significant difference (χ2=5.3, p<.05).
Table 3.
Mean pre vs. post-training scores on neurocognitive measures, performance-based social skills and other-rated rated psychosocial function.
| Variable | Group | n | Pre- training (Mean +/− SD) |
Post- training (Mean +/− SD) |
F- statistic |
p-value | Effect Size (d-value) |
|---|---|---|---|---|---|---|---|
|
Cognitive
(Proximal Measures) |
|||||||
| PCPT TP | COG REM |
24 | −1.26 (3.20) |
−1.26 (3.10) |
.09 | .76 | .18 |
| Control | 24 | −1.80 (3.10) |
−1.78 (2.73) |
||||
| Digit Span | COG REM |
26 | −.78 (.96) | −.56 (.86) | 4.22 | .045 | .46 |
| Control | 30 | −.89 (.89) | −.96 (.88) | ||||
| CVLT-II | COG REM |
25 | −1.29 (1.23) |
−1.09 (1.42) |
.01 | .937 | .15 |
| Control | 29 | −1.61 (1.22) |
−1.29 (1.27) |
||||
| PCET | COG REM |
24 | −.02 (1.17) |
−.06 (.89) | .106 | .746 | −.10 |
| Control | 26 | .03 (.89) | .04 (1.12) |
||||
|
Role-Play
Measure of Social-Skill |
|||||||
| SSPA | COG REM |
22 | 3.53 (.59) |
3.67 (.53) |
2.81 | .102 | .58 |
| Control | 21 | 3.37 (.74) |
3.35 (.57) |
||||
|
Psychosocial
Function |
|||||||
| QLS-B Total | COG REM |
23 | 19.0 (6.0) |
20.8 (6.6) |
.11 | .741 | .10 |
| Control | 25 | 18.6 (6.5) |
20.2 (4.9) |
||||
| QLS-B Empathy |
COG REM |
23 | 4.0 (1.3) | 4.2 (1.3) | 7.13 | .011 | .67 |
| Control | 25 | 3.9 (1.3) | 3.4 (1.1) | ||||
| QLS-B Active Acquaintances |
COG REM |
23 | 2.0 (2.1) | 1.7 (2.1) | 1.04 | .314 | −.14 |
| Control | 25 | 1.6 (1.9) | 2.0 (2.1) | ||||
| QLS-B Social Interaction |
COG REM |
23 | 2.5 (1.1) | 3.2 (1.7) | 1.52 | .224 | .24 |
| Control | 25 | 2.5 (2.0) | 2.8(1.7) |
Note: COG REM=Cognitive Remediation; PCPT=Penn Continuous Performance Test, CVLT-ll=California Verbal Learning Test-II, PCET=Penn Conditional Exclusion Test, SSPA=Social=Skill Performance Assessment; QLS-B=Quality-of-Life Scale, Brief version.
Across the entire sample the social skills performance measure (SSPA) did not significantly improve from pre- to post-training. The ANCOVA comparing the groups on the social skills measure (SSPA) was also not significant (see Table 3). Paired t-tests revealed improvement from pre to post-training in total QLS-B scores for the entire sample (t=2.11; p<.05), and on the social initiation item from the QLS-B (t=2.35; p<.05). Group comparisons of total scores and individual items related to social functioning from the QLS-B scale showed that individuals in the Cog Rem group improved more in empathy than those in the Computer Skills group (F[1,45]=7.13, p=.011; d=.67) (see Table 3). Other selected items from the QLS-B and the total score did not differ between the groups (ds<.25).
Discussion
This study is unique in its use of a cognitively active control group (Computer Skills) to evaluate the specific effects of augmenting an SST intervention with an abbreviated version of a standardized program of drill-and-practice cognitive remediation with demonstrated efficacy in previous, randomized controlled trials (Bell et al., 2001; Kurtz et al., 2007). Several key findings emerged. First, participants who received Cog Rem improved significantly more in attention and working memory (Digit Span) than those who received training in computer skills, similar to our previous research (Kurtz et al., 2007). Thus, remediation-linked improvements in working memory in this study suggest that neurocognitive training in skills related to holding information in mind and manipulating that information can be improved in individuals with schizophrenia. Given the careful matching of the control condition with the Cog Rem intervention (e.g., on exposure to the computer, interaction with the clinician, and the non-specific cognitive activation associated with learning new content), these findings suggest that unique aspects of the Cog Rem intervention may have contributed to greater improvements in working memory, such as the extensive task practice on exercises related directly to attention and working memory that comprise the first two modules of our Cog Rem program (see Table 1) .
There was overall improvement in the sample on a global measure of psychosocial function (the QLS-B) as well as on a rating of skills in social initiation. However, contrary to our hypotheses, participants who received Cog Rem did not show greater increases in a role play test of social skill or overall psychosocial functioning measured on the QLS-B. These findings are different from those that have evaluated the effects of Cog Rem as a potentiator of work outcomes in supported employment (e.g., McGurk et al., 2005, 2007). Partially consistent with our hypotheses, there was some evidence of generalization of Cog Rem training effects to an interview-based measure of interpersonal functioning targeted in the SST program: participants in Cog Rem improved more on empathy on the QLS-B than those in Computer Skills. These findings suggest that Cog Rem may have augmented attention and working memory skills that contributed to improved social cognition related to understanding another person’s feelings and perspective. The SST group may have provided critical opportunities for clients to improve their empathy skills based on the teaching approach that emphasizes group members both actively rehearsing communication skills in role plays and honing their performance based on feedback, and providing positive, specific feedback to other members regarding their performance in similar role plays. Greater improvements in sustained attention and working memory for participants in Cog Rem may have facilitated greater learning of emotion recognition and empathy during role play practice and feedback from other SST group members and the group leader.
Social skill performance on the SSPA did not improve significantly after treatment for the overall sample, reducing our ability to evaluate the differential benefit of Cog Rem vs. Computer Training on improved skill acquisition. The SSPA involved one role play of initiating a conversation with a new neighbor and another reporting a problem to a landlord. It is possible that the SSPA was either too brief or did not sufficiently tap the primary focus of the SST group on improving relationships with others and friendships.
The size (d=.46) and range of Cog Rem training effects in this study were smaller than those reported in some other studies (e.g., Fisher et al., 2009). Both the limited duration of treatment and the selection of an active control group that reflected the effects of factors beyond expectation alone, such as cognitive challenge, and has produced improvements in cognitive function in previous studies (Kurtz et al., 2007) may partly account for these differences.
Several limitations to the current study should be mentioned. First, participants in the Cog Rem and Computer Skills groups received approximately one-third the number of hours of training compared to our previous work [i.e., a mean of 23 hours for Cog Rem and 22 hours for Computer Skills in this study vs. a mean of 67 and 70 hours, respectively, in Kurtz et al. (2007)]. Stronger effects would likely have been detected with a larger average dose of training. These study differences however, underscore the robustness of the reported Cog Rem gains in working memory and their generalization to measures of empathy in the current report.
Second, the type of Cog Rem selected for the current study did not attempt to directly link the practice of targeted cognitive skills to the learning of social skills in the SST group or their role in everyday social interactions, a feature present in other forms of Cog Rem (e.g., Bowie et al., 2012; McGurk et al., 2005), which may have limited the generalization of the effects of this intervention. Third, the simultaneous administration of Cog Rem and SST may have limited the influence of acquired cognitive skills on acquisition of elementary social skills in SST by providing insufficient time for the application of those cognitive skills in the SST groups. Fourth, the durability of these observed effects of the combined Cog Rem and SST program on attention and working memory and empathy were not evaluated.
In summary, adding cognitive remediation to SST treatment improved working memory relative to an active control condition, with the generalization of effects evident on a measure of empathy. There were no differences between groups on a performance-based measure of social skill, or on other aspects of psychosocial functioning. Future studies aimed at evaluating the role of Cog Rem in enhancing response to SST in people with schizophrenia should ensure that study sample sizes are sufficiently large to detect the effects of both interventions and assess the durability of observed effects after termination of these interventions. Such studies will help elucidate the relationships between these two evidence-based psychosocial interventions for schizophrenia and will provide guidance for the appropriate administration of Cog Rem for those clients least likely to benefit from SST and other evidence-based psychosocial treatments in resource-limited clinical services. Such information will provide a crucial rationale for bridging the gap between the application of Cog Rem in research studies and the uptake of this practice in its most efficient form into clinical services.
Acknowledgements
This work was supported by grant K08 MH-69888 from the National Institute of Mental Health (NIMH), a Young Investigator Award from the National Alliance for Research on Schizophrenia and Depression (NARSAD) and gifts from the Spencer T. and Anne W. Olin Foundation to the Institute of Living, Hartford Hospital’s Mental Health Network.
Role of funding source
The funding sources for this study had no role in the study design, collection, analysis or interpretation of the data, the writing of the report and in the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors report no conflicts-of-interest in the conduct or preparation of this study.
References
- American Psychiatric Association . DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Fourth American Psychiatric Association; Washington, D.C: 1994. [Google Scholar]
- Bell MD, Bryson G. Work rehabilitation: does cognitive impairment limit improvement. Schizophrenia Bulletin. 2001;27:269–279. doi: 10.1093/oxfordjournals.schbul.a006873. [DOI] [PubMed] [Google Scholar]
- Bell M, Bryson G, Greig T, Corcoran C, Wexler BE. Neurocognitive enhancement therapy with work therapy: effects on neuropsychological test performance. Archives of General Psychiatry. 2001;58:163–168. doi: 10.1001/archpsyc.58.8.763. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Mueser KT, Gingerich S, Agresta J. Social Skills Training for Schizophrenia: A Step-by-Step Guide (2nd ed.) New York, NY; The Guilford Press: 2004. [Google Scholar]
- Bilker WB, Brensinger C, Kurtz MM, Kohler C, Gur RC, Siegel SJ, Gur RE. A method for abbreviating assessment scales: The schizophrenia quality of life scale. Neuropsychopharmacology. 2003;28:773–777. doi: 10.1038/sj.npp.1300093. [DOI] [PubMed] [Google Scholar]
- Bowie CR, Depp C, McGrath JA, Wolyniec P, Mausbach BT, Thornquist MH, Luke J, Patterson TL, Harvey PD, Pulver AE. Prediction of real-world functional disability in chronic mental disorders: a comparison of schizophrenia and bipolar disorder. American Journal of Psychiatry. 2010;167:1116–1124. doi: 10.1176/appi.ajp.2010.09101406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. American Journal of Psychiatry. 2012;169:710–718. doi: 10.1176/appi.ajp.2012.11091337. [DOI] [PubMed] [Google Scholar]
- Bracy O. PSS CogRehab, Version 95. Psychological Software Services, Inc.; Indianapolis, IN: 1995. [Google Scholar]
- Bracy O. NeuropsychOnline. Psychological Software Services, Inc.; Indianapolis, IN: 2008. [Google Scholar]
- Dickinson D, Bellack AS, Gold JM. Social/communication skills, social and vocational functioning in schizophrenia. Schizophrenia Bulletin. 2007;33(5):1213–1220. doi: 10.1093/schbul/sbl067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kramer JH, Kaplan E, Ober BA. CVLT-II. The Psychological Corporation; New York: 2000. [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin. 2010;36:48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0) Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Fisher M, Holland C, Merzenich MM, Vinogradov S. Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. American Journal of Psychiatry. 2009;166:805–811. doi: 10.1176/appi.ajp.2009.08050757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granholm E, McQuaid JR, Link PC, Fish S, Patterson T, Jeste DV. Neuropsychological predictors of functional outcome in Cognitive Behavioral Social Skills Training for older people with schizophrenia. Schizophrenia Research. 2008;100:133–143. doi: 10.1016/j.schres.2007.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold JM, Hahn B, Strauss GP, Waltz JA. Turning it upside down: areas of preserved cognitive functioning in schizophrenia. Neuropsychology Review. 2009;19:294–311. doi: 10.1007/s11065-009-9098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the "right stuff"? Schizophrenia Bulletin. 2000;26(1):119–36. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: Implications for MATRICS. Schizophrenia Research. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophrenia Bulletin. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: A quantitative review of the evidence. Neuropsychology. 1998;12(3):426–445. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- Hogarty GE, Flesher S, Ulrich R, Carter M, Greenwald D, Pogue-Geile M, Keshavan M, Cooley S, DiBarry AL, Garrett A, Parepally H, Zoretich R. Cognitive enhancement therapy for schizophrenia: Effects of a two-year randomized controlled trial on cognition and behavior. Archives of General Psychiatry. 2004;61:866–876. doi: 10.1001/archpsyc.61.9.866. [DOI] [PubMed] [Google Scholar]
- Irani F, Kalkstein S, Moberg EA, Moberg PJ. Neuropsychological performance in older patients with schizophrenia: a meta-analysis of cross-sectional and longitudinal studies. Schizophrenia Bulletin. 2011;37:1318–1326. doi: 10.1093/schbul/sbq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz MM. Neurocognition as a predictor of response to evidence-based psychosocial interventions in schizophrenia: What is the state of the evidence? Clinical Psychology Review. 2011;31:663–672. doi: 10.1016/j.cpr.2011.02.008. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern RS, Green MF, Satz P. Neuropsychological predictors of skills training for chronic psychiatric patients. Psychiatry Research. 1992;43:223–230. doi: 10.1016/0165-1781(92)90055-8. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Mueser KT. Social skills training for schizophrenia: A meta-analysis of controlled research. The Journal of Consulting and Clinical Psychology. 2008;76:491–504. doi: 10.1037/0022-006X.76.3.491. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Ragland JD, Bilker W, Gur RC, Gur RE. Comparison of the continuous performance test with and without working memory demands in healthy controls and patients with schizophrenia. Schizophrenia Research. 2001;48(2-3):307–316. doi: 10.1016/s0920-9964(00)00060-8. [DOI] [PubMed] [Google Scholar]
- Kurtz MM, Seltzer JC, Shagan DS, Thime WR, Wexler BE. Computer-assisted cognitive remediation in schizophrenia: What is the active ingredient? Schizophrenia Research. 2007;89:251–260. doi: 10.1016/j.schres.2006.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurtz MM, Wexler BE, Bell MD. The Penn Conditional Exclusion Test (PCET): Relationship to the Wisconsin Card Sorting Test and work function in patients with schizophrenia. Schizophrenia Research. 2004;68:95–102. doi: 10.1016/S0920-9964(03)00179-8. [DOI] [PubMed] [Google Scholar]
- Lindenmayer JP, McGurk SR, Mueser KT, Khan A, Wance D, Hoffman L, Wolfe R, Xie H. Psychiatric Services. 2008;59:241–247. doi: 10.1176/ps.2008.59.3.241. [DOI] [PubMed] [Google Scholar]
- Loong J. Progressive Attention Training. Wang Neuropsychological Laboratory; 1988. [Google Scholar]
- McGurk SR, Mueser KT. Cognitive functioning and employment in severe mental illness. Journal of Nervous and Mental Disease. 2003;191(12):789–98. doi: 10.1097/01.nmd.0000100921.31489.5a. 2003. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, Covell NH, Cicerone KD, Drake RE, Silverstein SM, Medalia A, Myers R, Bellack AS, Bell MD, Essock SM. Mental health system funding of cognitive enhancement interventions for schizophrenia: Summary and update of the New York Office of Mental Health Expert Panel and Stakeholder Meeting. Psychiatric Rehabilitation Journal. 2013;36:133–45. doi: 10.1037/prj0000020. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A. Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial. American Journal of Psychiatry. 2007;164:437–41. doi: 10.1176/ajp.2007.164.3.437. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, Pascaris A. Cognitive training and supported employment for persons with severe mental illness: One year results from a randomized controlled trial. Schizophrenia Bulletin. 2005;31:898–909. doi: 10.1093/schbul/sbi037. [DOI] [PubMed] [Google Scholar]
- McKee M, Hull JW, Smith TE. Cognitive and symptom correlates of participation in social skills training groups. Schizophrenia Research. 1997;23:223–229. doi: 10.1016/s0920-9964(96)00090-4. [DOI] [PubMed] [Google Scholar]
- Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: a meta-analytic review. Neuropsychology. 2009;23:315–336. doi: 10.1037/a0014708. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Bellack AS, Douglas MS, Wade JH. Prediction of social skill acquisition in schizophrenic and major affective disorder from memory and symptomatology. Psychiatry Research. 1991;37:281–296. doi: 10.1016/0165-1781(91)90064-v. [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, Essock S, Frese F, Gold J, Goldberg T, Heaton RK, Keefe RS, Kramer H, Mesholam-Gately R, Seidman LJ, Stover E, Weinberger D, Zalcman S, Marder SR. The MATRICS consensus cognitive battery: part 1: tests selection, reliability and validity. American Journal of Psychiatry. 2008;165:203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Moscona S, McKibben CL, Davidson K, Jeste DV. Social skills performance assessment among older patients with schizophrenia. Schizophrenia Research. 2001;48:351–360. doi: 10.1016/s0920-9964(00)00109-2. [DOI] [PubMed] [Google Scholar]
- Rosvold HE, Mirsky A, Sarason I, Bransome ED, Beck LH. A continuous performance test of brain damage. The Journal Consulting and Clinical Psychology. 1956;20:343–350. doi: 10.1037/h0043220. [DOI] [PubMed] [Google Scholar]
- Seltzer J, Cassens G, Ciocca C, O’Sullivan L. 1997 [PubMed] [Google Scholar]
- Silverstein SM, Spaulding WD, Menditto AA, Savitz A, Liberman RP, Berten S, Starobin H. Attention shaping: a reward-based learning method to enhance skills training outcomes in schizophrenia. Schizophrenia Bulletin. 2009;35:222–232. doi: 10.1093/schbul/sbm150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaulding WD, Reed D, Sullivan M, Richardson C, Weiler M. Effects of cognitive treatment in psychiatric rehabilitation. Schizophrenia Bulletin. 1999;25(4):657–676. doi: 10.1093/oxfordjournals.schbul.a033409. [DOI] [PubMed] [Google Scholar]
- Ucok A, Cakir S, Duman ZC, Discgil A, Kandemir P, Atli H. Cognitive predictors of skill acquisition in social problem solving in patients with schizophrenia. European Archives Psychiatry Clinical Neuroscience. 2006;256:388–394. doi: 10.1007/s00406-006-0651-9. [DOI] [PubMed] [Google Scholar]