Abstract
Rationale: Post-traumatic stress disorder (PTSD) has been associated with asthma in cross-sectional studies. Whether PTSD leads to clinically significant bronchodilator response (BDR) or new-onset asthma is unknown.
Objectives: We sought to determine the relationship between probable PTSD and both BDR and incident asthma in a high-risk cohort of World Trade Center workers in New York (NY).
Methods: This study was conducted on data from a high-risk cohort of 11,481 World Trade Center workers in New York, including 6,133 never smokers without a previous diagnosis of asthma. Of the 6,133 never smokers without asthma, 3,757 (61.3%) completed a follow-up visit several years later (mean = 4.95 yr, interquartile range = 3.74–5.90 yr). At the baseline visit, probable PTSD was defined as a score 44 points or greater in the PTSD Checklist questionnaire, and BDR was defined as both a change of 12% or greater and an increment of 200 ml or greater in FEV1 after bronchodilator administration. Incident asthma was defined as a self-report of new physician-diagnosed asthma after the baseline visit. Multivariable logistic regression was used for the analysis of probable PTSD and baseline BDR or incident asthma.
Measurements and Main and Results: At baseline, probable PTSD was associated with BDR among all participants (adjusted odds ratio = 1.43; 95% confidence interval = 1.19–1.72), with similar results among never smokers without asthma. Among 3,757 never smokers, probable PTSD at baseline was associated with incident asthma, even after adjustment for baseline BDR (odds ratio = 2.41; 95% confidence interval = 1.85–3.13). This association remained significant in a confirmatory analysis after excluding 195 subjects with baseline BDR.
Conclusions: In a cohort of adult workers exposed to a severe traumatic event, probable PTSD is significantly associated with BDR at baseline and predicts incident asthma.
Keywords: post-traumatic stress disorder, bronchodilator response, incident asthma, World Trade Center
At A Glance Commentary
Scientific Knowledge on the Subject
A few cross-sectional studies have shown that exposure to traumatic events or post-traumatic stress disorder (PTSD) is associated with asthma symptoms or self-reported asthma. Whether PTSD leads to clinically significant bronchodilator response (BDR; a key component of asthma) or new-onset asthma is unknown.
What This Study Adds to the Field
We show that probable PTSD is significantly associated with clinically significant BDR and predicts incident asthma in adult workers exposed to a severe traumatic event (the World Trade Center disaster of September 11, 2001). Our findings strongly support an expanding body of literature linking stress-related disorders, such as PTSD, to the pathogenesis of asthma, and suggest that physicians treating adults with PTSD should be aware of their potentially increased risk of asthma.
Asthma is a major public health issue, affecting approximately 25.7 million people in the United States (1). Asthma and post-traumatic stress disorder (PTSD) have become chronic common conditions among workers who conducted rescue and recovery tasks at the World Trade Center (WTC) disaster site in 2001–2002 (2, 3). In a follow-up study, the cumulative incidences of asthma and PTSD among WTC rescue and recovery workers were 27.6 and 9.3%, respectively (4).
Observational studies in adults have shown that exposure to war-related trauma and PTSD are associated with asthma symptoms or self-reported asthma (5–8), but those studies were limited by a cross-sectional design and lack of objective data on reversible airflow obstruction, a key component of asthma. Expiratory airflow response to short-acting inhaled β2-agonists (bronchodilator response [BDR]) is often used to assess reversibility of airflow obstruction. BDR is widely used to support a diagnosis of asthma in adults, both in clinical practice and in clinical trials.
Whether PTSD is associated with BDR or new-onset (incident) asthma is unknown. Given preliminary evidence of a link between PTSD and asthma (5–7), we hypothesized that PTSD is associated with clinically significant BDR, and that PTSD leads to new onset of asthma in adults (even in those without pre-existing asthma or BDR). We tested these hypotheses in a large cohort of WTC rescue and recovery workers (4).
Methods
Subject Recruitment and Study Procedures
In 2002, the WTC Worker and Volunteer Medical Screening Program was established to characterize WTC-related effects on medical and mental health. Details on subject recruitment and the study protocol have been previously reported (9). In brief, study subjects were all workers and volunteers who performed rescue, recovery, and service restoration duties at the WTC disaster site from September 11, 2001 to June 2002 (including all occupational groups, except firefighters) (9). Eligibility criteria to participate in the screening and longitudinal surveillance program have been described elsewhere (9). Beginning in July 2002, all subjects underwent a baseline screening evaluation, which included questionnaires on respiratory symptoms, occupational exposures, self-reported physicians’ diagnoses, and the PSTD Checklist (PCL) (10), and spirometry. Subsequent (“monitoring”) health surveillance visits, including a similar evaluation, were scheduled at 12- to 18-month intervals.
Our exposure of interest was probable PTSD at the baseline study visit, defined as a score equal to or greater than 44 points in the PCL questionnaire, a validated scale (10). This score has been used in a number of previous studies of the WTC and other cohorts, and is strongly correlated with a clinical diagnosis of PTSD (10). In a secondary analysis, we examined trajectories of probable PTSD between the baseline and second follow-up visits, as previously defined: resilient (no probable PTSD at either study visit), recovering (probable PTSD at the baseline study visit, but not at the second follow-up visit), late onset (probable PTSD at the second follow-up visit, but not at the baseline visit), and chronic (probable PTSD at both study visits) (11).
Spirometry was performed using a portable flow spirometer (ndd, Zurich, Switzerland). At the baseline visit, spirometry was repeated 15 minutes after administration of two puffs of albuterol in as many subjects (∼80%) as possible. All testing and interpretative approaches followed American Thoracic Society recommendations (12). BDR was calculated as percent change in FEV1, as follows: ([postbronchodilator FEV1 − prebronchodilator FEV1]/prebronchodilator FEV1) × 100). BDR was also calculated as absolute change in milliliters (postbronchodilator FEV1 − prebronchodilator FEV1). Clinically significant BDR (heretofore simply BDR, for ease of exposition) was then defined as both a percent change of 12% or greater and an absolute increment of 200 ml or greater in FEV1 after bronchodilator administration.
At the second follow-up visit (mean = 4.95 yr, interquartile range = 3.74–5.90 yr), incident asthma was defined as self-report of a new diagnosis of physician-diagnosed asthma among subjects who reported not ever having had physician-diagnosed asthma at baseline.
Baseline covariates of interest included age (grouped into five categories: 20–29 yr, 30–39 yr, 40–49 yr, 50–59 yr, and at least 60 yr), sex, race/ethnicity (defined as non-Latino white, non-Latino African American, Latino [of any race], Asian, and other), smoking history and intensity of cigarette smoking, WTC occupational exposure, education (categorized as less than a high school diploma, high school graduate, some college, or college graduate), body mass index (BMI), and physician-diagnosed asthma. A subject was considered a lifetime nonsmoker if (s)he had smoked less than 20 packs of cigarettes (or 12 oz. of tobacco) in a lifetime, or less than 1 cigarette/d (or 1 cigar/wk) for 1 year. A minimum of 12 months without tobacco use was required to deem a subject a former smoker. Smoking intensity was quantitated among ever smokers as pack-years. For WTC occupational exposure, we used a previously published categorization, based on exposure to the dust cloud on September 11, 2001, work at the pile of the collapsed towers, and exposure duration (8). The very-high-exposure group consisted of those who were exposed to the dust cloud, and who worked at least some time on the pile of debris and for more than 90 days at the site. The high-exposure group was comprised of workers who were exposed to the dust cloud, but either did not work more than 90 days or on the pile of debris. The intermediate group consisted of workers not exposed to the dust cloud, and who either worked between 40 and 90 days, or did not work on the pile of debris. The low-exposure group included those who were not exposed to the dust cloud from the tower collapse, did not work in the debris pile, and for at least 40 days. Given that only 3% of the cohort was very highly exposed, we collapsed the very high and high categories into a high-exposure group, leaving a total of three categories. We categorized BMI at baseline examination into normal, overweight, and obese (18–24.9, 25–29.9, and ≥30 kg/m2, respectively). We also considered weight change between the baseline and follow-up visit, which was classified as: (1) loss of more versus less than 2.5 kg; or (2) gain of less than 2.5 kg, 2.5–5.0 kg, or more than 5 kg.
The study was approved by the Mount Sinai Program for the Protection of Human Subjects (Mount Sinai, New York, NY), and restricted to patients who signed an informed consent document to participate in research studies.
Statistical Analysis
The main characteristics of subjects with and without probable PTSD at the baseline visit were compared using chi-square or t tests, as appropriate. Logistic regression was used for the analysis of probable PTSD and BDR (at baseline) or incident asthma (by the follow-up visit) in study participants.
For the analysis of baseline PTSD and BDR, all multivariable models were adjusted for age, sex, race/ethnicity, education, smoking status, intensity of cigarette smoking, WTC occupational exposure, and BMI. Because tobacco use and asthma are both correlated with BDR, we repeated this analysis after excluding subjects who had ever received a diagnosis of asthma or had ever smoked before September 11, 2001.
We next conducted a multivariable analysis of probable PTSD at the baseline study visit and incident physician-diagnosed asthma between the baseline and follow-up visits. To avoid potential confounding by tobacco smoke and to examine only new-onset asthma, this analysis was restricted to lifetime nonsmokers who had not been diagnosed with asthma at the baseline visit. Because baseline BDR could be a marker of subclinical or undiagnosed asthma, this multivariable analysis was adjusted for baseline BDR, in addition to age, sex, race/ethnicity, WTC occupational exposure, education, baseline BMI, and weight change between the baseline and follow-up visits. In confirmatory analyses, we repeated the multivariable analysis after additional adjustment for the time elapsed between the baseline and follow-up visits, while also conducting a multivariable analysis restricted to subjects without BDR at baseline. Finally, we conducted a secondary analysis of probable PTSD trajectories and incident physician-diagnosed asthma between the baseline and follow-up visits, adjusting for the same variables as in our primary analysis above.
All analyses were conducted using the SAS statistical package (v. 9.3; SAS Institute, Cary, NC).
Results
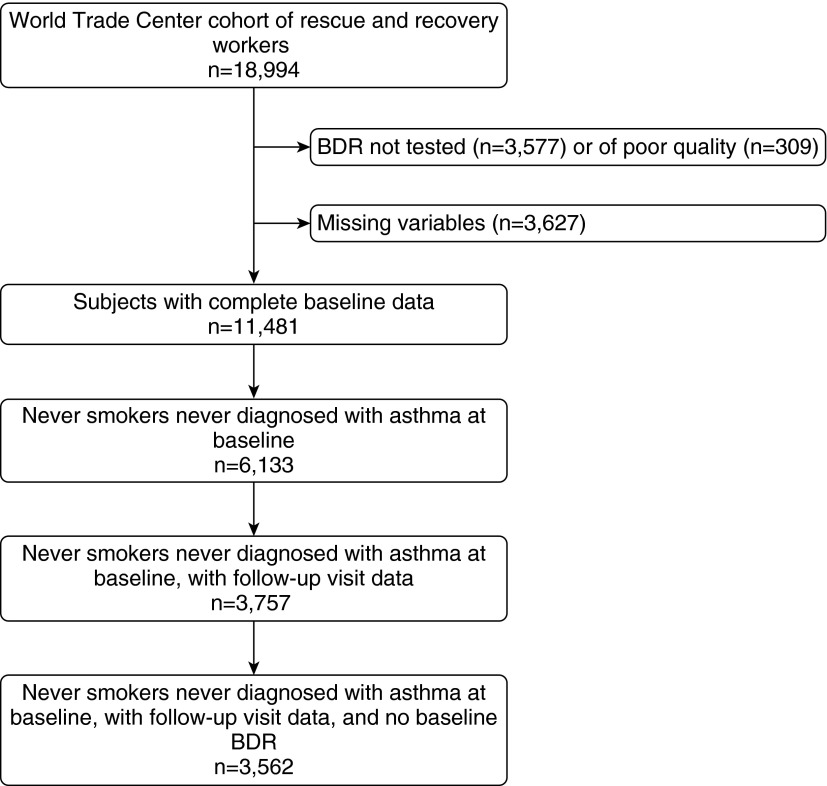
Of the 18,994 subjects who completed a baseline visit, 11,481 (60.4%) had complete data on probable PTSD, BDR, asthma, and the covariates of interest, and were thus included in the current analysis (see Figure 1). Compared with subjects excluded from the analysis of data from the baseline visit, those included were significantly more likely to be aged 20–39 years, to be Latino or non-Latino white or non-Latino Asian, to be lifetime nonsmokers, and to have intermediate WTC occupational exposure. On the other hand, subjects included in the analysis were less likely to be 50 years of age or older, to be of “other” race or ethnicity, to be a former or current smoker, to have probable PTSD, or to have BDR than those excluded. There was no significant sex difference between subjects who were and were not included in the analysis (see Table E1 in the online supplement).
Figure 1.
Flow diagram for subjects included in the study. BDR = bronchodilator response.
Table 1 shows a comparison of the main characteristics of the study participants who did and did not have probable PTSD at the baseline study visit. Among all 11,481 study participants, those who had probable PTSD were significantly more likely to be female, to be 50 years of age or older, to be Latino, to be current smokers and to have higher pack-years of smoking, to lack or not to have attained more than a high school diploma, to have had an intermediate WTC occupational exposure, and to have BDR than those without probable PTSD. There was no significant difference in having ever had physician-diagnosed asthma, or in having an overweight or obesity classification between subjects with and without PTSD. Similar findings were obtained for the comparison of the main characteristics of subjects with and without probable PTSD among the 6,133 never smokers who had not been diagnosed with asthma.
Table 1.
Comparison of the Main Characteristics of Study Participants Who Did and Did Not Have Probable Post-traumatic Stress Disorder at Their Baseline Visit
| Variable | Entire Cohort (n = 11,481) |
Never Smokers, Never Diagnosed with Asthma (n = 6,133) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PTSD* |
No PTSD* |
P Value | PTSD* |
No PTSD* |
P Value | |||||
| n or Mean† | % or SD† | n or Mean† | % or SD† | n or Mean† | % or SD† | n or Mean† | % or SD† | |||
| Sex | ||||||||||
| Male | 1,526 | 80.0 | 8,143 | 85.1 | <0.001 | 674 | 76.9 | 4,486 | 85.3 | <0.001 |
| Female | 382 | 20.0 | 1,430 | 14.9 | 202 | 23.1 | 771 | 14.7 | ||
| Age | ||||||||||
| 20–29 yr | 107 | 5.6 | 464 | 4.9 | 0.16 | 57 | 6.5 | 267 | 5.1 | 0.08 |
| 30–39 yr | 555 | 29.1 | 3,395 | 35.5 | <0.001 | 282 | 32.2 | 2,050 | 39.0 | <0.001 |
| 40–49 yr | 734 | 38.5 | 3,893 | 40.7 | 0.07 | 324 | 37.0 | 2,158 | 41.1 | 0.02 |
| 50–59 yr | 409 | 21.4 | 1,442 | 15.1 | <0.001 | 180 | 20.6 | 647 | 12.3 | <0.001 |
| ≥60 yr | 103 | 5.4 | 379 | 4.0 | 0.004 | 33 | 3.8 | 135 | 2.6 | 0.04 |
| Race/ethnicity | ||||||||||
| Non-Latino white | 900 | 47.2 | 5,439 | 56.8 | <0.001 | 353 | 40.3 | 2,791 | 53.1 | <0.001 |
| Latino | 768 | 40.3 | 2,748 | 28.7 | <0.001 | 411 | 46.9 | 1,613 | 30.7 | <0.001 |
| Non-Latino African American | 199 | 10.4 | 1,183 | 12.4 | 0.02 | 90 | 10.3 | 729 | 13.9 | 0.004 |
| Non-Latino Asian | 28 | 1.5 | 141 | 1.5 | 0.99 | 16 | 1.8 | 87 | 1.7 | 0.71 |
| Other | 13 | 0.7 | 62 | 0.7 | 0.87 | 6 | 0.7 | 37 | 0.7 | 0.95 |
| Smoking history | ||||||||||
| Lifetime nonsmoker | 1,066 | 55.9 | 6,211 | 64.9 | <0.001 | 876 | 100 | 5,257 | 100 | — |
| Former smoker | 439 | 23.0 | 2,135 | 22.3 | 0.50 | — | — | — | — | |
| Current smoker | 403 | 21.1 | 1,227 | 12.8 | <0.001 | — | — | — | — | |
| Pack-years of smoking | 6.05 | 11.86 | 4.99 | 11.12 | <0.001 | — | — | — | — | — |
| World Trade Center occupational exposure | ||||||||||
| Low | 187 | 9.8 | 1,367 | 14.3 | <0.001 | 103 | 11.8 | 736 | 14.0 | 0.07 |
| Intermediate | 1330 | 69.7 | 6,215 | 64.9 | <0.001 | 597 | 68.2 | 3,382 | 64.3 | 0.03 |
| High | 391 | 20.5 | 1,991 | 20.8 | 0.76 | 176 | 20.1 | 1,139 | 21.7 | 0.29 |
| Educational level | ||||||||||
| No high school diploma | 312 | 16.4 | 628 | 6.6 | <0.001 | 155 | 17.7 | 286 | 5.4 | <0.001 |
| High school diploma | 549 | 28.8 | 2,092 | 21.9 | <0.001 | 228 | 26.0 | 1,005 | 19.1 | <0.001 |
| Some college | 657 | 34.4 | 3,954 | 41.3 | <0.001 | 298 | 34.0 | 2,177 | 41.4 | <0.001 |
| College graduate | 390 | 20.4 | 2,899 | 30.3 | <0.001 | 195 | 22.3 | 1,789 | 34.0 | <0.001 |
| BMI‡ | ||||||||||
| Normal | 345 | 18.1 | 1,564 | 16.3 | 0.06 | 147 | 16.8 | 846 | 16.1 | 0.61 |
| Overweight | 829 | 43.5 | 4,292 | 44.8 | 0.27 | 406 | 46.4 | 2,416 | 46.0 | 0.83 |
| Obese | 734 | 38.5 | 3,717 | 38.8 | 0.77 | 323 | 36.9 | 1995 | 38.0 | 0.54 |
| BDR§ | ||||||||||
| No | 1,737 | 91.0 | 8,960 | 93.6 | <0.001 | 816 | 93.2 | 5,020 | 95.5 | 0.003 |
| Yes | 171 | 9.0 | 613 | 6.4 | 60 | 6.9 | 237 | 4.5 | ||
| Ever asthma | ||||||||||
| No | 1,606 | 84.2 | 8,166 | 85.3 | 0.21 | 876 | 100 | 5,257 | 100 | — |
| Yes | 302 | 15.8 | 1,407 | 14.7 | 0 | 0 | 0 | 0 | ||
Definition of abbreviations: BDR = bronchodilator response; BMI = body mass index; PTSD = post-traumatic stress disorder.
Probable PTSD, based on PSTD Checklist score of 44 points or greater.
Values are shown as n and % for categorical variables and as mean and SD for continuous variables.
Normal, BMI = 18–24.9 kg/m2; overweight, BMI = 25–29.9 kg/m2; obese, BMI ≥ 30 kg/m2.
BDR defined as both a percent change of 12% or greater and an absolute increment of 200 ml or greater from baseline FEV1 after bronchodilator administration.
Tables 2 and 3 show the results of the unadjusted and adjusted logistic regression analysis of probable PTSD and BDR at the baseline study visit. Among all study participants (Table 2), probable PTSD was significantly associated with 1.44 times increased odds of having BDR. Similar results for probable PTSD were obtained in a multivariable analysis of BDR adjusting for age, sex, and other covariates (Table 2). In this multivariable analysis, Latino ethnicity was significantly associated with reduced odds of having BDR, whereas female sex, an age of 60 years or greater, and obesity were each significantly associated with increased odds of BDR. In both the unadjusted and multivariable analyses of probable PTSD and BDR among never smokers who had never been diagnosed with asthma (Table 3), probable PTSD was significantly associated with 1.56 times increased odds of having BDR. In this subgroup analysis, no other covariate was significantly associated with BDR.
Table 2.
Logistic Regression Analysis of Probable Post-traumatic Stress Disorder and Bronchodilator Response at the Baseline Study Visit in All Participants
| Variable | All Participants (n = 11,481) |
|||||||
|---|---|---|---|---|---|---|---|---|
| BDR* |
No BDR* |
Unadjusted |
Adjusted† |
|||||
| n or Mean‡ | % or SD‡ | n or Mean‡ | % or SD‡ | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Sex | ||||||||
| Male | 624 | 6.5% | 9,045 | 93.6% | 1.0 | 1.0 | ||
| Female | 160 | 8.8% | 1,652 | 91.2% | 1.40 (1.17–1.68) | <0.001 | 1.52 (1.25–1.84) | <0.001 |
| Age | ||||||||
| 20–29 yr | 38 | 6.7% | 533 | 93.4% | 1.0 | 1.0 | ||
| 30–39 yr | 246 | 6.2% | 3704 | 93.8% | 0.93 (0.65–1.33) | 0.69 | 0.89 (0.62–1.28) | 0.53 |
| 40–49 yr | 296 | 6.4% | 4,331 | 93.6% | 0.96 (0.68–1.36) | 0.81 | 0.86 (0.61–1.23) | 0.42 |
| 50–59 yr | 144 | 7.8% | 1,707 | 92.2% | 1.18 (0.82–1.71) | 0.37 | 1.02 (0.69–1.49) | 0.93 |
| ≥60 yr | 60 | 12.5% | 422 | 87.6% | 1.99 (1.30–3.05) | 0.002 | 1.70 (1.09–2.65) | 0.02 |
| Race or ethnicity | ||||||||
| Non-Latino White | 440 | 6.9% | 5,899 | 93.1% | 1.0 | 1.0 | ||
| Latino | 211 | 6.0% | 3,305 | 94.0% | 0.86 (0.72–1.01) | 0.07 | 0.82 (0.68–0.98) | 0.03 |
| Non-Latino African American | 111 | 8.0% | 1,271 | 92.0% | 1.17 (0.94–1.45) | 0.15 | 1.10 (0.88–1.38) | 0.41 |
| Non-Latino Asian | 13 | 7.7% | 156 | 92.3% | 1.12 (0.63–1.98) | 0.71 | 1.22 (0.69–2.18) | 0.5 |
| Other | 9 | 12.0% | 66 | 88.0% | 1.83 (0.91–3.69) | 0.09 | 1.82 (0.90–3.70) | 0.1 |
| Smoking status | ||||||||
| Lifetime nonsmoker | 476 | 6.5% | 6,801 | 93.5% | 1.0 | 1.0 | ||
| Former smoker | 206 | 8.0% | 2,368 | 92.0% | 1.24 (1.05–1.47) | 0.01 | 1.09 (0.89–1.33) | 0.39 |
| Current smoker | 102 | 6.3% | 1,528 | 93.7% | 0.95 (0.77–1.19) | 0.67 | 0.88 (0.68–1.14) | 0.34 |
| Pack-years of smoking | 6.07 | 12.61 | 5.10 | 11.15 | — | — | — | — |
| Per each pack-year | — | — | — | — | 1.01 (1.00–1.01) | 0.02 | 1.00 (1.0–1.01) | 0.31 |
| World Trade Center occupational exposure | ||||||||
| Low | 110 | 7.1% | 1,444 | 92.9% | 1.0 | 1.0 | ||
| Intermediate | 521 | 6.9% | 7,024 | 93.1% | 0.97 (0.79–1.21) | 0.81 | 0.98 (0.79–1.22) | 0.86 |
| High | 153 | 6.4% | 2,229 | 93.6% | 0.90 (0.70–1.16) | 0.42 | 0.91 (0.70–1.17) | 0.45 |
| Educational level | ||||||||
| No high school diploma | 66 | 7.0% | 874 | 93.0% | 1.0 | 1.0 | ||
| High school diploma | 178 | 6.7% | 2,463 | 93.3% | 0.96 (0.71–1.28) | 0.77 | 0.99 (0.73–1.33) | 0.93 |
| Some college | 321 | 7.0% | 4,290 | 93.0% | 0.99 (0.75–1.30) | 0.95 | 1.04 (0.78–1.39) | 0.77 |
| College graduate | 219 | 6.6% | 3,070 | 93.3% | 0.95 (0.71–1.26) | 0.7 | 0.97 (0.72–1.31) | 0.85 |
| BMI§ | ||||||||
| Normal | 118 | 6.2% | 1791 | 93.8% | 1.0 | 1.0 | ||
| Overweight | 330 | 6.4% | 4,791 | 93.6% | 1.05 (0.84–1.30) | 0.69 | 1.17 (0.94–1.47) | 0.17 |
| Obese | 336 | 7.6% | 4,115 | 92.5% | 1.24 (1.0–1.54) | 0.05 | 1.38 (1.10–1.73) | 0.005 |
| Probable PTSD|| | ||||||||
| No | 613 | 6.4% | 8960 | 93.6% | 1.0 | 1.0 | ||
| Yes | 171 | 9.0% | 1,737 | 91.0% | 1.44 (1.21–1.72) | <0.001 | 1.43 (1.19–1.72) | <0.001 |
Definition of abbreviations: BDR = bronchodilator response; BMI = body mass index; CI = confidence interval; OR = odds ratio; PTSD = post-traumatic stress disorder.
BDR defined as both a percent change of 12% or greater and an absolute increment of 200 ml or greater from baseline FEV1 after bronchodilator administration.
Multivariable model adjusted for all covariates in the corresponding table column.
Values are shown as n and % for categorical variables and as mean and SD for continuous variables.
Normal, BMI = 18–24.9 kg/m2; overweight, BMI = 25–29.9 kg/m2; obese, BMI ≥ 30 kg/m2.
Probable PTSD, based on PSTD Checklist score of 44 points or greater.
Table 3.
Logistic Regression Analysis of Probable Post-traumatic Stress Disorder and Bronchodilator Response at the Baseline Study Visit in the Subgroup of Never Smokers Never Diagnosed with Asthma
| Variable | Never Smokers Never Diagnosed with Asthma (n = 6,133) |
|||||||
|---|---|---|---|---|---|---|---|---|
| BDR* |
No BDR* |
Unadjusted |
Adjusted† |
|||||
| n | % | n | % | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Sex | ||||||||
| Male | 238 | 4.6 | 4,922 | 95.4 | 1 | 1 | ||
| Female | 59 | 6.1 | 914 | 93.9 | 1.34 (1.0–1.79) | 0.05 | 1.35 (0.99–1.85) | 0.06 |
| Age | ||||||||
| 20–29 yr | 15 | 4.6 | 309 | 95.4 | 1 | 1 | ||
| 30–39 yr | 119 | 5.1 | 2,213 | 94.9 | 1.11 (0.64–1.92) | 0.72 | 1.09 (0.62–1.90) | 0.76 |
| 40–49 yr | 101 | 4.1 | 2,381 | 95.9 | 0.87 (0.50–1.52) | 0.63 | 0.82 (0.47–1.44) | 0.49 |
| 50–59 yr | 49 | 5.9 | 778 | 94.1 | 1.30 (0.72–2.35) | 0.39 | 1.15 (0.63–2.10) | 0.66 |
| ≥60 yr | 13 | 7.7 | 155 | 92.3 | 1.73 (0.80–3.72) | 0.16 | 1.49 (0.68–3.24) | 0.32 |
| Race or ethnicity | ||||||||
| Non-Latino white | 151 | 4.8 | 2,993 | 95.2 | 1 | 1 | ||
| Latino | 84 | 4.2 | 1,940 | 95.9 | 0.86 (0.65–1.13) | 0.27 | 0.76 (0.57–1.02) | 0.07 |
| Non-Latino African American | 52 | 6.4 | 767 | 93.7 | 1.34 (0.97–1.86) | 0.07 | 1.29 (0.93–1.80) | 0.13 |
| Non-Latino Asian | 7 | 6.8 | 96 | 93.2 | 1.45 (0.66–3.17) | 0.36 | 1.46 (0.66–3.22) | 0.35 |
| Other | 3 | 7.0 | 40 | 93.0 | 1.49 (0.46–4.86) | 0.51 | 1.48 (0.45–4.87) | 0.52 |
| Smoking status | ||||||||
| Lifetime nonsmoker | 297 | 4.8 | 5,836 | 95.2 | — | — | — | — |
| World Trade Center occupational exposure | ||||||||
| Low | 51 | 6.1 | 788 | 93.9 | 1 | 1 | ||
| Intermediate | 188 | 4.7 | 3,791 | 95.3 | 0.77 (0.56–1.05) | 0.1 | 0.77 (0.56–1.06) | 0.11 |
| High | 58 | 4.4 | 1,257 | 95.6 | 0.71 (0.48–1.05) | 0.09 | 0.71 (0.48–1.05) | 0.08 |
| Educational level | ||||||||
| No high school diploma | 25 | 5.7 | 416 | 94.3 | 1 | 1 | ||
| High school diploma | 58 | 4.7 | 1,175 | 95.3 | 0.82 (0.51–1.33) | 0.42 | 0.86 (0.52–1.42) | 0.56 |
| Some college | 117 | 4.7 | 2,358 | 95.3 | 0.83 (0.53–1.29) | 0.4 | 0.85 (0.53–1.37) | 0.51 |
| College graduate | 97 | 4.9 | 1,887 | 95.1 | 0.86 (0.54–1.34) | 0.5 | 0.86 (0.53–1.39) | 0.54 |
| BMI‡ | ||||||||
| Normal | 46 | 4.6 | 947 | 95.4 | 1 | 1 | ||
| Overweight | 136 | 4.8 | 2,686 | 95.2 | 1.04 (0.74–1.47) | 0.81 | 1.15 (0.81–1.64) | 0.43 |
| Obese | 115 | 5.0 | 2,203 | 95.0 | 1.08 (0.76–1.53) | 0.69 | 1.19 (0.83–1.71) | 0.34 |
| Probable PTSD§ | ||||||||
| No | 237 | 4.5 | 5,020 | 95.5 | 1 | 1 | ||
| Yes | 60 | 6.9 | 816 | 93.2 | 1.56 (1.16–2.09) | 0.003 | 1.56 (1.15–2.11) | 0.005 |
For definition of abbreviations, see Table 2.
BDR defined as both a percent change of 12% or greater and an absolute increment of 200 ml or greater from baseline FEV1 after bronchodilator administration.
Multivariable model adjusted for all covariates in the corresponding table column.
Normal, BMI = 18–24.9 kg/m2; overweight, BMI = 25–29.9 kg/m2; obese, BMI ≥ 30 kg/m2.
Probable PTSD, based on PSTD Checklist score of 44 points or greater.
We were then interested in examining the relationship between probable PTSD at baseline and incident asthma at the follow-up visit. To minimize confounding by cigarette smoking or inclusion of subjects with pre-existing asthma, this analysis was restricted to never smokers who had no asthma diagnosis at the baseline study visit. Of these 6,133 subjects, 3,757 (61.3%) completed the follow-up visit. Compared with subjects who did not complete the follow-up visit, those who did were significantly more likely to be aged 50–59 years and to be non-Latino Asian, but less likely to be 20–29 years old or to have a low level of WTC occupational exposure (Table E2). There were no significant differences in sex, race/ethnicity other than non-Latino Asian, BDR, or PTSD between subjects who did and did not complete the follow-up visit.
Among the 3,757 subjects who completed the follow-up visit, the time interval elapsed since the baseline visit (as mean [SD]) was not significantly different between those who did (n = 553) and did not (n = 3,204) have probable PTSD at baseline (4.94 [1.73] yr versus 4.94 [1.84] yr, P for comparison = 0.80). In these 3,757 subjects, the time interval between visits was slightly, but significantly, different between subjects who did (n = 374) and did not (n = 3,383) develop incident asthma (5.17 [1.80] yr versus 4.92 [1.83] yr, P = 0.02).
Table 4 shows the results of the logistic regression analysis of probable PTSD at baseline and incident asthma in 3,757 never smokers. In the unadjusted analysis, probable PTSD at baseline was significantly associated with 2.64 times increased odds of incident asthma. After adjustment for age, sex, and other covariates, probable PTSD remained significantly associated with 2.41 times increased odds of incident asthma. In this multivariable analysis, baseline BDR was significantly associated with 3.13 increased odds of incident asthma. As expected, a repeat multivariable analysis after additional adjustment for the time interval elapsed between study visits yielded nearly identical results (data not shown).
Table 4.
Logistic Regression Analysis of Probable Post-traumatic Stress Disorder at Baseline and Incident Asthma by the Follow-up Visit among Never Smokers without a Previous Diagnosis of Asthma
| Variable | Never Smokers Not Diagnosed with Asthma at the Baseline Visit (n = 3,757) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Asthma |
No Asthma |
Unadjusted |
Adjusted* |
|||||
| n | % | n | % | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Sex | ||||||||
| Male | 297 | 9.4 | 2,853 | 90.6 | 1.0 | 1.0 | ||
| Female | 77 | 12.7 | 530 | 87.3 | 1.40 (1.07–1.82) | 0.01 | 1.38 (1.03–1.85) | 0.03 |
| Age | ||||||||
| 20–29 yr | 21 | 11.7 | 158 | 88.3 | 1.0 | 1.0 | ||
| 30–39 yr | 136 | 9.7 | 1,262 | 90.3 | 0.81 (0.50–1.32) | 0.4 | 0.86 (0.52–1.42) | 0.55 |
| 40–49 yr | 146 | 9.5 | 1,396 | 90.5 | 0.79 (0.48–1.28) | 0.33 | 0.81 (0.49–1.35) | 0.42 |
| 50–59 yr | 56 | 10.4 | 481 | 89.6 | 0.88 (0.51–1.49) | 0.63 | 0.80 (0.46–1.39) | 0.42 |
| ≥60 yr | 15 | 14.9 | 86 | 85.2 | 1.31 (0.64–2.68) | 0.45 | 1.21 (0.58–2.56) | 0.61 |
| Race/ethnicity | ||||||||
| Non-Latino white | 193 | 10.0 | 1,729 | 90.0 | 1.0 | 1.0 | ||
| Latino | 129 | 10.5 | 1,096 | 89.5 | 1.05 (0.83–1.33) | 0.66 | 0.89 (0.69–1.16) | 0.39 |
| Non-Latino African American | 35 | 6.9 | 474 | 93.1 | 0.66 (0.46–0.96) | 0.03 | 0.62 (0.42–0.91) | 0.01 |
| Non-Latino Asian | 9 | 12.3 | 64 | 87.7 | 1.26 (0.62–2.57) | 0.53 | 1.32 (0.63–2.74) | 0.46 |
| Other | 8 | 28.6 | 20 | 71.4 | 3.59 (1.56–8.25) | 0.003 | 3.58 (1.52–8.46) | 0.004 |
| World Trade Center occupational exposure | ||||||||
| Low | 40 | 8.4 | 438 | 91.6 | 1.0 | 1.0 | ||
| Intermediate | 253 | 10.3 | 2,214 | 89.7 | 1.25 (0.88–1.77) | 0.21 | 1.21 (0.85–1.73) | 0.3 |
| High | 81 | 10.0 | 731 | 90.0 | 1.21 (0.82–1.80) | 0.34 | 1.21 (0.81–1.82) | 0.36 |
| Educational level | ||||||||
| No high school diploma | 38 | 13.3 | 247 | 86.7 | 1.0 | 1.0 | ||
| High school diploma | 89 | 11.7 | 675 | 88.4 | 0.86 (0.57–1.29) | 0.46 | 1.03 (0.67–1.60) | 0.88 |
| Some college | 131 | 9.0 | 1,322 | 91.0 | 0.64 (0.44–0.95) | 0.03 | 0.85 (0.56–1.30) | 0.46 |
| College graduate | 116 | 9.2 | 1,139 | 90.8 | 0.66 (0.45–0.98) | 0.04 | 0.86 (0.56–1.33) | 0.49 |
| BMI† | ||||||||
| Normal | 58 | 9.3 | 568 | 90.7 | 1.0 | 1.0 | ||
| Overweight | 165 | 9.3 | 1,614 | 90.7 | 1.00 (0.73–1.37) | 0.99 | 1.10 (0.79–1.54) | 0.56 |
| Obese | 151 | 11.2 | 1,201 | 88.8 | 1.23 (0.90–1.69) | 0.2 | 1.42 (1.01–2.00) | 0.04 |
| Weight gain | ||||||||
| ≤−2.5 kg | 67 | 8.7 | 703 | 91.3 | 1.0 | 1.0 | ||
| −2.5 to 0 kg | 78 | 10.3 | 679 | 89.7 | 1.21 (0.86–1.70) | 0.29 | 1.33 (0.93–1.89) | 0.12 |
| 0–2.5 kg | 67 | 8.8 | 694 | 91.2 | 1.01 (0.71–1.44) | 0.94 | 1.06 (0.74–1.53) | 0.76 |
| 2.5–5 kg | 79 | 11.6 | 602 | 88.4 | 1.38 (0.98–1.94) | 0.07 | 1.42 (0.99–2.02) | 0.05 |
| >5 kg | 83 | 10.5 | 705 | 89.5 | 1.24 (0.88–1.73) | 0.22 | 1.23 (0.87–1.75) | 0.24 |
| BDR‡ | ||||||||
| No | 325 | 9.1 | 3,237 | 90.9 | 1.0 | 1.0 | ||
| Yes | 49 | 25.1 | 146 | 74.9 | 3.34 (2.37–4.71) | <0.001 | 3.13 (2.20–4.46) | <0.001 |
| Probable PTSD§ | ||||||||
| No | 267 | 8.3 | 2,937 | 91.7 | 1.0 | 1.0 | ||
| Yes | 107 | 19.4 | 446 | 80.7 | 2.64 (2.07–3.37) | <0.001 | 2.41 (1.85–3.13) | <0.001 |
For definition of abbreviations, see Table 2.
Adjusted for all covariates in the corresponding column.
Normal, BMI = 18–24.9 kg/m2; overweight, BMI = 25–29.9 kg/m2; obese, BMI ≥ 30 kg/m2.
BDR defined as both a percent change of 12% or greater and an absolute increment of 200 ml or greater from baseline FEV1 after bronchodilator administration.
Probable PTSD, based on PSTD Checklist score of 44 points or greater.
We found no significant modification of the estimated effect of baseline PTSD on incident asthma by baseline BDR or WTC occupational exposure (P for interaction ≥ 0.21 in both instances). Although there was no significant modification of the estimated effect of baseline PTSD on incident asthma by baseline BDR, we repeated the multivariable analysis shown in Table 4 after excluding 195 subjects with BDR at the baseline study visit to further exclude possibly undiagnosed asthma at baseline. In this confirmatory analysis, probable PTSD remained significantly associated with incident asthma (odds ratio [OR] = 2.58; 95% confidence interval [CI] = 1.96–3.41; P < 0.001).
In a secondary analysis, we examined probable PTSD trajectories and incident asthma between the baseline and follow-up visits (Table E3). In a multivariable analysis, both late-onset (OR = 3.07; 95% CI = 2.18–4.31; P < 0.001) and chronic (OR = 4.18; 95% CI = 3.06–5.72; P < 0.001) probable PTSD were significantly associated with incident asthma. In this analysis, recovering probable PTSD was not significantly associated with incident asthma (OR = 1.34; 95% CI = 0.81–2.23; P = 0.26).
Discussion
A cross-sectional analysis previously showed an association between probable PTSD and self-reported physician-diagnosed asthma among New York community dwellers and WTC rescue and recovery workers (6). In this cohort of WTC workers, PTSD has also been associated with self-reported incident lower respiratory symptoms during follow up (13). To our knowledge, however, this is the first report of an association between probable PTSD and either BDR or incident (new-onset) asthma. Our findings suggest that PTSD leads to both clinically significant BDR (a marker of clinical and subclinical asthma) and incident physician-diagnosed asthma among adults exposed to a severe traumatic event, such as the WTC terrorist attack or the subsequent rescue and recovery tasks at the disaster site.
Unlike results from previous cross-sectional studies (5–7), “reverse causation” (e.g., asthma leading to PTSD symptoms) is an improbable explanation for our findings for incident asthma, as this analysis was first conducted after excluding subjects who had a pre-existing asthma diagnosis at baseline, and then repeated after further exclusion of subjects with clinically significant BDR at baseline, obtaining very similar results. Although undiagnosed asthma is still possible among subjects who had neither an asthma diagnosis nor BDR at baseline, this would likely cause a small degree of misclassification, without a major effect on our overall results.
Confounding by cigarette smoking is also an unlikely explanation for our findings on asthma or BDR, as our findings were similar after either adjusting for smoking or excluding former or current smokers from multivariable analyses. Although we cannot exclude residual confounding by WTC occupational exposure, this is improbable as the sole or major explanation for our results, because the proportion of subjects who did and did not have high WTC occupational exposure was very similar between those with and those without probable PTSD at baseline (Table 1). Moreover, all multivariable analyses were adjusted for WTC occupational exposure, and we obtained nearly identical results in a confirmatory analysis using four instead of three levels of occupational exposure (see Methods [and data not shown]). Selection bias due to differential loss of follow-up (related to both PTSD and asthma) is a possible, but improbable, cause for our results for incident asthma, as there was no significant difference in either probable PTSD or BDR at baseline between never smokers with and without complete follow-up data. Although subjects who were included in the cross-sectional analysis of BDR at the baseline study visit (n = 11,481) had lower prevalence of PTSD or BDR than those excluded (n = 7,513), this difference would probably ameliorate the observed association between probable PTSD and BDR. Increased disease detection among subjects with probable PTSD (due to more frequent contact with the healthcare system, if subjects with PTSD symptoms in the PCL questionnaire were ultimately diagnosed with PTSD) may partly explain our results for asthma. However, the association between probable PTSD at baseline and incident asthma persisted after excluding subjects with baseline BDR (who may have had subclinical asthma and thus be more likely to be diagnosed with asthma as a result of frequent healthcare visits) from the analysis. Thus, our findings strongly suggest that PTSD leads to both BDR and asthma among rescue and recovery workers exposed to the WTC disaster.
The biologic mechanisms linking PTSD to asthma are insufficiently characterized (2). Hyperventilation, often present in individuals with anxiety, could cause cooling and osmotic change in the bronchial epithelium, leading to increased airway responsiveness. Alternatively, PTSD may cause dysregulation of the hypothalamic pituitary axis and the sympathetic–adrenal–medullary system, ultimately leading to abnormal immune responses and increased airway inflammation (14). Chronic stress can alter systemic levels of glucocorticoids and catecholamines (15), which may change effector functions of macrophages and lymphocytes, with downstream implications for immune responses (16), reactivity to asthma triggers, airway inflammation, and airflow obstruction (17, 18). Recent findings further suggest that anxiety-related disorders, such as PTSD, may affect asthma by altering expression of disease-susceptibility genes through gene-by-stress interactions or epigenetic mechanisms (14, 19).
We recognize several limitations of our findings. First, we lacked information on potential confounders or modifiers of the estimated effect of PTSD on incident asthma, including other mental illnesses, family history of asthma, atopy, environmental exposures other than tobacco use or WTC dust, and history of childhood abuse (20). Moreover, we had limited statistical power to examine modification of the estimated effect of probable PTSD at baseline on incident asthma by baseline BDR. Second, we lacked BDR data for the follow-up visit, which would have further supported a diagnosis of incident asthma. However, BDR at the baseline study visit was associated with incident asthma among never smokers, which strengthens our confidence in the accuracy of the diagnosis. Third, we did not have information about a clinical diagnosis of PTSD, and thus had to use information about probable PTSD based on self-reported symptoms in a standardized questionnaire (the PCL). However, the PCL score used to identify WTC workers with probable PTSD has been validated against clinical PTSD, and the PCL scale has robust psychometric properties and excellent diagnostic accuracy (including high sensitivity, high specificity, and high positive predictive value) (2). Moreover, findings from our secondary analysis of trajectories of probable PTSD further suggest a causal relationship, given that the magnitude of the association between late-onset or chronic probable PTSD and incident asthma was greater than that between recovering probable PTSD and incident asthma.
In summary, probable PTSD is associated with both clinically significant BDR and incident asthma among WTC rescue and recovery workers and volunteers. This finding strongly supports an expanding body of literature linking stress-related disorders, such as PTSD, to the pathogenesis of asthma (14, 21), and suggests that physicians treating adults with PTSD should be aware of their potentially increased risk of asthma. Whether treatment of PTSD prevents or helps treat asthma is unknown, but merits examination in future studies.
Acknowledgments
Acknowledgment
The authors thank all participants in this study, and the staff of the Mount Sinai World Trade Center Health Program Clinical Center of Excellence (director, Michael Crane, M.D.), and Data Center (director, Roberto Lucchini, M.D.) (New York, NY).
Footnotes
Supported by Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (CDC/NIOSH) contracts 200-2011-39377 and 200-2011-39356, by CDC/NIOSH grant U01-OH040701 (R.E.D.), and by National Institutes of Health grant HL117191 and funds from the Heinz Endowments (J.C.C.).
The contents of this article are the sole responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health.
Author Contributions: Study conception and design—R.E.D. and J.C.C.; acquisition, analysis, or interpretation of data—all authors; critical revision for important intellectual content—all authors; statistical analysis—Y.J., R.E.D., and J.C.C.; obtained funding—R.E.D. and J.C.C; administrative, technical, or material support—G.E.M. and J.P.W.; study supervision—R.E.D. and J.C.C; all authors approved the final version of the manuscript before submission.
Originally Published in Press as DOI: 10.1164/rccm.201605-1067OC on August 22, 2016
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, Liu X. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. 2012;(94):1–8. [PubMed] [Google Scholar]
- 2.Brackbill RM, Hadler JL, DiGrande L, Ekenga CC, Farfel MR, Friedman S, Perlman SE, Stellman SD, Walker DJ, Wu D, et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA. 2009;302:502–516. doi: 10.1001/jama.2009.1121. [DOI] [PubMed] [Google Scholar]
- 3.de la Hoz RE, Shohet MR, Chasan R, Bienenfeld LA, Afilaka AA, Levin SM, Herbert R. Occupational toxicant inhalation injury: the World Trade Center (WTC) experience. Int Arch Occup Environ Health. 2008;81:479–485. doi: 10.1007/s00420-007-0240-x. [DOI] [PubMed] [Google Scholar]
- 4.Wisnivesky JP, Teitelbaum SL, Todd AC, Boffetta P, Crane M, Crowley L, de la Hoz RE, Dellenbaugh C, Harrison D, Herbert R, et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet. 2011;378:888–897. doi: 10.1016/S0140-6736(11)61180-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright RJ, Fay ME, Suglia SF, Clark CJ, Evans JS, Dockery DW, Behbehani J. War-related stressors are associated with asthma risk among older Kuwaitis following the 1990 Iraqi invasion and occupation. J Epidemiol Community Health. 2010;64:630–635. doi: 10.1136/jech.2009.090795. [DOI] [PubMed] [Google Scholar]
- 6.Shiratori Y, Samuelson KW. Relationship between posttraumatic stress disorder and asthma among New York area residents exposed to the World Trade Center disaster. J Psychosom Res. 2012;73:122–125. doi: 10.1016/j.jpsychores.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Spitzer C, Koch B, Grabe HJ, Ewert R, Barnow S, Felix SB, Ittermann T, Obst A, Völzke H, Gläser S, et al. Association of airflow limitation with trauma exposure and post-traumatic stress disorder. Eur Respir J. 2011;37:1068–1075. doi: 10.1183/09031936.00028010. [DOI] [PubMed] [Google Scholar]
- 8.Szema AM, Peters MC, Weissinger KM, Gagliano CA, Chen JJ. New-onset asthma among soldiers serving in Iraq and Afghanistan. Allergy Asthma Proc. 2010;31:67–71. doi: 10.2500/aap.2010.31.3383. [DOI] [PubMed] [Google Scholar]
- 9.Herbert R, Moline J, Skloot G, Metzger K, Baron S, Luft B, Markowitz S, Udasin I, Harrison D, Stein D, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114:1853–1858. doi: 10.1289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 11.Adams RE, Boscarino JA. Predictors of PTSD and delayed PTSD after disaster: the impact of exposure and psychosocial resources. J Nerv Ment Dis. 2006;194:485–493. doi: 10.1097/01.nmd.0000228503.95503.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Thoracic Society. Standardization of spirometry, 1994 update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 13.Kotov R, Bromet EJ, Schechter C, Broihier J, Feder A, Friedman-Jimenez G, Gonzalez A, Guerrera K, Kaplan J, Moline J, et al. Posttraumatic stress disorder and the risk of respiratory problems in World Trade Center responders: longitudinal test of a pathway. Psychosom Med. 2015;77:438–448. doi: 10.1097/PSY.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg SL, Miller GE, Brehm JM, Celedón JC. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J Allergy Clin Immunol. 2014;134:1009–1015. doi: 10.1016/j.jaci.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5:243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 16.Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nat Rev Immunol. 2011;11:625–632. doi: 10.1038/nri3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen E, Miller GE. Stress and inflammation in exacerbations of asthma. Brain Behav Immun. 2007;21:993–999. doi: 10.1016/j.bbi.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005;5:23–29. doi: 10.1097/00130832-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Chen W, Boutaoui N, Brehm JM, Han YY, Schmitz C, Cressley A, Acosta-Pérez E, Alvarez M, Colón-Semidey A, Baccarelli AA, et al. ADCYAP1R1 and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2013;187:584–588. doi: 10.1164/rccm.201210-1789OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen RT, Canino GJ, Bird HR, Celedón JC. Violence, abuse, and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2008;178:453–459. doi: 10.1164/rccm.200711-1629OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yonas MA, Lange NE, Celedón JC. Psychosocial stress and asthma morbidity. Curr Opin Allergy Clin Immunol. 2012;12:202–210. doi: 10.1097/ACI.0b013e32835090c9. [DOI] [PMC free article] [PubMed] [Google Scholar]