Abstract
Introduction
People living with HIV (PLWH) need to adhere to antiretroviral therapy (ART) to achieve optimal health. One reason for ART non-adherence is HIV-related stigma.
Objectives
We aimed to examine whether HIV treatment self-efficacy (an intrapersonal mechanism) mediates the stigma – adherence association. We also examined whether self-efficacy and the concern about being seen while taking HIV medication (an interpersonal mechanism) are parallel mediators independent of each other.
Methods
180 PLWH self-reported internalized HIV stigma, ART adherence, HIV treatment self-efficacy, and concerns about being seen while taking HIV medication. We calculated bias-corrected 95% confidence intervals (CIs) for indirect effects using bootstrapping to conduct mediation analyses.
Results
Adherence self-efficacy mediated the relationship between internalized stigma and ART adherence. Additionally, self-efficacy and concern about being seen while taking HIV medication uniquely mediated and explained almost all of the stigma – adherence association in independent paths (parallel mediation).
Conclusion
These results can inform intervention strategies to promote ART adherence.
Keywords: HIV stigma, ART adherence, mediators
INTRODUCTION
For people living with HIV (PLWH) adherence to antiretroviral therapy (ART) is crucial in order to achieve desired treatment outcomes. One reason for non-adherence is HIV-related stigma1–6, which encompasses experiences of prejudice, discrimination, or other negative attitudes due to one’s HIV diagnosis7–10. Some PLWH internalize stigma, accepting negative evaluations about having HIV as valid6,7,11,12. Internalized stigma often predicts sub-optimal ART adherence6,7,12.
How does internalized HIV-related stigma lead to ART non-adherence? The limited literature on mediating mechanisms explaining this association identified intrapersonal mechanisms such as depression8,12,13, as well as interpersonal mechanisms such as attachment-related anxiety and loneliness7 as potential mediators.
An interpersonal mechanism associated with HIV-related stigma is the concern about being seen by others while taking HIV medication7. HIV treatment is a challenging process, involving the need to take medication the same time each day and sometimes during inconvenient situations or in public settings. Thus, PLWH with such concerns may skip taking their medications in certain situations2. This concern has been reported as a mediating variable in the association between internalized stigma and medication non-adherence7.
An intrapersonal mechanism that has gained attention in relation to ART adherence is treatment adherence self-efficacy14,15. Self-efficacy is an individual’s confidence in his or herself to carry out a certain behavior or complete a task16. HIV treatment self-efficacy refers to one’s confidence in his or her ability to adhere to a treatment plan despite obstacles14. While adherence self-efficacy has been shown to predict optimal ART adherence14,15,17,18, only one study, to our knowledge, has found an inverse association between internalized HIV stigma and adherence self-efficacy19.
Only one study examined adherence self-efficacy as a mediator in the stigma–adherence association20. However, the self-efficacy measure in that study asked participants questions that are usually used when assessing adherence, such as “I can always follow my HIV medication schedule,” which may have inflated the association between self-efficacy and adherence. Additionally, experienced stigma rather than internalized stigma was assessed, and according to recent theoretical approaches and empirical data, internalized stigma is a better unique predictor of adherence, since stigma may have to be internalized in order to affect a person’s behavior6,21,22.
Here we examined whether adherence self-efficacy is associated with a widely used measure of internalized stigma and mediates the association between internalized stigma and adherence. Given that previous research has found both interpersonal and intrapersonal mechanisms to be involved in the association between internalized stigma and medication adherence, we also aimed to examine the independent unique mediating roles (i.e., parallel mediation) of concern about being seen taking HIV medication (an interpersonal mechanism) and adherence self-efficacy (an intrapersonal mechanism) in the stigma—adherence association, where both mechanisms were entered as mediators simultaneously. Examining simultaneous parallel mediation effects is important since it may be the case that two variables are significant mediators in two separate mediation analyses, but when entered simultaneously, one (or both) may fail to be a significant unique mediator (above and beyond the other mediating path) due to overlap in the mediation effects23–25. Ajzen and Fishbein26 provided support for their hypothesis that interpersonal and intrapersonal factors contribute independently to the prediction of behavior (also see27 for a dual-pathway theory of interpersonal and intrapersonal mechanisms in the association between poverty stigma and depression). Using simultaneous entry, one can also compare the two specific indirect effects to see if the mediating effect of one is stronger than the other.
We used the same sample (and the data on adherence, stigma, and concern about being seen taking HIV medication) used in our previously reported work7 on the mediating role of concern about being seen taking HIV medication in the stigma—adherence association. The current analyses take this program of research a step further by investigating the mediating effect of self-efficacy, as well as by examining simultaneous roles of these interpersonal and intrapersonal mechanisms in the relationship between stigma and medication adherence in an attempt to tease apart the independent mediating roles of these variables. This, in turn, may allow us to better understand the complex factors affecting treatment outcomes for PLWH, with the goal of developing more effective ART adherence interventions.
METHODS
Participants and Procedures
Patients from an HIV clinic in Birmingham, AL gave written informed consent to participate in this IRB approved study between March 2013 and January 2015. Exclusion criteria included not being prescribed ART and/or being a current substance user. In the present analyses, 180 participants with data on the primary study variables were included. Time on ART and daily frequency of prescribed HIV medications (single pill once daily versus more complex regimens) was extracted from medical records. Participants self-reported their socio-economic status (SES).
Measures
Medication Adherence was assessed using a single-item where participants reported their ability to take all HIV medication prescribed using a 6-point rating scale ranging from 1 (very poor) to 6 (excellent). Literature suggests this is a valid adherence measure associated with viral suppression28,29. The scores were not normally distributed: 128 participants reported excellent adherence and 52 participants reported less than excellent adherence; therefore, this measure was dichotomized: Excellent adherence (1) or less than excellent adherence (0).
Internalized stigma was assessed using the 7-item Negative Self-Image subscale of the HIV Stigma Scale11,30. A sample item is: “Having HIV in my body is disgusting to me.” Participants rated items using a Likert-type scale ranging from (strongly disagree to strongly agree (Cronbach’s α=.85 in this study).
Concern about being seen by others while taking HIV medication: Two items from two separate measures were used. Item 1: “I don’t want people to see me take my HIV medicines” (rated using a Likert-type scale from 1 to 5) was taken from the Patient Medication Adherence Questionnaire Version 1.0 (PMAQ-V1.0)31, and Item 2: “Did not want others to notice you taking medication” (rated using a Likert-type scale from 1 to 4) was taken from the Adult AIDS Clinical Trial Group Adherence to Combination Therapy (AACTG) Questionnaire32. After standardizing, the mean of the responses to both items was used in analyses.
Adherence self-efficacy: The HIV Treatment Adherence Self-Efficacy Scale14 consists of 12 items with the stem: “How confident do you feel that you can do these things related to HIV?” Participants used a rating scale ranging from 1 (cannot do it all) to 10 (certain can do it). An example item is: “Stick to your treatment schedule even when your daily routine is disrupted.” In the current data, Cronbach’s α was .94.
Data Analyses
Age, race, gender, SES, and duration of ART were entered as covariates in all analyses (using α=0.05). Because preliminary analyses did not reveal significant associations between daily frequency of prescribed HIV medication and the main study variables (i.e., internalized stigma, self-efficacy, concern about being seen by others while taking HIV medication, and medication adherence), analyses did not include daily frequency of medication as a covariate. (Results were similar, and conclusions the same when this variable was used as a covariate.) Multiple regression was used to assess the association between internalized stigma and self-efficacy. Logistic regression was used to examine the association between self-efficacy and medication adherence (a dichotomous outcome), with internalized stigma included or excluded from the analyses. To test for the mediating role of self-efficacy in the relationship between internalized-stigma and medication adherence, we calculated bias-corrected 95% confidence intervals for indirect effects using bootstrapping with Process33. To test for parallel mediation of concern about being seen taking HIV medication and self-efficacy in the relationship between internalized stigma and medication adherence, we also used Process to calculate simultaneous (specific) indirect effects. Sensitivity analyses evaluated ART adherence based upon raw (continuous) scores rather than dichotomized adherence using bootstrapping (with no assumptions about distributions) in linear regression and mediation analyses.
RESULTS
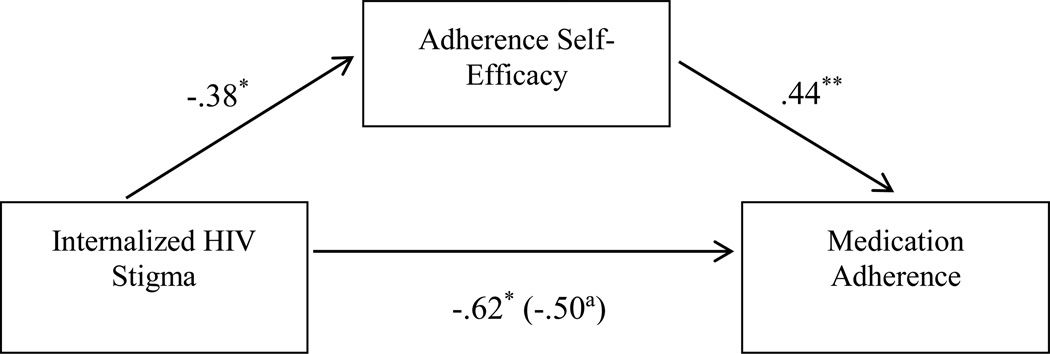
Of the 180 participants, 62% were Black and 64% were male, with an average age of 45.37 years (SD = 10.96); 35% were on a single pill once daily. In a regression analysis, internalized stigma was significantly associated with lower self-efficacy (B = −0.43, t = −2.82, p = .005). When entered into a logistic regression together with the covariates, self-efficacy was associated with a higher likelihood of excellent medication adherence ((Adjusted Odds Ratio (AOR) = 1.62, p = .001, 95% CI [1.23, 2.14]). When self-efficacy and internalized stigma were entered simultaneously, self-efficacy remained significantly associated with excellent medication adherence; AOR = 1.56, p = .001, 95% CI [1.19, 2.04], whereas the effect of internalized stigma was no longer significant (AOR = .61, p = .09, 95% CI [.34, 1.08]). Mediation analysis revealed a significant indirect effect of internalized stigma on non-optimal adherence through the pathway of lower self-efficacy (B = −.17, SE = .14, CI [−.53, −.02]; see Figure 1).
Figure 1.
HIV Treatment adherence self-efficacy mediates the effect of internalized HIV stigma on medication adherence.
Note. Associations are presented as path coefficients (unstandardized).
a Direct effect, which is the remaining effect of internalized HIV stigma on adherence after accounting for the mediating effect of adherence self-efficacy.
* p < .05
** p < .01
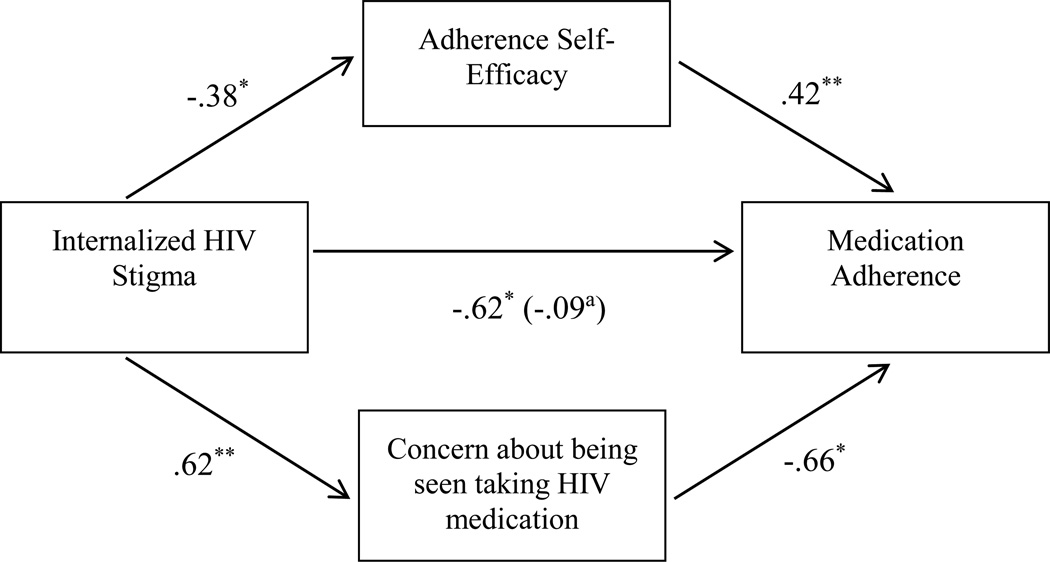
When entered simultaneously into a mediation analysis, both concern about being seen taking HIV medication and adherence self-efficacy had significant parallel mediating effects on the association between internalized stigma and medication adherence (B = −.16, SE = .13, CI [−.48, −.01] and B = −.41, SE = .23, CI [−.88, −.02], respectively for self-efficacy and concern about being seen taking HIV medication). Paths in this model are presented in Figure 2. Internalized stigma was associated with both lower self-efficacy and increased concerns about being seen taking HIV medication, and both mediators were associated with sub-optimal ART adherence in paths that are independent of each other. When the two mediations were accounted for, the remaining direct effect (which also includes indirect effects of variables not measured in this study) was reduced to almost zero (B = −0.09, p = .80; which was significant without the two mediators in the model: B = −0.62, p = .02). Contrast analysis did not reveal a significant difference in the size of the two mediating paths (B = 0.25, SE = 0.27, CI [−.26, .81]). Sensitivity analyses using medication adherence as a continuous dependent variable yielded very similar results (see Supplemental Digital Content 1).
Figure 2.
HIV treatment adherence self-efficacy and concern about being seen taking HIV medication simultaneously mediate the effect of internalized HIV stigma on medication adherence.
Note. Associations are presented as path coefficients (unstandardized).
a Direct effect, which is the remaining effect of internalized HIV stigma on adherence after accounting for the mediating effects of both adherence self-efficacy and concern about being seen taking HIV medication.
* p < .05
** p < .01
DISCUSSION
Results suggest that PLWH who internalize HIV-related stigma have decreased confidence in their ability to adhere to their treatment regimen when faced with challenges, which in turn decreases medication adherence. Thus, low adherence self-efficacy seems to be one mechanism by which internalized stigma affects medication adherence. In contrast, PLWH with low internalized stigma may tend to persevere and overcome obstacles in order to adhere to their treatment regimen.
We also found that adherence self-efficacy and concern about being seen taking HIV medication both mediate the association between internalized stigma and ART adherence in paths independent of each other. Moreover, these two factors accounted for nearly all of the observed association between internalized stigma and ART adherence. Findings outline the vital importance of independent roles of both interpersonal (concern about being seen) and intrapersonal (adherence self-efficacy) mechanisms in explaining the effects of internalized HIV stigma on ART adherence.
Katz et al5 maintain that HIV-related stigma reduction interventions should target multiple levels of influence including both interpersonal and intrapersonal factors to achieve maximum effectiveness. This view coincides with present results that demonstrate the importance of both interpersonal and intrapersonal factors in undermining ART adherence. Adherence interventions may be successful by either targeting stigma in the community, reducing internalized stigma, building self-efficacy, or addressing interpersonal concerns, or if resources permit, by targeting all of these factors simultaneously. Targeting a mediating construct will be effective to the degree that it explains the association between stigma and adherence. Targeting multiple mediators simultaneously may increase the effect of the intervention, provided that these factors have significant specific indirect effects independent of each other. Another intervention strategy is to find ways to block the paths from internalized stigma to self-efficacy or to interpersonal concerns, or to block the paths from low-self efficacy and from interpersonal concerns to non-adherence.
This study had limitations. We used self-report measures, which have known disadvantages. Mediation analyses are exploratory and causal inferences cannot be made because our study was cross-sectional. Furthermore, in mediation analysis there may be unobserved variables associated with both the mediators and the outcome, biasing results. Future research should replicate these findings using longitudinal designs and/or using non-questionnaire measures, such as the experience sampling method, which has started to be used in HIV research15.
The present study is the first to demonstrate parallel mediation of both inter- and intrapersonal factors in the stigma-ART adherence association and highlights the importance of addressing both types of factors in understanding this association as well as for interventions.
Supplementary Material
Acknowledgments
Sources of support:
This research was supported by the University of Alabama at Birmingham (UAB) Center for AIDS Research CFAR, an NIH funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). We would like to thank C. Blake Helms, Maria Lechtreck, Wesley Browning, Christy Thai, and all the research assistants for their help in data collection. This article is based in part on an undergraduate honors thesis conducted by Victoria Seghatol-Eslami under the supervision of Dr. Bulent Turan at the University of Alabama at Birmingham.
Footnotes
Meetings at which parts of the data were presented:
11th International Conference on HIV Treatment and Prevention Adherence, Fort Lauderdale, May 9–11, 2016
Conflicts of interest:
The authors declared that no conflicts of interest exist.
REFERENCES
- 1.Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- 2.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDS. 2006;20(5):359–368. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 3.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. Journal of general internal medicine. 2009;24(10):1101–1108. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sweeney SM, Mitzel LD, Vanable PA. Impact of HIV-related stigma on medication adherence among persons living with HIV. Current Opinion in Psychology. 2015;5:96–100. [Google Scholar]
- 5.Katz IT, Ryu AE, Onuegbu AG, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS. Soc. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helms CB, Turan JM, Atkins G, et al. Interpersonal Mechanisms Contributing to the Association Between HIV-Related Internalized Stigma and Medication Adherence. AIDS Behav. 2016:1–10. doi: 10.1007/s10461-016-1320-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mitzel LD, Vanable PA, Brown JL, Bostwick RA, Sweeney SM, Carey MP. Depressive symptoms mediate the effect of HIV – related stigmatization on medication adherence among HIV – infected men who have sex with men. AIDS Behav. 2015;19(8):1454–1459. doi: 10.1007/s10461-015-1038-6. [DOI] [PubMed] [Google Scholar]
- 9.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742–753. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 10.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one’s HIV – positive status, stigma and social support. AIDS Care. 2008;20(10):1266–1275. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 11.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 12.Turan B, Smith W, Cohen M, et al. Mechanisms for the negative effects of internalized HIV-related stigma on ART adherence in women: the roles of social isolation and depression. JAIDS. 2016;72(2):198–205. doi: 10.1097/QAI.0000000000000948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rao D, Feldman BJ, Fredericksen RJ, et al. A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS and Behavior. 2012;16(3):711–716. doi: 10.1007/s10461-011-9915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES) J. Behav. Med. 2007;30(5):359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turan B, Fazeli P, Raper JL, Mugavero MJ, Johnson MO. Social support and moment-to-moment changes in treatment self-efficacy in men living with HIV: Psychosocial moderators and clinical outcomes. Health Psychol. doi: 10.1037/hea0000356. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- 17.Ammassari A, Trotta MP, Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J. Acquir. Immune Defic. Syndr. 2002;31(Suppl 3):S123–S127. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- 18.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19(2):124–133. [PubMed] [Google Scholar]
- 19.Tyler-Viola LA, Corless IB, Webel A, Reid P, Sullivan KM, Nichols P. Predictors of medication adherence among HIV- positive women in North America. JOGNN. 2013;43(2):168–178. doi: 10.1111/1552-6909.12288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DiIorio C, McCarthy F, Depadilla L, et al. Adherence to antiretroviral medication regimens: a test of a psychosocial model. AIDS Behav. 2009;13(1):10–22. doi: 10.1007/s10461-007-9318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Turan B, Budhwani H, Fazeli PL, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. 2016:1–9. doi: 10.1007/s10461-016-1451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.West SG, Aiken LS. Toward understanding individual effects in multicomponent prevention programs: Design and analysis strategies. In: Bryant KJWM, West SG, editors. The science of prevention: Methodological advances from alcohol and substance abuse research. Washington, DC: American Psychological Association; 1997. pp. 167–209. [Google Scholar]
- 24.Judd CM, Kenny DA. Process analysis estimating mediation in treatment evaluations. Evaluation review. 1981;5(5):602–619. [Google Scholar]
- 25.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 26.Ajzen I, Fishbein M. Attitudinal and normative variables as predictors of specific behavior. J. Pers. Soc. Psychol. 1973;27(1):41. [Google Scholar]
- 27.Mickelson KD, Williams SL. Perceived stigma of poverty and depression: examination of interpersonal and intrapersonal mediators. J. Soc. Clin. Psychol. 2008;27(9):903. [Google Scholar]
- 28.Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–318. doi: 10.1007/s10461-012-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu M, Safren SA, Skolnik P, et al. Optimal recall period and response task for self – reported HIV medication adherence. AIDS Behav. 2008;12:86–94. doi: 10.1007/s10461-007-9261-4. [DOI] [PubMed] [Google Scholar]
- 30.Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- 31.DeMasi RA, Graham NM, Tolson JM, et al. Correlation between self-reported adherence to highly active antiretroviral therapy (HAART) and virologic outcome. Adv. Ther. 2001;18(4):163–173. doi: 10.1007/BF02850110. [DOI] [PubMed] [Google Scholar]
- 32.Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12(3):255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 33.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.