Abstract
Background:
Challenges to ensuring timely linkage to and retention in HIV care are well documented. Combination intervention strategies can be effective in improving the HIV care continuum. Data on feasibility and acceptability of intervention types within intervention packages are limited.
Methods:
The Engage4Health study assessed the effectiveness of a combination intervention strategy to increase linkage and retention among adults newly diagnosed with HIV in Mozambique. The study included 2 health communication interventions—modified delivery of pre-antiretroviral therapy (pre-ART) counseling sessions and SMS reminders—and 3 structural interventions—point-of-care CD4 testing after diagnosis, accelerated ART initiation, and noncash financial incentives. We used a process evaluation framework to assess dose delivered—extent each intervention was delivered as planned—and dose received—participant acceptability—of health communication versus structural interventions in the effectiveness study to understand associated benefits and challenges. Data sources included study records, participant interviews, and clinical data.
Results:
For dose delivered of health communication interventions, 98% of eligible clients received pre-ART counseling and 90% of participants received at least one SMS reminder. For structural interventions, 74% of clients received CD4 testing and 53% of eligible participants initiated ART within 1 month. Challenges for structural interventions included facility-level barriers, staffing limitations, and machine malfunctions. For dose received, participants reported pre-ART counseling and CD4 testing as the most useful interventions for linkage and financial incentives as the least useful for linkage and retention.
Discussion:
Findings demonstrate that health communication interventions can be feasibly and acceptably integrated with structural interventions to create combination intervention strategies.
Key Words: linkage, retention, health communication interventions, Mozambique
INTRODUCTION
Despite significant progress in scaling-up HIV services across sub-Saharan Africa (SSA) over the past decade, attrition across the HIV care continuum continues to contribute to morbidity and mortality among people living with HIV/AIDS (PLWH).1,2 In SSA, between 35% and 88% of adults link to care within 3 months of diagnosis.2,3 Among those who link to care, only two-thirds of eligible individuals ever initiate antiretroviral therapy (ART), and an estimated 65% of those initiating ART are retained in care after 3 years.4 Challenges to timely linkage to and sustained retention in care include: (1) behavioral barriers, such as forgotten appointments and limited understanding of HIV; (2) structural barriers, including insufficient financial resources, limited transportation availability, and time constraints due to work/childcare responsibilities required to make multiple trips to the health facility; and (3) facility-level barriers, including lengthy wait times and poor quality of care.5–9
To achieve the ambitious 2020 UNAIDS 90-90-90 target, pragmatic, evidence-based combination intervention packages targeting the multiplicity of barriers that PLWH face are needed.10–12 These packages may include a variety of intervention types, including health communication interventions targeting individual behavior change, biomedical interventions to improve provision of care, and interventions to reduce structural barriers.13 Although evidence regarding the effectiveness of combination intervention strategies is growing, questions remain regarding implementation and functionality of these interventions.11,13 In particular, the implementation of combination intervention strategies that include health communication interventions to address behavioral determinants of linkage and retention are of increasing interest.14,15
The primary objective of the Engage4Health implementation science study was to evaluate the effectiveness of a combination intervention strategy composed of evidence-based practical interventions in enhancing linkage to and retention in HIV care in Mozambique.16 Beyond providing data on the effectiveness of the combination intervention strategy (which will be presented separately), the study offers an unique opportunity to document and assess “real-world” implementation successes and challenges for a set of interventions targeting linkage to and retention in HIV care. Given the growing interest in identifying feasible and acceptable health communication interventions, this paper presents results from a process evaluation which compares the feasibility and acceptability of health communication versus structural interventions as part of the combination intervention strategy.
METHODS
A brief description of the design and methods used to assess the primary effectiveness objective of the Engage4Health study is provided below as background, followed by a summary of the interventions and a detailed description of the methods used for the process evaluation which is the focus of this paper.
Engage4Health Effectiveness Study
A full description of the Engage4Health study is available elsewhere.16 In brief, the study used a 2-arm cluster site-randomized design to determine the effectiveness of a combination intervention strategy compared with the standard of care in improving linkage and retention among adults after HIV diagnosis. The study was conducted at 10 health facilities in urban Maputo City and rural Inhambane Province. Five health facilities assigned to the intervention arm were provided 2 health communication and 3 structural interventions as described in Table 1 and below. A pre–post intervention 2-sample design was nested within the intervention arm to assess the incremental effectiveness of the combination intervention strategy plus financial incentives (referred to as the “enhanced intervention”) compared with the combination intervention strategy without financial incentives. Participants were recruited immediately after HIV diagnosis during the period of April 2013 to June 2015.
TABLE 1.
Standard of Care Versus Combination Intervention Strategy Interventions
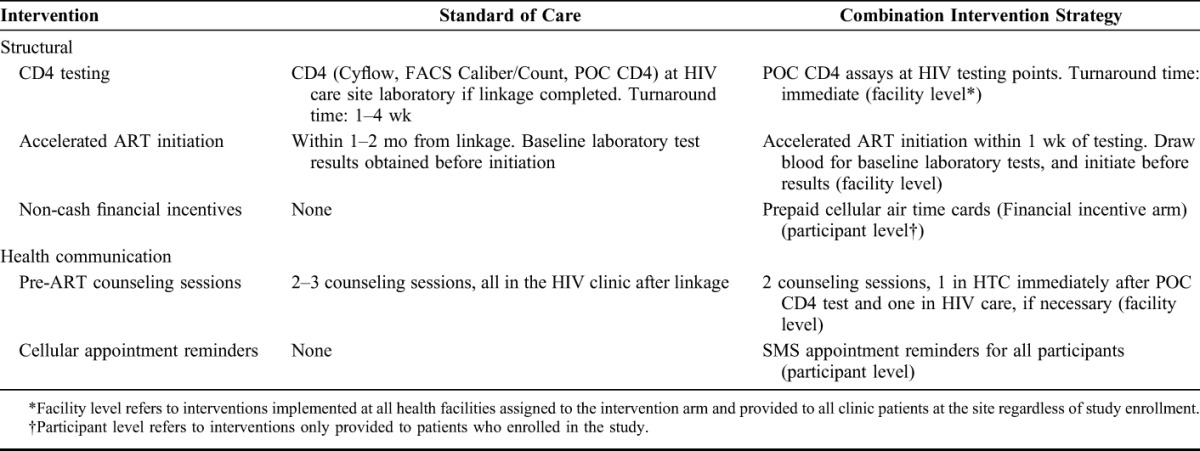
Structural Interventions
Point-of-Care CD4 Count Testing
To facilitate early identification of ART eligible clinic patients, all individuals testing HIV-positive received a point-of-care (POC) CD4 count test immediately after diagnosis in the HIV testing and counseling (HTC) clinic as opposed to the HIV clinic after they linked to care. HTC counselors provided and explained the results to the patient.
Accelerated ART Initiation for Eligible Patients
Accelerated ART initiation was originally conceptualized as a single intervention with 2 components: modified patient flow after diagnosis to fast-track clinical consultation and reduce time to ART initiation (structural), and modified number, timing, and location of pre-ART counseling sessions (health communication). To facilitate comparison of intervention types in this paper, this intervention is addressed separately as 2 interventions. With regards to fast-tracking ART initiation, clinic patients with POC CD4 counts ≤350 cells per microliter were escorted to the receptionist's office for immediate enrollment in HIV care and expedited scheduling of the first clinical consultation. Health care workers were trained and instructed to initiate ART eligible patients as soon as possible, without waiting for laboratory results, ideally within 1 week of diagnosis. The pre-ART counseling component is described under health communication interventions.
Noncash Financial Incentives
Study participants in the enhanced intervention arm were eligible to receive up to 3 noncash financial incentives in the form of prepaid air-time cards worth $5 USD each if they reached prespecified linkage and retention milestones. Milestones included linkage to care, defined as having a clinical consultation within 1 month of diagnosis, and retention in care 6 and 12 months after diagnosis. Study participants who did not have phones could opt to sell or trade the cards.
Health Communication Interventions
Modified Pre-ART Counseling for Eligible Patients
Immediately after POC CD4 count testing, HTC counselors provided the first pre-ART counseling session to ART-eligible clinic patients in the HTC clinic before linkage to care rather than in the HIV clinic after linkage to care. This modification to the timing and location of pre-ART counseling sessions meant that individuals eligible to initiate ART immediately received information on ART initiation and had more time to discuss HIV diagnosis, linkage to care, and ART initiation than they would with basic posttest counseling. Providing this information before linkage to care was designed to reduce behavioral barriers, such as lack of knowledge or fear of HIV care and ART initiation, and encourage accelerated linkage and ART initiation.
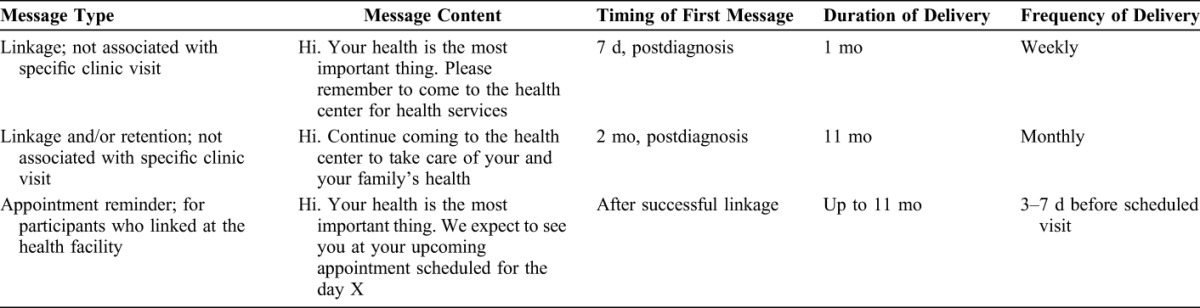
Cellular Appointment Reminders
SMS text messages with health promotion and appointment reminder messages designed to encourage linkage into HIV care were sent to all study participants who provided a telephone number. The message content, timing, and frequency are outlined in Table 2. Study participants received weekly reminders to encourage linkage during the first 4 weeks after diagnosis and then monthly reminders to encourage linkage to and/or retention in care for the remaining 11 months of the study. Participants who successfully linked to care received appointment reminders 3–7 days before scheduled clinic visits. As phone sharing is common in resource-limited settings, to protect patient confidentiality, none of the messages mentioned HIV, AIDS, or the name of the health facility.
TABLE 2.
Description of Cellular Appointment Reminders Sent to Study Participants
Process Evaluation Study Design
A summative process evaluation was developed using the Steckler and Linnan framework and the Saunders, Evans, and Joshi framework as guides.17,18 The process evaluation components, evaluation questions, and data sources are shown in Table 3. Data were identified and abstracted from pre-existing sources as described below. For most data sources, data are presented on the 1237 adult study participants enrolled at the 5 facilities assigned to provide the intervention: 744 from the intervention arm (490 female and 254 male) and 493 from the enhanced intervention arm who additionally received financial incentives (319 female and 174 male). However, in the case of the study reports, data for some indicators were available on the entire clinic population of study participants and nonparticipants. As 3 of the interventions were implemented at the facility-level, where available, data on the entire clinic population are included as they allow for a more complete analysis of whether the interventions were implemented as planned.
TABLE 3.
Process Evaluation Components, Evaluation Questions, and Data Sources
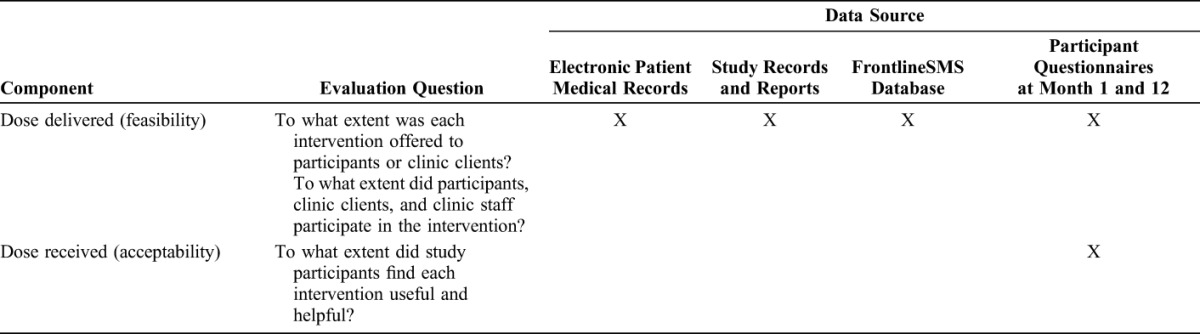
Routinely Collected Clinical Data
As part of routine clinical care at each health facility, providers recorded baseline and follow-up data for clinic patients enrolled in HIV care on structured clinical encounter forms and data clerks enter these data into an electronic medical record system. For this evaluation, we extracted the following data elements: date of initial and follow-up CD4 counts; CD4 test results; and dates associated with enrollment in care, pre-ART counseling sessions, ART initiation, and follow-up clinical consultations.
Study Reports
In-country study staff compiled monthly reports documenting progress implementing the study and interventions, including challenges that arose. Of relevance to the process evaluation, these reports contained indicators to track delivery of each intervention, including the proportion of all newly HIV diagnosed adults (study participants and nonparticipants) who received a POC CD4 count test, the proportion of ART-eligible individuals who received a pre-ART counseling session immediately after diagnosis (study participants and non-participants), and the proportion of eligible study participants who received the financial incentives.
Participant Questionnaires
As part of the effectiveness study, study participants completed closed-ended interviews 1 and 12 months after diagnosis. Data on the acceptability of each intervention was abstracted from the questionnaires for the process evaluation. Participants were asked to rank the relative usefulness of each of the interventions for linkage to and retention in care.
FrontlineSMS Database
SMS messages were sent to study participants using a Frontline database (Occam Technologies, Inc., Washington, DC). Records of message delivery were extracted from the database for this process evaluation.
Ethics
The Engage4Health study and delivery of all interventions were approved by the Institutional Review Board at Columbia University and by Mozambique's National Committee for Bioethics in Health. Participants provided written informed consent before study enrollment.
RESULTS
Dose Delivered
Table 4 summarizes data on dose delivered by intervention type.
TABLE 4.
Dose Delivered of Study Interventions
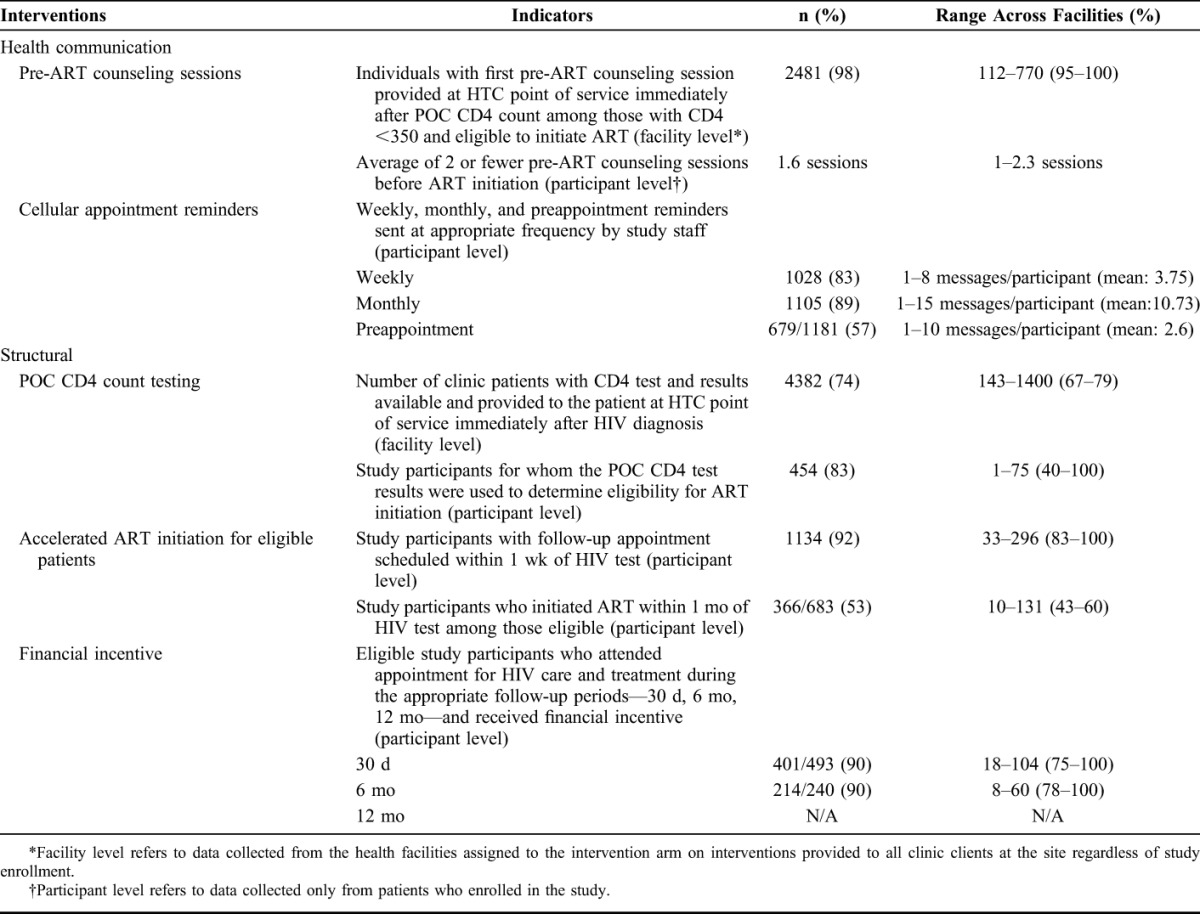
Structural Interventions
POC CD4 Test
Over the 3-year study period, 74% of all clinic patients newly diagnosed with HIV received same-day POC CD4 test in the HTC clinic (range across facilities: 67%–79%) with no meaningful difference over time (range across years: 73%–76%). Barriers to complete provision of POC CD4 tests included machine malfunctions and facility power outages ranging from 1 day to over a month; staff shortages due to absenteeism, vacations, and persistent understaffing ranging from 1 day of absenteeism to multiple months of understaffing; and engagement of temporary or new staff in the HTC clinic who did not know how to operate the machine. Overall, 83% of study participants (range across facilities: 55%–100%) who initiated ART did so without a subsequent CD4 test before initiation, a 10% increase from the first year of implementation. Clinician-reported reasons for ordering additional CD4 tests before prescribing ART included mistrust in the POC CD4 result and lack of knowledge of the guidelines to initiate ART on the basis of POC CD4 test results.
Accelerated ART Initiation
Of the 683 clinic patients found to be ART eligible on the basis of the POC CD4 test, 53% initiated ART within a month of diagnosis (range across facilities: 43%–60%), with a median time to initiation of 17.5 days (interquartile range: 7–35). The challenges to ensuring accelerated ART initiation included resistance from receptionists to opening patient files, high patient volume causing a backlog of clinical appointments, and clinician reluctance to prescribe ART before receipt of lab results (eg, hemoglobin and chemistries) or additional pre-ART counseling.
Financial Incentives
Among the 493 study participants in the enhanced intervention arm, 445 (90%) linked to care within 30 days of diagnosis and were eligible to receive the first financial incentive; of these, 401 (90%) actually received it (range across facilities: 75%–100%). A total of 240 (49%) of the 493 study participants in the enhanced intervention arm were eligible to receive the second financial incentive for a follow-up clinic visit 6 months after diagnosis, and 215 (90%) actually received it (range across facilities: 78%–100%). Complete disbursement of the incentives to eligible participants was hindered by confusion regarding how to collect the incentive, limited time to complete the procedures for collection, and errors by the study staff in determining participant eligibility. Data collection of financial incentives for 12 months retention is ongoing and not reported here.
Health Communication Interventions
Pre-ART Counseling
Routinely collected monitoring data from study reports indicated that 98% of all HTC clients at the facility who received a POC CD4 test and were determined to be ART eligible received same day pre-ART counseling in the HTC clinic (range across facilities: 95%–100%). Limited availability of counselors was the primary barrier to delivery of this intervention. Clinicians were oriented to initiate patients after same-day pre-ART counseling unless there was a specific need for additional sessions. Among study participants who linked to care, those eligible to initiate ART at enrollment received an average of 1.6 counseling sessions (range across facilities: 1–2.3). Dose delivered of pre-ART counseling intervention implementation improved over time, with a reduction from an average of 2.3 counseling session in year 1 to 1.3 sessions in year 3.
SMS Reminders
At enrollment, 92% of study participants in the intervention arm reported having access to a cell phone and provided a contact number to study staff (urban: 96%, rural: 87%). Ultimately, 90% of study participants received at least one SMS message. Eighty-three percent (range across facilities: 78%–88%) received at least 1 weekly reminder to link to care and 89% (range across facilities: 83%–95%) received at least 1 monthly reminder to link to or remain in care. Seventy-eight percent received all 4 weekly messages (mean = 3.8 messages/participant). Sixty-eight percent received all 11 monthly messages (mean = 10.7 messages/participant). Of the 1181 study participants who linked to care in the 12 months after diagnosis, 57% received an appointment reminder (range: 1–10, mean: 2.6). Documented barriers included delays in entering appointment dates in the electronic patient medical record, inability to program the SMS platform to automatically deliver messages, and loss of data on message delivery during a platform upgrade.
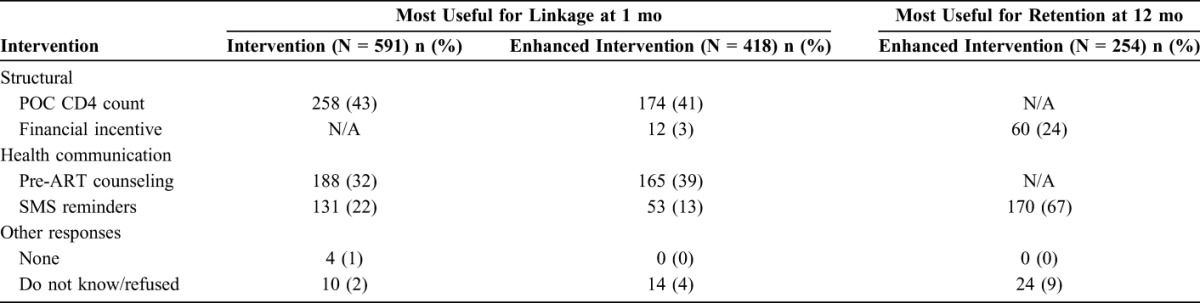
Dose Received
Participant perceptions of the usefulness of the interventions for linkage to care did not differ by intervention type (Table 5). Study participants who linked to care before their 1 month follow-up interview (n = 1009) ranked POC CD4 count testing (intervention arm: 43%; enhanced intervention arm: 41%) and same day pre-ART counseling (intervention arm: 32%; enhanced intervention arm: 39%) as the most useful interventions in facilitating linkage to care. In comparison, fewer study participants ranked the SMS message reminders as the most useful for timely linkage to care (intervention arm: 22%; enhanced intervention arm: 13%), and 3% of enhanced intervention participants cited the financial incentive as the most useful intervention. It was not possible to assess perceptions of accelerated ART initiation in facilitating linkage as it was originally conceived as a single intervention in conjunction with pre-ART counseling. Assessments of the most useful intervention for retention was limited to 254 study participants in the enhanced intervention arm who were retained in care 12 months after diagnosis, and thus had the opportunity to receive both the SMS reminders and financial incentives. Of those participants, 67% reported that the SMS reminders was the most useful intervention in facilitating retention and 24% reported that the financial incentive was the most useful intervention.
TABLE 5.
Study Participant Rankings of the “Most” Useful Intervention in Supporting Timely Linkage to and Retention in HIV Care
DISCUSSION
Using a process evaluation framework, we assessed dose delivered and dose received for structural versus health communication interventions implemented as part of a combination intervention strategy which aimed to increase linkage and retention after HIV diagnosis. Overall, dose delivered of the health communications interventions was higher than dose delivered of the structural interventions. There were also fewer documented barriers to delivery of the health communication interventions as compared with the structural interventions. Furthermore, dose delivered of the health communication interventions improved over time, whereas dose delivered of the structural interventions remained relatively constant. In assessing dose received, our evaluation highlighted the overall acceptability of both intervention types for supporting linkage to care. However, for retention in care, there was higher acceptability of the health communication intervention (SMS reminders) than of the structural intervention (financial incentives).
Our findings on dose delivered for structural versus health communication interventions highlight real-world implementation of evidence-based interventions.19 Though the successes of interventions are often well-documented, the challenges to implementation are not as well understood.20 Our results provide further insight into the barriers that are unique to each intervention type, and identify the reasons for additional challenges to implementing structural versus health communications interventions. Structural interventions consisting of POC CD4 testing and accelerated ART initiation required significant additional training of health care workers, acceptance and coordination between health care workers to implement the new patient flow, and task-shifting of CD4 testing to HTC staff. Despite substantial pre-study and refresher trainings of facility staff on intervention procedures, challenges to implementing these interventions remained throughout the 3-year study period. In particular, health facilities were overburdened and struggled to absorb the increased number of patients eligible for ART initiation in a timely manner after implementation of the interventions.
In contrast, modified pre-ART counseling, a health communication intervention, relied primarily on counselors accepting to modify the location and timing of service delivery. Though all 3 interventions were implemented at the facility level, there were far fewer barriers to implementation of this intervention, as counselors were already trained and providing pre-ART counseling. The potential reduction in workload, as clients did not have to return for multiple pre-ART counseling sessions after linkage, may have also facilitated counselor acceptance and delivery of this intervention. The reduction in number of pre-ART counseling sessions per patient over time also reflects increased clinician acceptance of the intervention.
The SMS reminders and financial incentives were provided to study participants over a 12-month period after diagnosis to encourage timely linkage and sustained retention in care. Dose delivered and dose received of the SMS reminders as compared with the financial incentives draw attention to additional differences between health communication versus structural interventions delivered over time. The barriers to delivery of the SMS reminders were primarily related to the use of the FrontlineSMS platform and were addressed early on in study implementation. As a result, dose delivered for appointment reminders increased significantly over time. Dose received results followed a similar trajectory. Perceptions of the utility of the SMS reminders for linkage were relatively low compared with the pre-ART counseling and POC CD4 testing interventions, possibly due to initial challenges in message delivery. However, the number of study participants reporting positive perceptions of the SMS reminders for retention in care as compared with linkage was significantly higher. Of note, this intervention was implemented by study staff, and integration into routine service delivery at health facilities would be important for scale-up. Other studies have reported on successful implementation of SMS systems in clinical settings in SSA, but highlight context-specific challenges that can reduce effectiveness of SMS systems, including low literacy.21–23
With regards to financial incentives, the process evaluation revealed unexpected challenges for both dose delivered and dose received. For dose delivered, although 80% of enhanced intervention participants were eligible for and received the first incentive for linkage to care, only 40% were eligible for and received the second incentive for retention in care at 6 months. This suggests that even after receiving the first incentive, approximately half of study participants did not return for a follow-up clinical visit to receive the second incentive. For dose received, only 3% of the enhanced intervention participants reported the financial incentive as the most useful intervention in facilitating linkage to care. Additionally, when compared with high rankings of the SMS reminders for supporting retention, participant endorsement of the utility of the financial incentives intervention was surprisingly low. These findings suggest the need for additional evaluation of incentive types and delivery methods that would be more acceptable to PLWH, such as tiered incentives which provide greater rewards over time.24
The comparison of feasibility and acceptability of 2 intervention types, each composed of several interventions, is an important strength of this process evaluation. Although evaluations of individual interventions are common, as combination intervention strategies gain momentum, there is a pressing need for information on implementation challenges of different types of interventions.25 Use of multiple, complementary data sources, including study records, participant interviews, and routinely collected clinical data further strengthened this evaluation. Additionally, we examined the feasibility and acceptability of interventions delivered in real-world settings, which provide important insights for governments, implementing partners, and donors who may consider implementing these same interventions. Several limitations should also be noted, however. Comparison of health communication versus structural interventions was not an original objective of the Engage4Health study. Therefore, data to tease out acceptability of accelerated ART initiation from the pre-ART counseling intervention were limited. For dose delivered, much of the data were extracted from electronic patient medical records which are of variable quality due to backlogs and errors in data entry.
CONCLUSIONS
As evidence on the effectiveness of combination intervention strategies targeting outcomes across the HIV care continuum grows, documenting and understanding implementation challenges of the disparate intervention types embedded within those strategies is critical. To our knowledge, this is the first evaluation to compare the feasibility and acceptability of structural versus health communication interventions. Our findings demonstrate unique challenges of each intervention type. They also highlight lessons learned for feasible and acceptable implementation of both intervention types as part of a combination intervention strategy to reduce structural and behavioral barriers to linkage and retention. Critically, these findings demonstrate the particular successes of implementing health communication interventions within combination intervention strategies. Additional evaluations of health communication interventions implemented within intervention packages are critical to expanding this evidence-base.
ACKNOWLEDGMENTS
The authors thank the Mozambican Ministry of Health, health facility staff and study team for their support and contribution to the study. The authors are also grateful to the study participants included in this study.
Footnotes
This study is funded by the United States Agency for International Development (USAID), USAID Award Number: AID-OAA-A-12-00022. USAID is the donor and advisory institution for this study. They are not directly engaged with the study. USAID employees consequently have no contact with study participants and no access to individually identifiable private information.
The authors have no funding or conflicts of interest to disclose.
Trial registration: Clinicaltrials.gov, NCT01930084.
REFERENCES
- 1.Fox MP, Rosen S. Patient retention in antiretroviral therapy programs up to three years on treatment in sub-Saharan Africa, 2007-2009: systematic review. Trop Med Int Health. 2010;15(suppl 1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosen S, Fox MP. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. PLoS Med. 2011;8:e1001056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Micek MA, Gimbel-Sherr K, Baptista AJ, et al. Loss to follow-up of adults in public HIV care systems in central Mozambique: identifying obstacles to treatment. J Acquir Immune Defic Syndr. 2009;52:397–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kranzer K, Govindasamy D, Ford N, et al. Quantifying and addressing losses along the continuum of care for people living with HIV infection in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2012;15:17383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geng EH, Bangsberg DR, Musinguzi N, et al. Understanding reasons for and outcomes of patients lost to follow-up in antiretroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic Syndr. 2010;53:405–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS. 2012;26:2059–2067. [DOI] [PubMed] [Google Scholar]
- 7.Lahuerta M, Ue F, Hoffman S, et al. The problem of late ART initiation in sub-Saharan Africa: a transient aspect of scale-up or a long-term phenomenon? J Health Care Poor Underserved. 2013;24:359–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maskew M, MacPhail P, Menezes C, et al. Lost to follow up: contributing factors and challenges in South African patients on antiretroviral therapy. S Afr Med J. 2007;97:853–857. [PubMed] [Google Scholar]
- 9.Posse M, Bultussen R. Barriers to access to antiretroviral treatment in Mozambique, as perceived by patients and health workers in urban and rural settings. AIDS Patient Care STDS. 2009;23:867–875. [DOI] [PubMed] [Google Scholar]
- 10.Holmes CB, Sanne I. Changing models of care to improve progression through the HIV treatment cascade in different populations. Curr Opin HIV AIDS. 2015;10:447–450. [DOI] [PubMed] [Google Scholar]
- 11.McNairy ML, El-Sadr WM. Antiretroviral therapy for the prevention of HIV transmission: what will it take? Clin Infect Dis. 2014;58:1003–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joint United Nations Programme on HIV/AIDS. 90-90-90: An Ambitious Treatment Target to Help End the AIDS Epidemic. Geneva, Switzerland: UNAIDS; 2014. [Google Scholar]
- 13.Barnighausen T, Chaiyachati K, Chimbindi N, et al. Interventions to increase antiretroviral adherence in sub-Saharan Africa: a systematic review of evaluation studies. Lancet Infect Dis. 2011;11:942–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomori C, Risher K, Limaye RJ, et al. A role for health communication in the continuum of HIV care, treatment, and prevention. J Acquir Immune Defic Syndr. 2014;66(suppl 3):S306–S310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vermund SH, Van Lith LM, Holtgrave D. Strategic roles for health communication in combination HIV prevention and care programs. J Acquir Immune Defic Syndr. 2014;66(suppl 3):S237–S240. [DOI] [PubMed] [Google Scholar]
- 16.Elul B, Lahuerta M, Abacassamo F, et al. A combination strategy for enhancing linkage to and retention in HIV care among adults newly diagnosed with HIV in Mozambique: study protocol for a site-randomized implementation science study. BMC Infect Dis. 2014;14:549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saunders R, Evans MH, Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: a how-to guide. Health Promot Pract. 2005;6:134–147. [DOI] [PubMed] [Google Scholar]
- 18.Steckler A, Linnan L. Process Evaluations for Public Health Intervention and Research. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- 19.Chang LW, Serwadda D, Quinn TC, et al. Combination implementation for HIV prevention: moving from clinical trial evidence to population-level effects. Lancet Infect Dis. 2013;13:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vojnov L, Markby J, Boeke C, et al. POC CD4 testing improves linkage to HIV care and timeliness of ART initiation in a public health approach: a systematic review and meta-analysis. PLoS One. 2016;11:e0155256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Georgette N, Siedner MJ, Zanoni B, et al. The acceptability and perceived usefulness of a weekly clinical SMS program to promote HIV antiretroviral medication adherence in KwaZulu-Natal, South Africa. AIDS Behav. 2016;20:2629–2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bigna JJ, Noubiap JJ, Plottel CS, et al. Barriers to the implementation of mobile phone reminders in pediatric HIV care: a pre-trial analysis of the Cameroonian MORE CARE study. BMC Health Serv Res. 2014;14:523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bassett IV, Wilson D, Taaffe J, et al. Financial incentives to improve progression through the HIV treatment cascade. Curr Opin HIV AIDS. 2015;10:451–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Govindasamy D, Meghij J, Negussi EK, et al. Interventions to improve or facilitate linkage to or retention in pre-ART (HIV) care and initiation of ART in low- and middle-income settings–a systematic review. J Int AIDS Soc. 2014;17:19032. [DOI] [PMC free article] [PubMed] [Google Scholar]


