Abstract
Different suture techniques have been used for anastomosis in coronary artery bypass graft surgery. Bypass surgery may be difficult for patients who have small coronary arteries or marked size discrepancies between target coronary arteries and grafts. For proximal and distal anastomoses, three continuous stitches are first placed in the heel and toe of the small coronary arteries; for sequential anastomosis, an interrupted eight-stitch technique is used. We applied these anastomotic suture techniques in patients requiring coronary artery bypass graft surgery, achieving an early angiographic patency rate of 100%.
Keywords: Coronary artery bypass, Suture techniques, Anastomosis
Introduction
For anastomoses to target coronary arteries during coronary artery bypass graft (CABG) surgery, different continuous suture techniques have been used [1,2]. A competent anastomotic technique can achieve satisfactory antegrade and retrograde arterial patency in the anastomotic sites of the target coronary arteries and grafts. Here, we introduce a simple technique for obtaining satisfactory anastomosis of coronary arteries and grafts in patients who have small coronary arteries (<1.2 mm) or marked size discrepancies between the target coronary arteries and grafts.
Technique
1) Distal anastomosis of a graft to a target coronary artery
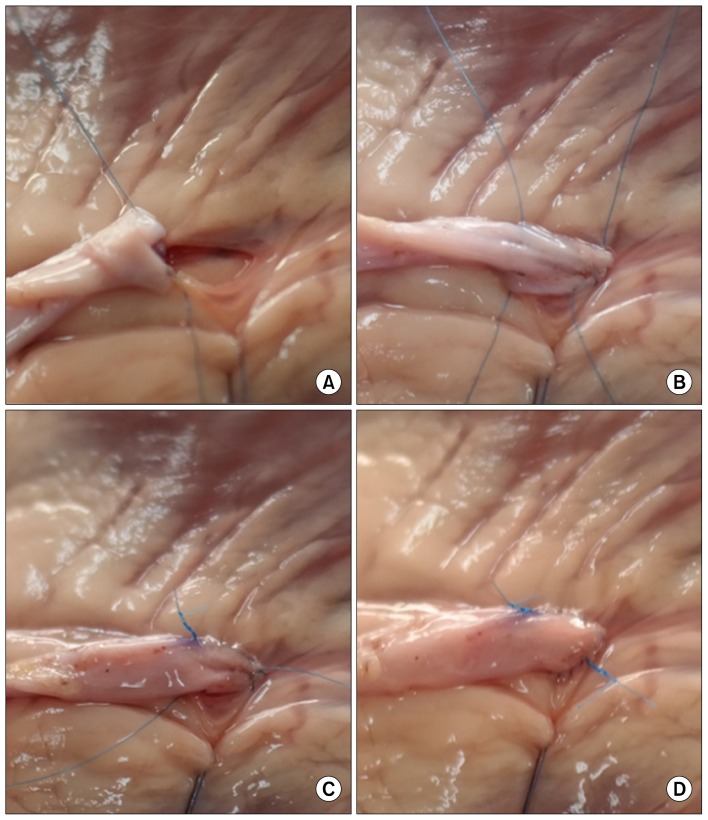
For distal anastomosis of the graft to the coronary artery, we used a continuous suture technique with two suture materials. For this method, the graft is anchored to the proximal and distal ends of the coronary arteriotomy with three stitches on each end using two 7-0 or 8-0 polypropylene monofilaments. The length of the coronary arteriotomy should be 20% shorter than the beveled length of the graft, thus leaving a hood. In detail, the first three-stitch continuous suture is placed counterclockwise at the heel of the graft and at the proximal end of the coronary arteriotomy. After the graft is anchored, two ends of the suture are grasped with two silicone-shod clamps (Fig. 1A). Next, with the second suture material, the toe of the graft is anchored to the distal end of the coronary arteriotomy, again using the same technique (continuous counterclockwise stitches) (Fig. 1B). The second suture is continued counterclockwise toward the starting point of the first heel suture and tied (Fig. 1C). At this time, three lumens of the anastomosed graft and the proximal and distal ends of the coronary arteriotomy may be carefully checked with a 1-mm flexible probe. The opposite suture line is completed counterclockwise with the other arm of the first heel suture (Fig. 1D).
Fig. 1.
Distal anastomosis of graft to target coronary artery. (A, B) Heel and toe of the coronary artery and graft are anchored by continuous three-stitch technique for each side, and (C, D) the remaining suture lines are completed in counterclockwise direction.
2) Sequential anastomosis of the graft to the coronary arteries
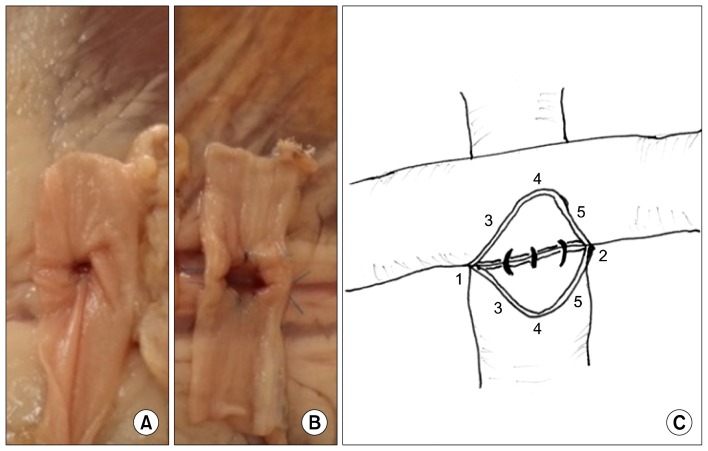
For sequential graft anastomoses to coronary arteries, the arteriotomy length is approximately 1.5 times the arterial diameter and the graft incision should be 20% longer than the arteriotomy. Rather than a continuous technique, the interrupted eight-stitch technique in a diamond configuration is used to avoid the purse-string effect (Fig. 2A) and obtain a sufficient anastomotic opening (Fig. 2B) [3]. In detail, three interrupted sutures using 7-0 or 8-0 polypropylene monofilament are first placed in the proximal side of the coronary arteriotomy, through the graft, and then tied into place. The remaining five interrupted sutures are then placed at even intervals and tied (Fig. 2C). This method can result in a large anastomotic opening associated with satisfactory hemostasis (Fig. 2B).
Fig. 2.
Sequential anastomosis using (A) continuous and (B) interrupted eight-stitch techniques. (A) The continuous suture technique causes a marked purse-string effect. (B) The interrupted suture technique forms a round sufficient anastomotic opening. (C) For interrupted eight-suture technique, three interrupted sutures are placed and tied in the heel side of the coronary arteriotomy and the graft, with the remaining five sutures placed in even spaces.
3) Proximal anastomosis of the graft to the aortic opening
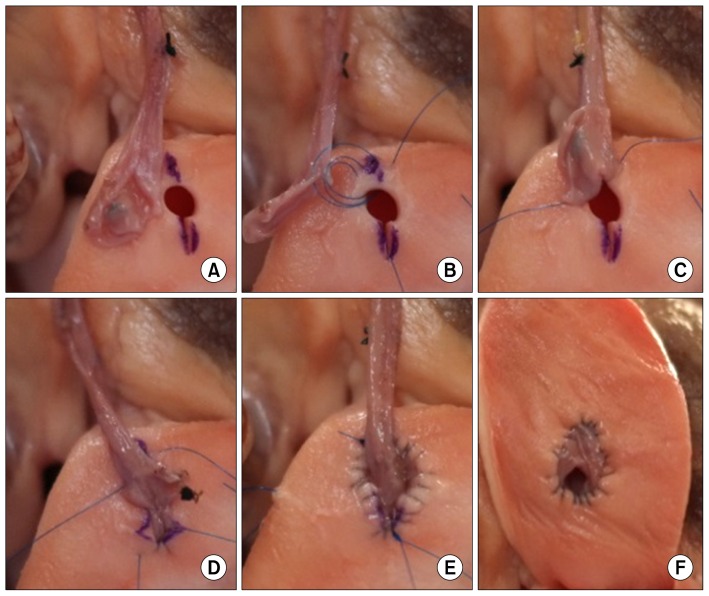
For this method, an aortic incision <1 cm for proximal anastomosis is made with a small (e.g., no. 15) blade in an appropriate direction, and the distal end of the aortic incision is enlarged with a 3.5-mm aortic punch (Fig. 3A). The long-axis of the graft opening should be 1.2 to 1.3 times the aortic incision. The suture technique is the same as the two-suture material technique described above for distal anastomosis. First, the heel of the graft is anchored at the distal end (punch opening) of the aortic incision by three continuous stitches (clockwise in images shown in Figs. 3B, C), and the toe of the graft is anchored at the other end of the aortic incision by three continuous clockwise stitches using a second suture material (Fig. 3D). The remaining continuous stitches should be made in one direction, either clockwise or counterclockwise ( Fig. 3 E). When the stitches are tightened, all graft margins inside the stitches should be inverted into the aortic opening to achieve appropriate hemostasis and a smooth internal lumen (Fig. 3F).
Fig. 3.
Proximal anastomosis of a graft to an aortic opening. (A) After aortic incision, a small punch opening (3.5 mm) is made in the distal aortic incision, (B, C) where the heel of the vein graft is first anchored to the aortic opening by continuous clockwise three-stitch technique. (D–F) The remaining sutures are made as shown in Fig. 1 for distal anastomosis.
Discussion
Most anastomotic techniques for CABG surgery are continuous sutures using polypropylene monofilaments. For bypass grafting to small coronary arteries, it may be difficult to achieve patency with continuous sutures in anastomotic sites of the target coronary artery and graft. Three stitches anchoring the graft at each end of the coronary arteriotomy can guarantee patency of the proximal and distal coronary arterial lumens. Additionally, all stitches are performed in-outward in coronary arteries and out-inward on grafts. Anchoring both ends of the graft at the arteriotomy can reduce instrument manipulation to the graft during suturing and produce a concise anastomotic line with even spaces. This suture technique can also be used in proximal anastomosis of the graft to aortic opening with the same advantages. With sequential anastomosis, a continuous suture technique in diamond configuration can cause a purse-string effect, leading to a small anastomotic opening. An alternative interrupted eight-stitch technique [3] is not more time-consuming than the continuous technique or the four-stitch technique [4]. For proximal anastomosis of the graft to aortic opening, a round, wide aortic opening made with a 4.5 to 5.0-mm punch may cause a stretched graft in the aortic opening after anastomosis. A small punch opening (3.5-mm) in the distal end of the aortic incision produces a more concise graft hood.
The suture techniques described here are not only useful in small target coronary arteries but also a reliable teaching technique of CABG surgery to inexperienced cardiac surgeons. We have now used this technique for 1 year in approximately 40 patients with variable-sized coronary arteries and who require on-pump CABG surgery and confirmed 100% graft patency on postoperative computed tomography angiograms. Additional study about the suture technique in off-pump CABG surgery is necessary.
Footnotes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Greason KL, Sundt TM., III . Myocardial revascularization with cardiopulmonary bypass. In: Cohn LH, editor. Cardiac surgery in the adult. 4th ed. New York (NY): McGraw-Hill; 2012. pp. 479–503. [Google Scholar]
- 2.Kouchoukos NT, Blackstone EH, Hanley FL, Kirklin JK. Kirklin/Barrat-Boyes cardiac surgery: stenotic arteriosclerotic coronary artery disease. 4th ed. Philadelphia (PA): Elsevier Saunders; 2013. pp. 353–428. [Google Scholar]
- 3.Lytle BW. Anastomotic techniques. Oper Tech Thorac Cardiovasc Surg. 2000;5:222–30. doi: 10.1053/2000.otct.18708. [DOI] [Google Scholar]
- 4.Kawahito K, Muraoka A, Misawa Y. Side-to-side anastomosis using 4 interrupted sutures in small coronary arteries. Asian Cardiovasc Thorac Ann. 2014;22:115–7. doi: 10.1177/0218492313485373. [DOI] [PubMed] [Google Scholar]