Abstract
Background
Average sodium intake and stroke mortality in northern China are both among the highest in the world. An effective, low-cost strategy to reduce sodium intake in this population is urgently needed.
Objective
We sought to determine the effects of a community-based sodium reduction program on salt consumption in rural northern China.
Design
This study was a cluster-randomized trial done over 18 months in 120 townships (one village from each township) from five provinces. Sixty control villages were compared to 60 intervention villages that were given access to a reduced-sodium, added-potassium salt substitute in conjunction with a community-based health education program focusing on sodium reduction. The primary outcome was the difference in 24-hour urinary sodium excretion between randomized groups.
Results
Among 1,903 people with valid 24-hour urine collections, mean urinary sodium excretion in intervention compared with control villages was reduced by 5.5% (-14mmol/day, 95% confidence interval -26 to -1; p = 0.03), potassium excretion was increased by 16% (+7mmol/day, +4 to +10; p<0.001), and sodium to potassium ratio declined by 15% (-0.9, -1.2 to -0.5; p<0.001). Mean blood pressure differences were -1.1 mm Hg systolic (-3.3 to +1.1; p = 0.33) and -0.7 mm Hg diastolic (-2.2 to +0.8, p = 0.35) and the difference in the proportion with hypertension was -1.3% (-5.1 to 2.5, p = 0.56).
Conclusion
There were clear differences in population sodium and potassium intake between villages that were most likely a consequence of increased use of salt substitute. The absence of effects on blood pressure reflects the moderate changes in sodium and potassium intake achieved.
Trial Registration
Clinicaltrials.gov identifier: NCT01259700.
Introduction
Stroke is the leading cause of death in China, responsible for about 1.7 million deaths each year [1,2]. Excess sodium intake is a key determinant of high blood pressure [3], the leading cause of stroke [4]. The magnitude of the effect of sodium on blood pressure is such that each 75mmol difference in daily salt intake translates into an approximate 5.4mmHg difference in systolic blood pressure amongst individuals with hypertension and 2.4mmHg amongst individuals with non-hypertensive starting levels of blood pressure[3]. China, especially in the rural areas, has one of the highest sodium intake levels in the world [5,6]. In western populations most dietary sodium derives from processed and restaurant foods but in rural China the majority comes from salt added in cooking and condiments at home [7]. In this situation, the substitution of salt with an alternate product lower in sodium may provide a particular opportunity to deliver a large public health benefit at low cost [8]. Beneficial effects of salt substitution on urinary electrolytes and blood pressure have been achieved in randomised trials done in selected populations including those in rural China [9–14] but whether effects can be achieved in the general community is unknown. We therefore undertook a trial of a pragmatic intervention using a reduced-sodium, added-potassium salt substitute to determine whether this could reduce average population sodium intake in rural China.
Subjects and Methods
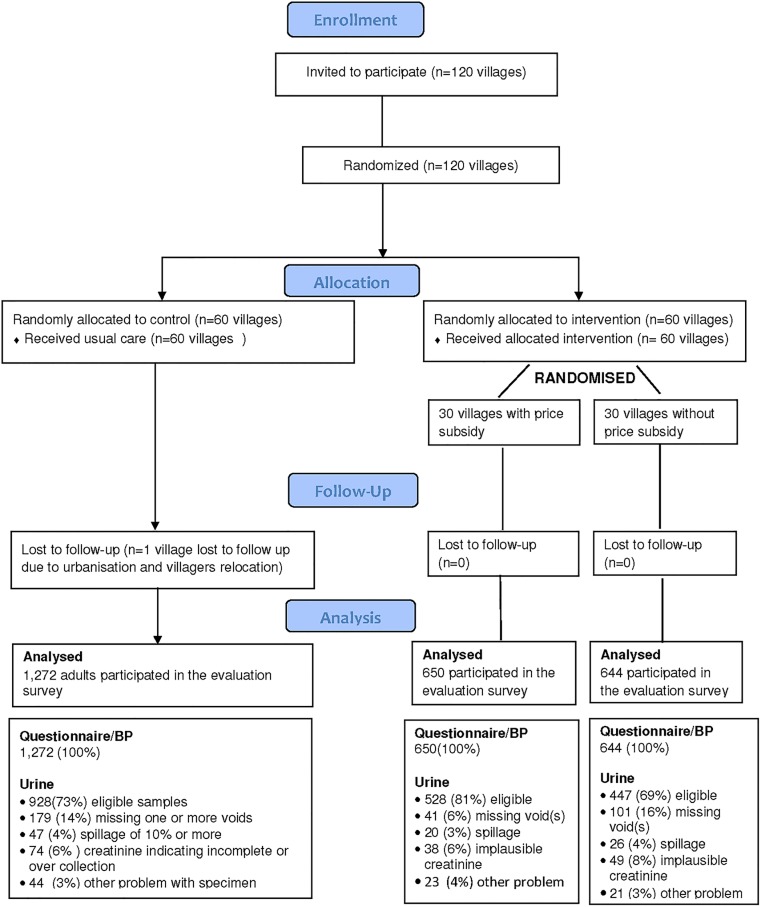
Details of the rationale and design of the China Rural Health Initiative Sodium Reduction Study have been described previously [15]. In brief, the sodium reduction study is one of the two parallel cluster-randomized controlled trial of the China Rural Health Initiative Project conducted in northern rural China between May 2011 and November 2012. It was done in collaboration with local academic institutions and governments in Hebei, Liaoning, Shanxi and Shaanxi provinces and the Ningxia Autonomous Region. The China Rural Health Initiative was registered with clinicaltrial.gov (NCT01259700). The study design is summarized in Fig 1.
Fig 1. Study CONSORT Flow Diagram.
Ethics
The project was reviewed and approved by the Institutional Review Boards of the Peking University Health Science Center in Beijing, China and of the Duke University Health System in Durham, USA. We have obtained verbal group consent from the chief of each of the study villages to implement the study intervention and obtained written consent from all individuals who participated in the end of the study survey. Verbal group consent from the village chiefs have been approved by the above mentioned ethics committees.
Provinces, townships and villages included
Two counties were selected from each province/autonomous region and 12 townships from each county, making a total of 120 townships. Within each township one village was selected for participation. The risk of contamination between adjacent intervention and control villages was minimized by the organizational separation of the townships and a geographic separation of 10 kilometers or more between participating villages. A typical township in the study comprised about 17 villages and included 25,000 people with at least one village doctor providing basic health services in each village. The average population size of included villages was 1,867 individuals living in 512 households with an annual per capita income of US$884.
Randomization
Townships were randomized in a 1:1 ratio to either the sodium reduction program or continued usual practices with stratification by county. Intervention villages were then further assigned at random to receive subsidization of the price of salt substitute, or not, using the same approach to stratification.
Intervention and control
Intervention villages—the salt reduction program comprised community-based health education and availability of reduced-sodium, added-potassium salt substitute at village shops. The health education component was delivered by the township health educators with assistance from the village council and the village doctors through public lectures, the display and distribution of promotional materials, and special interactive education sessions targeted towards individuals at elevated risk of vascular diseases [15]. The salt substitute was made available for purchase in all intervention villages and promoted through the health education component of the intervention. Residents in villages randomized to the price subsidy were provided with coupons that enabled the purchase of salt substitute at the same price as usual salt. Control villages—continued their usual practices and were exposed to little by way of efforts to achieve individual or population-wide salt reduction.
Evaluation
A population survey was done at the end of the intervention period amongst an age- and sex-stratified random sample of 20 or more consenting adults drawn from each of 119 villages, resulting in 2,566 survey participants. One village in the control group was lost to follow-up with the site urbanized and the villagers relocated. The survey included a brief interviewer-administered questionnaire, measurement of blood pressure, height and weight, and the collection of a 24-hour urine sample. Blood pressure was measured in duplicate with the participant seated after 5 minutes rest, using an automated electronic sphygmomanometer (Omron Intellisense HEM 7301 IT) with measurements made at least two minutes apart. Materials and instructions for collecting a timed 24-hour urine sample were provided. On the day of collection, participants were asked to urinate and discard that sample, and then collect all urine in the following 24 hours. At the same time the next day they were asked to urinate and collect that void before completing the 24 hour urine collection. The samples were collected, the volume was recorded, and an aliquot was shipped to a central lab for assay of sodium, potassium, and creatinine.9 Individuals that were pregnant, breastfeeding, menstruating, vomiting, had diarrhea, excessive sweating, or symptoms of a urinary tract infection did not provide a urine collection. Urine samples were excluded if participants reported missing the first morning void, missing more than one void, a collection period less than 22 hours or longer than 26 hours, or spilling more than 10% of the total volume. Samples contaminated with faeces were also excluded as were collections that had a volume of less than 500mL or greater than 6000mL, or a 24-hour creatinine excretion of less than 4mmol or greater than 25mmol in women and less than 6mmol or greater than 30mmol in men [16–19].
For each individual, the 24-hour sodium excretion value (mmol/day) was calculated as the concentration of sodium in the urine (mmol/L) multiplied by the urinary volume (L/day). The conversion from sodium (Na) to salt (NaCl) was made by multiplying the sodium value in mmol by 23 to obtain the sodium value in milligrams and then multiplying that figure by 2.54 to obtain the value for salt (NaCl) in milligrams.
Outcomes
The primary outcome was 24-hour urinary sodium excretion measured as a proxy for salt intake. The secondary outcomes were 24-hour urinary potassium excretion, urinary sodium to potassium ratio, systolic blood pressure, diastolic blood pressure, and the proportion with hypertension (defined as a measured systolic blood pressure of 140mmHg or above, a measured diastolic blood pressure of 90mmHg or above, or the use of blood pressure lowering therapy in the last two weeks). A series of process outcomes measuring knowledge and behaviors relating to salt and salt substitute were also recorded as were spontaneously reported adverse events.
Statistical power
The study was designed to provide at least 90% power (with a two-sided alpha = 0.05) to detect a difference in mean 24-hour excretion of sodium of at least 11mmol/day (0.65g/day salt) between intervention and control clusters. This estimate assumed a standard deviation of 24-hour sodium excretion of 60mmol/day (observed in study 95mmol/day), an intra-cluster correlation coefficient of 0.05 (observed in study 0.07), and a sample of 2,400 individuals drawn from 120 clusters randomized equally between intervention and control.
Analysis
Statistical analyses were done using the SAS system version 9.2 (Chinese simplified).
Analysis of treatment effects was by intention to treat with between group comparisons for the study outcomes made using generalized estimating equations (GEE) with clusters accounted for as random effects for continuous outcomes and using GEE logistic regression model with clusters accounted for as fixed effects for categorical outcomes. All statistical analyses were adjusted for the effects of clustering and additional adjustment were not done. Where data were missing, the number of observation was reported and missing values were not imputed. A derived variable was considered missing (for example, 24 hour urinary sodium excretion) when one or more of the related variables was missing (urinary sodium concentration and/or 24 hour urine volume). Generalized estimating equations (GEE) accounting for clustering effects were used to obtain effect estimates, 95% confidence intervals, and p-values for all outcomes. The primary comparison was between intervention clusters (n = 60) and control clusters (n = 59) with outcome data. In addition, the effects of subsidizing the price of the salt substitute were explored by estimating effects in the intervention clusters with price subsidy (n = 30) vs. those without price subsidy (n = 30). Finally, analyses were repeated in participant subgroups defined by median age (58 years), sex, years of education, median BMI (24kg/m2), smoking status, and alcohol consumption. A p-value of less than 0.05 was considered significant for the primary comparison but results for secondary analyses and tests of interaction were interpreted in light of the multiple comparisons made.
Results
The mean age of the 2,566 survey participants was 55 years, 50% were female, and one third smoked (Table 1). Survey participants provided 1,903 eligible urine samples (975 from intervention villages and 928 from control villages) with 663 samples missing entirely or deemed ineligible for another reason. The main reasons for ineligible samples were failure to collect all urine voids (321 individuals) and reported spillage (93 individuals) (Fig 1). There were no differences in the reasons for missing samples between intervention and control villages. Individuals with missing urine samples were noted to have on average lower levels of BMI (23.8 vs. 24.5kg/m2; p<0.001) but there were no differences in age and gender.
Table 1. Characteristics of survey participants.
| 60 intervention villages (n = 1,294) | 59 control villages (n = 1,272) | |
|---|---|---|
| Female (%) | 50 | 50 |
| Age (years) ± SD | 55±15 | 55±14 |
| Formal education (%)* | ||
| ≤6 years | 54 | 56 |
| 6 to 9 years | 38 | 35 |
| >9 years | 8 | 9 |
| Current smoker (%) | 33 | 30 |
| Drinks alcohol& (%) | 25 | 25 |
| Height (cm) ± SD | 161 ±8.5 | 161±8.9 |
| Weight (kg) ± SD | 63 ± 11 | 63 ±11 |
| Body Mass Index (kg/m2) ± SD | 24 ±3.5 | 25 ±3.6 |
*As reported by participant. SD = standard deviation.
&Drinks alcohol is defined as having consumed any type of alcohol in the three months prior to the survey.
Among the 1,903 people with eligible 24-hour urine collections, mean urinary sodium excretion in intervention compared with control villages was 5.5% lower (-14mmol/day, 95% confidence interval -26 to -1; p = 0.03), potassium excretion was 16% higher (+7mmol/day, +4 to +10; p<0.001), and sodium to potassium ratio 15% lower (-0.9, -1.2 to -0.5; p<0.001) (Table 2). The results were similar if analyses were done including urines from 468 additional individuals with urine samples that were not entirely missing but deemed ineligible for the primary analyses (ST1). Mean blood pressure differences were -1.1 mm Hg systolic (-3.3 to +1.1; p = 0.33), -0.7 mm Hg diastolic (-2.2 to +0.8 p = 0.35), and percentage with hypertension was 1.
Table 2. Estimated effects of sodium reduction strategy for 60 intervention compared to 59 control villages.
| n | Intervention | Control | Difference between intervention and control (95% confidence interval) | p-value | |
|---|---|---|---|---|---|
| Primary outcome | |||||
| Urinary sodium (mmol/day)* | 1903 | 237±97 | 251±94 | -14 (-26 to -1) | 0.03 |
| Secondary outcomes | |||||
| Urinary potassium (mmol/day)* | 1903 | 53±25 | 45±19 | 7 (4 to 10) | <0.001 |
| Urinary sodium:potassium ratio* | 1903 | 5.2±3.1 | 6.1±2.5 | -0.9 (-1.2 to -0.5) | <0.001 |
| Systolic blood pressure (mmHg)* | 2564 | 141±22 | 142±23 | -1.1 (-3.3 to 1.1) | 0.33 |
| Diastolic blood pressure (mmHg)* | 2565 | 86±14 | 86±14 | -0.7 (-2.2 to 0.8) | 0.35 |
| Percentage with hypertension& (%) | 2566 | 56 | 58 | -1.3 (-5.1 to 2.5) | 0.56 |
| Process outcomes | |||||
| Know excess salt intake is harmful (%) | 2562 | 84 | 76 | 8.3 (5.2 to 11) | <0.001 |
| Know daily limit is ≤6g/day (%) | 2564 | 53 | 16 | 37 (33 to 40) | <0.001 |
| Know reducing salt lowers BP (%) | 2564 | 67 | 52 | 15 (12 to 19) | <0.001 |
| Concerned about salt in diet (%) | 2545 | 76 | 62 | 14 (11 to 18) | <0.001 |
| Household uses salt substitute (%) | 2562 | 62 | 6 | 56 (53 to 59) | <0.001 |
| Other outcomes | |||||
| Antihypertensive drug use (%) | 2566 | 19 | 21 | -2.1 (-5.2 to 1.0) | 0.18 |
*Numbers reported after ± are standard deviations unless otherwise stated
&Hypertension defined as having systolic blood pressure at or above 140 mm Hg and/or a diastolic blood pressure at or above 90 mm Hg and/or reports use of blood pressure lowering medication in the last two weeks.
3% lower (-5.1 to 2.5%, p = 0.56) (Table 2). There was no heterogeneity of effects of intervention versus control on sodium excretion in the subgroups studied (all p>0.4).
There was a numerically, but not statistically significant, greater effect of the intervention on the primary outcome with subsidization of the price of salt substitute (p = 0.20) (Table 3). The same was true for all the secondary outcomes (all p>0.06) and the findings were again comparable if analyses included individuals with urine specimens collected but deemed ineligible on the basis of the pre-specified urine inclusion criteria (ST 2).
Table 3. Estimated effects of sodium reduction strategy for 30 intervention villages with price subsidy for salt substitute compared to 30 intervention villages without price subsidy for salt substitute.
| With price subsidy | Without price subsidy | Difference between price subsidy and no price subsidy (95% confidence interval) | p-value | |||
|---|---|---|---|---|---|---|
| Primary outcome | n | Mean ± SD | n | Mean ± SD | ||
| Urinary sodium (mmol/day)* | 528 | 232±95 | 447 | 243±98 | -11 (-29 to 6) | 0.20 |
| Secondary outcomes | n | Mean ± SD* | n | Mean ± SD* | ||
| Urinary potassium (mmol/day)* | 528 | 55±26 | 447 | 51±25 | 4 (-1 to 9) | 0.13 |
| Urinary sodium:potassium ratio* | 528 | 5.0±3.4 | 447 | 5.5±2.7 | -0.5 (-1.0 to 0.0) | 0.06 |
| Systolic blood pressure (mmHg)* | 650 | 140±22 | 643 | 141±22 | -1.4(-4.6 to 1.8) | 0.40 |
| Diastolic blood pressure (mmHg)* | 649 | 86±13 | 644 | 86±14 | -0.3 (-2.5 to 1.9) | 0.80 |
| Percentage with hypertension& (%) | 650 | 54 | 644 | 59 | -4.4 (-9.7 to 1.0) | 0.18 |
| Process outcomes | n | % | n | % | ||
| Know excess salt intake is harmful (%) | 650 | 83 | 643 | 85 | -1.7 (-5.7 to 2.3) | 0.52 |
| Know daily limit is ±6g/day (%) | 650 | 56 | 643 | 50 | 5.2 (-0.20 to 11) | 0.30 |
| Know reducing salt lowers BP (%) | 650 | 67 | 643 | 68 | -1.7 (-6.8 to 3.4) | 0.71 |
| Concerned about salt in diet (%) | 647 | 78 | 641 | 74 | 4.0 (-0.69 to 8.7) | 0.23 |
| Household uses salt substitute (%) | 650 | 78 | 643 | 44 | 35 (30 to 40) | <0.001 |
| Other outcomes | n | % | n | % | ||
| Antihypertensive drug use (%) | 650 | 18 | 644 | 20 | -1.9 (-6.2 to 2.4) | 0.40 |
*Mean ± standard deviations unless otherwise stated.
&Hypertension defined as having systolic blood pressure at or above 140 mm Hg and/or a diastolic blood pressure at or above 90 mm Hg and/or reports use of blood pressure lowering medication in the last two weeks.
There was greater knowledge about the adverse effects of salt, the harm caused by high blood pressure, concern about the levels of salt in the diet, and the recommended upper limit for daily salt consumption in intervention compared to control villages (all p<0.001) (Table 2). Use of salt substitute was ten-fold higher in the intervention villages and among these villages, the reported use of salt substitute was double in the villages with the price subsidy compared to the villages without the price subsidy (Table 3).
The most commonly reported adverse events occurring during the study period were dizziness, headache, weakness, stomach ache, hypotension, and fall which occurred at similar rates in the two randomised groups (all p>0.41). Serious vascular events were reported by few of those surveyed with no significant differences between randomised groups for stroke, coronary heart disease, heart failure, kidney disease or hyperkalaemia (all p>0.15).
Discussion
The salt reduction program achieved the intended lower urinary sodium excretion with a reduction of about three quarters of a gram of salt per day against a background daily consumption of approximately fourteen grams. The increase in urinary potassium, fall in the urinary sodium to potassium ratio, and ten-fold higher reported use of salt substitute among intervention compared to control villages, suggest that the fall in urinary sodium consumption was achieved primarily through use of salt substitute. Effects on blood pressure were modest and non-significant but consistent in magnitude with the fall in sodium reduction achieved. A larger study would be required to reliably detect any effect on blood pressure of the observed changes in sodium consumption.
Salt substitute costs about twice as much as usual salt (4CNY [US$0.65] vs. 2CNY [US$0.33] per kg). While salt substitute is still a low cost condiment, we anticipated that this would be a disincentive to use. Accordingly, we investigated the effect of price subsidy and found the uptake of salt substitute in villages with a subsidy to be almost twice that of villages with no price subsidy. If the price differential could be removed, or salt substitute could in some other way replace usual salt as the staple commodity, then average population sodium consumption could likely be reduced by considerably more than the 5.5% reduction achieved in this trial. A larger sodium reduction, in conjunction with a rise in potassium, would be expected to translate into major public health benefits resulting from reductions in blood pressure levels, the incidence of stroke, and other blood pressure-related diseases [3]. Given that effects of salt substitutes are larger amongst individuals with higher baseline blood pressure levels the magnitude of protection would be expected to be greater amongst hypertensives.
The trial has a number of strengths. It was carried out in a rural setting in China where most sodium in the diet is from cooking or condiment use and where salt substitute has the greatest potential to reduce sodium intake [20]. The trial benefitted from its large size and robust randomized design, and included gold standard assessment of dietary sodium consumption using 24-hour urine collections. The exclusion of individuals with suspected inaccurate or incomplete 24hr urine samples maximized the precision of the estimates in each group and our capacity to detect changes. It was, however, an open rather than a blinded study and to avoid bias considerable efforts were required to ensure that the population surveys were done identically in intervention and control villages [15]. The study was powered to detect effects on urinary markers of sodium and potassium consumption but was not designed to detect effects on blood pressure and hypertension which were specified only as secondary outcomes. While the intended sample size was not achieved the study still had reasonable power to detect the primary effect under investigation. Baseline survey data were not available because of resource constraints. Although an assessment based upon follow-up surveys alone was an entirely valid approach to evaluation of the intervention, the lack of baseline data reduced the statistical power and made the treatment effect comparison between two treatment groups less robust. It is also possible that there were chance baseline imbalances between groups that this design would not have controlled for. Antihypertensive drug use can influence urinary electrolyte excretion but seems unlikely to have substantively influenced trial results given the comparable rates of usage in each randomised group. Salt substitutes have been available in multiple markets around the world including China for many years and are considered safe and well-tolerated.[21–24] Accordingly we did not systematically collect tolerability data during this study and advised use in the intervention communities according to established practices in China.
There are eight randomized trials of salt substitute published to date with six reporting significant falls in systolic blood pressure [9–14] and the remainder trends toward blood pressure reduction[21,22,25,26]. These trials all provided salt substitute to intervention participants at no cost and showed much larger reductions in sodium excretion and blood pressure than were achieved with the strategy used in the present study. Our study demonstrates that a low-intensity community-based sodium reduction strategy can lower average sodium intake but also highlights the rather limited impact that can be achieved by this approach. The full potential of salt substitution in rural China will only be delivered by a policy that makes salt substitute the standard condiment for the entire population. Were this polity to be promoted throughout rural China, it should result in a population wide decline in blood pressure and the prevention of many tens of thousands of strokes and heart attacks each year. [3,20]
Conclusion
Population sodium intake was reduced by our intervention, primarily through increased use of salt substitute. Larger effects could be achieved in rural China by a wholesale switch from salt to salt substitute, with the potential for major public health benefit in this population which is at very high risk of stroke.
Supporting Information
Estimated effects of sodium reduction strategy for 60 intervention compared to 59 control villages on urinary outcomes (with all urine samples)
(DOCX)
Estimated effects of sodium reduction strategy for 30 intervention villages with price subsidy for salt substitute compared to 30 intervention villages without price subsidy for salt substitute on urinary outcomes (with all urine samples)
(DOCX)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
Acknowledgments
The Steering Committee for the China Rural Health Initiative is comprised of: Qide Han (Honorary Chair), Yang Ke (Chair), Yangfeng Wu (Vice Chair and Secretary General), Michael Merson (Vice Chair), Bruce Neal (Vice Chair), Paul Elliott, Xiangxian Feng, Stephen Leeder, Lingzhi Kong, Alan Lopez, Qun’an Mao, Jingpu Shi, Jianxin Zhang, Ruijuan Zhang and Yuhong Zhang. The Scientific Committee for the Sodium Reduction Study is comprised of Bruce Neal (Chair), Lijing L. Yan (Vice Chair), Elizabeth DeLong, Michael Dibley, Jixiang Ma, Wenyi Niu, Yangfeng Wu. Ad hoc members of the Scientific Committee are Darwin Labarthe and Paul Elliott.
We would like to thank the supports from the national, provincial, county, township, and village governments and health authorities and cooperation of our study participants. We would also like to thank the county leaders (Zhongbao Ji, Xintai Liu, Jianwei Liang, Shusheng Liu, Wenli Wang, Fangjie Liu, Hongyi Su, Lei Pan, Xuanmin Yang, Xiaowei Xing), county health educators (Jianhua Zhang, Wangui Qi, Haigen Li, Jianghai Yao, Jing Liu, Lizhong Wu, Kefeng Cai, Hongyi Su, Xiujuan Tian, Shuai Huang, Weiping Zhu), county project officers (Xinchun He, Min Wang, Yunfeng Bai, Junhui Ren, Hui Li, Yan Yuan, Xiaobing Liu, Yuxia Ma, Zhonggang Zhao, Mingliang Ren, Xin Mao), and project coordination center team members (Yanqing Wang, Xuejun Yin, Cong Li, Maoyi Tian) for their contributions to our study.
Data Availability
We have confirmed with our major funding agency National Heart, Lung and Blood Institute in The United States in July this year, that the study dataset will be made available upon request from September 2016 onwards through the NIH data repository-BioLINCC. The website address is: https://biolincc.nhlbi.nih.gov/home/.
Funding Statement
This project has been funded in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, and National Center for Chronic Disease Prevention and Health Promotion (CDC), under Contract No. HHSN268200900027C. Additional support has been received from the UnitedHealth Group Chronic Disease Initiative. Bruce Neal is supported by an Australian Research Council Future Fellowship and National Health and Medical Research Council Senior Research Fellowship and Nicole Li by an Australian National Health and Medical Research Council Overseas Fellowship. Paul Elliott is supported through the MRC-PHE Centre for Environment and Health, Imperial College London, and by the National Institute for Health Research (NIHR) Biomedical Research Centre at Imperial College Healthcare NHS Trust and Imperial College London; he is an NIHR Senior Investigator. The views expressed are those of the authors and not necessarily those of any sponsors.
References
- 1.China Ministry of Health (2013) China Annual Health Statistics Yearbook, 2011.
- 2.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380: 2095–2128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He FJ, Li J, Macgregor GA (2013) Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 346: f1325 10.1136/bmj.f1325 [DOI] [PubMed] [Google Scholar]
- 4.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 367: 1747–1757. 10.1016/S0140-6736(06)68770-9 [DOI] [PubMed] [Google Scholar]
- 5.INTERSALT Cooperative Research Group (1988) INTERSALT: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 287: 319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, et al. (2003) Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. Journal of Human Hypertension 17: 623–630. 10.1038/sj.jhh.1001605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan Q, Zhao L, et al. (2010) Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. Journal of the American Dietetic Association 110: 736–745. 10.1016/j.jada.2010.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. (2011) Priority actions for the non-communicable disease crisis. Lancet 377: 1438–1447. 10.1016/S0140-6736(11)60393-0 [DOI] [PubMed] [Google Scholar]
- 9.Gilleran G, O'Leary M, Bartlett WA, Vinall H, Jones AF, Dodson PM. (1996) Effects of dietary sodium substitution with potassium and magnesium in hypertensive type II diabetics: a randomised blind controlled parallel study. Journal of Human Hypertension 10: 517–521. [PubMed] [Google Scholar]
- 10.Chang HY, Hu YW, Yue CS, Wen YW, Yeh WT, Hsu LS, et al. (2006) Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr 83: 1289–1296. [DOI] [PubMed] [Google Scholar]
- 11.The China Salt Substitute Study Collaborative Group (2007) Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. Journal of Hypertension 25: 2011–2018. 10.1097/HJH.0b013e3282b9714b [DOI] [PubMed] [Google Scholar]
- 12.Charlton KE, Steyn K, Levitt N, Peer N, Jonathan D, Gogela T, et al. (2008) A food-based dietary strategy lowers blood pressure in a low socio-economic setting: a randomised study in South Africa. Public Health Nutrition 11: 1397–1406. 10.1017/S136898000800342X [DOI] [PubMed] [Google Scholar]
- 13.Mu J, Liu Z, Liu F, Xu X, Liang Y, Zhu D. (2009) Family-Based Randomized Trial to Detect Effects on Blood Pressure of a Salt Substitute Containing Potassium and Calcium in Hypertensive Adolescents. American Journal of Hypertension 22: 943–947. 10.1038/ajh.2009.136 [DOI] [PubMed] [Google Scholar]
- 14.Sarkkinen E, Kastarinen M, Niskanen TH, Karjalainen PH, Venäläinen TM, Udani JK, et al. (2011) Feasibility and antihypertensive effect of replacing regular salt with mineral salt -rich in magnesium and potassium- in subjects with mildly elevated blood pressure. Nutrition Journal 10: 88 10.1186/1475-2891-10-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li N, Yan L, Niu W, Labarthe D, Feng X, Shi J, et al. (2013) A Large-Scale Cluster Randomized Trial to Determine the Effects of Community-Based Dietary Sodium Reduction- The China Rural Health Initiative Sodium Reduction Study. American Heart Journal 166: 815–822. 10.1016/j.ahj.2013.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vandevijvere S, De Keyzer W, Chapelle JP, Jeanne D, Mouillet G, Huybrechts I, et al. (2010) Estimate of total salt intake in two regions of Belgium through analysis of sodium in 24-h urine samples. Eur J Clin Nutr 64: 1260–1265. 10.1038/ejcn.2010.148 [DOI] [PubMed] [Google Scholar]
- 17.Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerova J, Richart T, et al. (2011) Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA 305: 1777–1785. 10.1001/jama.2011.574 [DOI] [PubMed] [Google Scholar]
- 18.Venezia A, Barba G, Russo O, Capasso C, De Luca V, Farinaro E, et al. (2010) Dietary sodium intake in a sample of adult male population in southern Italy: results of the Olivetti Heart Study. Eur J Clin Nutr 64: 518–524. 10.1038/ejcn.2010.22 [DOI] [PubMed] [Google Scholar]
- 19.The INTERSALT Co-operative Research Group (1986) INTERSALT Study an international co-operative study on the relation of blood pressure to electrolyte excretion in populations. I. Design and methods. J Hypertens 4: 781–787. [DOI] [PubMed] [Google Scholar]
- 20.Blood Pressure Lowering Treatment Trialists' Collaboration. (2003) Effects of different blood pressure lowering regimens on major cardiovascular events: Second cycle of prospectively designed overviews. Lancet 362: 1527–1535. [DOI] [PubMed] [Google Scholar]
- 21.Karppanen H, Tanskanen A, Tuomilehto J, Puska P, Vuori J, Jäntti V, et al. (1984) Safety and effects of potassium- and magnesium-containing low sodium salt mixtures. Journal of Cardiovascular Pharmacology 6 Suppl 1: S236–243. [DOI] [PubMed] [Google Scholar]
- 22.Kawasaki T, Itoh K, Kawasaki M (1998) Reduction in blood pressure with a sodium-reduced, potassium- and magnesium-enriched mineral salt in subjects with mild essential hypertension. Hypertension Research—Clinical & Experimental 21: 235–243. [DOI] [PubMed] [Google Scholar]
- 23.Mervaala EM, Paakkari I, Laakso J, Nevala R, Teravainen TM, Fyhrquist F, et al. (1994) Replacement of salt by a novel potassium- and magnesium-enriched salt alternative improves the cardiovascular effects of ramipril. British Journal of Pharmacology 111: 1189–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neutel J. Replacing regular salt with a reduced sodium salt containing potassium and magnesium may offer a non-pharmacological approach to lowering blood pressure; 1996.
- 25.Geleijnse JM, Witteman JC, Bak AA, den Breeijen JH, Grobbee DE (1994) Reduction in blood pressure with a low sodium, high potassium, high magnesium salt in older subjects with mild to moderate hypertension. BMJ 309: 436–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou X, Liu J, Shi R, Yang N, Song D, Pang W, et al. (2009) Compound Ion Salt, a Novel Low-Sodium Salt Substitute: From Animal Study to Community-Based Population Trial. American Journal of Hypertension 22: 934–942. 10.1038/ajh.2009.135 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Estimated effects of sodium reduction strategy for 60 intervention compared to 59 control villages on urinary outcomes (with all urine samples)
(DOCX)
Estimated effects of sodium reduction strategy for 30 intervention villages with price subsidy for salt substitute compared to 30 intervention villages without price subsidy for salt substitute on urinary outcomes (with all urine samples)
(DOCX)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
Data Availability Statement
We have confirmed with our major funding agency National Heart, Lung and Blood Institute in The United States in July this year, that the study dataset will be made available upon request from September 2016 onwards through the NIH data repository-BioLINCC. The website address is: https://biolincc.nhlbi.nih.gov/home/.