Abstract
Objectives
The aim of the present study was to assess human and bacterial peptidylarginine deiminase (PAD) activity in the gingival crevicular fluid (GCF) in the context of serum levels of antibodies against citrullinated epitopes in rheumatoid arthritis and periodontitis.
Materials and Methods
Human PAD and Porphyromonas gingivalis-derived enzyme (PPAD) activities were measured in the GCF of 52 rheumatoid arthritis (RA) patients (48 with periodontitis and four without) and 44 non-RA controls (28 with periodontitis and 16 without). Serum antibodies against citrullinated epitopes were measured by ELISA. Bacteria being associated with periodontitis were determined by nucleic-acid based methods.
Results
Citrullination was present in 26 (50%) RA patients and 23 (48%) controls. PAD and PPAD activities were detected in 36 (69%) and 30 (58%) RA patients, respectively, and in 30 (68%) and 21 (50%) controls, respectively. PPAD activity was higher in RA and non-RA patients with periodontitis than in those without (p = 0.038; p = 0.004), and was detected in 35 of 59 P. gingivalis positive samples, and in in 16 of 37 P. gingivalis-negative samples in association with high antibody levels against that species.
Conclusions
PAD and PPAD activities within the periodontium are elevated in RA and non-RA patients with periodontitis. PPAD secreted by P. gingivalis residing in epithelial cells may exert its citrullinating activity in distant regions of the periodontium or even distant tissues.
Clinical relevance
In periodontitis, the citrullination of proteins/peptides by human and bacterial peptidylarginine deiminases may generate antibodies after breaching immunotolerance in susceptible individuals.
Keywords: periodontitis, rheumatoid arthritis, citrullination, Porphyromonas gingivalis, citrullinated peptides antibodies
Introduction
The relationship between periodontitis and rheumatoid arthritis (RA) has gained increasing interest in recent years. In contrast to large epidemiological studies finding a weak association between these two diseases [1, 2], many well design pointed investigations show that periodontitis is more prevalent in patients with RA than in those without [3, 4], and conversely, the prevalence of RA is high among periodontitis patients [5]. Furthermore, patients undergoing treatment for RA show improved periodontal indices [6], and the disease activity of RA decreases after periodontal therapy [7, 8].
RA and periodontitis are chronic inflammatory diseases that share several pathological features, including bone and tissue destruction and high levels of inflammatory markers [9]. Exposure to common genetic or environmental factors (e.g., smoking) may contribute to a non-causal association between these two diseases [10].
RA is an immune mediated multigenic arthritis of unknown origin characterized by the presence of disease-specific autoantibodies against citrullinated proteins [11, 12]. Citrullination is the post-translational modification of arginine residues in polypeptides (peptidylarginine) into citrulline residues. The reaction is catalyzed by a family of five peptidylarginine deiminases (PADs), among which PAD-2 and PAD-4, which are expressed in joints, are important in RA [12, 13].
Porphyromonas gingivalis, a gram-negative anaerobic bacterium, is an important etiological agent in chronic periodontal disease [14]. Cysteine proteases, referred to as gingipains, are the main virulence factors of P. gingivalis [15]. While arginine-specific gingipains (RgpA and RgpB) are encoded by two genes (rgpA and rgpB), a lysine-specific enzyme is a product of a single gene (kgp) [16]. In addition, P. gingivalis is the only human pathogen, which produces the unique PAD (PPAD) [17, 18], also considered as a virulence factor. Because of the PPAD expression P. gingivalis was proposed as the principal link between periodontitis and RA [19]. The levels of antibodies against P. gingivalis are elevated in patients with RA [20, 21]. Recent work from our group showed that bacterial endogenous citrullination is abundant in P. gingivalis and absent in other oral bacteria, and that PPAD citrullinates fibrinogen and α-enolase, which are major autoantigens in RA [22].
The purpose of the present study was to quantify the activities of citrullinating enzymes derived from both host and P. gingivalis in gingival crevicular fluid (GCF). To determine the contribution of P. gingivalis to the autoimmune character of RA in the context of periodontitis, the PAD and PPAD activities in GCF were correlated with the presence of P. gingivalis and serum antibody levels against citrullinated proteins/peptides in RA patients and non-RA individuals with and without periodontitis.
Materials and methods
Subjects and clinical data
RA patients were recruited from the Department of Rheumatology, Clinical Immunology and Allergology of the University Hospital of Bern (Bern, Switzerland). Patients with chronic periodontitis were enrolled from the Department of Periodontology, University of Bern. Age-matched patients without periodontitis from the Department of Preventive, Restorative and Pediatric Dentistry, School of Dental Medicine, University of Bern completed the study cohort. The study was conducted in accordance with ethical principles, including those established by the World Medical Association Declaration of Helsinki (version 2008). All individuals signed a written informed consent before participating in the study. The study protocol was reviewed and approved by the Ethical Committee of the Canton Bern, Switzerland (KEK approval #236/10). Exclusion criteria were pregnancy and lactation, uncontrolled medical conditions, systematic periodontal treatment within the last 6 months, the use of antibiotics within the last 3 months. However, supportive periodontal therapy including supragingival tooth cleaning and, if needed, localized subgingival debridement, was not an exclusion criterion.
All subjects were Caucasian and 18 years or older. All patients with RA met the 2010 Rheumatoid Arthritis Classification Criteria of the American College of Rheumatology/European League Against Rheumatism Collaborative Initiative [23].
Epidemiologic and anamnestic data [gender, age, smoking, disease activity 28 (DAS28)-erythrocyte sedimentation rate (ESR), medications, and duration of RA] were recorded. All participants were examined by an experienced specialist in periodontology (O.L.) and assigned a Periodontal Screening and Recording Index (PSR) [24]. Individuals with a PSR score ≥3 (probing depth ≥3.5 mm, plaque or calculus accumulation, and bleeding on probing) in at least two sextants were grouped as periodontitis patients (PER). Severe periodontitis was defined by a PSR of 4 (Probing depth ≥5.5 mm, plaque or calculus accumulation, and bleeding on probing). Pseudopockets were excluded from the diagnosis of periodontitis. GCF and peripheral blood samples were collected.
Sampling of serum and GCF
Venous blood samples (10 ml) were obtained and centrifuged at 400 g for 10 min, and serum was stored at − 20°C until analysis.
Crevicular washes were obtained using a previously described method [25]. In each patient, the four deepest sites were chosen. A gel-loading capillary tip was carefully inserted into the crevice at a level approximately 1 mm below the gingival margin. Sequential washes with 15 μl of 0.9% sodium chloride (two per site) were performed using a micropipette. Washes were pooled and transferred into a microcentrifuge tube, immediately frozen, and kept at − 20°C until analyzed. All samples containing blood were discarded.
Microbiological analysis
DNA was extracted from 5 μl of the pooled GCF washes using the Chelex method [26]. Five periodontopathogens (Aggregatibacter actinomycetemcomitans, P. gingivalis, Tannerella forsythia, Treponema denticola, and Prevotella intermedia) were detected using the microIDent® (Hain Lifescience, Nehren, Germany) according to the manufacturer’s instructions. P. gingivalis was analyzed by real-time PCR as described recently [27].
Activities of citrullinating enzymes
Human PAD activity was analyzed with the Antibody Based Assay for PAD (ABAP) (Modiquest Research, Nijmegen, Netherlands) according to the manufacturer’s instructions. Briefly, 1 μl of GCF was dissolved in 100 μl of deamination buffer. Recombinant human PAD4 was used to generate an activity calibration curve, and 2.0–0.002 mU of human PAD4 was used for the standard curve. Absorbance was measured at 450 nm.
The presence of citrulline and PPAD activity was determined using the modified Boyde and Rahmatullah method [28], which is based on the chemical modification of the citrulline side chain and colorimetric detection of the derivative. To measure the basic levels of citrullination and PPAD enzymatic activity, 2 μl of GCF in 8 μl of phosphate buffered saline (PBS) was pipetted into each well of 96-well plates, then 40 μl of 10 nM N-Ac-L-Arg-OH (Sigma-Aldrich, St. Louis, MO, USA) in 0.1 M Tris and 5 mM DTT was added, and the plate was incubated at 55°C. Of note, human PADs are inactive against C-terminal arginine residues and do not deiminate the Arg residue in Ac-Arg-OH. To measure the basal level of citrullination in GCF samples, 40 μl of PBS was added instead of the substrate, and the sample was immediately treated with 10 μl of 5 M HClO4. This basal level of citrullination in crevicular fluid is due to the presence of citrullinated proteins/peptides and free citrulline generated by arginine deiminases, a group of enzymes distinct from PAD/PPAD that acts only on free arginine residues. After 1 h of incubation, 10 μl of 5 M HClO4 was added to stop the enzymatic reaction. For color development, 150 μl of a freshly prepared 1:2 mixture of solution A (0.5% diacetyl monoxime and 0.01% thiosemicarbazide in water) and B (0.25 mg/ml of FeCl3 in 24.5% H2SO4 and 17% H3PO4 in water) was added to each well and incubated at 110°C for 17 min. The optical density (OD) at 535 nm was measured using a SpectraMax microplate reader (Molecular Devices, Sunnyvale, CA, USA). The OD read-out was converted to μmol of citrulline using a calibration standard curve prepared using free L-citrulline at 1–100 nmol per well and developed accordingly on the 96-well plate. For each sample, the background (basal) citrulline level was subtracted from the read-out with the substrate, and the resulting value represented the PPAD activity in the sample. One enzymatic unit was defined as the production of 1 μmol of citrulline in 1 h at 55°C.
Antibodies in serum
Anti-cyclic citrullinated peptide (CCP) antibodies were evaluated using an anti-CCP ELISA test kit (Euro Diagnostica, Sweden) according to the manufacturer’s instructions. Antibodies against gingipain (RgpB), citrullinated and non-citrullinated forms of vimentin, fibrinogen, and enolase were determined by a previously described ELISA method [29, 30]. Briefly, 96-well plates were coated overnight at 4°C with antigen diluted to 10 μg/ml (except for RgpB at 5 μg/ml) with coating buffer. After washing and blocking for 2 h, serum samples were diluted 1:100, and incubated for 1.5 h at room temperature. Plates were washed and incubated with peroxidase-conjugated mouse anti-human IgG (Hybridoma Reagent Laboratory, Baltimore, USA) (1:3000) in RIA buffer for 1 h at room temperature. After a final wash, tetramethylbenzidine substrates (KPL, Gaithersburg, USA) were added to detect the bound antibodies. H2SO4 (1 M) was added to stop the reaction, and the absorbance was measured at 450 nm. Samples were analyzed in duplicate. A standard curve, as a reference control, was constructed for each of the citrullinated peptides, expressed as U/ml. Arbitrary units/ml were used for antibodies against RgpB, as no standard curve was available.
Statistics
Although there were no data about the presence of citrullinated proteins in GCF available at the beginning of the study, a power analysis was performed by using a study which determined the presence of citrullinated proteins in serum of RA patients with and without periodontitis [31]. Based on the data of that study where 5 of 13 patients without periodontitis and 4 of 55 with periodontitis were negatively tested for citrullinated proteins, our study with p of 0.05 and a power of 0.8 would need a total number of 56 patients. Statistical analysis was performed using PASW 21.0 (SPSS Statistics, IBM Corporation, New York, USA). The Chi2-test was used to compare qualitative data. Quantitative data were compared with non-parametric tests. The Mann–Whitney test was used to analyze differences between independent groups, and associations between variables were determined by Spearman correlation. The level of significance was set to p=0.05.
Results
Study cohort
The study included 52 patients with RA who underwent a thorough periodontal examination. Of these patients, four had a healthy periodontium (RA/non-PD), and the remaining 48 were diagnosed with periodontal disease (RA/PD) ranging from mild to severe periodontitis. The DAS28ESR score of RA patients was 2.73 ± 1.27 and 3.19 ± 1.49 in the RA/non-PD and RA/PD groups, respectively, with no significant difference in the current inflammatory RA disease severity between the two groups. There was no significant difference between the groups in the disease duration (8.75 ± 12.84 and 16.69 ± 11.24 years in the RA/non-PD and RA/PD groups, respectively). Of 44 controls without RA (non-RA), 28 had periodontitis (non-RA/PD) and 16 did not (non-RA/non-PD). Epidemiologic data are presented in Table 1.
Table 1.
Epidemiologic data of the rheumatoid arthritis (RA) and non-RA patients
| RA | non-RA | |
|---|---|---|
| N | 52 | 44 |
| Age (years, mean±SD) | 57±11 | 53±12 |
| Gender (male/female) | 11/41 | 18/26 |
| Smokers (no/yes/former) | 37/11/4 | 26/15/3 |
| Periodontitis (no/yes) | 4/48 | 16/28 |
| DAS28CRP | 2.63±1.28 | n.a. |
| DAS28ESR | 3.14±1.46 | n.a. |
| Disease duration (years, mean±SD) | 16±11 | n.a. |
| Corticosteroids (n/%) | 12 (23%) | n.a. |
| Synthetic DMARDs (n/%) | 32 (62%) | n.a. |
| Biological DMARDs (n/%) | 33 (63%) | n.a. |
DAS28CRP, DAS28ESR: Disease activity score of rheumatoid arthritis based on 28 joints and C-reactive protein (CRP)-level in serum and erythrocyte sedimentation rate (ESR) respectively
DMARDs: Disease-modifying antirheumatic drugs
The incidence of severe periodontitis, as indicated by a PSR of 4, was statistically significantly higher in non-RA/PD patients (89%) than in RA/PD patients (52%) (Chi2: p = 0.001). Within the RA group, the RA-disease activity did not differ significantly between patients with moderate and severe periodontitis (DAS28ESR: 3.08 ± 1.56 vs. 3.34 ± 1.44; p = 0.421).
Bacteria
Periodontal disease severity was not correlated with the presence of P. gingivalis, as detected in the gingival washes. P. gingivalis was detected in GCF samples from 23 (52%) of 44 control subjects without clinical signs of RA (17 non-RA/PD and six non-RA/non-PD) and in those of 36 (69%) of 52 RA patients (33 RA/PD and three RA/non-PD), indicating a higher P. gingivalis prevalence in RA patients than in controls. Nevertheless, the difference between the groups was not statistically significant (Table 2). The only organism showing significant differences between RA and non-RA patients was A. actinomycetemcomitans, which was detected more often in RA patients (Chi2: p = 0.012). A. actinomycetemcomitans and P. gingivalis were often found together (Non-RA 3/5 and RA 14/17 of A. actinomycetemcomitans positive samples), but there was no significant difference in their co-occurrence between RA and non-RA.
Table 2.
Rheumatoid arthritis (RA) and non-RA patients with and without periodontal disease (PD) testing positive for selected bacterial species associated with periodontitis
| A. actinomycetem-comitans | P. gingivalis | T. forsythia | T. denticola | P. intermedia | |
|---|---|---|---|---|---|
| RA/non-PD (n = 4) | 3 (75%) | 3 (75%) | 1 (25%) | 0 (0%) | 0 (0%) |
| RA/PD (n = 48) | 14 (29.2%) | 33 (69%) | 33 (68%) | 24 (50%) | 6 (12.5%) |
| non-RA/non-PD (n = 16) | 1 (6%) | 6 (38%) | 7 (44%) | 4 (25%) | 1 (6%) |
| non-RA/PD (n = 28) | 4 (14%) | 17 (61%) | 16 (57%) | 13 (46%) | 4 (17%) |
Basal citrullination, PAD and PPAD activities
Basal levels of citrullination were detected in the gingival crevicular washes of 26 (50%) RA patients and 23 (48%) non-RA patients. PAD and PPAD activities were detected in 36 (69%) and 30 (58%) RA patients, respectively, and in 30 (68%) and 21 (50%) non-RA patients, respectively. Differences between patients with RA and those without were not significant; however, positive results for baseline citrullination and PPAD activity were significantly higher in Non-RA patients with periodontitis than in those without (Table 3).
Table 3.
Rheumatoid arthritis (RA) and non-RA patients with and without periodontal disease (PD) whose GCF samples were positive for basal citrullination and the activities of human peptidyl arginine deiminase (PAD) and P. gingivalis peptidyl arginine deiminase (PPAD)
| Basal citrullination | PAD activity | PPAD activity | ||||
|---|---|---|---|---|---|---|
| Positive (%) | chi2 test | Positive (%) | chi2 test | Positive (%) | chi2 test | |
| RA/non-PD (n = 4) | 1 (25%) | 0 (0%) | 0 (0%) | |||
| RA/PD (n = 48) | 25 (52%) | 0.298 | 36 (75%) | 0.002 | 30 (63%) | 0.015 |
| non-RA/non-PD (n = 16) | 3 (19%) | 8 (50%) | 2 (13%) | |||
| non-RA/PD (n = 28) | 20 (71%) | 0.001 | 22 (79%) | 0.050 | 19 (68%) | <0.001 |
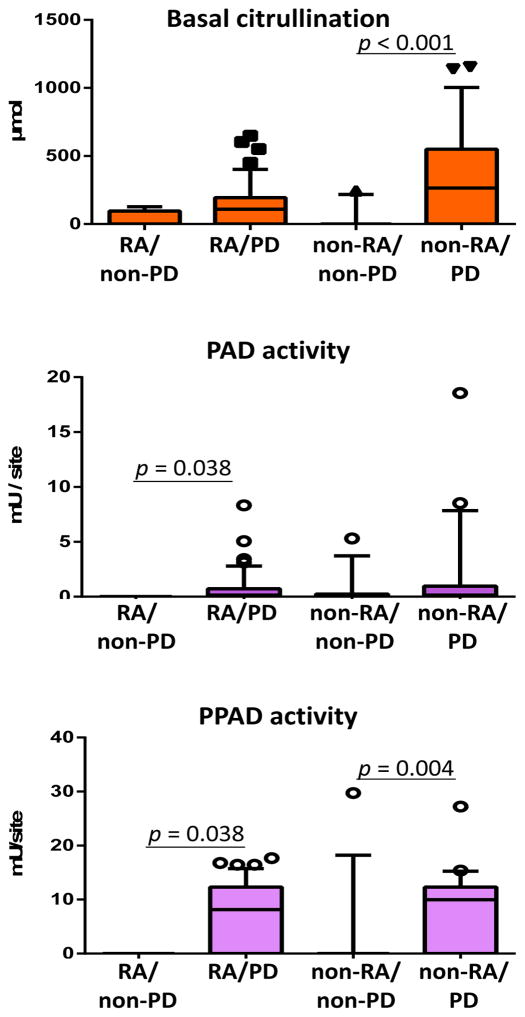
Quantitative assessment showed no significant differences in basal citrullination and PAD and PPAD activities between RA and non-RA patients (basal citrullination: p = 0.142; PAD: p = 0.893; and PPAD: p = 0.633). Basal citrullination levels and PPAD activities were significantly higher in GCF washes of non-RA/PD than in those of non-RA/non-PD patients. PAD and PPAD activities were significantly higher in the RA/PD group than in the RA/non-PD group (Fig. 1).
Fig. 1.
Basal citrullination (A), human endogenous peptidyl arginine deiminase (PAD) (B), and P. gingivalis peptidyl arginine deiminase (PPAD) (C) activities in GCF samples from patients with rheumatoid arthritis without (RA/non-PD) and with (RA/PD) periodontitis, and from individuals without rheumatoid arthritis without (non-RA/non-PD) and with (non-RA/PD) periodontitis, including significant differences (Mann–Whitney test).
Serum samples
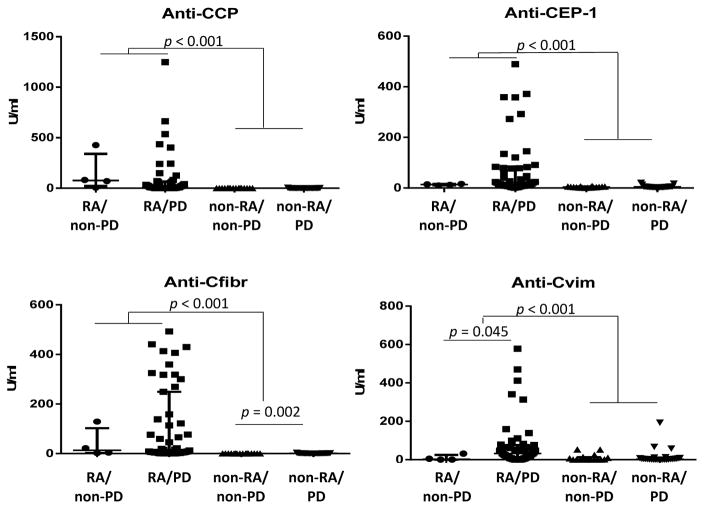
The levels of antibodies against CCP and citrullinated enolase (CEP-1) were elevated in RA patients with no differences between the RA/PD and RA/non-PD groups. Anti-citrullinated fibrinogen (Cfibr) antibody titers were higher in RA than in non-RA patients, and non-RA/PD patients had higher amounts of IgGs against Cfibr than non-RA/non-PD patients. Antibodies against citrullinated vimentin (Cvim) were high in RA patients, especially in those with periodontitis, with significant differences between the RA and non-RA pair and between the RA/PD and RA/non-PD groups (Fig. 2).
Fig. 2.
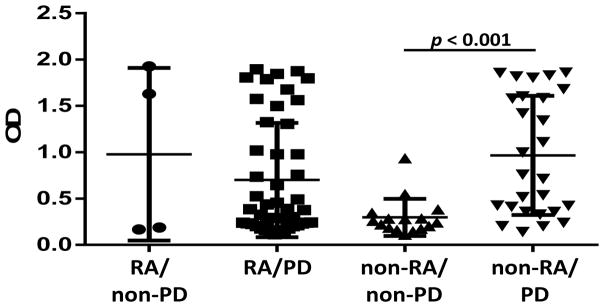
Serum levels of antibodies against RgpB in patients with rheumatoid arthritis without (RA/non-PD) and with (RA/PD) periodontitis, and from individuals without rheumatoid arthritis without (non-RA/non-PD) and with (non-RA/PD) periodontitis, including significant differences (Mann–Whitney test).
Among non-RA subjects, the levels of antibodies against RgpB, a P. gingivalis cysteine protease, were higher in non-RA/PD than in non-RA/non-PD subjects, whereas no differences were observed between the RA-groups (Fig. 3). Anti-RgpB antibody levels were higher in patients testing positive for P. gingivalis in plaque than in those testing negative (p < 0.001).
Fig. 3.
Serum levels of antibodies against several citrullinated peptides and proteins in patients with rheumatoid arthritis without (RA/non-PD) and with (RA/PD) periodontitis, and from individuals without rheumatoid arthritis without (nonRA/non-PD) and with (non-RA/PD) periodontitis, including significant differences (Mann–Whitney test).
Associations of PAD and PPAD activities in GCF
PAD activity was not significantly correlated with other variables; however, PPAD activity in GCF was positively correlated with basal citrullination (R = 0.260, p = 0.011), and serum levels of antibodies against RgpB (R = 0.271, p = 0.008). PPAD activity was not associated with P. gingivalis counts. PPAD activity was detected in 35 of 59 P. gingivalis positive samples, and in 16 of 37 P. gingivalis-negative samples; with the difference between the groups being not significant (p = 0.145).
Discussion
In this study we determined in GCF of RA and non-RA patients, with and without PD, activity of human PAD and for the first time of PPAD. The elevated activity of both enzymes was clearly associated with PD but to a less extent with RA and the presence of P. gingivalis.
Increasing evidence suggests that RA is associated with a high prevalence of periodontal disease [5, 31]. In the present study, 48 (92%) of 52 RA patients were diagnosed with periodontitis, confirming the association between these two diseases. It was not possible to include more than four RA patients without periodontitis. Following, comparisons between RA/non-PD and RA/PD patients have to be considered with care. However, the severity of the periodontal disease was lower in RA patients than in non-RA patients. Data on periodontal health rank Switzerland as the healthiest among European countries [32], and most RA patients in the present study had received continuous supportive periodontal treatment. However, the non-RA periodontitis group was recruited from the Department of Periodontology at the University of Bern, which is a specialized center for treatment of severe periodontitis.
Antibodies against CCP, which are disease-specific in RA [33], are also detectable in GCF [34]. In the present study, serum anti-CCP IgGs were high in RA, whereas no differences were observed between RA/non-PD and RA/PD patients. These results contradict those of previous studies showing that anti-CCP levels are associated with periodontal disease in RA [31, 35]. However, a different study found no correlation between six citrullinated peptides and periodontal disease in first-degree relatives of RA patients [36].
The correlation between anti-CCP and P. gingivalis infection in RA patients remains unclear. A weak correlation between anti-P. gingivalis and anti-CCP antibodies was reported [37], whereas this relationship was questioned in an earlier study [20]. Our results showed no correlation between anti-CCP and anti-RgpB antibodies in RA and Non-RA patients, which is in agreement with the latter study and suggests that periodontitis per se is not sufficient to induce RA.
Antibodies against citrullinated vimentin and enolase are highly specific antibodies in RA [38, 39], and our present results confirm this observation. RA/PD patients showed high levels of anti-Cvim IgGs. Autoantibodies against citrullinated vimentin induce osteoclastogenesis [40]. Vimentin, a major protein of intermediate filaments, is produced in epithelial and mesenchymal cells [41, 42], and is abundant in periodontal ligaments [43] and in gingival connective tissue cells in the periodontium [44]. It is likely that the inflamed periodontal tissue is a source of citrullinated vimentin, which induces the production of antibodies. Fibrinogen, which is found in GCF in periodontitis patients [45], may function as an autoantigen in its citrullinated form, inducing autoimmune response in the inflammatory milieu of chronic periodontitis. Therefore, our findings showing significantly higher levels of anti-Cfibr in non-RA/PD than in non-RA/non-PD patients are important.
Data on the subgingival microbiota in RA patients are limited. A multiplexed 454-pyrosequencing study of 31 patients with new-onset RA, 34 with “chronic” RA, and 18 without RA showed an association between the microbiome and periodontal status [46]. However, another study found no differences in the subgingival occurrence of P. gingivalis between RA and non-RA controls [47]. In the present study, we used a cut-off between 103 (A. actinomycetemcomitans) and 104 bacteria to identify bacterial species associated with periodontitis. Therefore, only samples in which the bacterial counts were above the threshold level were included. In addition, we used a sensitive real-time PCR method for P. gingivalis detection. In our study cohort, the presence of P. gingivalis was not associated with RA. A. actinomycetemcomitans was more prevalent in the microbiome of RA patients, including the comparison between the RA/non-PD and non-RA/non-PD groups (p = 0.013), suggesting that the role of A. actinomycetemcomitans in RA needs to be determined. Studies that used whole cells of A. actinomycetemcomitans as antigens showed no differences in antibody levels between RA and non-RA patients [20, 48]; however, higher antibody levels against A. actinomycetemcomitans heat shock protein 40 were found in RA than in non-RA patients [49].
The main purpose of the present study was to determine the activities of citrullinating enzymes, particularly PPAD, within the periodontium. The presence of citrullinated proteins in periodontal tissue, particularly in infiltrating inflammatory cells, was recently reported in non-RA subjects [34, 50]. PAD-2 and PAD-4 expression was detected in periodontal tissue at the protein and mRNA levels [34]. Here, we confirmed the presence of citrullinated proteins and PAD activity in GCF and their association with periodontitis. However, no difference between the RA and non-RA groups was observed, suggesting that citrullination and PAD activity are primarily associated with inflammation and bone destruction in the periodontium and not with RA. In addition to human endogenous PAD activity, we measured PPAD activity in GCF. The preferred substrates of PPADs are C-terminal arginine residues, which cannot be citrullinated by human enzymes, allowing distinction between host and P. gingivalis-derived peptidylarginine deiminase activity. In addition, PPAD activity was increased in periodontitis samples from RA and non-RA patients, whereas no correlation with PAD activity was found. The significant but weak correlation with basal citrullination underlines that PPAD activity contributes but is not the sole source of citrullination in GCF.
PPAD catalyzes the citrullination of fibrinogen, human and bacterial enolase [22], fibrin, and vimentin [51], and inactivates epidermal growth factor and C5a (PMID: 25324545), hindering tissue repair and antibacterial immune responses, respectively [52]. PPAD accelerates the development and aggravates collagen-induced arthritis in mice [53].
In the present study, PPAD activity was detected in samples negative for P. gingivalis. In these samples, the activity of PPAD was not correlated with that of host enzymes. These patients had high levels of serum IgG against PPAD-derived peptides, suggesting a lingering P. gingivalis infection hiding within epithelial cells [54]. PPAD activity in C-terminal Arg residues can be detected at very low enzyme concentrations, as shown by the citrullination of an insulin-derived peptide by low levels of PPAD contaminating a purified P. gingivalis protease sample [55]. Therefore, PPAD secreted by P. gingivalis residing in epithelial cells may exert its citrullinating activity in distant regions of the periodontium or even distant tissues.
In summary, moderate periodontitis is highly prevalent in RA-patients. With no difference between RA and non-RA individuals, human endogenous and P. gingivalis-derived peptidylarginine deiminases are active in vivo and can citrullinate proteins and peptides in the chronic inflammatory environment of the periodontium. In non-RA susceptible periodontitis patients this may contribute to breaching immunotolerance, leading to the development of autoantibodies.
Acknowledgments
The authors would like to thank Marianne Weibel (Department of Periodontology, Laboratory of Oral Microbiology, School of Dental Medicine, University of Bern) for technical assistance. We are indebted Walter Bürgin (University of Bern) for statistical advice.
Funding: The study was funded by the participating departments and a research grant of the German Society of Periodontology (DGParo/GABA), along with grants from: US NIH (DE 022597), the European Commission (FP7-PEOPLE-2011-ITN-290246 “RAPID” and FP7-HEALTH-F3-2012-306029 “TRIGGER”), Polish National Centre of Science project OPUS 2012/05/B/NZ6/00581 and Polish Ministry of Science and Higher Education (project 2975/7.PR/13/2014/2). Faculty of Biochemistry, Biophysics and Biotechnology of Jagiellonian University is a partner of the Leading National Research Center (KNOW) supported by the Ministry of Science and Higher Education. Oliver Laugisch was supported by German Academic Exchange Service (grant No: 314-D/08/48763) and the German Society of Periodontology (grant for a foreign training and research grant).
Footnotes
Conflict of Interest: There are no conflicts of interest to declare.
Contributor Information
Oliver Laugisch, Department of Periodontology, School of Dental Medicine, University of Bern, Freiburgstrasse 7, CH-3010 Bern, Switzerland.
Alicia Wong, Department of Microbiology, Faculty of Biochemistry, Biophysics and Biotechnology, Jagiellonian University in Krakow, 30-387 Krakow, Poland.
Aneta Sroka, Department of Microbiology, Faculty of Biochemistry, Biophysics and Biotechnology, Jagiellonian University in Krakow, 30-387 Krakow, Poland.
Tomasz Kantyka, Department of Microbiology, Faculty of Biochemistry, Biophysics and Biotechnology, Jagiellonian University in Krakow, 30-387 Krakow, Poland. Malopolska Center of Biotechnology, Jagiellonian University, 30-387 Krakow, Poland.
Joanna Koziel, Department of Microbiology, Faculty of Biochemistry, Biophysics and Biotechnology, Jagiellonian University in Krakow, 30-387 Krakow, Poland.
Klaus Neuhaus, Department of Preventive, Restorative and Pediatric Dentistry, School of Dental Medicine, University of Bern, Bern, Switzerland.
Anton Sculean, Department of Periodontology, School of Dental Medicine, University of Bern, Freiburgstrasse 7, CH-3010 Bern, Switzerland.
Patrick J. Venables, Kennedy Institute, Nuffield Dept of Orthopaedics, Rheumatology & Musculoskeletal Sciences, University of Oxford, Roosevelt Drive, Headington, Oxford, OX3 7FY
Jan Potempa, Department of Microbiology, Faculty of Biochemistry, Biophysics and Biotechnology, Jagiellonian University in Krakow, 30-387 Krakow, Poland. Malopolska Center of Biotechnology, Jagiellonian University, 30-387 Krakow, Poland. Department of Oral Immunology and Infectious Diseases, University of Louisville School of Dentistry, Louisville, KY 40202, USA.
Burkhard Möller, Department of Rheumatology, Clinical Immunology and Allergology, University Hospital of Bern, Bern, Switzerland.
Sigrun Eick, Department of Periodontology, School of Dental Medicine, University of Bern, Freiburgstrasse 7, CH-3010 Bern, Switzerland.
References
- 1.Demmer RT, Molitor JA, Jacobs DR, Jr, Michalowicz BS. Periodontal disease, tooth loss and incident rheumatoid arthritis: results from the First National Health and Nutrition Examination Survey and its epidemiological follow-up study. J Clin Periodontol. 2011;38:998–1006. doi: 10.1111/j.1600-051X.2011.01776.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen HH, Huang N, Chen YM, Chen TJ, Chou P, Lee YL, Chou YJ, Lan JL, Lai KL, Lin CH, Chen DY. Association between a history of periodontitis and the risk of rheumatoid arthritis: a nationwide, population-based, case-control study. Ann Rheum Dis. 2013;72:1206–11. doi: 10.1136/annrheumdis-2012-201593. [DOI] [PubMed] [Google Scholar]
- 3.Joseph R, Rajappan S, Nath SG, Paul BJ. Association between chronic periodontitis and rheumatoid arthritis: a hospital-based case-control study. Rheumatol Int. 2013;33:103–9. doi: 10.1007/s00296-011-2284-1. [DOI] [PubMed] [Google Scholar]
- 4.Torkzaban P, Hjiabadi T, Basiri Z, Poorolajal J. Effect of rheumatoid arthritis on periodontitis: a historical cohort study. J Periodontal Implant Sci. 2012;42:67–72. doi: 10.5051/jpis.2012.42.3.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nesse W, Dijkstra PU, Abbas F, Spijkervet FK, Stijger A, Tromp JA, van Dijk JL, Vissink A. Increased prevalence of cardiovascular and autoimmune diseases in periodontitis patients: a cross-sectional study. J Periodontol. 2010;81:1622–8. doi: 10.1902/jop.2010.100058. [DOI] [PubMed] [Google Scholar]
- 6.Kobayashi T, Okada M, Ito S, Kobayashi D, Ishida K, Kojima A, Narita I, Murasawa A, Yoshie H. Assessment of interleukin-6 receptor inhibition therapy on periodontal condition in patients with rheumatoid arthritis and chronic periodontitis. J Periodontol. 2014;85:57–67. doi: 10.1902/jop.2013.120696. [DOI] [PubMed] [Google Scholar]
- 7.Erciyas K, Sezer U, Ustun K, Pehlivan Y, Kisacik B, Senyurt SZ, Tarakcioglu M, Onat AM. Effects of periodontal therapy on disease activity and systemic inflammation in rheumatoid arthritis patients. Oral Dis. 2013;19:394–400. doi: 10.1111/odi.12017. [DOI] [PubMed] [Google Scholar]
- 8.Biyikoglu B, Buduneli N, Aksu K, Nalbantsoy A, Lappin DF, Evrenosoglu E, Kinane DF. Periodontal therapy in chronic periodontitis lowers gingival crevicular fluid interleukin-1beta and DAS28 in rheumatoid arthritis patients. Rheumatol Int. 2013;33:2607–16. doi: 10.1007/s00296-013-2781-5. [DOI] [PubMed] [Google Scholar]
- 9.Culshaw S, McInnes IB, Liew FY. What can the periodontal community learn from the pathophysiology of rheumatoid arthritis? J Clin Periodontol. 2011;38(Suppl 11):106–13. doi: 10.1111/j.1600-051X.2010.01669.x. [DOI] [PubMed] [Google Scholar]
- 10.de Pablo P, Chapple IL, Buckley CD, Dietrich T. Periodontitis in systemic rheumatic diseases. Nat Rev Rheumatol. 2009;5:218–24. doi: 10.1038/nrrheum.2009.28. [DOI] [PubMed] [Google Scholar]
- 11.Mewar D, Wilson AG. Autoantibodies in rheumatoid arthritis: a review. Biomed Pharmacother. 2006;60:648–55. doi: 10.1016/j.biopha.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Wegner N, Lundberg K, Kinloch A, Fisher B, Malmstrom V, Feldmann M, Venables PJ. Autoimmunity to specific citrullinated proteins gives the first clues to the etiology of rheumatoid arthritis. Immunol Rev. 2010;233:34–54. doi: 10.1111/j.0105-2896.2009.00850.x. [DOI] [PubMed] [Google Scholar]
- 13.Kinloch A, Lundberg K, Wait R, Wegner N, Lim NH, Zendman AJ, Saxne T, Malmstrom V, Venables PJ. Synovial fluid is a site of citrullination of autoantigens in inflammatory arthritis. Arthritis Rheum. 2008;58:2287–95. doi: 10.1002/art.23618. [DOI] [PubMed] [Google Scholar]
- 14.Hajishengallis G, Darveau RP, Curtis MA. The keystone-pathogen hypothesis. Nat Rev Microbiol. 2012;10:717–25. doi: 10.1038/nrmicro2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo Y, Nguyen KA, Potempa J. Dichotomy of gingipains action as virulence factors: from cleaving substrates with the precision of a surgeon’s knife to a meat chopper-like brutal degradation of proteins. Periodontol 2000. 2010;54:15–44. doi: 10.1111/j.1600-0757.2010.00377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Potempa J, Banbula A, Travis J. Role of bacterial proteinases in matrix destruction and modulation of host responses. Periodontol 2000. 2000;24:153–92. doi: 10.1034/j.1600-0757.2000.2240108.x. [DOI] [PubMed] [Google Scholar]
- 17.McGraw WT, Potempa J, Farley D, Travis J. Purification, characterization, and sequence analysis of a potential virulence factor from Porphyromonas gingivalis, peptidylarginine deiminase. Infect Immun. 1999;67:3248–56. doi: 10.1128/iai.67.7.3248-3256.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goulas T, Mizgalska D, Garcia-Ferrer I, Kantyka T, Guevara T, Szmigielski B, Sroka A, Millan C, Uson I, Veillard F, Potempa B, Mydel P, Sola M, Potempa J, Gomis-Ruth FX. Structure and mechanism of a bacterial host-protein citrullinating virulence factor, Porphyromonas gingivalis peptidylarginine deiminase. Sci Rep. 2015;5:11969. doi: 10.1038/srep11969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenstein ED, Greenwald RA, Kushner LJ, Weissmann G. Hypothesis: the humoral immune response to oral bacteria provides a stimulus for the development of rheumatoid arthritis. Inflammation. 2004;28:311–8. doi: 10.1007/s10753-004-6641-z. [DOI] [PubMed] [Google Scholar]
- 20.Okada M, Kobayashi T, Ito S, Yokoyama T, Komatsu Y, Abe A, Murasawa A, Yoshie H. Antibody responses to periodontopathic bacteria in relation to rheumatoid arthritis in Japanese adults. J Periodontol. 2011;82:1433–41. doi: 10.1902/jop.2011.110020. [DOI] [PubMed] [Google Scholar]
- 21.Mikuls TR, Payne JB, Reinhardt RA, Thiele GM, Maziarz E, Cannella AC, Holers VM, Kuhn KA, O’Dell JR. Antibody responses to Porphyromonas gingivalis (P. gingivalis) in subjects with rheumatoid arthritis and periodontitis. Int Immunopharmacol. 2009;9:38–42. doi: 10.1016/j.intimp.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wegner N, Wait R, Sroka A, Eick S, Nguyen KA, Lundberg K, Kinloch A, Culshaw S, Potempa J, Venables PJ. Peptidylarginine deiminase from Porphyromonas gingivalis citrullinates human fibrinogen and alpha-enolase: implications for autoimmunity in rheumatoid arthritis. Arthritis Rheum. 2010;62:2662–72. doi: 10.1002/art.27552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, 3rd, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JM, Hobbs K, Huizinga TW, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Menard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovsky J, Wolfe F, Hawker G. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569–81. doi: 10.1002/art.27584. [DOI] [PubMed] [Google Scholar]
- 24.Lo Frisco C, Cutler R, Bramson JB. Periodontal screening and recording: perceptions and effects on practice. J Am Dent Assoc. 1993;124:226–9. 231–2. doi: 10.14219/jada.archive.1993.0256. [DOI] [PubMed] [Google Scholar]
- 25.Guentsch A, Kramesberger M, Sroka A, Pfister W, Potempa J, Eick S. Comparison of gingival crevicular fluid sampling methods in patients with severe chronic periodontitis. J Periodontol. 2011;82:1051–60. doi: 10.1902/jop.2011.100565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guentsch A, Ronnebeck M, Puklo M, Preshaw PM, Pfister W, Eick S. Influence of serum on interaction of Porphyromonas gingivalis ATCC 33277 and Aggregatibacter actinomycetemcomitans Y4 with an epithelial cell line. J Periodontal Res. 2010;45:229–38. doi: 10.1111/j.1600-0765.2009.01224.x. [DOI] [PubMed] [Google Scholar]
- 27.Eick S, Straube A, Guentsch A, Pfister W, Jentsch H. Comparison of real-time polymerase chain reaction and DNA-strip technology in microbiological evaluation of periodontitis treatment. Diagn Microbiol Infect Dis. 2011;69:12–20. doi: 10.1016/j.diagmicrobio.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 28.Boyde TR, Rahmatullah M. Optimization of conditions for the colorimetric determination of citrulline, using diacetyl monoxime. Anal Biochem. 1980;107:424–31. doi: 10.1016/0003-2697(80)90404-2. [DOI] [PubMed] [Google Scholar]
- 29.de Pablo P, Dietrich T, Chapple IL, Milward M, Chowdhury M, Charles PJ, Buckley CD, Venables PJ. The autoantibody repertoire in periodontitis: a role in the induction of autoimmunity to citrullinated proteins in rheumatoid arthritis? Ann Rheum Dis. 2014;73:580–6. doi: 10.1136/annrheumdis-2012-202701. [DOI] [PubMed] [Google Scholar]
- 30.Quirke AM, Lugli EB, Wegner N, Hamilton BC, Charles P, Chowdhury M, Ytterberg AJ, Zubarev RA, Potempa J, Culshaw S, Guo Y, Fisher BA, Thiele G, Mikuls TR, Venables PJ. Heightened immune response to autocitrullinated Porphyromonas gingivalis peptidylarginine deiminase: a potential mechanism for breaching immunologic tolerance in rheumatoid arthritis. Ann Rheum Dis. 2014;73:263–9. doi: 10.1136/annrheumdis-2012-202726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dissick A, Redman RS, Jones M, Rangan BV, Reimold A, Griffiths GR, Mikuls TR, Amdur RL, Richards JS, Kerr GS. Association of periodontitis with rheumatoid arthritis: a pilot study. J Periodontol. 2010;81:223–30. doi: 10.1902/jop.2009.090309. [DOI] [PubMed] [Google Scholar]
- 32.Konig J, Holtfreter B, Kocher T. Periodontal health in Europe: future trends based on treatment needs and the provision of periodontal services--position paper 1. Eur J Dent Educ. 2010;14(Suppl 1):4–24. doi: 10.1111/j.1600-0579.2010.00620.x. [DOI] [PubMed] [Google Scholar]
- 33.Lopez-Longo FJ, Sanchez-Ramon S, Carreno L. The value of anti-cyclic citrullinated peptide antibodies in rheumatoid arthritis: do they imply new risk factors? Drug News Perspect. 2009;22:543–8. doi: 10.1358/dnp.2009.22.9.1416992. [DOI] [PubMed] [Google Scholar]
- 34.Harvey GP, Fitzsimmons TR, Dhamarpatni AA, Marchant C, Haynes DR, Bartold PM. Expression of peptidylarginine deiminase-2 and -4, citrullinated proteins and anti-citrullinated protein antibodies in human gingiva. J Periodontal Res. 2013;48:252–61. doi: 10.1111/jre.12002. [DOI] [PubMed] [Google Scholar]
- 35.Potikuri D, Dannana KC, Kanchinadam S, Agrawal S, Kancharla A, Rajasekhar L, Pothuraju S, Gumdal N. Periodontal disease is significantly higher in non-smoking treatment-naive rheumatoid arthritis patients: results from a case-control study. Ann Rheum Dis. 2012;71:1541–4. doi: 10.1136/annrheumdis-2011-200380. [DOI] [PubMed] [Google Scholar]
- 36.Barra L, Scinocca M, Saunders S, Bhayana R, Rohekar S, Racape M, Coles R, Cairns E, Bell DA. Anti-citrullinated protein antibodies in unaffected first-degree relatives of rheumatoid arthritis patients. Arthritis Rheum. 2013;65:1439–47. doi: 10.1002/art.37911. [DOI] [PubMed] [Google Scholar]
- 37.Mikuls TR, Payne JB, Yu F, Thiele GM, Reynolds RJ, Cannon GW, Markt J, McGowan D, Kerr GS, Redman RS, Reimold A, Griffiths G, Beatty M, Gonzalez SM, Bergman DA, Hamilton BC, 3rd, Erickson AR, Sokolove J, Robinson WH, Walker C, Chandad F, O’Dell JR. Periodontitis and Porphyromonas gingivalis in patients with rheumatoid arthritis. Arthritis Rheum. 2014;66:1090–100. doi: 10.1002/art.38348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bang H, Egerer K, Gauliard A, Luthke K, Rudolph PE, Fredenhagen G, Berg W, Feist E, Burmester GR. Mutation and citrullination modifies vimentin to a novel autoantigen for rheumatoid arthritis. Arthritis Rheum. 2007;56:2503–11. doi: 10.1002/art.22817. [DOI] [PubMed] [Google Scholar]
- 39.Lundberg K, Kinloch A, Fisher BA, Wegner N, Wait R, Charles P, Mikuls TR, Venables PJ. Antibodies to citrullinated alpha-enolase peptide 1 are specific for rheumatoid arthritis and cross-react with bacterial enolase. Arthritis Rheum. 2008;58:3009–19. doi: 10.1002/art.23936. [DOI] [PubMed] [Google Scholar]
- 40.Harre U, Georgess D, Bang H, Bozec A, Axmann R, Ossipova E, Jakobsson PJ, Baum W, Nimmerjahn F, Szarka E, Sarmay G, Krumbholz G, Neumann E, Toes R, Scherer HU, Catrina AI, Klareskog L, Jurdic P, Schett G. Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J Clin Invest. 2012;122:1791–802. doi: 10.1172/JCI60975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steinert PM, Jones JC, Goldman RD. Intermediate filaments. J Cell Biol. 1984;99:22s–27s. doi: 10.1083/jcb.99.1.22s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Goldman RD, Cleland MM, Murthy SN, Mahammad S, Kuczmarski ER. Inroads into the structure and function of intermediate filament networks. J Struct Biol. 2012;177:14–23. doi: 10.1016/j.jsb.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sculean A, Berakdar M, Windisch P, Remberger K, Donos N, Brecx M. Immunohistochemical investigation on the pattern of vimentin expression in regenerated and intact monkey and human periodontal ligament. Arch Oral Biol. 2003;48:77–86. doi: 10.1016/s0003-9969(02)00164-4. [DOI] [PubMed] [Google Scholar]
- 44.Hunter N, Nicholls B, Srivastava M, Chapple CC, Zoellner HF, Gibbins JR. Reactive pocket epithelium in untreated chronic periodontal disease: possible derivation from developmental remnants of the enamel organ and root sheath. J Oral Pathol Med. 2001;30:178–86. doi: 10.1034/j.1600-0714.2001.300308.x. [DOI] [PubMed] [Google Scholar]
- 45.Hidaka N, Maeda K, Kawakami C, Aono M, Okada H. Fibrinolytic activity in periodontal disease. The relationship between fibrinolytic activity and severity of periodontal disease. J Periodontol. 1981;52:181–6. doi: 10.1902/jop.1981.52.4.181. [DOI] [PubMed] [Google Scholar]
- 46.Scher JU, Ubeda C, Equinda M, Khanin R, Buischi Y, Viale A, Lipuma L, Attur M, Pillinger MH, Weissmann G, Littman DR, Pamer EG, Bretz WA, Abramson SB. Periodontal disease and the oral microbiota in new-onset rheumatoid arthritis. Arthritis Rheum. 2012;64:3083–94. doi: 10.1002/art.34539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smit MD, Westra J, Vissink A, Doornbos-van der Meer B, Brouwer E, van Winkelhoff AJ. Periodontitis in established rheumatoid arthritis patients: a cross-sectional clinical, microbiological and serological study. Arthritis Res Ther. 2012;14:R222. doi: 10.1186/ar4061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ogrendik M, Kokino S, Ozdemir F, Bird PS, Hamlet S. Serum antibodies to oral anaerobic bacteria in patients with rheumatoid arthritis. MedGenMed. 2005;7:2. [PMC free article] [PubMed] [Google Scholar]
- 49.Yoshida A, Nakano Y, Yamashita Y, Oho T, Ito H, Kondo M, Ohishi M, Koga T. Immunodominant region of Actinobacillus actinomycetemcomitans 40-kilodalton heat shock protein in patients with rheumatoid arthritis. J Dent Res. 2001;80:346–50. doi: 10.1177/00220345010800010901. [DOI] [PubMed] [Google Scholar]
- 50.Nesse W, Westra J, van der Wal JE, Abbas F, Nicholas AP, Vissink A, Brouwer E. The periodontium of periodontitis patients contains citrullinated proteins which may play a role in ACPA (anti-citrullinated protein antibody) formation. J Clin Periodontol. 2012;39:599–607. doi: 10.1111/j.1600-051X.2012.01885.x. [DOI] [PubMed] [Google Scholar]
- 51.Abdullah SN, Farmer EA, Spargo L, Logan R, Gully N. Porphyromonas gingivalis peptidylarginine deiminase substrate specificity. Anaerobe. 2013;23:102–8. doi: 10.1016/j.anaerobe.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 52.Pyrc K, Milewska A, Kantyka T, Sroka A, Maresz K, Koziel J, Nguyen KA, Enghild JJ, Knudsen AD, Potempa J. Inactivation of epidermal growth factor by Porphyromonas gingivalis as a potential mechanism for periodontal tissue damage. Infect Immun. 2013;81:55–64. doi: 10.1128/IAI.00830-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maresz KJ, Hellvard A, Sroka A, Adamowicz K, Bielecka E, Koziel J, Gawron K, Mizgalska D, Marcinska KA, Benedyk M, Pyrc K, Quirke AM, Jonsson R, Alzabin S, Venables PJ, Nguyen KA, Mydel P, Potempa J. Porphyromonas gingivalis Facilitates the Development and Progression of Destructive Arthritis through Its Unique Bacterial Peptidylarginine Deiminase (PAD) PLoS Pathog. 2013;9:e1003627. doi: 10.1371/journal.ppat.1003627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Madianos PN, Papapanou PN, Nannmark U, Dahlen G, Sandros J. Porphyromonas gingivalis FDC381 multiplies and persists within human oral epithelial cells in vitro. Infect Immun. 1996;64:660–4. doi: 10.1128/iai.64.2.660-664.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hayashi H, Morioka M, Ichimiya S, Yamato K, Hinode D, Nagata A, Nakamura R. Participation of an arginyl residue of insulin chain B in the inhibition of hemagglutination by Porphyromonas gingivalis. Oral Microbiol Immunol. 1993;8:386–9. doi: 10.1111/j.1399-302x.1993.tb00616.x. [DOI] [PubMed] [Google Scholar]