Abstract
Researchers often rely on respondents’ self-rated health (SRH) to measure social disparities in health, but recent studies suggest that systematically different reporting styles across groups can yield misleading conclusions about disparities in SRH. In this study, we test whether this finding extends to ethnic differences in self-assessments of health in particular domains. We document differences between US-born whites and four Latino subgroups in respondents’ assessments of health in six health domains using data from the second wave of the Los Angeles Family and Neighborhood Study (N=1468). We use both conventional methods and an approach that uses vignettes to adjust for differential reporting styles.
Our results suggest that despite consistent evidence from the literature that Latinos tend to rate their overall health more poorly than whites, and that Latino immigrants report worse SRH than US-born Latinos, this pattern is not true of self-reports in individual health domains. We find that at the bivariate level, US-born whites (and often US-born Mexicans) have significantly more pessimistic reporting styles than Latino immigrants. After adding controls, we find evidence of significantly different reporting styles for only one domain: US-born Mexicans and whites consistently interpret head pain more severely than the other Latino subgroups. Finally, we find that both before and after adjusting for differences in rating styles across groups, non-Mexican Latino immigrants report better social and physical functioning and less pain than other groups.
Our findings underscore the advantages of domain-specific ratings when evaluating ethnic differences in self-assessments of health. We encourage researchers studying social disparities in health to consider respondents’ self-assessments in a variety of domains, and to also investigate (when possible) potential biases in their findings due to different reporting styles. The anchoring vignettes approach we use is one potential method for overcoming biases due to different rating styles across groups.
Keywords: Self-rated health, health disparities, vignettes, racial/ethnic disparities
Global self-rated health (hereafter referred to as SRH) is one of the most commonly-used measures of individual health status in public health and social science research. Originally developed as part of the SF-36 health survey from the Medical Outcomes Study (Ware, 2000), the SRH question is used in many surveys and asks respondents to rate their own health using a question similar to: “Overall, how would you rate your health? Excellent, very good, good, fair or poor?” Several studies demonstrate that, in the presence of controls for objective health status and other factors, SRH is correlated with future mortality and health outcomes (for reviews, see DeSalvo et al. 2006; Fayers & Sprangers 2002; Idler 2008; Idler & Benyamini 1997; Jylhä 2009). However, previous research in the US shows that Latinos report poorer self-rated health than non-Latino whites (hereafter referred to as whites), despite having comparable or superior objective health status and survival (Arcia, Skinner, Bailey, & Correa, 2001; Bzostek, Goldman & Pebley 2007; Finch, Hummer, Reindl, & Vega, 2002; Ren & Amick, 1996; Su, Wen and Markides, 2013). Bzostek et al. (2007) conclude that differences in self-reports between Latinos and whites, as well as among Latino groups, arise in part because of group differences in socioeconomic status and language and translation issues; they also speculate that culturally-influenced expressions of health and choices of reference groups are important, but, like other previous studies, the data they used were inadequate to investigate potential ethnic and cultural differences in assessing health and in referents.
In this paper, we use a novel approach to examine some of these questions in the context of domain-specific, rather than overall, health. Specifically, we investigate the role of Latino-white differences in health rating styles, using a set of six self-ratings that span the major domains of health. Although these questions are subject to some of the same limitations as the simple SRH question, they allow us to examine ethnic differences in reporting styles in greater depth. We adjust domain-specific self-ratings for ethnic differences in reporting styles by using vignette reports – i.e., respondents’ assessments of hypothetical individuals’ health status in the same health domains. We also examine Mexican-origin Latinos by place of birth separately from other Latinos to investigate national origin and nativity differences. Our results suggest that separate questions about distinct domains of health, hereafter referred to as DSH (for domain-specific health), provide a substantially different picture of health disparities between Latinos and whites than the standard SRH question, and that reporting styles do sometimes differ systematically across the ethnic groups we consider. The paper contributes to a growing literature about the potential shortcomings of survey questions about self-rated health because of social group differences in subjective perceptions, frames of reference, and norms about self-description (see, e.g., Dowd & Todd 2011; Grol-Prokopcyzk, Freese & Hauser 2011; Kapteyn, Smoth & Van Soest 2007). Our results also provide important information about Mexican-origin Latinos, other Latinos, and whites’ perceptions of their own health by identifying specific domains in which each group reports poorer and better health.
Background
Comparing Latinos’ and whites’ self-rated health: Previous findings and limitations
Previous research indicates that Latinos tend to report worse overall SRH than whites in the US (Arcia et al. 2001; Bzostek et al. 2007; Cho, Frisbie, Hummer & Rogers 2004; Finch, Hummer, Reindl, & Vega, 2002; Ren & Amick, 1996). This is true even though evidence suggests that, for many other measures of health, Latinos fare better than whites despite their lower average levels of socioeconomic status – a phenomenon often referred to as the “Hispanic health paradox” (Franzini, Ribble, & Keddie, 2001; Morales, Lara, Kington, Valdez, & Escarce, 2002; Williams, 2001).
There are several possible explanations for these findings. A common one is that US-born Latinos, immigrant Latinos, and whites differ in social and economic status, which in turn affects their health. Differences may also result from cultural influences, such as reluctance among traditionally-oriented Latinos to sound boastful or optimistic about their health, behaviors which may vary with the degree of acculturation of Latinos to American society (Angel & Angel 1992; Shetterly, Baxter, Mason, & Hamman, 1996). Latinos may also feel less comfortable expressing emotional distress and may be more likely to “somatize,” or to express emotional distress through physical symptoms (Angel & Guarnaccia 1989; Finch, Kolody, & Vega, 2000; Finch, Hummer, Kolody, & Vega, 2001). There is also evidence that poorer health ratings of Latinos relative to whites are due in part to differences in the meaning of the response categories, particularly “fair” in English vs. “regular” in Spanish (Angel & Guarnaccia 1989; Bzostek et al. 2007; Franzini & Fernandez-Esquer, 2004; Phillips, Hammock & Blanton, 2005; Viruell-Fuentes, Morenoff, Williams & House, 2011).
One major source of potential bias in measuring intergroup differences based on SRH is variation in reporting styles, including variation in health-related optimism or pessimism across ethnic or racial groups (e.g., Spencer et al. 2009, Su et al. 2003). Increasing recognition of this problem, which also affects self-reported measures other than SRH (e.g., MacIntosh & Strickland 2011), has led some researchers to incorporate anchoring vignettes into health interview surveys and to use both self-reports and vignette responses in statistical models to adjust for systematic differences in reporting styles (e.g., Zajacova & Dowd 2011).
The anchoring vignette approach
With adequate data, such as those used in this paper, and a few key assumptions, adjusting self-reports with anchoring vignettes can standardize self-assessment ratings across individuals. The technique is based on the idea that, in any self-rating, differences could be due to either true differences in a status or phenomenon or to different rating styles, known as response category differential item functioning, or DIF (King et al. 2004, King & Wand 2007). In this method, respondents rate hypothetical individuals’ health based on fictitious scenarios of symptoms, conditions, or limitations. These hypothetical vignette ratings are intended to capture general rating style and are used to adjust responses to questions about respondents’ own health. After adjustment for these responses, remaining differences across respondents’ ratings about their own health should be due to actual differences in underlying health, rather than differential rating styles.
The bias introduced by differential rating styles can be illustrated by considering individual or group differences in the cut-points or thresholds used to distinguish one response category from the next, which would undermine comparisons. For example, rather than all respondents sharing the same cut-points, some may have higher thresholds than other raters for reporting good versus very good, or poor versus fair health. For this reason, two individuals with identical “true” health might report a different level of health solely due to differences in reporting styles. Figure 1 (below) provides a hypothetical illustration of different reporting styles between two groups, reflecting different thresholds for reporting a higher (worse) rating category. Here, we depict the hypothesis that individuals in Group 1 have more pessimistic rating styles than those in Group 2, as shown by their lower thresholds for reporting worse health. Statistical models that incorporate information from the anchoring vignettes allow researchers to relax the assumption of constant cut-points across individuals by modeling and adjusting for different thresholds across respondents.
Figure 1.
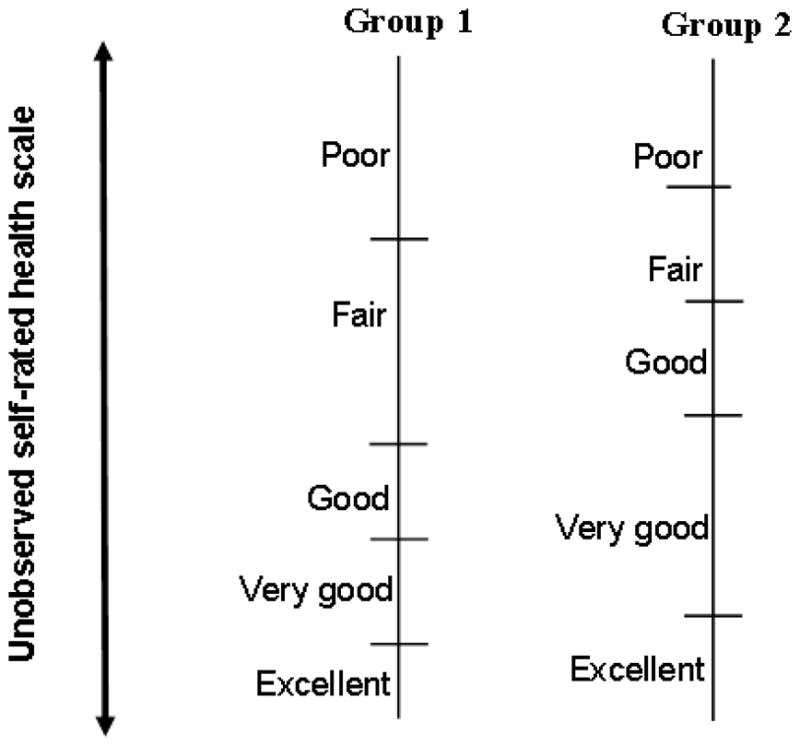
Hypothetical illustration of different reporting styles between groups
Recent studies have used this method to address reporting style differences in individuals’ assessments of health, but rarely with regard to the standard SRH question. A major limitation with the use of anchoring vignettes to adjust SRH itself, rather than domain-specific health (DSH) measures as we do here, is that the response categories used in the SRH question (excellent, very good, good, fair, and poor) are not generally used in questions about specific health problems (e.g., for pain the response categories are none, very mild, mild, moderate, or severe). Moreover, response categories often vary depending on the specific health issue (for example, physical functioning vs. pain). One exception is Grol-Prokopcyzk et al. (2011), who design and use vignettes specifically intended to adjust SRH—using the same response categories for the vignettes as the SRH question—in the Wisconsin Longitudinal Survey, and argue that vignettes are a promising tool. However, their procedure requires a large number (12) of vignettes and may have been successful because they have the unusual advantage of a relatively homogenous sample: a cohort of predominantly white Wisconsin high school seniors and their siblings and spouses.
More commonly, studies use vignettes to adjust self-reported health in a set of domains that reflect different aspects of health (see, for example, Salomon, Tandon & Murray 2004; Kapteyn et al. 2007; Dowd & Todd 2011). For example, Dowd and Todd (2011) focus on reporting differences in six health domains among older adults in the US. They find that models often underestimate social and racial inequalities in health if they do not account for reporting differences. Although they also examine differences between Latino and non-Latino respondents, their analysis does not consider Latino subgroups by nativity or nationality and the sample is restricted to adults ages 50 and over.
In this paper, we use data from the second wave of the Los Angeles Family and Neighborhood Study (L.A.FANS-2) to assess whether the direction and magnitude of differences in Latinos’ and whites’ reports of health change when we adjust for differential reporting styles in six specific health domains (DSH). Results from both the first and second wave of L.A.FANS (not shown here) confirm the general SRH differential noted in the literature, namely that Latinos – especially first generation immigrants – report considerably worse SRH than whites (Bzostek et al. 2007). We add to this literature by assessing differences in DSH between whites and various Latino groups, both before and after taking potential differences in reporting styles into account.
Although we hypothesize that there will be systematic reporting differences across groups and that adjusting for these differences will alter DSH comparisons, the direction of such differences is difficult to predict. Health domains related to physically intensive activities could be particularly sensitive to reporting differences because of different occupational experiences (e.g., physical labor vs. sedentary jobs). Emotional symptoms may also be especially sensitive to reporting differences, because of differences in social and cultural understandings and expressions of mental and emotional distress and illness. Finally, there may be substantial differences across Latino groups based on both origin region and nativity. Bzostek et al.’s (2007) summary of previous research suggests that Mexican-born and US-born individuals may perceive and report “normal” health differently.
Data and Methods
Data for this study come from the second wave of the Los Angeles Family and Neighborhood Survey (L.A.FANS-2), conducted in 2006–2008. L.A.FANS is based on a multistage, probability sample designed to represent the population of Los Angeles County (Sastry et al. 2006). The interview completion rate among all eligible adult respondents in L.A.FANS-2 was 59 percent (Peterson et al. 2011). Response rates varied within a narrow range by ethnicity. For example, they were 58 percent for Latinos and 64 percent for non-Latino whites. Our sample includes Latino adult respondents and US-born white adult respondents. Non-Latino, non-white respondents as well as whites born outside of the United States were excluded from our analyses. There were 1,468 cases with valid information for the self-rated health measures and vignette ratings used in our analyses. We used imputation with chained equations (Royston 2009) to impute a small number of missing predictor variables for 49 cases (3% of the sample).
Variables
Self-assessed domain-specific health (DSH)
Our analyses examine respondents’ self-assessments of health in six domains: physical functioning, role limitations, bodily pain, vitality, social functioning, and mental health. These six domains were drawn from the SF-36 health assessment, a widely-used, well-validated metric for measuring health status in a general way that does not focus on a particular age group, health profile, or disease state (Reed, 1998; Ware et al., 1995; Ware & Sherbourne 1992). Although the SF-36 includes eight domains of health, our analyses using L.A.FANS focus on only six of these domains, for two reasons. First, we do not include the domain of general health in our analyses. L.A.FANS-2 did not include general health status vignette questions (i.e., respondents rating the general health status of hypothetical individuals) because the focus of L.A.FANS was on understanding general health through examining the individual domains of health. Second, L.A.FANS-2 combined two of the SF health domains (role limitations due to physical problems and role limitations due to emotional problems) into a single domain that captures role limitations in general. The six domains of DSH used in our analyses are intended to represent the key components of health status.
Vignette ratings
After asking respondents to rate a set of their own domain-specific health measures, L.A.FANS-2 asked each respondent to rate a set of brief vignettes that described the same health domain for hypothetical individuals using the same response categories as in the self-assessment measure. All self-assessments were completed prior to the set of hypothetical assessments. Table 1 presents a summary of the vignettes and the corresponding self-assessment questions included in L.A.FANS-2, representing the six domains of DSH.
Table 1.
Summary of L.A.FANS-2 Self-Reported Health Status and Vignettes, 2006–2008
| Domain | Health status question | Vignette |
|---|---|---|
| 1. Physical functioning | During the past 4 weeks, how much did health problems limit your physical activities (such as walking or climbing stairs)? | [NAME] goes walking every day for half an
hour, about one mile. [NAME] does not do any strenuous sports because she/he feels out of breath when he/she walks very quickly or runs. |
| Would you say not at all, very little, somewhat, a lot, or severely?” | How much did health problems limit [NAME]’s physical activities? | |
| Would you say not at all, very little, somewhat, a lot, or severely? | ||
|
| ||
| 2. Role limitations | During the past 4 weeks, how much difficulty did you have doing work, both at home and on the job, because of health or emotional problems? | [NAME] suffers from allergies every month. Because of the symptoms, he/she is unable to go to work for one or two days but has no problem catching up with his/her tasks. |
| Would you say none at all, very little, some, a lot, or severe? | How much difficulty did [NAME] have doing work because of his/her health? | |
| Would you say none at all, very little, some, a lot, or severe? | ||
|
| ||
| 3. Social functioning | During the past 4 weeks, how much did health or emotional problems limit your social activities with family or friends? | [NAME] is usually an outgoing and cheerful person who has many friends and enjoys going out. Three or four days a month, he/she feels sad all day so tends to avoid people. |
| Would you say not at all, very little, somewhat, a lot, or severely? | How much did health or emotional problems limit [NAME]’s usual social activities with family or friends? | |
| Would you say not at all, very little, somewhat, a lot, or severely? | ||
|
| ||
| 4. Pain | How much physical pain did you have during the past 4 weeks? | [NAME] has a headache once a month that gets better if he/she takes a pill. When he/she has a headache, he/she can continue to do her/his normal activities. |
| Would you say none, very mild, mild, moderate, or severe? | How much physical pain did [NAME] have? | |
| Would you say none, very mild, mild, moderate, or severe? | ||
|
| ||
| [NAME] has pain that radiates down his/her right arm and wrist when he/she is working on a computer at work. It is slightly better in the evenings when he/she does not use a computer. | ||
| How much physical pain did [NAME] have? | ||
| Would you say none, very mild, mild, moderate, or severe? | ||
|
| ||
| 5. Vitality | During the past 4 weeks, how much energy did you have? | [NAME] is not a physically active person but enjoys a walk around the neighborhood most weekends. Whenever he/she walks a mile or more, he/she feels tired afterwards and needs to rest for an hour or so. |
| Would you say none, a little, some, a lot, or very much? | How much energy did [NAME] have? | |
| Would you say none, a little, some, a lot, or very much? | ||
|
| ||
| [NAME] feels tired every afternoon, which makes any task that he/she does a great effort. Whenever he/she does the dishes, tidies the house, or prepares a meal for more than 10 minutes he/she needs to sit down and rest. | ||
| How much energy did [NAME] have? | ||
| Would you say none, a little, some, a lot, or very much? | ||
|
| ||
| 6. Emotional problems | During the past 4 weeks, how much have you been bothered by emotional problems (such as feeling anxious, depressed or irritable)? | [NAME] feels nervous and anxious. He/She worries and thinks negatively about the future, but feels better when he/she is not alone or when doing something that really interests him/her. When he/she is alone he/she tends to feel useless and empty. |
| Would you say not at all, very mildly, mildly, moderately, or severely? | How much was [NAME] bothered by emotional problems? | |
| Would you say not at all, very mildly, mildly, moderately, or severely? | ||
In the vignettes, the hypothetical individual’s name was randomly varied across respondents using a pre-specified list intended to signify both sex and racial/ethnic diversity. See Sastry et al. (2013) and Sastry & Pebley (2005) for more details about the design of the DSH and vignette measures in L.A.FANS-2.
Ethnicity and nativity status
We use the following categories to capture ethnicity and nativity status among Latinos, based on respondents’ ethnicity and place of birth/country of origin: 1) US-born white; 2) US-born Mexican; 3) US-born non-Mexican Latino; 4) Mexican immigrant; and 5) Non-Mexican Latino immigrant. The great majority (89 percent) of non-Mexican Latinos in the sample were from the countries of Central America. The remainder was from a wide range of countries in South America and the Caribbean. Further subdivision of the category of non-Mexican Latinos or of the immigrant subgroups by age at immigration resulted in sample sizes too small for analysis. Although limited sample sizes precluded us from incorporating duration in the US into our analyses, the (unweighted) distribution of time in the US was relatively similar among Mexican and non-Mexican Latino immigrants. On average, Mexican immigrants reported having been in the US for 21.5 years and non-Mexican Latino immigrants reported having lived in the US for 20.6 years. The large majority of both groups (nearly 91 percent among Mexican and 87 percent among non-Mexican Latino immigrants) had been in the US for at least 10 years, and relatively few (2 percent among Mexican immigrants and 3 percent among non-Mexican Latino immigrants) reported living in the US for fewer than five years.
Additional immigration/acculturation variables
We also include three immigration and acculturation-related variables: Spanish language of interview and measures of social and linguistic acculturation. Language of interview is important both as a measure of linguistic integration and because previous research suggests differences in the meaning of Spanish and English response categories in SRH (Angel & Thoits 1987; Bzostek et al. 2007; Shetterly et al. 1996; Viruell-Fuentes et al 2011). L.A.FANS-2 collected two other acculturation-related items, both derived from a bi-dimensional acculturation scale developed by Marín et al. (1987) for Latino populations in the US. The Marín scale included two domains: social interaction with others of the same or different race/ethnicity and language use in various settings (e.g., language spoken at home, preferred language for reading a paper, listening to radio or TV). L.A.FANS-2 included 6 of the 12 items in the original scale.
Most of the acculturation items included in L.A.FANS-2 focus on language use, and only two focus on the social interaction domain. The social items ask respondents, regardless of ethnicity, how many of their close friends and coworkers are from the same ethnic group as the respondent. We use only the question about close friends because not everyone in the sample is employed (and, in particular, Latino women are less likely than men or non-Latino women to be employed). The response categories for the question about the ethnicity of the respondent’s close friends range from 1 (all of the respondent’s close friends) to 4 (none of the respondent’s close friends). We include a dichotomous version of this measure, which is coded as 0 if the respondent reports that all or most of the respondent’s close friends are the same ethnicity as the respondent, and 1 if all or most of the respondent’s close friends are of other ethnicities or the respondent’s close friends are equally split between other ethnicities and the respondent’s own ethnicity. Respondents who report having a more ethnically diverse group of close friends may be more likely to experience the culturally-influenced habits and behaviors and understanding of health of other groups.
The language acculturation scale we use is based on four questions asking which language the respondent speaks and reads best, and which language the respondent speaks and reads most often. The scale is intended to capture the language in which the respondent primarily functions verbally. This measure was developed by Creighton et al. (2012), who conducted principal components analysis on the language items. As they report, the first factor from the unrotated matrix of the unweighted data captured over 90% of the variance. Our analyses use a standardized version of this measure (mean of 0 and standard deviation of 1).
Control variables
The models include control variables to minimize potential confounding of the association between ethnicity and respondents’ DSH, including the following demographic characteristics: age (in years) and age-squared, sex, and whether the respondent is currently married or cohabiting versus not living with a romantic partner. We also control for several socioeconomic characteristics: the respondent’s educational attainment (less than high school, high school diploma or GED, or some post-secondary education); current employment status (working full-time; working part-time, or an unknown amount; and unemployed, not working or away from work); and whether the respondent has health insurance. We include a three-category control for the poverty stratum of the respondent’s census tract to account for the oversample in L.A.FANS of poor and very poor tracts (Sastry et al., 2006).
The models also include the following measures of the respondent’s health, health care, and health-related behaviors: whether the respondent has ever been diagnosed with a severe condition (heart attack, cancer, heart disease or lung disease) or diagnosed with another chronic condition (high blood pressure or hypertension, diabetes or high blood sugar, arthritis or rheumatism, or asthma); whether the respondent has a regular source of health care; whether the respondent is obese (using interviewer-measured height and weight in most cases, and self-reported height and weight in approximately 12 percent of cases where measurements were not available); a dichotomous indicator of depressive symptoms from the Composite International Diagnostic Interview Short-Form (CIDI-SF) Depression Inventory (Kessler et al. 1998); whether the respondent currently smokes; and the respondent’s SRH in L.A.FANS-1 (the previous survey wave).
Analytic strategy
We first present descriptive statistics for the full analytic sample and separately by categories of ethnicity/nativity (Table 2). Second, we use ordered logistic regression models to assess whether there are ethnic differences in respondents’ ratings of the hypothetical vignettes in the six domains; these models are estimated with and without covariates (Table 3). Significant differences by ethnicity in these models would provide initial evidence of systematic differences in rating styles (DIF) across groups. Third, we estimate the corresponding models predicting respondents’ self-assessments in each of the same six domains using ordered logistic regression models, with and without covariates (Models 1 & 2 for each domain in Table 4).
Table 2.
Descriptive statistics by ethnicity and nativity status, adult respondents in Los Angeles Family and Neighborhood Study, Wave 2 (L.A.FANS-2), 2006–2008
| Total | U.S.born, non-Latino white | U.S.-born Mexican | U.S.-born non-Mexican Latino | Mexican immigrant | Non-Mexican Latino immigrant | |
|---|---|---|---|---|---|---|
| N (Unweighted) | 1468 | 375 | 342 | 66 | 506 | 179 |
| Language & Acculturation measures | ||||||
| Interviewed in Spanish vs. English (%) | 26.5% | 0.0% | 2.5% ** | 9.0% ** | 71.6% ** | 64.0% ** |
| All/most friends are of different ethnicities, or split halfway (%) | 36.2% | 41.2% | 47.2% | 54.0% | 20.5% ** | 31.6% |
| Mean linguistic acculturation scale (sd) | 0.2 (.05) | 1.0 (.02) | 0.5 (.05) ** | 0.3 (.1) ** | −.9 (.05) ** | −.9 (.08) ** |
| Demographic Information | ||||||
| Mean age in years (sd) | 42.4 (.9) | 49.5 (1.4) | 29.8 (1.4) ** | 24.1 (1.5) ** | 42.5 (1.2) ** | 44.7 (2.6) |
| Male vs. female (%) | 56.7% | 58.5% | 52.7% | 64.9% | 59.6% | 46.4% |
| Married/cohabiting vs. single (%) | 49.5% | 56.1% | 32.0% ** | 20.5% ** | 56.7% | 48.2% |
| Socioeconomic Status | ||||||
| Educational attainment (%)a | ||||||
| <High school | 27.6% | 5.4% | 16.7% ** | 15.0% * | 60.7% ** | 52.1% ** |
| HS Diploma/GED | 18.0% | 14.0% | 21.5% | 27.4% | 20.2% | 17.6% |
| Some post-secondary | 54.5% | 80.6% | 61.9% | 57.6% | 19.1% | 30.3% |
| Current employment status (%)a | ||||||
| Employed full-time | 51.5% | 51.3% | 44.1% | 36.0% | 59.9% | 49.0% |
| Working part-time/unknown amount | 14.1% | 12.7% | 23.0% | 7.6% | 9.4% | 17.6% |
| Unemployed/not working/away from work | 34.5% | 36.0% | 32.9% | 56.4% | 30.7% | 33.4% |
| Covered by health insurance vs. uninsured (%) | 71.5% | 88.9% | 72.3% ** | 67.6% ** | 52.9% ** | 52.2% ** |
| Census tract-level poverty stratuma | ||||||
| Very poor (top 10% of poverty distribution) | 9.5% | 0.5% | 9.6% ** | 10.1% ** | 18.8% ** | 19.5% ** |
| Poor (60–89% of poverty distribution) | 35.5% | 13.5% | 39.0% | 68.5% | 53.6% | 56.1% |
| Non-poor (bottom 60% of poverty distribution) | 55.0% | 86.0% | 51.4% | 21.4% | 27.6% | 24.3% |
| Health & Health-Related Behavior | ||||||
| Diagnosed severe condition vs. no condition (%) | 9.8% | 13.8% | 4.7% ** | 3.0% | 5.7% ** | 17.4% |
| Diagnosed other chronic condition (%) | 39.5% | 49.7% | 29.9% ** | 22.7% * | 31.9% ** | 44.3% |
| Has usual source of health care (%) | 75.7% | 89.4% | 73.6% ** | 68.6% ** | 60.2% ** | 69.3% ** |
| Obese (%) | 31.3% | 25.8% | 29.9% | 42.4% | 38.8% * | 31.8% |
| Depressive symptoms meet diagnostic criteria vs. do not (%) | 12.4% | 14.7% | 9.2% | 23.3% | 10.3% | 11.7% |
| Fair/poor self-rated health (SRH) in previous survey wave (%) | 13.5% | 6.1% | 7.6% | 14.4% | 23.8% ** | 33.3% ** |
| Missing information about poor SRH in previous wave (%) | 14.3% | 8.4% | 12.5% | 32.7% ** | 16.9% * | 28.4% ** |
| Current smoker vs. non-smoker (%) | 16.4% | 17.8% | 13.5% | 4.6% ** | 16.7% | 19.2% |
p<.05,
p<.01,
Pearson chi-square tests (for categorical measures) and t-tests (for continuous measures) compared with US-born, non-Latino whites.
F-test of distribution compared with US-born, non-Latino whites.
Notes: All estimates have been weighted using the L.A.FANS-2 sampling weights.
Table 3.
Ordered logistic regression models predicting respondents’ ratings of hypothetical vignette characters’ health (higher values = worse health), L.A.FANS-2, 2006–2008, N= 1468
| Mental health |
Physical functioning |
Social functioning |
Role limitations |
|||||
|---|---|---|---|---|---|---|---|---|
| No covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | |
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||
| 1) U.S.-born Mexican | 0.15 3,4 (.2) | 0.54 (.28) | −0.22 (.2) | −0.10 (.24) | 0.06 (.22) | 0.35 (.28) | −0.32 (.21) | −0.21 (.25) |
| 2) U.S.-born non-Mexican Latino | −0.23 3,4 (.25) | 0.51 (.35) | −0.67 (.57) | −0.40 (.57) | −0.80 (.47) | −0.32 (.52) | −0.49 (.36) | −0.29 (.4) |
| 3) Mexican immigrant | −0.87 **,1,2 (.21) | 0.37 (.36) | −0.67 ** (.2) | −0.08 (.32) | −0.35 (.21) | 0.16 (.33) | −0.56 ** (.2) | −0.02 (.32) |
| 4) Non-Mexican Latino immigrant | −0.94 **,1,2 (.31) | 0.01 (.41) | −0.63 * (.31) | −0.01 (.39) | 0.04 (.31) | 0.45 (.42) | −0.71 * (.31) | −0.32 (.37) |
| Log pseudo-likelihood | −1918.75 | −1821.29 | −1953.07 | −1917.51 | −1986.66 | −1938.66 | −2002.46 | −1954.56 |
| a Wald chi-square test statistic (4 df) | 31.06 ** | 85.11 ** | 12.66 * | 44.08 ** | 6.22 | 44.67 * | 10.21 * | 54.35 ** |
|
| ||||||||
| Pain 1 (head) |
Pain 2 (arm) |
Vitality 1 (walk) |
Vitality 2 (tired) |
|||||
| No covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | |
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||
| 1) U.S.-born Mexican | −0.05 2,3,4 (.21) | 0.29 2,3,4 (.27) | 0.18 3 (.21) | 0.60 * (.26) | −0.02 (.2) | 0.01 (.24) | −0.01 2,3 (.21) | 0.10 (.26) |
| 2) U.S.-born non-Mexican Latino | −1.66 **, 1 (.42) | −1.24 **,1 (.44) | −0.09 (.33) | 0.39 (.42) | −0.07 (.51) | 0.00 (.56) | −0.73 *, 1 (.33) | −0.47 (.47) |
| 3) Mexican immigrant | −2.28 **, 1 (.21) | −0.90 *, 1 (.36) | −0.62 **, 1 (.2) | 0.37 (.4) | 0.00 (.22) | 0.08 (.36) | −0.60 **, 1 (.21) | 0.13 (.38) |
| 4) Non-Mexican Latino immigrant | −2.05 **, 1 (.36) | −1.00 *, 1 (.43) | −0.02 (.36) | 0.77 (.41) | 0.51 (.33) | 0.55 (.37) | −0.72 (.38) | −0.12 (.41) |
| Log pseudo-likelihood | −1838.59 | −1711.89 | −1869.80 | −1791.91 | −1686.65 | −1666.11 | −1895.81 | −1857.99 |
| a Wald chi-square test statistic (4 df) | 152.53 ** | 325.04 ** | 16.7 ** | 76.82 ** | 2.82 | 24.13 | 14.75 ** | 45.54 * |
Notes: *p<.05, **p<.01, compared with white US-born. Superscripted numbers indicate significant differences among Latino subgroups (p<.05). Superscripted number 1 indicates that the coefficient for that group was significantly (p<.05) different than US-born Mexicans, superscripted number 2 indicates a significant difference from US-born non-Mexican Latinos, superscripted number 3 indicates a significant difference from Mexican immigrants, and superscripted number 4 indicates a significant difference from non-Mexican Latino immigrants. Models “with covariates” included controls for the following variables: Age, gender, marital status, Spanish language of interview, social acculturation, linguistic acculturation, employment status, educational attainment, census tract-level poverty stratum, insurance coverage status, regular source of health care, self-rated health in previous survey wave, diagnosed severe conditions, diagnosed other chronic conditions, obesity, current smoking, and depressive symptoms. All estimates have been weighted using the L.A.FANS-2 sampling weights, and standard errors have been adjusted to account for clustering at the individual level. Missing data on covariates were imputed using imputation with chained equations in Stata. Because of the design of L.A.FANS, a sizeable number of respondents in Wave 2 were not interviewed in Wave 1. For these respondents, we include a flag in our regression models with covariaties to indicate that they were not interviewed in Wave 1.
Test statistic results are for Wald chi-square tests of the joint significance of the group of race/ethnicity variables.
p<.05,
p<.01.
Table 4.
Ordered logistic regression models predicting respondents’ self-rated health across subdomains with and without adjustments for vignette ratings (higher values = worse health), L.A.FANS-2, 2006–2008, N = 1468
| Mental health |
Physical functioning |
Social functioning |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
|
|
|
|
|
|
|
||||
| Standard ologit |
Vignette-Adjusted |
Standard ologit |
Vignette-Adjusted |
Standard ologit |
Vignette-Adjusted |
||||
| No covar. β (se) | With covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | With covar. β (se) | |
| Race/ethnicity (vs. U.S.-born non-Latino white) | |||||||||
| 1) U.S.-born Mexican | −0.25 (.22) | −0.28 (.28) | −0.42 (.56) | −0.98 **,3 (.25) | −0.40 3 (.34) | −0.32 (.59) | −0.61 * (.28) | −0.57 (.36) | 0.06 (.62) |
| 2) U.S.-born non-Mexican Latino | −0.14 (.5) | −0.65 (.72) | −0.17 (1.05) | −0.49 (.6) | 0.52 (.64) | 0.84 (.8) | −0.14 (.56) | −0.46 (.86) | 1.24 4 (1.12) |
| 3) Mexican immigrant | 0.07 (.21) | −0.12 (.4) | 0.14 (.7) | −0.23 1 (.21) | 0.59 1,4 (.46) | 0.95 4 (.78) | −0.08 4 (.25) | −0.32 4 (.54) | 0.41 4 (1.07) |
| 4) Non-Mexican Latino immigrant | −0.43 (.31) | −0.61 (.59) | −0.27 (.78) | −0.80 * (.34) | −0.63 3 (.59) | −0.26 3 (.86) | −0.89 *,3 (.38) | −1.69 *,3 (.8) | −1.83 2,3 (1.21) |
| a Log pseduo-likelihood/log likelihood | −1666.89 | −1477.49 | −3209.56 | −1554.73 | −1347.58 | −3159.28 | −1116.73 | −959.24 | −2774.82 |
| b Wald chi-square test statistic (4 df) | 3.95 | 149.82 ** | 1.62 | 19.03 ** | 184.73 ** | 7.78 | 9.43 | 139.27 ** | 8.05 |
|
| |||||||||
| Role limitations |
Pain |
Vitality |
|||||||
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
|
|
|
|
|
|
|
||||
| Standard ologit |
Vignette-Adjusted |
Standard ologit |
Vignette-Adjusted |
Standard ologit |
Vignette-Adjusted |
||||
| No covar. β (se) | With covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | With covar. β (se) | No covar. β (se) | With covar. β (se) | With covar. β (se) | |
| Race/ethnicity (vs. U.S.-born non-Latino white) | |||||||||
| 1) U.S.-born Mexican | −0.69 * (.27) | −0.24 (.34) | 0.40 (.49) | −0.56 * (.22) | −0.16 4 (.28) | −0.62 (.48) | −0.19 (.18) | −0.10 (.24) | 0.08 (.47) |
| 2) U.S.-born non-Mexican Latino | −0.41 (.55) | −0.06 (.99) | 0.71 (1.21) | −0.51 (.45) | −0.28 (.45) | −0.19 (.73) | −0.54 (.49) | −0.74 (.43) | 0.00 (.65) |
| 3) Mexican immigrant | −0.27 (.24) | 0.34 (.49) | 1.08 (.72) | −0.22 (.21) | −0.12 4 (.38) | −0.07 4 (.68) | −0.06 (.2) | 0.08 (.34) | 0.13 (.56) |
| 4) Non-Mexican Latino immigrant | −0.58 (.37) | −0.52 (.63) | 0.23 (.84) | −0.79 * (.35) | −1.11 *1,3 (.46) | −1.70 *,3 (.82) | −0.21 (.4) | −0.35 (.5) | −0.18 (.63) |
| a Log pseduo-likelihood/log likelihood | −1329.30 | −1168.44 | −3040.59 | −1951.74 | −1790.76 | −5487.19 | −1976.78 | −1878.72 | −5321.21 |
| b Wald chi-square test statistic (4 df) | 7.55 | 91.15 ** | 3.35 | 10.12 * | 148.47 ** | 9.66 * | 2.17 | 84.18 ** | 0.63 |
Notes: *p<.05, **p<.01, compared with white US-born. Superscripted numbers indicate significant differences among Latino subgroups (p<.05). Superscripted number 1 indicates that the coefficient for that group was significantly (p<.05) different than US-born Mexicans, superscripted number 2 indicates a significant difference from US-born non-Mexican Latinos, superscripted number 3 indicates a significant difference from Mexican immigrants, and superscripted number 4 indicates a significant difference from non-Mexican Latino immigrants. Models “with covariates” included controls for the following variables: Age, gender, marital status, Spanish language of interview, social acculturation, linguistic acculturation, employment status, educational attainment, census tract-level poverty stratum, insurance coverage status, regular source of health care, self-rated health in previous survey wave, diagnosed severe conditions, diagnosed other chronic conditions, obesity, current smoking, and depressive symptoms. All estimates have been weighted using the L.A.FANS-2 sampling weights, and standard errors have been adjusted to account for clustering at the individual level. Missing data on covariates were imputed using imputation with chained equations in Stata. Because of the design of L.A.FANS, a sizeable number of respondents in Wave 2 were not interviewed in Wave 1. For these respondents, we include a flag in our regression models with covariaties to indicate that they were not interviewed in Wave 1.
The ologit routine in Stata used for our ordered logistic regression models is estimated using pseudo-likelihood estimation and reports the log pseudo-likelihood. In contrast, the vignette-adjusted models use the gllamm routine in Stata, which uses actual maximum likelihood estimation. We therefore present the true log likelihood for the vignette-adjusted models.
Test statistic results are for Wald chi-square tests of the joint significance of the group of race/ethnicity variables.
p<.05,
p<.01.
In the fourth and final step, we examine the effects of vignette-based adjustments for DIF on our results by comparing results with and without these adjustments (Model 3 in Table 4). The “vignette-adjusted” models are hierarchical ordered logit models, developed by Gary King and colleagues. More detailed description of these models can be found in King et al. (2004) and King & Wand (2007).
These models allow thresholds between response categories in a particular domain of DSH to vary across individuals and by explanatory variables, using the data from the vignettes for identification. They rely on two key assumptions: (1) that all respondents understand and interpret the hypothetical individual’s health described in the vignette in exactly the same way (since all respondents receive identical vignette descriptions), except for a random error term (“vignette equivalence”); and (2) that respondents use the same response selection process for vignettes as for self-reports (“response consistency”). We model the cut-points with the same set of covariates used in the standard ordered logit models. Differences in the results between the unadjusted and adjusted models indicate that adjusting for DIF changes our conclusions regarding Latino/white differentials in these health domains.
In the vignette-adjusted statistical models of self-rated health, the data are arranged so that each individual in the sample contributes at least two observations. One observation is a self-report of their own health status, while a second observation is their response to the vignette question for the same health domain (for health domains that have two vignette items, each individual contributes three observations). These “stacked” models include a covariate(s) to distinguish the vignette report(s) from the self-report; the models also include covariates just for the self-assessments that are operationalized by an interaction with a dummy variable for the self-assessment (the main effect of which is omitted). By allowing the thresholds to vary, this model relaxes the assumption of proportional odds that underlies standard ordered logistic regression models. The entire estimation procedure is described in Rabe-Hesketh & Skronda (2002).
All analyses are conducted using Stata MP 14.0 (StataCorp 2015) and use the L.A.FANS sample weights, which account for non-response, attrition, and unequal probability of selection. We include controls for respondents’ census tract-level poverty stratum to account for the oversample of poor and very poor neighborhoods in L.A.FANS. We report robust standard errors that account for clustering of the observations at the individual level.
For each of the six health domains in the vignette-adjusted models, respondent i’s latent health status, Yi*, is modeled as:
| (1) |
where Xi comprises the following covariates: age, gender, marital status, Spanish language of interview, the social acculturation measure, the linguistic acculturation measure, employment status, educational attainment, tract-level poverty stratum, insurance coverage status, having a regular source of health care, diagnosed severe conditions and other chronic conditions, obesity, current smoking, depressive symptoms, and SRH in L.A.FANS-1; β are parameters, and εi is a residual error term. The five-category ordered observed responses k = 1,…5—corresponding to reports of limitations due to health problems, such as “not at all” (1), “very little” (2), “somewhat” (3), “a lot” (4), and “severely” (5)—are generated through a threshold model with person-specific thresholds τik,
| (2) |
The four thresholds are modeled as:
| (3) |
where Vi are covariates (comprising some or all of the covariates in Xi) and γk are parameters.
Each domain has either one or two corresponding vignettes in the L.A.FANS data; we use vignette reports only from the same health domain. The jth vignette, j = (1) or (1, 2), depending on the health domain, has a similar ordered-response model,
| (4) |
where θj is the true health status for the person described in the jth vignette (and takes the same value for all respondents based on the assumption of vignette equivalence) and uij is a random person-specific error term associated with the ith individual’s response to the jth vignette question. The observed vignette responses are generated by the same thresholds as shown in Equation (2) for the corresponding self-reports of health status:
| (5) |
where the thresholds are modeled as in (3).
Results
Table 2 displays weighted descriptive statistics for the sample. The first row shows the unweighted sample sizes for each of the five ethnicity/nativity groups. Approximately 57 percent of the sample is male, the average age is 42 years, and about half of the sample is currently married or cohabiting. There is considerable variation across ethnic/nativity groups for several covariates, particularly age and educational attainment. For example, US-born, especially white, respondents have higher average levels of education than respondents born elsewhere. The average age of respondents ranges from 24 years among US-born non-Mexican Latinos to 50 years among US-born whites. Language of interview also varies. Although 27 percent of the overall sample was interviewed in Spanish, this ranged from 0 percent among the US-born white respondents to 72 percent among Mexican immigrants. The average score on the linguistic acculturation index varied dramatically across groups. Significantly more US-born whites have health insurance coverage and a regular source of health care than each Latino subgroup in the sample. The prevalence of obesity in the sample is high, at 31 percent overall. All of the covariates are included as controls throughout the analysis (with the exception of the models that include no controls).
Vignette ratings using ordered logistic regression models
Table 3 presents coefficients and estimated standard errors from the ordered logistic regression models predicting vignette ratings for each of the six health domains, both without and with adjustment for the covariates described above. Positive coefficients indicate worse ratings and negative values indicate better ratings, relative to the reference group. For example, the first coefficient in the table indicates that, without covariates, US-born Mexicans have 16 percent higher odds (exp[0.15]) on average than US-born whites of rating mental health in the hypothetical vignette in a particular category or a worse one. The asterisks in the table represent statistically significant differences relative to US-born whites, and the superscripted numbers indicate significant differences among the Latino subgroups. A superscripted number 1, for example, indicates that the coefficient is significantly (p<.05) different from US-born Mexicans.
The first column within each domain shows unadjusted differences in vignette ratings. There are no statistically significant differences between the Latino subgroups and US-born whites or among the Latinos subgroups in respondents’ ratings of the social functioning and walking vitality vignettes. For all six of the other vignettes, however, Latino immigrants rate the vignettes significantly less severely than US-born whites. Among the Latino subgroups, there are several cases in which Latino immigrants (particularly Mexicans) rate the vignettes less severely than US-born Mexicans. There are fewer significant differences between US-born non-Mexican Latinos and the immigrant subgroups (although always in the direction of immigrants rating the vignettes less severely), and no significant differences between the Mexican and non-Mexican Latino immigrants in the severity they assign to the vignettes.
For all domains except pain, white-Latino subgroup differences disappear once covariates are included. In the case of head pain, all of the other Latino groups still rate the health of the vignette individual as significantly better than both US-born whites and US-born Mexicans even after the covariates are added. The only other statistically significant difference once covariates are included is that US-born Mexicans rate the arm pain described in the vignette as worse than US-born whites. Thus, although the unadjusted models suggest a number of differences in vignette ratings across groups, in every case except head pain, these differences are not statistically significant once the covariates are included in the models.
Self-assessments without vignette adjustments
Table 4 presents coefficients from standard ordered logit models of self-ratings, with and without covariates, along with the corresponding coefficients from the vignette-adjusted models. Estimates in the first model (no covariates) indicate that US-born Mexicans have significantly better ratings than US-born whites for four of the six domains of DSH, and non-Mexican Latino immigrants have significantly better self-assessments than US-born whites for three domains. In no cases do any of the Latino groups have significantly worse ratings than US-born whites.
With the inclusion of covariates in model 2, most of the differences in DSH between US-born white and Latino respondents are attenuated and become statistically non-significant. The two differences that remain statistically significant in model 2 indicate that non-Mexican Latino immigrants report significantly better social functioning and significantly less pain than US-born whites. Thus, although many of the differences disappear once controls are added, the only differences that remain significant suggest better health among Latino immigrants than among US-born whites.
The superscripted numbers beside the coefficients indicate statistically significant differences among the Latino subgroups. These results suggest that non-Mexican Latino immigrants, in addition to reporting better health than US-born whites as described above, also stand out as having especially good health relative to Mexicans (both US-born and immigrants). Specifically, even after controls are included in the models, they report better physical and social functioning and lower levels of pain than Mexican immigrants, and lower levels of pain than US-born Mexicans. The only other statistically significant difference among the Latino subgroups in the models with controls is that US-born Mexicans report significantly better physical functioning than Mexican immigrants.
Self-assessments with vignette adjustments
In model 3 in Table 4, we predict respondents’ DSH while using the vignette ratings to adjust for differential rating styles. As described above, our analyses predicting vignette ratings (Table 3) found that US-born Mexicans and US-born whites both rated head pain more severely than the other Latino subgroups. In the model predicting respondents’ own DSH in the pain subdomain (model 2 in Table 4), we found that these two groups (along with Mexican immigrants) reported significantly higher levels of pain than non-Mexican Latino immigrants. In model 3 in Table 4, we combine these findings. After accounting for rating styles (model 3), we see that although non-Mexican Latino immigrants no longer report significantly less pain than US-born Mexicans, they still report significantly less pain than US-born whites and Mexican immigrants.
The ordered logit models predicting DSH revealed significant differences in the physical and social functioning subdomains (model 2). Some of these differences disappear once we adjust for vignette ratings in model 3. For example, although US-born Mexicans reported significantly better physical functioning than Mexican immigrants in model 2, this difference is not significant once we account for vignette ratings in model 3. Additionally, although non-Mexican Latino immigrants reported significantly better social functioning than US-born whites in model 2, this difference is not statistically significant in model 3. The differences that remain statistically significant in these two domains suggest that non-Mexican Latino immigrants often stand out as having better social and physical functioning than other Latinos.
Discussion
In this paper, we use data from the second wave of the Los Angeles Family and Neighborhood Study to examine differences in Latinos’ and whites’ self-assessments of domain-specific health (DSH) across six domains drawn from the widely-used SF-36: physical functioning, role limitations, bodily pain, vitality, social functioning, and mental health. We compare respondents’ DSH in these domains using both conventional methods and methods that allow us to adjust for different rating styles across groups. Our results point to three primary conclusions.
First, despite consistent evidence from the literature that Latinos tend to rate their overall health (SRH) more poorly than whites, and that foreign-born Latinos report worse SRH than their US-born counterparts, this pattern is not true of self-reports in individual health domains. For several domains (physical functioning, social functioning, and pain), we find significantly better health reports among Latino immigrants than among US-born Latinos. The differences in results for these types of questions (DSH versus SRH) may be due in part to translation issues, which appear to be more problematic for the response categories used in the SRH question than those in the DSH questions. However, there may be other causes as well. For example, ethnic, nativity, and national origin groups may implicitly use different weights for each domain in responding to the SRH question. If Latinos give heavier weight than whites to particular domains in which Latino health is poorer when answering the SRH question, it could account for at least part of the ethnic differences observed in reporting SRH and DSH.
Second, our analysis of potential differences in rating styles across groups indicates that these differences vary considerably across subdomains. There are particularly large differences between US-born whites and US-born Mexicans, on one hand, and the other Latino subgroups, on the other hand, in the severity they assign to the head pain vignette. US-born Mexicans and whites consistently interpret the vignette individual’s head pain more severely than the other Latino groups. At the bivariate level, we observe the same pattern (more severe vignette ratings among US-born whites and sometimes US-born Mexicans than among the other Latino subgroups) for many of the other domains of health. But once we include control variables, we see little evidence of systematic differences by ethnicity in reporting styles for the other domains of health other than head pain. If this result is replicated with other data, it would be important to investigate why head pain is perceived differently for US-born Mexicans and whites versus other Latinos. One difference in the wording of the vignettes (Table 1) is that in the head pain vignette, the hypothetical individual is able to continue regular functioning, while in many of the other vignettes, he/she is not. We also speculate that head pain may be perceived differently in the US or portrayed differently in American media than in Latin America. However, we have no way of determining whether differences in wording or perceptions of head pain play a role in the results.
A third finding is that both with and without the vignette adjustments, non-Mexican Latino immigrants report better health than other groups in the areas of social and physical functioning and pain. In fact, all of the differences that are statistically significant in the models including the full array of covariates and vignette adjustments (Table 4, model 3) involve non-Mexican Latino immigrants. None of the other differences—either between US-born whites and other Latino subgroups, or among the other Latino subgroups—is statistically significant in the final models. Non-Mexican Latino immigrants in our sample represent a small but fairly heterogeneous group: As described above, most are from Central America and the remainder from the rest of Latin America. Central Americans have a very different immigrant history from Mexicans – originally arriving in the US to flee civil war in their home countries rather than immigrating to the US primarily for economic reasons. We speculate that these experiences may have affected their assessments of their own social and physical function and of pain.
Like most studies, our analyses have some limitations. The sample sizes for certain groups are small, which limited our ability to identify statistically significant differences across groups. Throughout the text and tables, we only interpret differences that were statistically significant at conventional levels (p<.05). Small sample sizes also prevented us from distinguishing among nationality groups of non-Mexican Latinos and, for immigrants, by age at immigration and level of acculturation. We have conducted a fairly large number of statistical tests, suggesting further caution in the interpretation of significant results. L.A.FANS included only a limited set of measures of acculturation, and it is possible that other measures would have yielded different results. The information in L.A.FANS, however, is considerably more detailed than in many studies in the literature, which rely exclusively on home language use, interview language, or duration of time in the U.S. as proxy measures of acculturation. Our measure of “non-severe” chronic conditions may also be limited, because it depends on whether respondents have access to and have used health care providers. This concern is at least partially addressed by controlling for whether respondents have health insurance and a regular source of health care. Finally, as in all studies using vignette-adjusted models, the assumptions necessary for applying the vignette-based correction to the problem of response category differential item functioning could affect our results if violated.
Overall, our findings underscore the advantages of domain-specific ratings when evaluating ethnic differences in self-assessments of health. We find, for example, that differences across ethnic groups vary considerably across specific domains of health. Studies using the SRH measure alone are not able to identify these important distinctions. In the future, health surveys focused on health status differences among social groups may want to consider increasing the amount of information collected and reducing reporting style biases by collecting the entire SF-36 (or the shorter SF-12 or SF-8) (Ware, 2000), rather than—or in addition to—the single SRH question. Because the SF-36, SF-12 and SF-8 collect self-reports about a wider range of health-related outcomes, they provide a more complete picture of health, albeit still subject to reporting style bias. The anchoring vignettes approach we use here is one potential method for overcoming reporting style bias, when the underlying assumptions are met. Collecting the entire SF-36, SF-12, or SF-8, however, could pose a heavy burden for many surveys because of the number of questions and the amount of interview time required. An alternative solution is the development and testing of measures of health and/or specific health domains that are less subject to differences in reporting styles.
Table A1.
Ordered logistic regression models predicting respondents’ ratings of hypothetical vignette characters’ health (higher values = worse health), L.A.FANS-2, 2006–2008, N= 1468
| Mental health | Physical functioning | Social functioning | Role limitations | Pain 1 (head) | Pain 2 (arm) | Vitality 1 (walk) | Vitality 2 (tired) | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| β (se) | β (se) | β (se) | β (se) | β (se) | β (se) | β (se) | β (se) | |
| Without covariates | ||||||||
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||
| 1) U.S.-born Mexican | 0.15 3,4 | −0.22 | 0.06 | −0.32 | −0.05 2,3,4 | 0.18 3 | −0.02 | −0.01 2,3 |
| (.2) | (.2) | (.22) | (.21) | (.21) | (.21) | (.2) | (.21) | |
| 2) U.S.-born non-Mexican Latino | −0.23 3,4 | −0.67 | −0.80 | −0.49 | −1.66 **, 1 | −0.09 | −0.07 | −0.73 *, 1 |
| (.25) | (.57) | (.47) | (.36) | (.42) | (.33) | (.51) | (.33) | |
| 3) Mexican immigrant | −0.87 **,1, 2 | −0.67 ** | −0.35 | −0.56 ** | −2.28 **, 1 | −0.62 **, 1 | 0.00 | −0.60 **, 1 |
| (.21) | (.2) | (.21) | (.2) | (.21) | (.2) | (.22) | (.21) | |
| 4) Non-Mexican Latino immigrant | −0.94 **,1, 2 | −0.63 * | 0.04 | −0.71 * | −2.05 **, 1 | −0.02 | 0.51 | −0.72 |
| (.31) | (.31) | (.31) | (.31) | (.36) | (.36) | (.33) | (.38) | |
| Threshold cutpoints | ||||||||
| cutpoint 1 | −5.07 | −3.62 | −3.29 | −2.94 | −4.64 | −2.75 | −3.91 | −3.26 |
| (.31) | (.24) | (.26) | (.21) | (.3) | (.21) | (.32) | (.23) | |
| cutpoint 2 | −2.52 | −1.50 | −1.08 | −0.77 | −2.13 | −0.09 | −2.17 | −2.48 |
| (.18) | (.15) | (.14) | (.14) | (.16) | (.15) | (.18) | (.17) | |
| cutpoint 3 | −0.92 | 0.40 | 0.69 | 0.95 | −0.37 | 1.53 | 0.15 | −1.27 |
| (.15) | (.14) | (.14) | (.15) | (.14) | (.17) | (.14) | (.13) | |
| cutpoint 4 | 0.62 | 2.27 | 2.52 | 2.54 | 1.92 | 3.31 | 2.99 | 0.76 |
| (.15) | (.18) | (.2) | (.22) | (.17) | (.27) | (.22) | (.13) | |
| Log likelihood | −1918.75 | −1953.07 | −1986.66 | −2002.46 | −1838.59 | −1869.80 | −1686.65 | −1895.81 |
| a Wald chi-square test statistic (4 df) | 31.06 ** | 12.66 * | 6.22 | 10.21 * | 152.53 ** | 16.7 ** | 2.82 | 14.75 ** |
|
| ||||||||
| With covariates | ||||||||
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||
| 1) U.S.-born Mexican | 0.54 | −0.10 | 0.35 | −0.21 | 0.29 2,3,4 | 0.60 * | 0.01 | 0.10 |
| (.28) | (.24) | (.28) | (.25) | (.27) | (.26) | (.24) | (.26) | |
| 2) U.S.-born non-Mexican Latino | 0.51 | −0.40 | −0.32 | −0.29 | −1.24 **,1 | 0.39 | 0.00 | −0.47 |
| (.35) | (.57) | (.52) | (.4) | (.44) | (.42) | (.56) | (.47) | |
| 3) Mexican immigrant | 0.37 | −0.08 | 0.16 | −0.02 | −0.90 *, 1 | 0.37 | 0.08 | 0.13 |
| (.36) | (.32) | (.33) | (.32) | (.36) | (.4) | (.36) | (.38) | |
| 4) Non-Mexican Latino immigrant | 0.01 | −0.01 | 0.45 | −0.32 | −1.00 *, 1 | 0.77 | 0.55 | −0.12 |
| (.41) | (.39) | (.42) | (.37) | (.43) | (.41) | (.37) | (.41) | |
| Covariates | ||||||||
| Age (in years) | 0.00 | −0.01 | 0.02 | −0.02 | 0.05 | 0.02 | −0.02 | −0.05 |
| (.03) | (.03) | (.03) | (.03) | (.03) | (.03) | (.03) | (.03) | |
| Age-squared | −8E-05 | −3E-05 | −2E-04 | 2E-04 | 0.00 | −1E-04 | 0.00 | 4E-04 |
| (.) | (.) | (.) | (.) | (.) | (.) | (.) | (.) | |
| Male (vs. female) | −0.21 | 0.05 | −0.40 * | −0.17 ** | −0.51 ** | −0.35 * | −0.16 | −0.35 |
| (.18) | (.17) | (.18) | (.18) | (.17) | (.17) | (.18) | (.2) | |
| Married/cohabiting (vs. single) | 0.11 | 0.34 | 0.26 | 0.29 | −0.04 | 0.13 | 0.31 | 0.22 |
| (.21) | (.19) | (.19) | (.19) | (.2) | (.19) | (.18) | (.19) | |
| Interviewed in Spanish (vs. English) | −0.49 | −0.12 | 0.11 | −1.03 | −1.90 ** | −0.66 | 0.01 | −0.06 |
| (.35) | (.31) | (.34) | (.32) | (.41) | (.3) | (.34) | (.38) | |
| Employment status (vs. working full-time) | ||||||||
| Working part-time/unknown amount | −0.42 | 0.18 | 0.09 | −0.44 | −0.20 | −0.11 | −0.14 | −0.29 |
| (.28) | (.26) | (.3) | (.23) | (.29) | (.26) | (.23) | (.28) | |
| Unemployed/not working/away from work | −0.31 | 0.17 | 0.32 | 0.03 | −0.25 | 0.05 | −0.20 | −0.70 ** |
| (.23) | (.2) | (.22) | (.22) | (.2) | (.19) | (.2) | (.24) | |
| Educational attainment (vs. less than HS) | ||||||||
| HS Diploma/GED | −0.06 | 0.36 | 0.15 | −0.06 | −0.43 | −0.43 | 0.59 * | 0.02 |
| (.28) | (.32) | (.31) | (.27) | (.27) | (.23) | (.28) | (.29) | |
| Some post-secondary | 0.04 | 0.50 * | 0.39 | 0.34 | 0.47 | 0.19 | 0.35 | 0.00 |
| (.27) | (.26) | (.26) | (.24) | (.24) | (.23) | (.24) | (.25) | |
| Covered by health insurance | −0.48 * | 0.22 | −0.17 | −0.31 * | 0.03 | −0.42 | 0.02 | −0.15 |
| (.22) | (.23) | (.22) | (.23) | (.23) | (.23) | (.24) | (.23) | |
| Has diagnosed severe condition | 0.18 | 0.20 | −0.08 | 0.20 | 0.31 | 1.14 ** | 0.17 | 0.00 |
| (.32) | (.28) | (.32) | (.3) | (.33) | (.34) | (.3) | (.32) | |
| Current smoker | 0.25 | −0.15 | 0.42 * | 0.24 | 0.15 | 0.19 | −0.21 | 0.00 |
| (.23) | (.22) | (.2) | (.24) | (.25) | (.28) | (.21) | (.2) | |
| Exhibits symptoms of depression | 0.06 | −0.04 | −0.24 | 0.01 | 0.39 | 0.16 | 0.28 | 0.30 |
| (.22) | (.28) | (.24) | (.3) | (.22) | (.21) | (.26) | (.25) | |
| Has usual source of health care | −0.41 * | 0.07 | −0.46 * | 0.54 | 0.20 | 0.06 | 0.08 | −0.17 |
| (.2) | (.24) | (.2) | (.23) | (.21) | (.21) | (.27) | (.25) | |
| Linguistic acculturation scale | 0.27 | 0.13 | 0.02 | −0.13 | 0.04 | 0.28 | −0.06 | 0.29 |
| (.19) | (.18) | (.2) | (.18) | (.19) | (.18) | (.2) | (.18) | |
| Obese | −0.36 * | 0.12 | −0.02 | −0.09 | −0.06 | 0.03 | −0.14 | −0.28 |
| (.18) | (.16) | (.2) | (.17) | (.16) | (.16) | (.19) | (.2) | |
| All/most friends are of different ethnicities, or split halfway | 0.12 | −0.47 ** | 0.06 | 0.01 | −0.26 | 0.16 | 0.03 | 0.05 |
| (.19) | (.18) | (.19) | (.17) | (.18) | (.17) | (.18) | (.18) | |
| Fair/poor self-rated health (SRH) in previous survey wave | 0.13 | 0.29 | −0.53 | 0.00 | −0.71 * | −0.59 * | 0.26 | −0.09 |
| (.27) | (.3) | (.35) | (.26) | (.31) | (.26) | (.3) | (.29) | |
| Missing information about poor SRH in previous wave | −0.26 | −0.30 | −0.08 | −0.03 | 0.04 | −0.03 | −0.23 | 0.10 |
| (.24) | (.25) | (.28) | (.27) | (.25) | (.24) | (.3) | (.28) | |
| Diagnosed other chronic condition | 0.39 | 0.07 | 0.43 * | 0.29 | 0.03 | 0.00 | 0.00 | 0.33 |
| (.23) | (.2) | (.21) | (.19) | (.21) | (.21) | (.2) | (.21) | |
| Census tract-level poverty stratum (vs. non-poor) | ||||||||
| Very poor | −0.59 * | −0.01 | −0.19 | −0.17 | 0.28 | 0.43 | 0.15 | −0.14 |
| (.25) | (.24) | (.24) | (.24) | 0.26 | (.22) | 0.29 | (.25) | |
| Poor | −0.33 | −0.25 | −0.18 | 0.03 | 0.40 | 0.50 * | −0.07 | −0.14 |
| (.19) | (.19) | (.21) | (.2) | 0.21 | (.2) | 0.21 | (.22) | |
|
| ||||||||
| Threshold cutpoints | ||||||||
| cutpoint 1 | −5.43 | −3.25 | −2.75 | −3.13 | −3.97 | −1.84 | −3.99 | −4.63 |
| (.96) | (.81) | (.76) | (.67) | 0.86 | (.72) | 0.75 | (.75) | |
| cutpoint 2 | −2.91 | −1.09 | −0.50 | −0.89 | −1.13 | 0.95 | −2.25 | −3.83 |
| (.94) | (.77) | (.74) | (.66) | 0.81 | (.69) | 0.75 | (.75) | |
| cutpoint 3 | −1.18 | 0.89 | 1.36 | 0.92 | 0.89 | 2.72 | 0.12 | −2.58 |
| (.9) | (.76) | (.74) | (.66) | 0.80 | (.71) | 0.73 | (.75) | |
| cutpoint 4 | 0.45 | 2.81 | 3.24 | 2.56 | 3.32 | 4.61 | 3.01 | −0.47 |
| (.88) | (.76) | (.75) | (.66) | 0.81 | (.74) | 0.77 | (.75) | |
| Log pseudo-likelihood | −1821.29 | −1917.51 | −1938.66 | −1954.56 | −1711.89 | −1791.91 | −1666.11 | −1857.99 |
| a Wald chi-square test statistic (4 df) | 85.11 ** | 44.08 ** | 44.67 * | 54.35 ** | 325.04 ** | 76.82 ** | 24.13 | 45.54 * |
Notes: *p<.05, **p<.01, compared with white US-born. Superscripted numbers indicate significant differences among Latino subgroups (p<.05). Superscripted number 1 indicates that the coefficient for that group was significantly (p<.05) different than US-born Mexicans, superscripted number 2 indicates a significant difference from US-born non-Mexican Latinos, superscripted number 3 indicates a significant difference from Mexican immigrants, and superscripted number 4 indicates a significant difference from non-Mexican Latino immigrants. All estimates have been weighted using the L.A.FANS-2 sampling weights, and standard errors have been adjusted to account for clustering at the individual level. Missing data on covariates were imputed using imputation with chained equations in Stata. Because of the design of L.A.FANS, a sizeable number of respondents in Wave 2 were not interviewed in Wave 1. For these respondents, we include a flag in our regression models with covariaties to indicate that they were not interviewed in Wave 1.
Test statistic results are for Wald chi-square tests of the joint significance of the group of race/ethnicity variables.
p<.05
p<.01.
Table A2.
Ordered logistic regression models predicting respondents’ self-rated health across subdomains with and without adjustments for vignette ratings (higher values = worse health), L.A.FANS-2, 2006–2008, N = 1468
| Mental health |
Physical functioning |
Social functioning |
Role limitations |
Pain |
Vitality |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Standard ologit |
Vignette- Adjusted |
Standard ologit |
Vignette- Adjusted |
Standard ologit |
Vignette- Adjusted |
Standard ologit |
Vignette- Adjusted |
Standard ologit |
Vignette- Adjusted |
Standard ologit |
Vignette- Adjusted |
|||||||
| No covar. β (se) |
With covar. β (se) |
With covar. β (se) |
No covar. β (se) |
With covar. β (se) |
With covar. β (se) |
No covar. β (se) |
With covar. β (se) |
With covar. β (se) |
No covar. β (se) |
With covar. β (se) |
With covar. β (se) |
No covar. β (se) |
With covar. β (se) |
With covar. β (se) |
No covar. β (se) |
With covar. β (se) |
With covar. β (se) |
|
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||||||||||||
| 1) U.S.-born Mexican | −0.25 | −0.28 | −0.42 | −0.98 **,3 | −0.40 3 | −0.32 | −0.61 * | −0.57 | 0.06 | −0.69 * | −0.24 | 0.40 | −0.56 * | −0.16 4 | −0.62 | −0.19 | −0.10 | 0.08 |
| (.22) | (.28) | (.56) | (.25) | (.34) | (.59) | (.28) | (.36) | (.62) | (.27) | (.34) | (.49) | (.22) | (.28) | (.48) | (.18) | (.24) | (.47) | |
| 2) U.S.-born non-Mexican Latino | −0.14 | −0.65 | −0.17 | −0.49 | 0.52 | 0.84 | −0.14 | −0.46 | 1.24 4 | −0.41 | −0.06 | 0.71 | −0.51 | −0.28 | −0.19 | −0.54 | −0.74 | 0.00 |
| (.5) | (.72) | (1.05) | (.6) | (.64) | (.8) | (.56) | (.86) | (1.12) | (.55) | (.99) | (1.21) | (.45) | (.45) | (.73) | (.49) | (.43) | (.65) | |
| 3) Mexican immigrant | 0.07 | −0.12 | 0.14 | −0.23 1 | 0.59 1,4 | 0.95 4 | −0.08 4 | −0.32 4 | 0.41 4 | −0.27 | 0.34 | 1.08 | −0.22 | −0.12 4 | −0.07 4 | −0.06 | 0.08 | 0.13 |
| (.21) | (.4) | (.7) | (.21) | (.46) | (.78) | (.25) | (.54) | (1.07) | (.24) | (.49) | (.72) | (.21) | (.38) | (.68) | (.2) | (.34) | (.56) | |
| 4) Non-Mexican Latino immigrant | −0.43 | −0.61 | −0.27 | −0.80 * | −0.63 3 | −0.26 3 | −0.89 *,3 | −1.69 *,3 | −1.83 2,3 | −0.58 | −0.52 | 0.23 | −0.79 * | −1.11 *1,3 | −1.70 *,3 | −0.21 | −0.35 | −0.18 |
| (.31) | (.59) | (.78) | (.34) | (.59) | (.86) | (.38) | (.8) | (1.21) | (.37) | (.63) | (.84) | (.35) | (.46) | (.82) | (.4) | (.5) | (.63) | |
| Covariates | ||||||||||||||||||
| Age (in years) | - | 0.00 | −0.02 | - | −0.01 | −0.05 | - | 0.00 | −0.01 | - | 0.03 | 0.07 | - | 0.03 | 0.03 | - | −0.03 | −0.05 |
| - | (.03) | (.06) | - | (.03) | (.06) | - | (.04) | (.06) | - | (.03) | (.05) | - | (.03) | (.05) | - | (.03) | (.05) | |
| Age-squared | - | 0.00 | 0.00 | - | 0.00 | 0.00 | - | 0.00 | 0.00 | - | 0.00 | 0.00 | - | 0.00 | 0.00 | - | 0.00 | 0.00 |
| - | (.) | (.) | - | (.) | (.) | - | (.) | (.) | - | (.) | (.) | - | (.) | (.) | - | (.) | (.) | |
| Male (vs. female) | - | −0.14 | −0.04 | - | −0.03 | −0.02 | - | −0.05 | 0.35 | - | 0.13 | 0.43 | - | −0.03 | 0.34 | - | −0.18 | −0.16 |
| - | (.21) | (.36) | - | (.23) | (.35) | - | (.26) | (.43) | - | (.23) | (.34) | - | (.19) | (.32) | - | (.18) | (.3) | |
| Married/cohabiting (vs. single) | - | −0.02 | 0.27 | - | 0.29 | 0.36 | - | −0.03 | −0.11 | - | −0.21 | −0.50 | - | 0.20 | 0.25 | - | 0.05 | 0.04 |
| - | (.2) | (.36) | - | (.23) | (.37) | - | (.25) | (.49) | - | (.23) | (.33) | - | (.2) | (.33) | - | (.19) | (.32) | |
| Interviewed in Spanish (vs. English) | - | −0.38 | −0.07 | - | −0.42 | −0.66 | - | −0.60 | −1.45 | - | −0.33 | 0.02 | - | 0.10 | 0.65 | - | −0.50 | 0.09 |
| - | (.38) | (.68) | - | (.42) | (.71) | - | (.47) | (.8) | - | (.42) | (.63) | - | (.35) | (.58) | - | (.37) | (.47) | |
| Employment status (vs. working full-time) | ||||||||||||||||||
| Working part-time/unknown amount | - | 0.24 | 0.46 | - | 0.13 | −0.27 | - | −0.12 | 0.93 | - | 0.42 | 0.50 | - | 0.52 * | 0.96 * | - | −0.25 | −0.72 |
| - | (.27) | (.51) | - | (.32) | (.57) | - | (.38) | (.69) | - | (.3) | (.5) | - | (.25) | (.47) | - | (.27) | (.43) | |
| Unemployed/not working/away from work | - | 0.25 | 1.00 ** | - | 0.42 | 0.37 | - | 0.37 | 1.37 ** | - | 0.25 | 0.58 | - | 0.12 | 0.42 | - | −0.04 | 0.48 |
| - | (.23) | (.38) | - | (.25) | (.43) | - | (.28) | (.51) | - | (.26) | (.35) | - | (.22) | (.37) | - | (.23) | (.36) | |
| Educational attainment (vs. less than HS) | ||||||||||||||||||
| HS Diploma/GED | - | −0.43 | −1.11 * | - | −0.56 | −1.01 | - | −0.41 | −0.13 | - | 0.10 | 0.17 | - | −0.46 | −0.22 | - | −0.65 * | −0.74 * |
| - | (.26) | (.51) | - | (.34) | (.57) | - | (.37) | (.55) | - | (.35) | (.49) | - | (.27) | (.43) | - | (.26) | (.35) | |
| Some post-secondary | - | −0.55 | −0.84 * | - | −0.65 | −1.47 ** | - | −0.57 | −1.25 * | - | −0.33 | −0.90 | - | −0.63 ** | −1.37 ** | - | −0.54 * | −0.53 |
| - | (.25) | (.4) | - | (.34) | (.49) | - | (.34) | (.6) | - | (.33) | (.48) | - | (.22) | (.38) | - | (.23) | (.36) | |
| Covered by health insurance | - | −0.10 | −0.10 | - | −0.08 | −0.16 | - | −0.22 | 0.02 | - | −0.23 | −0.07 | - | −0.05 | −0.19 | - | 0.55 * | 0.74 * |
| - | (.27) | (.44) | - | (.3) | (.45) | - | (.37) | (.56) | - | (.34) | (.51) | - | (.23) | (.38) | - | (.26) | (.33) | |
| Has diagnosed severe condition | - | 0.45 | −0.05 | - | 0.68 * | 0.60 | - | 0.99 * | 1.30 * | - | 0.57 | 0.78 | - | 0.17 | −0.19 | - | 0.78 * | 0.99 * |
| - | (.33) | (.53) | - | (.28) | (.45) | - | (.38) | (.52) | - | (.39) | (.58) | - | (.32) | (.43) | - | (.34) | (.49) | |
| Current smoker | - | 0.08 | 0.24 | - | 0.31 | 0.58 | - | 0.01 | −0.27 | - | 0.01 | −0.20 | - | 0.05 | −0.04 | - | 0.24 | 0.49 |
| - | (.26) | (.41) | - | (.26) | (.42) | - | (.34) | (.53) | - | (.32) | (.51) | - | (.25) | (.39) | - | (.26) | (.32) | |
| Exhibits symptoms of depression | - | 2.15 ** | 2.31 ** | - | 0.95 ** | 1.58 ** | - | 2.33 ** | 3.31 ** | - | 1.76 ** | 2.27 ** | - | 1.10 ** | 1.40 ** | - | 0.67 * | 0.72 |
| - | (.24) | (.39) | - | (.29) | (.4) | - | (.3) | (.43) | - | (.3) | (.41) | - | (.25) | (.42) | - | (.28) | (.38) | |
| Has usual source of health care | - | −0.16 | −0.10 | - | −0.42 | −0.58 | - | −0.23 | 0.11 | - | −0.31 | −0.86 | - | −0.33 | −0.86 * | - | −0.36 | 0.21 |
| - | (.3) | (.44) | - | (.32) | (.48) | - | (.38) | (.54) | - | (.35) | (.51) | - | (.23) | (.4) | - | (.28) | (.32) | |
| Linguistic acculturation scale | - | −0.04 | 0.02 | - | 0.16 | 0.36 | - | −0.38 | −0.36 | - | 0.09 | 0.48 | - | 0.10 | 0.05 | - | −0.04 | −0.35 |
| - | (.21) | (.38) | - | (.25) | (.44) | - | (.26) | (.54) | - | (.25) | (.37) | - | (.21) | (.35) | - | (.18) | (.28) | |
| Obese | - | 0.25 | 0.30 | - | 0.17 | 0.21 | - | 0.02 | −0.04 | - | 0.27 | 0.55 | - | 0.06 | 0.04 | - | 0.21 | 0.45 |
| - | (.21) | (.35) | - | (.23) | (.35) | - | (.27) | (.38) | - | (.23) | (.32) | - | (.19) | (.32) | - | (.18) | (.26) | |
| All/most friends are of different ethnicities, or split halfway | - | −0.04 | 0.29 | - | 0.54 * | 0.95 * | - | 0.13 | −0.49 | - | 0.09 | −0.21 | - | 0.31 | 0.47 | - | −0.20 | −0.17 |
| - | (.2) | (.32) | - | (.26) | (.38) | - | (.3) | (.42) | - | (.27) | (.36) | - | (.22) | (.36) | - | (.17) | (.3) | |
| Fair/poor self-rated health (SRH) in previous survey wave | - | 0.55 | 0.55 | - | 0.70 * | 0.78 * | - | 0.08 | 0.95 | - | 0.24 | 0.36 | - | 0.87 ** | 1.74 ** | - | 0.73 ** | 0.58 |
| - | (.33) | (.47) | - | (.28) | (.4) | - | (.39) | (.66) | - | (.34) | (.45) | - | (.3) | (.42) | - | (.27) | (.39) | |
| Missing information about poor SRH in previous wave | - | −0.11 | 0.11 | - | −0.28 | −0.08 | - | 0.36 | 1.12 ** | - | 0.27 | 0.53 | - | 0.03 | −0.02 | - | 0.28 | 0.50 |
| - | (.28) | (.49) | - | (.34) | (.57) | - | (.29) | (.43) | - | (.27) | (.42) | - | (.26) | (.52) | - | (.26) | (.33) | |
| Diagnosed other chronic condition | - | 0.05 | 0.18 | - | 1.15 ** | 1.48 ** | - | 0.66 * | 0.60 | - | 1.07 ** | 0.90 * | - | 0.90 ** | 1.40 ** | - | 0.15 | −0.28 |
| - | (.21) | (.37) | - | (.22) | (.38) | - | (.26) | (.43) | - | (.24) | (.39) | - | (.19) | (.32) | - | (.21) | (.33) | |
| Census tract-level poverty stratum (vs. non-poor) | ||||||||||||||||||
| Very poor | - | −0.14 | 1.19 * | - | 0.18 | 0.74 | - | −0.21 | −0.03 | - | 0.03 | 0.49 | - | −0.33 | −0.39 | - | 0.01 | 0.54 |
| - | (.28) | (.5) | - | (.31) | (.51) | - | (.3) | (.48) | - | (.31) | (.46) | - | (.27) | (.46) | - | (.32) | (.33) | |
| Poor | - | 0.06 | 0.91 * | - | −0.14 | 0.17 | - | −0.11 | −0.50 | - | −0.12 | −0.07 | - | −0.16 | −0.37 | - | 0.20 | 0.44 |
| - | (.23) | (.4) | - | (.26) | (.43) | - | (.28) | (.45) | - | (.3) | (.45) | - | (.24) | (.41) | - | (.23) | (.29) | |
|
| ||||||||||||||||||
| Vignette indicator | - | - | 4.39 ** | - | - | 3.68 * | - | - | 5.10 ** | - | - | 5.91 ** | - | - | 3.77 ** | - | - | 2.06 |
| - | - | (1.47) | - | - | (1.46) | - | - | (1.5) | - | - | (1.37) | - | - | (1.18) | - | - | (1.4) | |
| Vignette indicator | - | - | - | - | - | - | - | - | - | - | - | - | - | - | 2.61 * | - | - | 3.29 * |
| - | - | - | - | - | - | - | - | - | - | - | - | - | - | (1.18) | - | - | (1.41) | |
|
| ||||||||||||||||||
| Standard ologit cutpoints | ||||||||||||||||||
| Cutpoint 1 | 0.42 | 0.16 | - | 0.33 | 1.72 | - | 1.08 | 1.03 | - | 0.73 | 2.48 | - | −0.18 | 1.09 | - | −1.85 | −2.55 | - |
| (.15) | (.82) | - | (.16) | (.98) | - | (.18) | (1.) | - | (.17) | (.98) | - | (.14) | (.75) | - | (.13) | (.88) | - | |
| Cutpoint 2 | 1.32 | 1.21 | - | 1.22 | 2.84 | - | 2.06 | 2.26 | - | 1.67 | 3.64 | - | 0.56 | 1.96 | - | 0.16 | −0.37 | - |
| (.15) | (.82) | - | (.17) | (.99) | - | (.21) | (.99) | - | (.19) | (1.) | - | (.13) | (.75) | - | (.12) | (.89) | - | |
| Cutpoint 3 | 2.15 | 2.20 | - | 1.94 | 3.76 | - | 3.04 | 3.47 | - | 2.40 | 4.54 | - | 1.31 | 2.85 | - | 1.90 | 1.55 | - |
| (.17) | (.83) | - | (.2) | (1.02) | - | (.25) | (1.01) | - | (.21) | (1.05) | - | (.14) | (.75) | - | (.14) | (.94) | - | |
| Cutpoint 4 | 3.34 | 3.57 | - | 3.12 | 5.15 | - | 3.57 | 4.09 | - | 3.41 | 5.68 | - | 2.61 | 4.32 | - | 3.37 | 3.11 | - |
| (.24) | (.86) | - | (.23) | (.99) | - | (.34) | (1.01) | - | (.25) | (1.07) | - | (.19) | (.79) | - | (.27) | (.97) | - | |
| Vignette-adjusted cutpoints | ||||||||||||||||||
| Cutpoint 1 | ||||||||||||||||||
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||||||||||||
| U.S.-born Mexican | - | - | 0.03 | - | - | 0.09 | - | - | 0.75 | - | - | 0.71 | - | - | −0.37 | - | - | 0.76 |
| - | - | (.52) | - | - | (.43) | - | - | (.52) | - | - | (.37) | - | - | (.29) | - | - | (.52) | |
| U.S.-born non-Mexican Latino | - | - | 0.96 | - | - | 0.36 | - | - | 1.86 * | - | - | 0.89 * | - | - | 0.05 | - | - | 1.38 |
| - | - | (.59) | - | - | (.68) | - | - | (.73) | - | - | (.44) | - | - | (.45) | - | - | (.72) | |
| Mexican immigrant | - | - | 0.41 | - | - | 0.21 | - | - | 0.82 | - | - | 0.75 | - | - | 0.05 | - | - | 0.60 |
| - | - | (.63) | - | - | (.63) | - | - | (.93) | - | - | (.48) | - | - | (.41) | - | - | (.57) | |
| Non-Mexican Latino immigrant | - | - | 0.55 | - | - | 0.50 | - | - | 0.01 | - | - | 0.89 | - | - | −0.16 | - | - | 1.14 |
| - | - | (.76) | - | - | (.62) | - | - | (.87) | - | - | (.61) | - | - | (.5) | - | - | (.67) | |
| Age (in years) | - | - | −0.01 | - | - | −0.04 | - | - | 0.00 | - | - | 0.04 | - | - | −0.01 | - | - | 0.00 |
| - | - | (.07) | - | - | (.04) | - | - | (.05) | - | - | (.04) | - | - | (.04) | - | - | (.05) | |
| Age-squared | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 |
| - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | |
| Male (vs. female) | - | - | 0.08 | - | - | 0.01 | - | - | 0.38 | - | - | 0.27 | - | - | 0.31 | - | - | −0.23 |
| - | - | (.33) | - | - | (.25) | - | - | (.37) | - | - | (.24) | - | - | (.18) | - | - | (.34) | |
| Interviewed in Spanish (vs. English) | - | - | 0.20 | - | - | −0.27 | - | - | −0.92 | - | - | 0.30 | - | - | 0.17 | - | - | 0.73 |
| - | - | (.59) | - | - | (.53) | - | - | (.6) | - | - | (.37) | - | - | (.36) | - | - | (.52) | |
| Employment status (vs. working full-time) | ||||||||||||||||||
| Working part-time/unknown amount | - | - | 0.08 | - | - | −0.47 | - | - | 1.11 | - | - | −0.08 | - | - | 0.33 | - | - | −0.57 |
| - | - | (.5) | - | - | (.46) | - | - | (.65) | - | - | (.46) | - | - | (.28) | - | - | (.44) | |
| Unemployed/not working/away from work | - | - | 0.81 | - | - | −0.06 | - | - | 1.01 * | - | - | 0.32 | - | - | 0.33 | - | - | 1.31 ** |
| - | - | (.36) | - | - | (.38) | - | - | (.5) | - | - | (.24) | - | - | (.19) | - | - | (.39) | |
| Covered by health insurance | - | - | −0.02 | - | - | −0.01 | - | - | 0.33 | - | - | 0.24 | - | - | −0.12 | - | - | 0.66 * |
| - | - | (.37) | - | - | (.3) | - | - | (.36) | - | - | (.28) | - | - | (.23) | - | - | (.31) | |
| Has diagnosed severe condition | - | - | −0.62 | - | - | −0.30 | - | - | 0.25 | - | - | 0.29 | - | - | 0.00 | - | - | 0.32 |
| - | - | (.45) | - | - | (.4) | - | - | (.36) | - | - | (.3) | - | - | (.3) | - | - | (.55) | |
| Current smoker | - | - | 0.34 | - | - | 0.30 | - | - | −0.24 | - | - | −0.18 | - | - | 0.02 | - | - | 0.82 * |
| - | - | (.33) | - | - | (.3) | - | - | (.42) | - | - | (.28) | - | - | (.21) | - | - | (.33) | |
| Educational attainment (vs. less than HS) | ||||||||||||||||||
| HS Diploma/GED | - | - | −0.82 | - | - | −0.43 | - | - | 0.44 | - | - | 0.00 | - | - | 0.36 | - | - | 0.01 |
| - | - | (.48) | - | - | (.43) | - | - | (.44) | - | - | (.27) | - | - | (.26) | - | - | (.39) | |
| Some post-secondary | - | - | −0.29 | - | - | −0.87 ** | - | - | −0.65 | - | - | −0.62 * | - | - | −0.60 * | - | - | 0.10 |
| - | - | (.38) | - | - | (.3) | - | - | (.51) | - | - | (.28) | - | - | (.24) | - | - | (.39) | |
| Married/cohabiting (vs. single) | - | - | 0.29 | - | - | 0.12 | - | - | −0.06 | - | - | −0.23 | - | - | 0.06 | - | - | −0.06 |
| - | - | (.38) | - | - | (.25) | - | - | (.48) | - | - | (.25) | - | - | (.21) | - | - | (.35) | |
| Exhibits symptoms of depression | - | - | −0.30 | - | - | 0.83 ** | - | - | 0.83 ** | - | - | 0.38 | - | - | −0.41 | - | - | −0.13 |
| - | - | (.42) | - | - | (.25) | - | - | (.3) | - | - | (.22) | - | - | (.24) | - | - | (.42) | |
| Has usual source of health care | - | - | 0.11 | - | - | −0.08 | - | - | 0.35 | - | - | −0.53 * | - | - | −0.37 | - | - | 0.90 ** |
| - | - | (.36) | - | - | (.35) | - | - | (.37) | - | - | (.27) | - | - | (.24) | - | - | (.34) | |
| Linguistic acculturation scale | - | - | 0.08 | - | - | 0.25 | - | - | 0.04 | - | - | 0.43 | - | - | −0.13 | - | - | −0.44 |
| - | - | (.31) | - | - | (.38) | - | - | (.46) | - | - | (.27) | - | - | (.23) | - | - | (.29) | |
| Obese | - | - | −0.04 | - | - | 0.01 | - | - | −0.07 | - | - | 0.23 | - | - | −0.18 | - | - | 0.08 |
| - | - | (.34) | - | - | (.26) | - | - | (.29) | - | - | (.22) | - | - | (.19) | - | - | (.29) | |
| All/most friends are of different ethnicities, or split halfway | - | - | 0.42 | - | - | 0.34 | - | - | −0.65 * | - | - | −0.37 | - | - | 0.10 | - | - | 0.07 |
| - | - | (.32) | - | - | (.25) | - | - | (.33) | - | - | (.24) | - | - | (.17) | - | - | (.34) | |
| Fair/poor self-rated health (SRH) in previous survey wave | - | - | −0.02 | - | - | 0.04 | - | - | 0.93 | - | - | 0.13 | - | - | 0.29 | - | - | 0.01 |
| - | - | (.39) | - | - | (.35) | - | - | (.66) | - | - | (.27) | - | - | (.29) | - | - | (.5) | |
| Missing information about poor SRH in previous wave | - | - | 0.18 | - | - | 0.13 | - | - | 0.79 * | - | - | 0.23 | - | - | −0.14 | - | - | 0.28 |
| - | - | (.4) | - | - | (.41) | - | - | (.36) | - | - | (.27) | - | - | (.29) | - | - | (.34) | |
| Diagnosed other chronic condition | - | - | 0.19 | - | - | 0.23 | - | - | −0.03 | - | - | −0.31 | - | - | 0.05 | - | - | −0.67 |
| - | - | (.35) | - | - | (.26) | - | - | (.35) | - | - | (.27) | - | - | (.18) | - | - | (.37) | |
| Census tract-level poverty stratum (vs. non-poor) | ||||||||||||||||||
| Very poor | - | - | 1.42 | - | - | 0.71 * | - | - | 0.22 | - | - | 0.54 | - | - | 0.29 | - | - | 0.93 ** |
| - | - | (.4) | - | - | (.32) | - | - | (.33) | - | - | (.28) | - | - | (.25) | - | - | (.33) | |
| Poor | - | - | 0.91 | - | - | 0.37 | - | - | −0.39 | - | - | 0.15 | - | - | 0.01 | - | - | 0.41 |
| - | - | (.34) | - | - | (.31) | - | - | (.33) | - | - | (.27) | - | - | (.21) | - | - | (.34) | |
| Constant | - | - | −0.15 | - | - | 1.67 | - | - | 0.73 | - | - | 2.52 * | - | - | 1.01 | - | - | −4.12 ** |
| - | - | (1.) | - | - | (1.05) | - | - | (1.06) | - | - | (1.08) | - | - | (1.21) | - | - | (1.02) | |
| Cutpoint 2 | ||||||||||||||||||
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||||||||||||
| U.S.-born Mexican | - | - | −0.37 | - | - | 0.14 | - | - | −0.49 * | - | - | −0.23 | - | - | 0.02 | - | - | −0.30 * |
| - | - | (.29) | - | - | (.27) | - | - | (.24) | - | - | (.22) | - | - | (.16) | - | - | (.14) | |
| U.S.-born non-Mexican Latino | - | - | −1.60 | - | - | 0.48 | - | - | −0.84 * | - | - | −0.25 | - | - | 0.18 | - | - | −0.36 |
| - | - | (.54) | - | - | (.37) | - | - | (.41) | - | - | (.35) | - | - | (.21) | - | - | (.22) | |
| Mexican immigrant | - | - | −0.36 | - | - | 0.23 | - | - | −0.44 | - | - | −0.38 | - | - | 0.01 | - | - | −0.35 |
| - | - | (.42) | - | - | (.33) | - | - | (.45) | - | - | (.35) | - | - | (.21) | - | - | (.18) | |
| Non-Mexican Latino immigrant | - | - | −0.41 | - | - | −0.02 | - | - | −0.23 | - | - | −0.34 | - | - | −0.03 | - | - | −0.69 * |
| - | - | (.47) | - | - | (.36) | - | - | (.35) | - | - | (.39) | - | - | (.24) | - | - | (.27) | |
| Age (in years) | - | - | −0.02 | - | - | 0.01 | - | - | 0.01 | - | - | 0.00 | - | - | −0.01 | - | - | −0.01 |
| - | - | (.05) | - | - | (.02) | - | - | (.03) | - | - | (.02) | - | - | (.02) | - | - | (.02) | |
| Age-squared | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 |
| - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | |
| Male (vs. female) | - | - | 0.09 | - | - | −0.04 | - | - | 0.07 | - | - | −0.09 | - | - | −0.02 | - | - | 0.14 |
| - | - | (.23) | - | - | (.16) | - | - | (.17) | - | - | (.12) | - | - | (.1) | - | - | (.1) | |
| Interviewed in Spanish (vs. English) | - | - | 0.30 | - | - | 0.43 | - | - | 0.56 | - | - | 0.51 * | - | - | 0.49 * | - | - | −0.08 |
| - | - | (.49) | - | - | (.31) | - | - | (.31) | - | - | (.23) | - | - | (.19) | - | - | (.22) | |
| Employment status (vs. working full-time) | ||||||||||||||||||
| Working part-time/unknown amount | - | - | 0.23 | - | - | 0.25 | - | - | −0.31 | - | - | 0.36 | - | - | −0.03 | - | - | 0.04 |
| - | - | (.26) | - | - | (.22) | - | - | (.25) | - | - | (.2) | - | - | (.14) | - | - | (.14) | |
| Unemployed/not working/away from work | - | - | −0.16 | - | - | −0.12 | - | - | −0.34 | - | - | −0.11 | - | - | −0.12 | - | - | −0.49 ** |
| - | - | (.28) | - | - | (.3) | - | - | (.23) | - | - | (.16) | - | - | (.12) | - | - | (.15) | |
| Covered by health insurance | - | - | 0.01 | - | - | 0.02 | - | - | −0.06 | - | - | −0.01 | - | - | 0.19 | - | - | −0.24 * |
| - | - | (.22) | - | - | (.15) | - | - | (.15) | - | - | (.16) | - | - | (.12) | - | - | (.11) | |
| Has diagnosed severe condition | - | - | 0.17 | - | - | −0.02 | - | - | −0.29 | - | - | −0.40 * | - | - | −0.54 * | - | - | −0.08 |
| - | - | (.28) | - | - | (.28) | - | - | (.33) | - | - | (.18) | - | - | (.21) | - | - | (.26) | |
| Current smoker | - | - | −0.52 | - | - | −0.14 | - | - | −0.17 | - | - | 0.02 | - | - | 0.00 | - | - | −0.38 * |
| - | - | (.26) | - | - | (.18) | - | - | (.19) | - | - | (.15) | - | - | (.13) | - | - | (.15) | |
| Educational attainment (vs. less than HS) | ||||||||||||||||||
| HS Diploma/GED | - | - | 0.35 | - | - | 0.09 | - | - | −0.39 | - | - | −0.08 | - | - | 0.03 | - | - | −0.17 |
| - | - | (.29) | - | - | (.27) | - | - | (.24) | - | - | (.19) | - | - | (.15) | - | - | (.16) | |
| Some post-secondary | - | - | −0.09 | - | - | 0.08 | - | - | 0.10 | - | - | 0.10 | - | - | 0.17 | - | - | −0.12 |
| - | - | (.27) | - | - | (.19) | - | - | (.28) | - | - | (.19) | - | - | (.15) | - | - | (.15) | |
| Married/cohabiting (vs. single) | - | - | 0.15 | - | - | −0.06 | - | - | −0.15 | - | - | −0.04 | - | - | −0.04 | - | - | 0.03 |
| - | - | (.31) | - | - | (.13) | - | - | (.23) | - | - | (.12) | - | - | (.11) | - | - | (.12) | |
| Exhibits symptoms of depression | - | - | 0.15 | - | - | −0.54 * | - | - | −0.28 | - | - | −0.13 | - | - | 0.13 | - | - | 0.19 |
| - | - | (.24) | - | - | (.24) | - | - | (.16) | - | - | (.14) | - | - | (.12) | - | - | (.16) | |
| Has usual source of health care | - | - | −0.15 | - | - | 0.16 | - | - | −0.11 | - | - | 0.03 | - | - | 0.13 | - | - | −0.22 |
| - | - | (.28) | - | - | (.19) | - | - | (.15) | - | - | (.16) | - | - | (.12) | - | - | (.11) | |
| Linguistic acculturation scale | - | - | 0.01 | - | - | −0.01 | - | - | 0.00 | - | - | −0.14 | - | - | −0.10 | - | - | 0.05 |
| - | - | (.23) | - | - | (.22) | - | - | (.23) | - | - | (.19) | - | - | (.13) | - | - | (.08) | |
| Obese | - | - | 0.16 | - | - | −0.19 | - | - | 0.05 | - | - | −0.10 | - | - | 0.07 | - | - | 0.05 |
| - | - | (.24) | - | - | (.18) | - | - | (.13) | - | - | (.14) | - | - | (.1) | - | - | (.1) | |
| All/most friends are of different ethnicities, or split halfway | - | - | −0.28 | - | - | 0.04 | - | - | 0.20 | - | - | 0.20 | - | - | −0.06 | - | - | −0.01 |
| - | - | (.21) | - | - | (.18) | - | - | (.14) | - | - | (.13) | - | - | (.09) | - | - | (.12) | |
| Fair/poor self-rated health (SRH) in previous survey wave | - | - | 0.09 | - | - | −0.20 | - | - | −0.20 | - | - | −0.13 | - | - | 0.10 | - | - | −0.18 |
| - | - | (.23) | - | - | (.22) | - | - | (.38) | - | - | (.17) | - | - | (.13) | - | - | (.29) | |
| Missing information about poor SRH in previous wave | - | - | 0.14 | - | - | 0.20 | - | - | −0.32 | - | - | −0.05 | - | - | 0.17 | - | - | −0.02 |
| - | - | (.26) | - | - | (.24) | - | - | (.2) | - | - | (.16) | - | - | (.15) | - | - | (.13) | |
| Diagnosed other chronic condition | - | - | −0.18 | - | - | 0.02 | - | - | −0.24 | - | - | 0.08 | - | - | 0.00 | - | - | 0.06 |
| - | - | (.25) | - | - | (.17) | - | - | (.16) | - | - | (.14) | - | - | (.09) | - | - | (.12) | |
| Census tract-level poverty stratum (vs. non-poor) | ||||||||||||||||||
| Very poor | - | - | −0.09 | - | - | −0.14 | - | - | 0.12 | - | - | −0.27 | - | - | −0.34 * | - | - | −0.30 * |
| - | - | (.24) | - | - | (.18) | - | - | (.14) | - | - | (.15) | - | - | (.13) | - | - | (.14) | |
| Poor | - | - | −0.19 | - | - | 0.11 | - | - | 0.34 * | - | - | −0.16 | - | - | −0.24 * | - | - | −0.08 |
| - | - | (.18) | - | - | (.17) | - | - | (.14) | - | - | (.14) | - | - | (.11) | - | - | (.12) | |
| Constant | - | - | 1.01 | - | - | −0.21 | - | - | 1.03 | - | - | 0.58 | - | - | 0.56 | - | - | 1.73 ** |
| - | - | (.93) | - | - | (.58) | - | - | (.66) | - | - | (.64) | - | - | (.53) | - | - | (.39) | |
| Cutpoint 3 | ||||||||||||||||||
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||||||||||||
| U.S.-born Mexican | - | - | −0.25 | - | - | −0.15 | - | - | −0.12 | - | - | −0.34 | - | - | −0.02 | - | - | 0.05 |
| - | - | (.24) | - | - | (.16) | - | - | (.18) | - | - | (.19) | - | - | (.15) | - | - | (.13) | |
| U.S.-born non-Mexican Latino | - | - | −0.39 | - | - | −0.58 | - | - | −0.34 | - | - | −0.63 * | - | - | 0.08 | - | - | −0.17 |
| - | - | (.39) | - | - | (.31) | - | - | (.24) | - | - | (.3) | - | - | (.19) | - | - | (.18) | |
| Mexican immigrant | - | - | −0.51 | - | - | −0.35 | - | - | −0.08 | - | - | −0.39 | - | - | 0.29 | - | - | 0.17 |
| - | - | (.34) | - | - | (.23) | - | - | (.24) | - | - | (.26) | - | - | (.18) | - | - | (.19) | |
| Non-Mexican Latino immigrant | - | - | −0.29 | - | - | −0.22 | - | - | 0.06 | - | - | −0.29 | - | - | 0.39 | - | - | 0.02 |
| - | - | (.37) | - | - | (.25) | - | - | (.25) | - | - | (.3) | - | - | (.22) | - | - | (.23) | |
| Age (in years) | - | - | 0.01 | - | - | 0.03 | - | - | −0.02 | - | - | −0.04 * | - | - | −0.02 | - | - | 0.02 |
| - | - | (.03) | - | - | (.02) | - | - | (.02) | - | - | (.02) | - | - | (.02) | - | - | (.01) | |
| Age-squared | - | - | 0.00 | - | - | 0.00 * | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 |
| - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | |
| Male (vs. female) | - | - | 0.01 | - | - | 0.02 | - | - | −0.09 | - | - | 0.04 | - | - | 0.09 | - | - | 0.12 |
| - | - | (.16) | - | - | (.11) | - | - | (.11) | - | - | (.12) | - | - | (.11) | - | - | (.09) | |
| Interviewed in Spanish (vs. English) | - | - | −0.15 | - | - | −0.26 | - | - | −0.19 | - | - | −0.27 | - | - | 0.12 | - | - | −0.37 * |
| - | - | (.3) | - | - | (.22) | - | - | (.2) | - | - | (.22) | - | - | (.22) | - | - | (.16) | |
| Employment status (vs. working full-time) | ||||||||||||||||||
| Working part-time/unknown amount | - | - | 0.18 | - | - | −0.08 | - | - | −0.51 * | - | - | −0.18 | - | - | −0.31 * | - | - | 0.30 * |
| - | - | (.19) | - | - | (.17) | - | - | (.2) | - | - | (.17) | - | - | (.14) | - | - | (.14) | |
| Unemployed/not working/away from work | - | - | −0.10 | - | - | 0.06 | - | - | −0.58 ** | - | - | −0.27 | - | - | −0.07 | - | - | 0.01 |
| - | - | (.19) | - | - | (.13) | - | - | (.15) | - | - | (.14) | - | - | (.12) | - | - | (.1) | |
| Covered by health insurance | - | - | 0.46 | - | - | −0.24 | - | - | −0.12 | - | - | 0.10 | - | - | 0.02 | - | - | −0.06 |
| - | - | (.19) | - | - | (.13) | - | - | (.15) | - | - | (.14) | - | - | (.12) | - | - | (.1) | |
| Has diagnosed severe condition | - | - | 0.28 | - | - | 0.07 | - | - | 0.23 | - | - | 0.25 | - | - | 0.13 | - | - | −0.13 |
| - | - | (.22) | - | - | (.18) | - | - | (.21) | - | - | (.17) | - | - | (.18) | - | - | (.18) | |
| Current smoker | - | - | 0.09 | - | - | 0.10 | - | - | 0.11 | - | - | −0.06 | - | - | −0.25 | - | - | 0.02 |
| - | - | (.17) | - | - | (.15) | - | - | (.13) | - | - | (.14) | - | - | (.13) | - | - | (.11) | |
| Educational attainment (vs. less than HS) | ||||||||||||||||||
| HS Diploma/GED | - | - | 0.42 | - | - | 0.01 | - | - | 0.11 | - | - | 0.29 | - | - | −0.09 | - | - | 0.08 |
| - | - | (.19) | - | - | (.17) | - | - | (.18) | - | - | (.18) | - | - | (.17) | - | - | (.13) | |
| Some post-secondary | - | - | 0.21 | - | - | 0.28 * | - | - | 0.11 | - | - | 0.39 * | - | - | 0.13 | - | - | 0.05 |
| - | - | (.21) | - | - | (.14) | - | - | (.17) | - | - | (.16) | - | - | (.15) | - | - | (.14) | |
| Married/cohabiting (vs. single) | - | - | −0.31 | - | - | −0.35 ** | - | - | 0.09 | - | - | 0.06 | - | - | −0.06 | - | - | −0.11 |
| - | - | (.17) | - | - | (.12) | - | - | (.13) | - | - | (.13) | - | - | (.12) | - | - | (.09) | |
| Exhibits symptoms of depression | - | - | −0.12 | - | - | −0.20 | - | - | −0.09 | - | - | −0.47 ** | - | - | −0.05 | - | - | −0.32 * |
| - | - | (.18) | - | - | (.16) | - | - | (.18) | - | - | (.17) | - | - | (.12) | - | - | (.12) | |
| Has usual source of health care | - | - | 0.30 | - | - | −0.31 * | - | - | 0.23 | - | - | 0.04 | - | - | 0.22 | - | - | −0.22 * |
| - | - | (.19) | - | - | (.14) | - | - | (.14) | - | - | (.15) | - | - | (.11) | - | - | (.11) | |
| Linguistic acculturation scale | - | - | −0.43 | - | - | −0.28 * | - | - | −0.06 | - | - | −0.19 | - | - | 0.27 * | - | - | 0.14 |
| - | - | (.14) | - | - | (.12) | - | - | (.12) | - | - | (.14) | - | - | (.11) | - | - | (.08) | |
| Obese | - | - | 0.13 | - | - | 0.14 | - | - | 0.04 | - | - | 0.00 | - | - | 0.18 | - | - | 0.00 |
| - | - | (.15) | - | - | (.11) | - | - | (.12) | - | - | (.13) | - | - | (.11) | - | - | (.09) | |
| All/most friends are of different ethnicities, or split halfway | - | - | −0.17 | - | - | 0.02 | - | - | 0.15 | - | - | 0.04 | - | - | 0.03 | - | - | −0.03 |
| - | - | (.15) | - | - | (.11) | - | - | (.12) | - | - | (.13) | - | - | (.11) | - | - | (.12) | |
| Fair/poor self-rated health (SRH) in previous survey wave | - | - | −0.21 | - | - | 0.06 | - | - | −0.12 | - | - | 0.15 | - | - | 0.16 | - | - | 0.18 |
| - | - | (.26) | - | - | (.18) | - | - | (.21) | - | - | (.19) | - | - | (.15) | - | - | (.18) | |
| Missing information about poor SRH in previous wave | - | - | −0.10 | - | - | −0.21 | - | - | −0.16 | - | - | −0.26 | - | - | −0.27 | - | - | −0.15 |
| - | - | (.18) | - | - | (.18) | - | - | (.19) | - | - | (.19) | - | - | (.15) | - | - | (.14) | |
| Diagnosed other chronic condition | - | - | −0.40 | - | - | −0.34 ** | - | - | 0.10 | - | - | −0.18 | - | - | −0.09 | - | - | 0.22 * |
| - | - | (.18) | - | - | (.13) | - | - | (.13) | - | - | (.13) | - | - | (.12) | - | - | (.1) | |
| Census tract-level poverty stratum (vs. non-poor) | ||||||||||||||||||
| Very poor | - | - | −0.59 | - | - | −0.46 ** | - | - | −0.30 | - | - | 0.01 | - | - | −0.04 | - | - | −0.19 |
| - | - | (.2) | - | - | (.16) | - | - | (.16) | - | - | (.17) | - | - | (.13) | - | - | (.13) | |
| Poor | - | - | −0.11 | - | - | −0.29 * | - | - | −0.18 | - | - | 0.13 | - | - | 0.08 | - | - | −0.01 |
| - | - | (.17) | - | - | (.14) | - | - | (.13) | - | - | (.14) | - | - | (.11) | - | - | (.09) | |
| Constant | - | - | 0.19 | - | - | 0.78 | - | - | 1.43 ** | - | - | 1.56 ** | - | - | 0.67 | - | - | 0.34 |
| - | - | (.62) | - | - | (.42) | - | - | (.52) | - | - | (.52) | - | - | (.48) | - | - | (.36) | |
| Cutpoint 4 | ||||||||||||||||||
| Race/ethnicity (vs. U.S.-born non-Latino white) | ||||||||||||||||||
| U.S.-born Mexican | - | - | 0.32 | - | - | 0.10 | - | - | −0.39 | - | - | 0.56 | - | - | −0.15 | - | - | −0.11 |
| - | - | (.18) | - | - | (.24) | - | - | (.28) | - | - | (.29) | - | - | (.16) | - | - | (.12) | |
| U.S.-born non-Mexican Latino | - | - | 0.47 | - | - | −0.18 | - | - | −0.89 * | - | - | 0.01 | - | - | −0.69 * | - | - | 0.11 |
| - | - | (.28) | - | - | (.44) | - | - | (.42) | - | - | (.47) | - | - | (.29) | - | - | (.26) | |
| Mexican immigrant | - | - | 0.36 | - | - | 0.23 | - | - | −0.76 | - | - | 1.38 ** | - | - | −0.26 | - | - | −0.02 |
| - | - | (.25) | - | - | (.33) | - | - | (.42) | - | - | (.48) | - | - | (.23) | - | - | (.17) | |
| Non-Mexican Latino immigrant | - | - | 0.41 | - | - | 0.12 | - | - | −0.57 | - | - | 1.92 ** | - | - | −0.08 | - | - | 0.07 |
| - | - | (.3) | - | - | (.42) | - | - | (.41) | - | - | (.54) | - | - | (.29) | - | - | (.22) | |
| Age (in years) | - | - | 0.03 | - | - | −0.04 | - | - | 0.00 | - | - | −0.01 | - | - | 0.00 | - | - | 0.02 |
| - | - | (.02) | - | - | (.03) | - | - | (.03) | - | - | (.03) | - | - | (.02) | - | - | (.01) | |
| Age-squared | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 | - | - | 0.00 |
| - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | - | - | (.) | |
| Male (vs. female) | - | - | 0.07 | - | - | −0.30 | - | - | 0.06 | - | - | 0.11 | - | - | 0.14 | - | - | 0.01 |
| - | - | (.12) | - | - | (.16) | - | - | (.19) | - | - | (.2) | - | - | (.12) | - | - | (.08) | |
| Interviewed in Spanish (vs. English) | - | - | 0.06 | - | - | −0.54 | - | - | −0.41 | - | - | −0.81 * | - | - | −0.34 | - | - | −0.21 |
| - | - | (.27) | - | - | (.32) | - | - | (.34) | - | - | (.36) | - | - | (.28) | - | - | (.15) | |
| Employment status (vs. working full-time) | ||||||||||||||||||
| Working part-time/unknown amount | - | - | −0.33 | - | - | −0.56 * | - | - | 0.53 * | - | - | −0.19 | - | - | 0.13 | - | - | 0.04 |
| - | - | (.2) | - | - | (.25) | - | - | (.22) | - | - | (.32) | - | - | (.18) | - | - | (.12) | |
| Unemployed/not working/away from work | - | - | −0.30 | - | - | −0.59 ** | - | - | 0.04 | - | - | −0.13 | - | - | −0.11 | - | - | 0.06 |
| - | - | (.15) | - | - | (.19) | - | - | (.2) | - | - | (.23) | - | - | (.14) | - | - | (.09) | |
| Covered by health insurance | - | - | −0.15 | - | - | −0.17 | - | - | 0.06 | - | - | −0.30 | - | - | −0.05 | - | - | −0.07 |
| - | - | (.16) | - | - | (.23) | - | - | (.21) | - | - | (.24) | - | - | (.14) | - | - | (.12) | |
| Has diagnosed severe condition | - | - | −0.22 | - | - | 0.47 | - | - | 0.08 | - | - | −0.33 | - | - | 0.12 | - | - | 0.00 |
| - | - | (.19) | - | - | (.24) | - | - | (.34) | - | - | (.32) | - | - | (.18) | - | - | (.14) | |
| Current smoker | - | - | −0.20 | - | - | −0.06 | - | - | −0.05 | - | - | −0.03 | - | - | −0.05 | - | - | 0.08 |
| - | - | (.15) | - | - | (.2) | - | - | (.25) | - | - | (.23) | - | - | (.16) | - | - | (.11) | |
| Educational attainment (vs. less than HS) | ||||||||||||||||||
| HS Diploma/GED | - | - | −0.26 | - | - | −0.07 | - | - | −0.29 | - | - | 0.25 | - | - | 0.01 | - | - | −0.04 |
| - | - | (.2) | - | - | (.25) | - | - | (.28) | - | - | (.28) | - | - | (.21) | - | - | (.13) | |
| Some post-secondary | - | - | 0.14 | - | - | 0.59 ** | - | - | 0.09 | - | - | 0.40 | - | - | −0.04 | - | - | −0.06 |
| - | - | (.17) | - | - | (.22) | - | - | (.25) | - | - | (.28) | - | - | (.18) | - | - | (.12) | |
| Married/cohabiting (vs. single) | - | - | −0.31 | - | - | 0.31 | - | - | −0.39 * | - | - | −0.07 | - | - | −0.14 | - | - | −0.06 |
| - | - | (.14) | - | - | (.19) | - | - | (.17) | - | - | (.2) | - | - | (.12) | - | - | (.1) | |
| Exhibits symptoms of depression | - | - | 0.25 | - | - | −0.20 | - | - | −0.64 ** | - | - | −0.06 | - | - | 0.04 | - | - | 0.06 |
| - | - | (.14) | - | - | (.23) | - | - | (.24) | - | - | (.23) | - | - | (.15) | - | - | (.12) | |
| Has usual source of health care | - | - | 0.10 | - | - | 0.09 | - | - | 0.30 | - | - | −0.13 | - | - | −0.36 * | - | - | −0.10 |
| - | - | (.17) | - | - | (.2) | - | - | (.22) | - | - | (.25) | - | - | (.17) | - | - | (.12) | |
| Linguistic acculturation scale | - | - | 0.27 | - | - | −0.15 | - | - | −0.35 | - | - | 0.46 | - | - | 0.02 | - | - | −0.03 |
| - | - | (.13) | - | - | (.19) | - | - | (.2) | - | - | (.26) | - | - | (.13) | - | - | (.11) | |
| Obese | - | - | 0.02 | - | - | 0.13 | - | - | 0.42 * | - | - | 0.38 | - | - | 0.02 | - | - | −0.01 |
| - | - | (.13) | - | - | (.16) | - | - | (.18) | - | - | (.21) | - | - | (.13) | - | - | (.09) | |
| All/most friends are of different ethnicities, or split halfway | - | - | 0.02 | - | - | −0.12 | - | - | −0.15 | - | - | 0.01 | - | - | 0.08 | - | - | −0.01 |
| - | - | (.14) | - | - | (.16) | - | - | (.17) | - | - | (.19) | - | - | (.11) | - | - | (.09) | |
| Fair/poor self-rated health (SRH) in previous survey wave | - | - | 0.06 | - | - | −0.27 | - | - | −0.45 | - | - | −0.24 | - | - | −0.29 | - | - | −0.03 |
| - | - | (.23) | - | - | (.26) | - | - | (.27) | - | - | (.32) | - | - | (.24) | - | - | (.14) | |
| Missing information about poor SRH in previous wave | - | - | 0.04 | - | - | 0.14 | - | - | −0.03 | - | - | 0.07 | - | - | 0.15 | - | - | −0.01 |
| - | - | (.18) | - | - | (.19) | - | - | (.24) | - | - | (.3) | - | - | (.16) | - | - | (.12) | |
| Diagnosed other chronic condition | - | - | 0.13 | - | - | 0.39 * | - | - | −0.41 * | - | - | −0.26 | - | - | −0.16 | - | - | −0.05 |
| - | - | (.14) | - | - | (.18) | - | - | (.19) | - | - | (.2) | - | - | (.12) | - | - | (.09) | |
| Census tract-level poverty stratum (vs. non-poor) | ||||||||||||||||||
| Very poor | - | - | −0.22 | - | - | −0.65 ** | - | - | −0.40 | - | - | −0.67 * | - | - | 0.00 | - | - | −0.10 |
| - | - | (.17) | - | - | (.25) | - | - | (.26) | - | - | (.32) | - | - | (.17) | - | - | (.13) | |
| Poor | - | - | −0.29 | - | - | −0.45 * | - | - | 0.06 | - | - | −0.66 ** | - | - | −0.19 | - | - | −0.19 |
| - | - | (.16) | - | - | (.21) | - | - | (.2) | - | - | (.23) | - | - | (.13) | - | - | (.11) | |
| Constant | - | - | −0.07 | - | - | 1.71 ** | - | - | 1.09 | - | - | 0.37 | - | - | 1.16 * | - | - | 0.61 |
| - | - | (.5) | - | - | (.63) | - | - | (.72) | - | - | (.85) | - | - | (.5) | - | - | (.37) | |
|
| ||||||||||||||||||
| a Log pseduo-likelihood/log likelihood | −1666.89 | −1477.49 | −1554.73 | −1347.58 | −3159.28 | −1116.73 | −959.24 | −1329.30 | −1168.44 | −3040.59 | −1951.74 | −1790.76 | −5487.19 | −1976.78 | −1878.72 | −5321.21 | ||
| b Wald chi-square test statistic (4 df) | 3.95 | 149.82 ** | 19.03 ** | 184.73 ** | 7.78 | 9.43 | 139.27 ** | 7.55 | 91.15 ** | 3.35 | 10.12 * | 148.47 ** | 9.66 * | 2.17 | 84.18 ** | 0.63 | ||
Notes: *p<.05,**p<.01, compared with white US-born. Superscripted numbers indicate significant differences among Latino subgroups (p<.05). Superscripted number 1 indicates that the coefficient for that group was significantly (p<.05) different than US-born Mexicans, superscripted number 2 indicates a significant difference from US-born non-Mexican Latinos, superscripted number 3 indicates a significant difference from Mexican immigrants, and superscripted number 4 indicates a significant difference from non-Mexican Latino immigrants. All estimates have been weighted using the L.A.FANS-2 sampling weights, and standard errors have been adjusted to account for clustering at the individual level. Missing data on covariates were imputed using imputation with chained equations in Stata. Because of the design of L.A.FANS, a sizeable number of respondents in Wave 2 were not interviewed in Wave 1. For these respondents, we include a flag in our regression models with covariaties to indicate that they were not interviewed in Wave 1.
The ologit routine in Stata used for our ordered logistic regression models is estimated using pseudo-likelihood estimation and reports the log pseudo-likelihood. In contrast, the vignette-adjusted models use the gllamm routine in Stata, which uses actual maximum likelihood estimation. We therefore present the true log likelihood for the vignette-adjusted models.
Test statistic results are for Wald chi-square tests of the joint significance of the group of race/ethnicity variables.
p<.05
p<.01.
Research Highlights.
Despite worse overall SRH among Latinos vs. whites, this is not found in domain-specific health.
US-born Mexicans and whites interpret head pain more severely than other Latino subgroups.
Non-Mexican Latino immigrants report better social & physical function & less pain than others.
Acknowledgments
The authors gratefully acknowledge support for this research from NIH grants R24HD041022, R01HD058514, R01HD051764 and R01AG022005, as well as support for Bzostek through the Robert Wood Johnson Foundation Scholars in Health Policy Research program at Harvard University.
Contributor Information
Sharon Bzostek, Rutgers University.
Narayan Sastry, University of Michigan.
Noreen Goldman, Princeton University.
Anne Pebley, University of California-Los Angeles.
Denise Duffy, University of Michigan.
References
- Angel JL, Angel RJ. Age at migration, social connections, and well-being among elderly Hispanics. Journal of Aging and Health. 1992;4(4):480–499. doi: 10.1177/089826439200400402. [DOI] [PubMed] [Google Scholar]
- Angel R, Guarnaccia PJ. Mind, body, and culture: Somatization among Hispanics. Social Science & Medicine. 1989;28(12):1229–1238. doi: 10.1016/0277-9536(89)90341-9. [DOI] [PubMed] [Google Scholar]
- Angel R, Thoits P. The impact of culture on the cognitive structure of illness. Culture, Medicine and Psychiatry. 1987;11(4):465–494. doi: 10.1007/BF00048494. [DOI] [PubMed] [Google Scholar]
- Arcia E, Skinner M, Bailey D, Correa V. Models of acculturation and health behaviors among Latino immigrants to the US. Social Science & Medicine. 2001;53(1):41–53. doi: 10.1016/s0277-9536(00)00310-5. [DOI] [PubMed] [Google Scholar]
- Bzostek S, Goldman N, Pebley A. Why do Hispanics in the USA report poor health? Social Science and Medicine. 2007;65:990– 1003. doi: 10.1016/j.socscimed.2007.04.028. [DOI] [PubMed] [Google Scholar]
- Cho Y, Frisbie WP, Hummer RA, Rogers RG. Nativity, duration of residence, and the health of Hispanic adults in the United States. International Migration Review. 2004;38(1):184–211. [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, Jiang H, Munter P. Mortality prediction with a single general self-rated health question. Journal of General Internal Medicine. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd JB, Todd M. Does self-reported health bias the measurement of health inequalities in U.S. adults? Evidence using anchoring vignettes from the health and retirement study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2011;66(4):478–489. doi: 10.1093/geronb/gbr050. [DOI] [PubMed] [Google Scholar]
- Dowd JB, Zajacova A. Does self-rated health mean the same thing across socioeconomic groups? Evidence from biomarker data. Annals of Epidemiology. 2010;20:743–749. doi: 10.1016/j.annepidem.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fayers P, Sprangers M. Understanding self-rated health. The Lancet. 2002;359:187–188. doi: 10.1016/S0140-6736(02)07466-4. [DOI] [PubMed] [Google Scholar]
- Finch BK, Hummer RA, Kolody B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hispanic Journal of Behavioral Sciences. 2001;23(4):399–429. [Google Scholar]
- Finch BK, Hummer RA, Reindl M, Vega WA. Validity of self-rated health among Latino(a)s. American Journal of Epidemiology. 2002;155(8):755–759. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. Journal of Health and Social Behavior. 2000;41(3):295–313. [PubMed] [Google Scholar]
- Franzini L, Fernandez-Esquer ME. Socioeconomic, cultural, and personal influences on health outcomes in low income Mexican-origin individuals in Texas. Social Science & Medicine. 2004;59(8):1629–1646. doi: 10.1016/j.socscimed.2004.02.014. [DOI] [PubMed] [Google Scholar]
- Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethnicity and Disease. 2001;11(3):496–518. [PubMed] [Google Scholar]
- Grol-Prokopczyk H, Freese J, Hauser R. Using anchoring vignettes to assess group differences in general self-rated health. Journal of Health and Social Behavior. 2011;52:246. doi: 10.1177/0022146510396713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E. Self-rated health. In: Capezuti EA, Siegler EL, Mezey MD, editors. The Encyclopedia of Elder Care. 2. Springer Publishing Company; New York, NY: 2008. pp. 711–713. [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kapteyn A, Smith J, Van Soest A. Vignettes and self-reports of work disability in the United States and the Netherlands. The American Economic Review. 2007;97(1):461– 473. [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization composite international diagnostic interview short-form (CIDI-SF) International journal of methods in psychiatric research. 1998;7(4):171–185. [Google Scholar]
- King G, Murray C, Salomon J, JA, Tandon A. Enhancing the validity and cross-cultural comparability of measurement in survey research. American Political Science Review. 2004;98:191–205. [Google Scholar]
- King G, Wand J. Comparing incomparable survey responses: Evaluating and selecting anchoring vignettes. Political Analysis. 2007;15:46– 66. [Google Scholar]
- MacIntosh R, Strickland 0. Differential item responses on CES-D inventory: A comparison of elderly Hispanics and non-Hispanic Whites in the United States and item usage by elderly Hispanics across time. Aging & Mental Health. 2010;14(5):556–564. doi: 10.1080/13607860903421045. [DOI] [PubMed] [Google Scholar]
- Marín G, Sabogal F, Marín BV, Otero-Sabogal R, Pérez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9:183–205. [Google Scholar]
- Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. Journal of Health Care for the Poor and Underserved. 2002;13(4):477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, Pebley A, Sastry N, Yuhas K, Ghosh-Dastidar B, Haas A, Gregory J, Bitler M. Working Paper WR-240/20-LAFANS. RAND Corporation, Labor and Population Program; 2011. Los Angeles Family and Neighborhood Survey Wave 2: User’s guide and codebook. [Google Scholar]
- Phillips LJ, Hammock RL, Blanton JM. Predictors of self-rated health status among Texas residents. Preventing Chronic Disease: Public Health Research, Practice and Policy. 2005;2(4) [PMC free article] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skronda A. Estimating chopit models in gllamm: Political efficacy example from King et al. 2002 Available online at http://www.gllamm.org/chopit.pdf.
- Reed P. Medical outcomes study short form 36: testing and cross-validating a second-order factorial structure for health system employees. Health services research. 1998;33(5 Pt 1):1361. [PMC free article] [PubMed] [Google Scholar]
- Ren XS, Amick BC. Race and self assessed health status: The role of socioeconomic factors in the USA. Journal of Epidemiology and Community Health. 1996;50:269–273. doi: 10.1136/jech.50.3.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values: Further update of ice, with an emphasis on categorical variables. Stata Journal. 2009;9(3):466–477. [Google Scholar]
- Salomon J, Tandon A, Murray CJL. Comparability of self-rated health: Cross sectional multi-country survey using anchoring vignettes. British Medical Journal. 2004 Jan 31;328:258. doi: 10.1136/bmj.37963.691632.44. 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sastry N, Bzostek S, Duffy D, Pebley AR, Goldman N. Studying self-rated health using vignettes: New data and results from the Los Angeles Family and Neighborhood Survey. 2013 Manuscript. [Google Scholar]
- Sastry N, Pebley A. Vignettes for L.A.FANS-2. 2005 Unpublished memorandum. [Google Scholar]
- Sastry N, Ghosh-Dastidar B, Adams J, Pebley A. The design of a multilevel survey of children, families, and communities. The Los Angeles Family and Neighborhood Survey. Social Science Research. 2006;35(4):1000–1024. [Google Scholar]
- Shetterly SM, Baxter J, Mason LD, Hamman RF. Self-rated health among Hispanic vs non-Hispanic white adults: The San Luis Valley Health and Aging Study. American Journal of Public Health. 1996;86(12):1798–1801. doi: 10.2105/ajph.86.12.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer SM, Schulz R, Rooks RN, Albert SM, Thorpe RJ, Jr, et al. Racial differences in self-rated health at similar levels of physical functioning: An examination of health pessimism in the Health, Aging and Body Composition Study. The Journals of Gerontology. 2009;64(1):87–94. doi: 10.1093/geronb/gbn007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. Stata Users Guide, Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- Su D, Wen M, Markides KS. Is self-rated health comparable between non-Hispanic whites and Hispanics? Evidence from the Health and Retirement Study. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2013;68(4):622–632. doi: 10.1093/geronb/gbt037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Morenoff JD, Williams DR, House JS. Language of interview, self-rated health, and the other Latino health puzzle. American Journal of Public Health. 2011;101:1306–1313. doi: 10.2105/AJPH.2009.175455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE., Jr SF-36 health survey update. Spine. 2000;25(24):3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Medical Care. 1995:AS264–AS279. [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36). Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Williams DR. Racial variations in adult health status: Patterns, paradoxes, and prospects. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America becoming: Racial trends and their consequences. Vol. 2. National Research Council, Commission on Behavioral and Social Sciences and Education; Washington, D.C: National Academy Press; 2001. [Google Scholar]
- Zajacova A, Dowd JB. Reliability of self-rated health in US adults. American Journal of Epidemiology. 2011;174(8):977–983. doi: 10.1093/aje/kwr204. [DOI] [PMC free article] [PubMed] [Google Scholar]


