Abstract
We retrospectively studied 181 patients with polycythaemia vera (n=67), essential thrombocythaemia (n=67) or primary myelofibrosis (n=47), who presented a first episode of splanchnic vein thrombosis (SVT). Budd–Chiari syndrome (BCS) and portal vein thrombosis were diagnosed in 31 (17.1%) and 109 (60.3%) patients, respectively; isolated thrombosis of the mesenteric or splenic veins was detected in 18 and 23 cases, respectively. After this index event, the patients were followed for 735 patient years (pt-years) and experienced 31 recurrences corresponding to an incidence rate of 4.2 per 100 pt-years. Factors associated with a significantly higher risk of recurrence were BCS (hazard ratio (HR): 3.03), history of previous thrombosis (HR: 3.62), splenomegaly (HR: 2.66) and leukocytosis (HR: 2.8). Vitamin K-antagonists (VKA) were prescribed in 85% of patients and the recurrence rate was 3.9 per 100 pt-years, whereas in the small fraction (15%) not receiving VKA more recurrences (7.2 per 100 pt-years) were reported. Intracranial and extracranial major bleeding was recorded mainly in patients on VKA and the corresponding rate was 2.0 per 100 pt-years. In conclusion, despite anticoagulation treatment, the recurrence rate after SVT in myeloproliferative neoplasms is high and suggests the exploration of new avenues of secondary prophylaxis with new antithrombotic drugs and JAK-2 inhibitors.
Introduction
Splanchnic vein thrombosis (SVT) encompasses hepatic veins (Budd–Chiari syndrome, BCS) and portal, mesenteric and splenic veins, and is a rare event in the general population: the annual incidence accounts for 0.8 per million for BCS, 0.7 per 100 000 for portal vein thrombosis and 2.7 per 100 000 for mesenteric vein thrombosis.1, 2, 3, 4 In these cases, the JAK2V617F mutation, the hallmark of myeloproliferative neoplasms (MPNs), can be detected in 13.6–26.6% of non-cirrhotic and non-malignant SVT patients, even in the absence of a clear diagnostic picture of MPN.5 In fully expressed Philadelphia-negative MPN, including polycythaemia vera (PV), essential thrombocythaemia and primary myelofibrosis, the more frequent sites of thrombosis are arterial vessels or leg veins and pulmonary embolisms (PEs) but also include unusual sites such as cerebral veins6 and SVT. These latter occur at much higher frequency (1–10%)7 than in the general population, where the incidence of these rare events is no more than 2–3 per 100 000.1, 2, 3, 4
Whether the recurrent events have a higher frequency than in the non-MPN population has not yet been assessed in a large series of patients with a well-established diagnosis of fully expressed MPN. To prevent recurrence, there is a general consensus that vitamin K-antagonist (VKA) should be prescribed long-term, very often in combination with cytoreductive therapy.8, 9 However, this recommendation is based on a consensus among the experts and is not universally accepted. A recent survey involving expert haematologists revealed a marked heterogeneity of choices on the duration of VKA and on the use of cytoreduction; moreover, this survey showed great uncertainty regarding the use of aspirin either alone or in association with VKA.10
In this study, we retrospectively collected a cohort of 181 SVT index events occurring in strictly defined patients with PV, essential thrombocythaemia and primary myelofibrosis managed in the clinical practice of 23 haematologic European centres. We describe here the pattern of presentation and the rate and risk factors of recurrent thrombotic events, and report the bleeding associated with secondary prophylaxis therapy.
Patients and methods
Study patients
A retrospective study was conducted across 23 centres within the European Leukaemia Network on patients with a diagnosis of MPN according to the World Health Organization 2008 criteria,11 after the approval of the ethics committees (primary approval by the central ethics committees of the coordinating centre was obtained on 2 October 2014).
The participating centres were asked to select from their consecutive patients with MPN, the ones who had had venous thromboembolism (VTE) objectively documented from January 2005, including deep venous thrombosis (DVT) of the limbs, PE, thrombosis of the cerebral and splanchnic veins (hepatic, portal, mesenteric and splenic veins) and thrombosis of the retinal vein, and who had received a course of VKA or direct oral anticoagulants. The data were collected in an electronic system. Each centre reported the total number of medical files by data input into an electronic database developed to record all study data; patients were de-identified with an alphanumeric code to protect personal privacy.
The details of the survey procedure and the results obtained in the patients with DVT of the legs and/or PE have been previously published.12 Briefly, for each patient, the following information was recorded: demographic data, WHO diagnosis, location of thrombosis, method of objective diagnosis, the presence of microvascular disturbances (that is, erythromelalgia, transient ocular attacks, pulsatile headache, dizziness and tinnitus) or constitutional symptoms (that is, pruritus, fatigue, night sweats, fever, weight loss and pain in the limbs), mutational profile, results of the laboratory investigation for thrombophilia, full blood count at diagnosis and at thrombosis, and the presence of cardiovascular risk factors (that is, history of previous thrombosis before the index event, smoking habit, hypertension, dyslipidaemia and diabetes). Moreover, the presence of circumstantial risk factors at the time of any episode of VTE such as surgery, pregnancy, puerperium (until 6 weeks from delivery), oral contraceptive intake, hormone replacement therapy, trauma, leg cast, prolonged bed immobilization (>10 days) and long travel (>8 h) was also recorded; in the absence of the previously mentioned risk factors, VTE was considered unprovoked. Finally, the data regarding cytoreductive or antithrombotic treatment after VTE, the duration of the treatment and the reasons for discontinuation of the treatment was recorded. A diagnosis of VTE was accepted only if it was confirmed by objective methods according to current clinical practice, as previously reported,12 and was defined as a positive result using techniques such as angiography, ultrasonography, computerized tomography or nuclear magnetic resonance.
Outcomes
The aim of this study was to determine the rate of recurrent thrombosis in patients recruited in the general database, who had an SVT as an index event. SVT was defined as thrombosis of the hepatic, portal, mesenteric and splenic veins.
Venous or arterial thrombotic events that occurred after the index event were recorded only if objectively documented. Recurrent SVT was defined as an objectively established thrombus extension or occurrence in a previously patent segment, as previously defined.13 The following new manifestations, when objectively proven, were also defined as recurrent VTE: DVT of the arms or the limbs, PE and occlusion of cerebral veins. Finally, new arterial thrombotic events included ischaemic stroke, transient ischaemic attack, acute myocardial infarction, unstable angina pectoris and peripheral arterial thrombosis, when objectively diagnosed, as previously reported.12, 13, 14
Major bleeding was defined according to the criteria of the International Society on Thrombosis and Haemostasis15 when it was fatal and/or was symptomatic in a critical area or organ, such as intracranial bleeding, intraspinal bleeding, intraocular bleeding, retroperitoneal bleeding, intra-articular bleeding, pericardial bleeding, intramuscular bleeding with compartment syndrome and/or bleeding that led to a reduction of 2 g/dl or more in the haemoglobin concentration and/or necessitated the transfusion of two or more blood units.
Statistical methods
For continuous variables, the median and the range are provided. The annual incidence of recurrent thrombosis was calculated by dividing the number of events by the total number of patient years (pt-years). Differences in the proportions were estimated using the Fisher's exact test (statistical significance threshold set at P<0.05).
A multivariable model, including age >60 years, thrombosis history, cardiovascular risk factors, Hb >15 g/dl, Hct >45%, white blood cell (WBC) count >14 × 109/l, platelet count >500 × 109/l, splenomegaly, unprovoked event, BCS as index event versus other SVT index events, VKA treatment and other treatments, was performed to identify the significant predictors of recurrence or bleeding. Starting with all candidate variables, backward selection was used to test whether the deletion or retention of each variable improved the model, repeating this process until no further improvement was possible.
The probability of recurrence as a function of time was estimated using the Kaplan–Meier method by analysing the interval between the index thrombosis and a recurrent thrombotic event (uncensored observations) or the duration of time until death, or the time elapsed until the patient's final visit to the centre (censored observations). The thrombosis recurrence-free survival was compared between the groups using the log-rank test (statistical significance threshold set at P<0.05) and the relative risk of recurrence was estimated as a hazard ratio (HR) with a 95% confidence interval using a Cox proportional hazard regression model.
Results
Clinical and laboratory features of the patient cohort
Overall, 181 patients with SVT at MPN diagnosis (58%) or during the course of the disease were recruited (Table 1). The female sex was prevalent (65.2%); at the time of the index event, only a minority of patients (22.1%) were over 60 years of age and 28.2% were under 40 years of age.
Table 1. Clinical features of the cohort at the time of the index event.
| Male/female, N (%) | 63/118 (34.8/65.2) |
|---|---|
| Age, years, median (range) | 48 (29–74) |
| <40 years, n (%) | 51 (28.2) |
| 40–60 years, n (%) | 90 (49.7) |
| ⩾60 years, n (%) | 40 (22.1) |
| Diagnosis, N (%) | |
| PV | 67 (37.0) |
| ET | 67 (37.0) |
| PMF | 47 (26.0) |
| Years from diagnosis to index thrombosis, mean (±s.d.) | 2.01 (3.87) |
| Diagnosis at the time of index thrombosis, n (%) | 105 (58) |
| Hb gr/dl, median (range) | 13.4 (6.3–24.0) |
| Hct %, median (range) | 42.1 (22.0–70.0) |
| WBC count × 109/l, median (range) | 9.3 (3.0–50.0) |
| Platelet count × 109/l, median (range) | 424 (100–3000) |
| JAK2 mutation, N/N tested (%) | 166/178 (93.3) |
| CALR mutations, N/N tested | 4/25 (16.0) |
| MPL mutations, N/N tested | 1/28 (3.6) |
| Exon 12 mutations, N/N tested | 0/14 (0.0) |
| Abnormal karyotype, N/N tested (%) | 8/65 (12.3) |
| Microvascular disturbances, N (%) | 19 (10.5) |
| Constitutional symptoms, N (%) | 28 (15.5) |
| Palpable splenomegaly, N (%) | 119 (65.8) |
| Cm below costal margin, median (range) | 4 (1–25) |
| Localization of index thrombosis, N (%) | |
| Hepatic vein thrombosis (BCS) | 31 (17.1) |
| Portal vein thrombosis | 109 (60.3) |
| Mesenteric vein thrombosis | 18 (9.9) |
| Splenic vein thrombosis | 23 (12.7) |
| Unprovoked thrombosis, N (%) | 155 (85.6) |
| Provoked by, n (%) | 26 (14.4) |
| Oral contraceptives | 8 (4.4) |
| Hormone replacement therapy | 3 (1.7) |
| Infection | 3 (1.7) |
| Pregnancy/puerperium | 1 (0.6) |
| Cancer | 1 (0.6) |
| Surgery | 7 (3.9) |
| Liver disease | 3 (1.7) |
| Risk factors for index thrombosis | |
| History of thrombosis, N (%) | 14 (7.7) |
| History of arterial thrombosis, n (%) | 5 (2.8) |
| History of venous thrombosis, n (%) | 8 (4.4) |
| Presence of at least one vascular risk factor, N (%) | 52 (28.7) |
| Smoking habit | 19 (10.5) |
| Hypertension | 28 (15.5) |
| Dislipidemia | 7 (3.4) |
| Diabetes | 5 (2.8) |
| Presence of thrombophilia*, N/N tested (%) | 42/120 (35.0) |
| Inherited thrombophilia, N/N tested (%) | 21/120 (17.5) |
Abbreviations: BCS, Budd Chiari syndrome; ET, essential thrombocythaemia; Hb, haemoglobin; PMF, primary myelofibrosis; PV, polycythaemia vera; WBC, white blood cell.
Deficiency of antitrombin (n=1), deficiency of protein C or protein S (n=7), factor V Leiden and/or prothrombin G20210A (n=13), increased levels of homocysteine (n=16), antiphospholipids (n=6).
BCS and portal vein thrombosis were observed in 31 (17.1%) and 109 (60.3%) patients, respectively. The remaining 41 patients presented with isolated thrombosis of the mesenteric or splenic veins. The great majority were splenomegalic (median 4 cm below the costal margin) and one quarter reported microvascular disturbances and constitutional symptoms. Almost all (93.3%) carried the JAK2V617F mutation and 35% tested positive for genetic or acquired thrombophilia. No risk circumstance provoking SVT was present in the majority of the patients (85.6%). Of note, 113 patients (62.4%) had elevated blood counts, defined as Hct >45% and/or WBC>14 × 109/l and/or platelet count >500 × 109/l; no patient had WBC and platelet counts lower than 3.0 × 109 and 100 × 109/l, respectively.
Incidence of new vascular events after the index event and risk factors
All patients received a course of low-molecular-weight heparin as initial therapy, followed in the majority of the patients by VKA (153/181, 84.5%) as secondary prophylaxis (Table 2). Among patients on VKA, the drug was continued indefinitely in 136 (88.9%) for a median follow-up time of 3.5 years (range 8 months–15.8 years) and was discontinued in 17 (9.3%) after a median time of 2 years (range 1 month–6.2 years). The reasons for stopping VKA included a pre-established plan by the centres in six cases and major bleeding in three; in the remaining patients, VKA was discontinued because of the patient's preference or bleeding risk judged to be excessive by the care physician (for example, onset of thrombocytopenia during the course of the disease).
Table 2. Treatment after the index thrombosis.
| Total (%) |
Cytoreductiona |
||
|---|---|---|---|
| Yes | No | ||
| VKA | 143 (79.0) | 101 (70.6) | 42 (29.4) |
| VKA+antiplatelets | 10 (5.5) | 6 (60.0) | 4 (40.0) |
| Antiplatelets | 6 (3.3) | 6 (100) | 2 (0) |
| Heparin | 10 (5.5) | 7 (70.0) | 3 (30.0) |
| DOACs | 3 (1.7) | 2 (66.7) | 1 (33.3) |
| No antithrombotic treatment | 9 (5.0) | 8 (88.9) | 1 (11.1) |
| Total (%) | 181 (100) | 130 (71.8) | 51 (28.2) |
Abbreviations: DOAC, direct oral anticoagulant; VKA, vitamin K-antagonists.
Hydroxyurea in 108/130 cases (83%).
The overall observation time recorded after the SVT index event was 735 years (median 3.2, range 1 month to 15.8 years). There were 31 new episodes of thrombosis in 31 patients, with an overall incidence rate (IR) of 4.2 per 100 pt-years (95% confidence interval (95% CI): 2.9–5.9); 17 thrombotic events (54.8%) occurred within 2 years from the date of the index SVT. Sites of events were in the splanchnic veins in 45% and at other sites in 55%: cerebral veins, venous legs with or without PE and arterial occlusions (Table 3).
Table 3. Overall incidence of major outcomes after the index SVT.
| Events, n (%) | Incidence rate per 100 pt-years (95% CI) | |
|---|---|---|
| Thrombotic events | 31 (17.1) | 4.2 (2.9–5.9) |
| Venous thrombosis | 19 (10.5) | 2.5 (1.6–4.0) |
| Recurrent SVT | 1.9 (1.1–3.1) | |
| Hepatic vein thrombosis | 3 (1.7) | |
| Portal vein thrombosis | 4 (2.2) | |
| Mesenteric vein thrombosis | 6 (3.1) | |
| Splenic vein thrombosis | 1 (0.6) | |
| Venous thrombosis at other sites | 0.6 (0.2–1.5) | |
| DVT | 2 (1.1) | |
| PE | 2 (1.1) | |
| Cerebral vein thrombosis | 1 (0.6) | |
| Arterial thrombosis | 10 (5.5) | 1.3 (0.7–2.4) |
| Unstable angina | 1 (0.6) | |
| Myocardial infarction | 2 (1.1) | |
| Ischaemic stroke | 3 (1.7) | |
| Peripheral artery thrombosis | 3 (1.7) | |
| Retinal artery thrombosis | 1 (0.6) | |
| Not specified | 2 (1.1) | |
| Major bleeding | 16 (8.8) | 2.1 (1.3–3.5) |
| CNS | 4 (2.2) | |
| Gastrointestinal | 6 (3.1) | |
| Muscle hematoma | 2 (1.1) | |
| Unspecified | 4 (2.2) | |
| Hematologic evolutions | 15 (8.3) | 2.0 (1.2–3.3) |
| MF | 11 (6.1) | |
| AML | 4 (2.2) | |
| Solid cancer | 4 (2.2) | 0.5 (0.2–1.3) |
| Brain glioblastoma | 1 (0.5) | |
| Breast cancer | 1 (0.5) | |
| Nose skin cancer | 1 (0.5 | |
| Pancreas cancer | 1 (0.5) | |
| Deaths | 14 (7.7) | 1.9 (1.1–3.1) |
| ICH | 1 (0.6) | |
| Infection | 1 (0.6) | |
| MF | 1 (0.6) | |
| AML | 4 (2.2) | |
| Solid tumour | 2 (1.1) | |
| Other | 2 (1.1) | |
| Unknown | 3 (1.7) | |
Abbreviations: AML, acute myeloid leukemia; CI, confidence interval; CNS, central nervous system; DVT, deep vein thrombosis; ICH, intracranial haemorrhage; MF, myelofibrosis; PE, pulmonary embolism; pt-years, patient years; SVT, splanchnic vein thrombosis
No significant differences were found between the patients who had a recurrence and those who did not regarding diagnosis of PV (P=0.15), essential thrombocythaemia (P=0.41) and MF (P=0.82), the presence of JAK2V617F mutation (P=0.69) and thrombophilia (P=0.13).
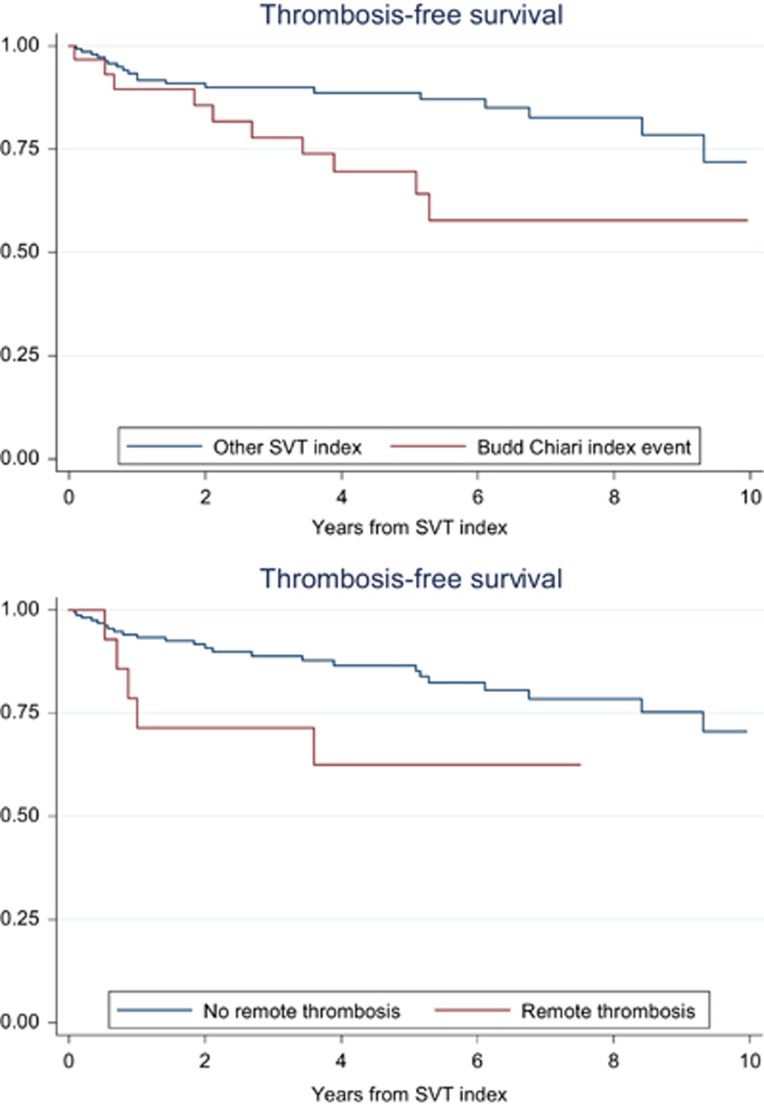
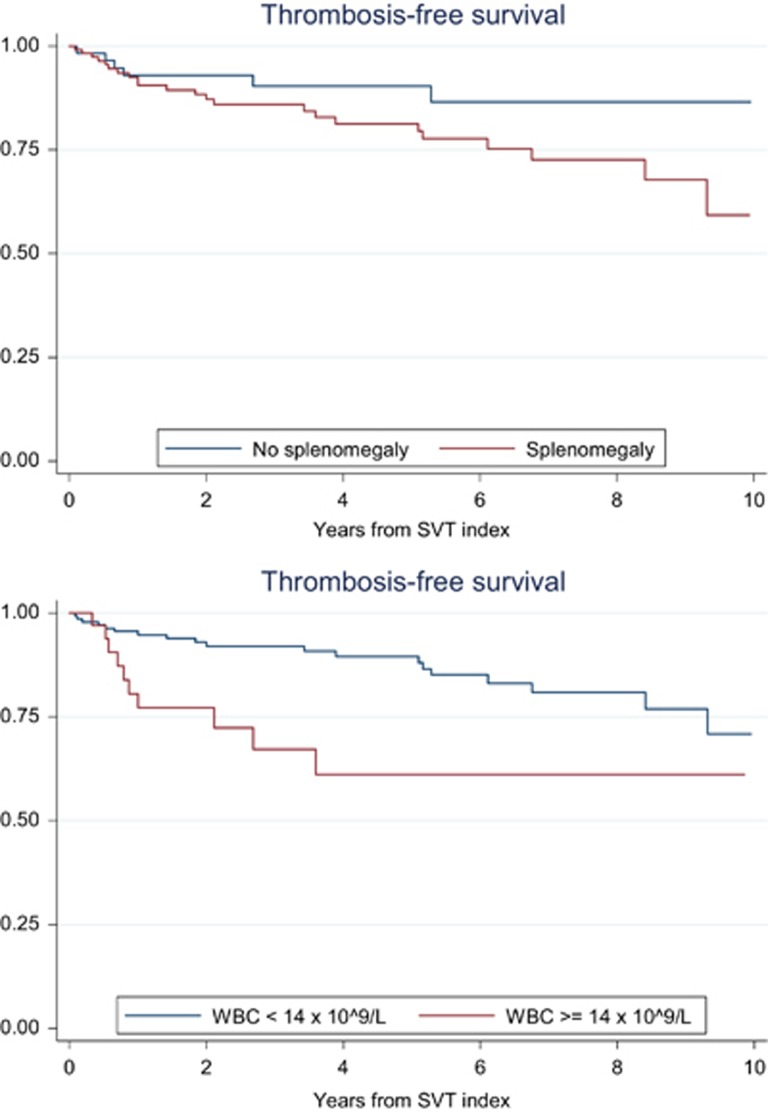
Backward logistic regression analysis showed an independent association with the new thrombotic event for BCS (HR: 3.03, 95% CI: 1.37–6.69), history of previous thrombosis (HR: 3.62, 95% CI: 1.22–10.78), splenomegaly (HR: 2.66, 95% CI: 1.06–6.64) and leukocytosis higher than the highest quartile, 14 × 109/l (HR: 2.8, 95% CI: 1.32–6.28). In particular, patients with BCS had an incidence rate of new events of 8.0 per 100 pt-years (95% CI: 4.0–14.4) that was significantly higher than in those with thrombosis of portal or other abdominal sites (Table 4). This difference was due to an increased rate of venous events in BCS patients, whereas no difference between the two groups was noticed in the rate of new arterial thromboses; of note, in patients with BCS there was a threefold increase in risk of recurrent SVT in respect to that of patients with other index SVT (5/31, 16.1% versus 9/150, 6%, odds ratio: 3.01, 95% CI: 0.93–9.71, P=0.06). The time to new events according to the presence of such risk factors is shown in the Kaplan–Meier curves of Figures 1 and 2.
Table 4. Sub-analysis of major outcomes and type of SVT index event (BCS vs other SVT).
| Index BCS (n=31) pt-years=136 | Other index SVT (n=150) pt-years=599 | P-value | |
|---|---|---|---|
| Thrombotic events, n (%) | 11 (35.4) | 20 (13.3) | 0.006 |
| Incidence rate, per 100 pt-years (95% CI) | 8.0 (4.0–14.4) | 3.3 (2.0–5.1) | 0.01 |
| Venous thrombosis, n (%) | 7 (22.5) | 12 (8.0) | 0.02 |
| Incidence rate, per 100 pt-years (95% CI) | 5.1 (2.0–10.6) | 2.0 (1.0–3.4) | 0.03 |
| Arterial thrombosis, n (%) | 3 (9.6) | 7 (4.6) | 0.37 |
| Incidence rate, per 100 pt-years (95% CI) | 2.2 (0.4–6.4) | 1.1 (0.4–2.4) | 0.34 |
| Major bleeding | 3 (9.6) | 13 (8.6 | 0.74 |
| Incidence rate, per 100 pt-years (95% CI) | 2.2 (0.4–6.4) | 2.1 (1.1–3.7) | 0.97 |
| Deaths | 2 (6.4) | 12 (8.0) | 1.00 |
| Incidence rate, per 100 pt-years (95% CI) | 1.4 (0.1–5.3) | 2.0 (1.0–3.4) | 0.64 |
Abbreviations: CI, confidence interval; BCS, Budd–Chiari syndrome; pt-years, patient years; SVT, splanchnic vein thrombosis.
Figure 1.
Thrombosis free-survival in patients with SVT index event according to the type of first event (BCS; HR: 2.38, 95% CI: 1.08–5.38, P=0.02; upper panel) and history of remote thrombosis (HR: 2.57, 95% CI: 0.99–6.88, P=0.04; lower panel).
Figure 2.
Thrombosis free-survival in patients with SVT index event according to presence of splenomegaly (HR: 2.24, 95% CI: 1.00–6.71, P=0.05; upper panel) and the presence of leukocytosis at the diagnosis (HR: 2.81, 95% CI: 1.17–6.34, P=0.08; lower panel).
Effect of VKA antithrombotic treatment on the incidence of recurrent thrombosis
Patients on VKA (n=136) experienced 23 new thrombotic events during a follow-up of 585 years, corresponding to a rate of 3.9 (95% CI: 2.4–5.8) per 100 pt-years. Fourteen events (60.8%) involved venous vesselsnine recurrent SVT, two DVT of the legs, two PE and one cerebral vein thrombosis. The remaining events were ischaemic stroke (n=3), acute coronary syndrome (n=2), peripheral artery thrombosis (n=2) and retinal artery thrombosis (n=1); the site of one event was not specified. In 13 cases, the international normalized ratio value at the time of recurrence was available, being within the therapeutic range 2.0–3.0 in six cases (range 2.10–2.80), <2.0 in five cases (range 1.70–1.85) and >3.0 in two cases (range 5.03–7.10).
Patients who discontinued VKA (n=17) and patients who never received VKA or direct oral anticoagulant prophylaxis (n=25) were followed up for 146 years and developed 4 and 4 events, respectively, corresponding to an overall annual rate of 5.4 (95% CI: 2.3–10.7) per 100 pt-years, which was not significantly different from that observed in patients receiving VKA (P=0.41). Five events (62.5%) were recurrent SVT. The remaining events were myocardial infarction (n=1) and peripheral artery thrombosis (n=1); the site of one event was not specified.
The comparison between the patients with ongoing VKA and those off VKA at the time of recruitment in the survey was repeated by analysis on-treatment. Among the patients who received VKA after the index event for a limited period of time, the total observation time was 36 pt-years on VKA; therefore, the overall pt-years on VKA and off VKA were 621 and 110, respectively. Accordingly, the rate of recurrences per 100 pt-years with or without VKA was 3.7 (95% CI: 2.3–5.5) and 7.2 (95% CI: 3.1–14.3), respectively (P=0.09). The 4 pt-years attributed to the three patients on direct oral anticoagulants were not computed in the analysis; none of these latter patients had a recurrent thrombosis.
The rate of new thrombotic events in patients receiving antiplatelet agents alone or in association with VKA (n=16) was 4.3 (95% CI: 0.5–15.7) per 100 pt-years and the combination of aspirin with VKA did not produce any advantage on the overall rate of thrombosis (P=0.79). However, all the arterial thrombotic events occurred in the absence of antiplatelet agents.
Effect of cytoreductive treatment on the incidence of recurrent thrombosis
Cytoreduction (mostly hydroxyurea) was administered to 130 patients (71.8% of the cohort) and was combined with VKA in 107 (82.3%). Patients with or without cytoreduction did not differ in the rate of PV, essential thrombocythaemia or MF diagnosis, age >60 years, BCS as index event, Hb >15 g/dl, WBC count >14 × 109/l, platelet count >500 × 109/l, splenomegaly and VKA treatment (data not shown). In patients receiving cytoreduction 23 recurrent events were recorded over 537 pt-years (IR 4.2 per 100 pt-years, 95% CI: 2.7–6.4) and in patients without cytoreductive treatment 8 recurrent events were recorded over 198 pt-years (IR 4.0 per 100 pt-years, 95% CI: 1.7–7.9; P=0.94). The analysis of the patients receiving both VKA and cytoreduction disclosed 20 recurrences over 471 pt-years (IR 4.2 per 100 pt-years, 95% CI: 2.5–6.5). Finally, four patients received ruxolitinib and had no recurrence after the SVT index event.
Overall, in patients not receiving cytoreduction after the index event, Hb >15 g/dl and/or WBC count >14 × 109/l, and/or a platelet count >500 × 109/l was recorded at the time of the recurrent thrombosis in three of eight cases with recurrences (37.5%). Similar blood values indicating a poor control of cell proliferation were observed at the time of the recurrence in 14 of the remaining 23 patients (60.8%) who had recurrent thrombosis during cytoreduction.
Incidence rate of major bleeding
Major bleeding occurred in 16 patients, with a rate of 2.1 (95% CI: 1.3–3.5) per 100 pt-years and was intracranial in 4 cases (Table 3). Thirteen events (81.2%) occurred in patients on VKA, one of which was a fatal intracranial haemorrhage. Two bleeding events occurred during treatment with ticlopidine; the remaining patient was not receiving any antithrombotic treatment. The incidences of major bleeding in patients taking and not taking VKA were 2.0 (95% CI: 1.1–3.5) and 2.7 (95% CI: 0.5–7.9) per 100 pt-years, respectively (P=0.67; on-treatment analysis).
A tendency towards a significantly higher IR of major bleeding was recorded in patients receiving cytoreduction (2.7 per 100 pt-years, 95% CI: 1.5–4.6) in respect to those without cytoreductive treatment (0.5 per 100 pt-years, 95% CI: 0.0–2.8; P=0.06).
Development of haematological transformation and solid cancer
During the follow-up (median 3.2 years), the progression to overt myelofibrosis and acute myeloid leukaemia was ascertained in 11 (6.1%) and 4 patients (2.2%), respectively; solid cancer was recorded in 4 patients (2.2% Table 3). The rate of haematological transformation tended to be higher in patients who had SVT during the follow-up after MPN diagnosis in comparison with patients who had SVT at the MPN diagnosis (11.8% vs 5.7%, P=0.15).
The disease transformation was unrelated to recurrent thrombotic events (odds ratio for transformation 1.8, 95% CI: 0.5–6.3, P=0.29).
Discussion
Despite the large number of reports of retrospective or prospective case series and meta-analyses concerning the association between SVT and MPN,5 the studies on prophylaxis after MPN-related SVT are limited to small series of no more than 50 patients.13, 16, 17, 18, 19, 20, 21 Our survey is the largest study cohort of MPN-related SVT ever reported, describing in detail the treatments after the index event, the subsequent outcomes and the risk factors for recurrence.
SVT was the heralding manifestation of MPN in 58% of the patients and followed the diagnosis of MPN in 42% this result is substantially aligned with the results of a meta-analysis in which 36% of the MPN-related SVT occurred during the follow-up after diagnosis.22 The most frequent site of thrombosis was the portal-mesenteric axis and BCS accounted for 17% this latter frequency is slightly higher than the value observed in the general population, where BCS accounts for 5 to 12% of SVT.13, 23, 24 The majority of patients were young females (65%), with a median age of 48 years, in agreement with previous MPN series16, 19, 25 and contrasting with the gender and older median age observed in the general population.13, 23
Inherited or acquired thrombophilia was found in one-third of the evaluated patients, with no difference compared with the diagnostic yield obtained in the general patient series.1, 13, 23 Of note, almost all patients (93%) carried the JAK2 V617F mutation, confirming the strength of association between this mutation and vascular events.5, 26
After a median follow-up of 3.2 years, 31 new thromboses were recorded, including both splanchnic and other venous, as well as arterial occlusions. The overall incidence rate of recurrent thrombosis was 4.2 per 100 pt-years, which is consistent with the prospective incidence of 5.9 per 100 pt-years reported in a small series of MPN-related SVT.13
Multivariable analysis revealed that BCS, history of thrombosis, splenomegaly and leukocytosis were independently associated with recurrence. The high incidence of recurrences in BCS was also reported by others, both in MPN patients20, 21 and in the non-MPN population.23 A predictive role for incident thrombosis in prior thrombotic history8, 9 and leukocytosis14, 27, 28 has been consistently found in MPN patients, including both arterial and venous thrombosis.
Interestingly, 38% of the patients had a blood cell count without hypercythaemia, which is a finding quite common in MPN-related SVT;25 moreover, no relevant leukopenia or thrombocytopenia was recorded. Therefore, anticoagulation was considered safe and was administered to 95% of patients, only a fraction of whom (71%) received cytoreductive therapy; this practice was likely to be due to the reluctance to use cytoreductive drugs in cases without overt elevated blood counts. However, cytoreductive treatment did not reduce the incidence rate of recurrent thrombotic events; nevertheless, it should be highlighted that 17 of the 31 events (55%) occurred in patients with hypercythaemia not receiving cytoreduction or in patients who failed to reach the haematological response in spite of cytoreduction.
Finally, splenomegaly emerged as an independent risk factor for recurrent thrombosis in our series with SVT. This result is consistent with other observations reporting a role of splenomegaly for new episodes of thrombosis in patients without SVT as well,29, 30 even though this finding has not been confirmed by other researchers.31 It has been speculated that splenomegaly should be considered an index of more intensive myeloproliferation; however, its association with recurrent SVT may also be due to a more extensive occlusion of the hepatic-portal venous axis. In patients with SVT, the JAK2/JAK1 inhibitor Ruxolitinib has shown significant activity in reducing the spleen volume,32 but no data are available thus far on whether this finding is associated with fewer recurrences. However, as reported in a recent meta-analysis, there is evidence suggesting that the drug may reduce the rate of total major thrombosis in myelofibrosis and PV.33 In our series only four patients received ruxolitinib, so that no conclusion can be drawn on this issue.
The incidence rate of recurrence in our patients was 3.9 per 100 pt-years in patients on VKA and 7.2 per 100 pt-years in patients off VKA. This frequency is a new finding and agrees with other studies of SVT in which the estimates were performed in the general population with SVT, including only a minority of MPN. In these reports, the frequency of recurrence ranged from 1.3 to 5.6 per 100 pt-years on VKA and from 3.3 to 11.9 per 100 pt-years after VKA discontinuation.13, 34, 35, 36 Notably, in patients with non-splanchnic DVT on long-term treatment with VKA, the recurrence rate is expected to be below 1 per 100 pt-years.37 The 2.0% rate of major bleeding on VKA among our cases was similar to the rate in SVT without MPN (from 1.2 to 3.9% pt-years)13, 34, 35, 36 and was slightly higher than expected in patients with non-splanchnic DVT on long-term VKA treatment (0.9 per 100 pt-years).37 These indirect comparisons suggest that in SVT, with or without MPN, antithrombotic prophylaxis is associated with an inferior efficacy and safety profile compared with other DVT cases. Therefore, antithrombotic prophylaxis in SVT, particularly in BCS, is an unmet clinical need and warrants prospective studies exploring the role of new direct oral anticoagulants38 and the new JAK2 inhibitors in MPN patients.
Acknowledgments
TB and AMV were supported by a grant from Associazione Italiana per la Ricerca sul Cancro (AIRC, Milano) ‘Special Program Molecular Clinical Oncology 5 × 1000' to AGIMM (AIRC-Gruppo Italiano Malattie Mieloproliferative). VDS was supported by an unrestricted grant from the Bruno Farmaceutici Foundation.
The authors declare no conflict of interest.
References
- De Stefano V, Martinelli I. Splanchnic vein thrombosis: clinical presentation, risk factors and treatment. Intern Emerg Med 2010; 5: 487–494. [DOI] [PubMed] [Google Scholar]
- Rajani R, Melin T, Björnsson E, Broomé U, Sangfelt P, Danielsson A et al. Budd-Chiari syndrome in Sweden: epidemiology, clinical characteristics and survival—an 18-year experience. Liver Int 2009; 29: 253–259. [DOI] [PubMed] [Google Scholar]
- Rajani R, Björnsson E, Bergquist A, Danielsson A, Gustavsson A, Grip O et al. The epidemiology and clinical features of portal vein thrombosis: a multicentre study. Aliment Pharmacol Ther 2010; 32: 1154–1162. [DOI] [PubMed] [Google Scholar]
- Acosta S, Alhadad A, Svensson P, Ekberg O. Epidemiology, risk and prognostic factors in mesenteric venous thrombosis. Br J Surg 2008; 95: 1245–1251. [DOI] [PubMed] [Google Scholar]
- De Stefano Qi X, Betti S, Rossi E. Splanchnic vein thrombosis and myeloproliferative neoplasms: molecular-driven diagnosis and long-term treatment. Thromb Haemost 2016; 115: 240–249. [DOI] [PubMed] [Google Scholar]
- Martinelli I, De Stefano V, Carobbio A, Randi ML, Santarossa C, Rambaldi A et al. Cerebral vein thrombosis in patients with Philadelphia-negative myeloproliferative neoplasms. An European LeukemiaNet study. Am J Hematol 2014; 89: E200–E205. [DOI] [PubMed] [Google Scholar]
- Sekhar M, McVinnie K, Burroughs AK. Splanchnic vein thrombosis in myeloproliferative neoplasms. Br J Haematol 2013; 162: 730–747. [DOI] [PubMed] [Google Scholar]
- Barbui T, Barosi G, Birgegard G, Cervantes F, Finazzi G, Griesshammer M et al. Philadelphia-negative classical myeloproliferative neoplasms: critical concepts and management recommendations from European LeukemiaNet. J Clin Oncol 2011; 29: 761–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vannucchi AM, Barbui T, Cervantes F, Harrison C, Kiladjian JJ, Kröger N et al. Philadelphia chromosome-negative chronic myeloproliferative neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015; 26(Suppl 5): v85–v99. [DOI] [PubMed] [Google Scholar]
- Ellis MH, Lavi N, Vannucchi A, Harrison C. Treatment of thromboembolic events coincident with the diagnosis of myeloproliferative neoplasms: a physician survey. Thromb Res 2014; 134: 251–254. [DOI] [PubMed] [Google Scholar]
- Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia 2008; 22: 14–22. [DOI] [PubMed] [Google Scholar]
- De Stefano V, Ruggeri M, Cervantes F, Alvarez-Larrán A, Iurlo A, Randi ML et al. High rate of recurrent venous thromboembolism in patients with myeloproliferative neoplasms and effect of prophylaxis with vitamin K antagonists. Leukemia 2016; 30: 2032–2038. [DOI] [PubMed] [Google Scholar]
- Ageno W, Riva N, Schulman S, Beyer-Westendorf J, Bang SM, Senzolo M et al. Long-term clinical outcomes of splanchnic vein thrombosis: results of an international registry. JAMA Intern Med 2015; 175: 1474–1480. [DOI] [PubMed] [Google Scholar]
- De Stefano V, Za T, Rossi E, Vannucchi AM, Ruggeri M, Elli E et al. Recurrent thrombosis in patients with polycythemia vera and essential thrombocythemia: incidence, risk factors, and effect of treatments. Haematologica 2008; 93: 372–380. [DOI] [PubMed] [Google Scholar]
- Schulman S, Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005; 3: 692–694. [DOI] [PubMed] [Google Scholar]
- Gangat N, Wolanskyj AP, Tefferi A. Abdominal vein thrombosis in essential thrombocythemia: prevalence, clinical correlates, and prognostic implications. Eur J Haematol 2006; 77: 327–333. [DOI] [PubMed] [Google Scholar]
- Amitrano L, Guardascione MA, Scaglione M, Pezzullo L, Sangiuliano N, Armellino MF et al. Prognostic factors in noncirrhotic patients with splanchnic vein thromboses. Am J Gastroenterol 2007; 102: 2464–2470. [DOI] [PubMed] [Google Scholar]
- Chinnakotla S, Klintmalm GB, Kim P, Tomiyama K, Klintmalm E, Davis GL et al. Long-term follow-up of liver transplantation for Budd-Chiari syndrome with antithrombotic therapy based on the etiology. Transplantation 2011; 92: 341–345. [DOI] [PubMed] [Google Scholar]
- Hoekstra J, Bresser EL, Smalberg JH, Spaander MC, Leebeek FW, Janssen HL. Long-term follow-up of patients with portal vein thrombosis and myeloproliferative neoplasms. J Thromb Haemost 2011; 9: 2208–2214. [DOI] [PubMed] [Google Scholar]
- Oldakowska-Jedynak U, Ziarkiewicz M, Ziarkiewicz-Wróblewska B, Dwilewicz-Trojaczek J, Górnicka B, Nyckowski P et al. Myeloproliferative neoplasms and recurrent thrombotic events in patients undergoing liver transplantation for Budd-Chiari syndrome: a single-center experience. Ann Transplant 2014; 19: 591–597. [DOI] [PubMed] [Google Scholar]
- Potthoff A, Attia D, Pischke S, Mederacke I, Beutel G, Rifai K et al. Long-term outcome of liver transplant patients with Budd-Chiari syndrome secondary to myeloproliferative neoplasms. Liver Int 2015; 35: 2042–2049. [DOI] [PubMed] [Google Scholar]
- Smalberg JH, Arends LR, Valla DC, Kiladjian JJ, Janssen HL, Leebeek FW. Myeloproliferative neoplasms in Budd-Chiari syndrome and portal vein thrombosis: a meta-analysis. Blood 2012; 120: 4921–4928. [DOI] [PubMed] [Google Scholar]
- Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE. Survival and recurrence in patients with splanchnic vein thromboses. Clin Gastroenterol Hepatol 2010; 8: 200–205. [DOI] [PubMed] [Google Scholar]
- Søgaard KK, Farkas DK, Pedersen L, Sørensen HT. Splanchnic venous thrombosis is a marker of cancer and a prognostic factor for cancer survival. Blood 2015; 126: 957–963. [DOI] [PubMed] [Google Scholar]
- Kiladjian JJ, Cervantes F, Leebeek FW, Marzac C, Cassinat B, Chevret S et al. The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases. Blood 2008; 111: 4922–4929. [DOI] [PubMed] [Google Scholar]
- Lussana F, Caberlon S, Pagani C, Kamphuisen PW, Büller HR, Cattaneo M. Association of V617F Jak2 mutation with the risk of thrombosis among patients with essential thrombocythaemia or idiopathic myelofibrosis: a systematic review. Thromb Res 2009; 124: 409–417. [DOI] [PubMed] [Google Scholar]
- Landolfi R, Di Gennaro L, Barbui T, De Stefano V, Finazzi G, Marfisi R et al. Leukocytosis as a major thrombotic risk factor in patients with Polycythemia Vera. Blood 2007; 109: 2446–2452. [DOI] [PubMed] [Google Scholar]
- Carobbio A, Antonioli E, Guglielmelli P, Vannucchi AM, Delaini F, Guerini V et al. Leukocytosis and risk stratification assessment in essential thrombocythemia. J Clin Oncol 2008; 26: 2732–2736. [DOI] [PubMed] [Google Scholar]
- Kaifie A, Kirschner M, Wolf D, Maintz C, Hänel M, Gattermann N et al. Bleeding, thrombosis, and anticoagulation in myeloproliferative neoplasms (MPN): analysis from the German SAL-MPN-registry. J Hematol Oncol 2016; 9: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andriani A, Latagliata R, Anaclerico B, Spadea A, Rago A, Di Veroli A et al. Spleen enlargement is a risk factor for thrombosis in essential thrombocythemia: evaluation on 1297 patients. Am J Hematol 2016; 91: 318–321. [DOI] [PubMed] [Google Scholar]
- Haider M, Gangat N, Hanson C, Tefferi A. Splenomegaly and thrombosis risk in essential thrombocythemia: the Mayo Clinic experience. Am J Hematol 2016; 91: E296–E297. [DOI] [PubMed] [Google Scholar]
- Pieri L, Paoli C, Arena U, Marra F, Mori F, Zucchini M et al. Long term follow up of a phase 2 study of Ruxolitinib in patients with splanchnic vein thrombosis associated with myeloproliferative neoplasm. Blood 2015; 126: 2803 [abstract]. [Google Scholar]
- Samuelson BT, Vesely SK, Chai-Adisaksopha C, Scott BL, Crowther M, Garcia D. The impact of ruxolitinib on thrombosis in patients with polycythemia vera and myelofibrosis: a meta-analysis. Blood Coagul Fibrinolysis 2016; 27: 648–652. [DOI] [PubMed] [Google Scholar]
- Riva N, Ageno W, Poli D, Testa S, Rupoli S, Santoro R et al. Safety of vitamin K antagonist treatment for splanchnic vein thrombosis: a multicenter cohort study. J Thromb Haemost 2015; 13: 1019–1027. [DOI] [PubMed] [Google Scholar]
- Riva N, Ageno W, Poli D, Testa S, Rupoli S, Santoro R et al. Recurrent thrombotic events after discontinuation of vitamin K antagonist treatment for splanchnic vein thrombosis: a multicenter retrospective cohort study. Gastroenterol Res Pract 2015; 2015: 620217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva N, Ageno W, Schulman S, Beyer-Westendorf J, Duce R, Malato A et al. Clinical history and antithrombotic treatment of incidentally detected splanchnic vein thrombosis: a multicentre, international prospective registry. Lancet Hematol 2016; 3: e267–e275. [DOI] [PubMed] [Google Scholar]
- Kearon C, Ginsberg JS, Kovacs MJ, Anderson DR, Wells P, Julian JA et al. Comparison of low-intensity warfarin therapy with conventional-intensity warfarin therapy for long-term prevention of recurrent venous thromboembolism. N Engl J Med 2003; 349: 631–639. [DOI] [PubMed] [Google Scholar]
- Finazzi G, Ageno W. Direct oral anticoagulants in rare venous thrombosis. Intern Emerg Med 2016; 11: 167–170. [DOI] [PubMed] [Google Scholar]