Introduction
Phaeohyphomycosis is a rare, opportunistic infection caused by melanized fungi that predominates in tropical climates.1, 2 The increase in the number of organ transplant recipients (OTRs), in conjunction with improvement in their long-term treatment, has led to an increase in the incidence of phaeohyphomycosis.1, 3, 4, 5, 6, 7 Phaeohyphomycosis has a wide range of clinical presentations, which are associated with the immune status of the host.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 We describe 7 cases of phaeohyphomycosis in OTRs, which clearly demonstrate that the clinical presentations can have profound variations and that treating this infection in this specific patient population can be challenging.
Materials and methods
We present a case series of 7 OTRs with phaeohyphomycosis that have been followed up with our specialized dermatologic clinic for more than 4 years. Their clinical presentations and treatment approaches are discussed. Table I summarizes the findings.
Table I.
Summary of demographics, diagnosis, treatment, and outcome for the 7 cases presented
| Sex, age | Occupation | Organ, time after transplant | Immunosuppressive medications | Clinical presentation, location | Diagnosis | Treatment | Outcome (period of follow-up) | |
|---|---|---|---|---|---|---|---|---|
| 1 | Male, 57 | Farmer | Kidney, 2 y | AZA, TACR, PDN | Sporotrichoid nodules, right leg | DE, culture, HP, stain | Surgery + itraconazole 6 mo | No relapse (6 mo) |
| 2 | Male, 59 | Gardener | Kidney, 18 mo | MMF, TACR, PDN | Plaque, right thigh | DE, culture, stain | Surgery + itraconazole 4 mo | No relapse (2 y) |
| 3 | Male, 43 | Rural worker | Heart, 2 y | MMF, CCP, PDN | Nodule, left knee | DE, culture, HP | Surgery + itraconazole 2 mo | No relapse (2 y) |
| 4 | Female, 64 | Maid | Heart, 9 mo | CCP, MMF, PDN | Nodule, right elbow | DE, culture, HP, stain | Surgery | No relapse (2 y) |
| 5 | Male, 42 | Retired policeman | Heart, 11 mo | MMF, TACR, PDN | Tumor, right leg | DE, culture, HP, stain | Surgery + itraconazole 4 mo | No relapse (2 y) |
| 6 | Female, 34 | Hair stylist | Kidney, 10 mo | TACR, MMF, PDN | Plaque, right foot | DE, culture, HP, stain | Refused | Lost to follow-up |
| 7 | Male, 43 | Mason | Heart, 16 mo | MMF, TACR, PDN | Plaque, right leg and left hand | DE, Culture, HP | Surgery + itraconazole 6 mo | No relapse (2 y) |
AZA, Azathioprine; CCP, cyclosporine; DE, direct exam; HP, histopathology; MMF, mycophenolate mofetil; PDN, prednisone; TACR, tacrolimus.
Results
Case 1
A 57-year-old male farmer presented with multiples nodules with a sporotrichoid pattern on his lower right limb that developed 2 years after kidney transplantation (Fig 1). There were no signs of systemic symptoms. His immunosuppressive medications included azathioprine, tacrolimus, and prednisone. A direct examination found dematiaceous filamentous fungi, and culture yielded Exophiala sp. Histopathologic analysis found granulomatous dermatitis, and fungal melanized structures were seen through Fontana-Masson stain. Imaging studies ruled out internal foci of infection. He was initially treated with 200 mg twice a day of voriconazole, which was discontinued very soon because of severe hyponatremia. Itraconazole, 200 mg twice a day was started afterwards, which was accompanied by severe headache, anorexia, and weight loss. After reducing the tacrolimus dose, the symptoms gradually resolved. The lesions were surgically removed. Itraconazole was continued for 6 months, and no relapse has occurred so far.
Fig 1.
Phaeohyphomycosis: clinical aspect of case 1.
Case 2
A 59-year-old male gardener presented with an erythematous violaceous plaque on his right thigh that developed 18 months after kidney transplantation (Fig 2). His immunosuppressive medications included mycophenolate mofetil, tacrolimus, and prednisone. Direct examination of the biopsy specimen found several melanized septate hyphae. Microscopic examination of the fungal colony identified Exophiala sp. The biopsy specimen underwent Fontana-Masson and Gridley stains, which also confirmed the diagnosis of phaeohyphomycosis. Treatment included surgical removal of the lesion along with 200 mg twice a day of itraconazole for 4 months. There was no recurrence 2 years after completion of the treatment.
Fig 2.

Phaeohyphomycosis: clinical aspect of case 2.
Case 3
A 43-year-old male rural worker presented with a nodule over his left knee that evolved 2 years after cardiac transplantation. His immunosuppressive medications included mycophenolate mofetil, cyclosporine, and prednisone. Direct microscopy examination of the biopsy specimen found dematiaceous hyphae, and microscopic examination of fungal colony found Exophiala sp (Fig 3, A and B). The histopathology findings showed neutrophilic infiltrate and giant cells with dematiaceous hyphae. The patient was treated with surgical excision followed by itraconazole, 200 mg/d orally for 2 months. He has been undergoing follow-up for more than 2 years without recurrence.
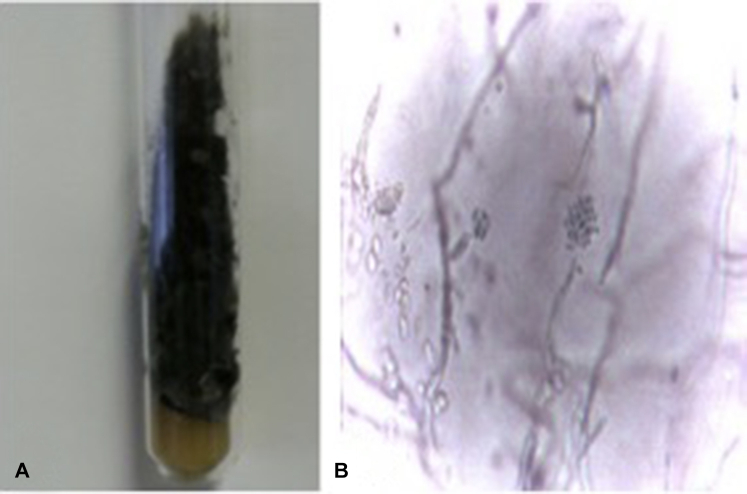
Fig 3.
Phaeohyphomycosis: macroscopic (A) and microscopic (B) aspects of the culture for case 3.
Case 4
A 64-year-old female maid presented an asymptomatic nodule on her right elbow that had grown 9 months after cardiac transplantation. There was no history of local trauma. Her immunosuppressive medications included cyclosporine, mycophenolate mofetil, and prednisone. The lesion was surgically removed. Direct microscopy examination of the biopsy specimen found dematiaceous hyphae, and microscopic analysis of fungal culture showed Exophiala sp. The histopathologic examination found granulomatous inflammatory infiltrate with multinucleated giant cells (Fig 4). Filamentous fungi were seen through Grocott stain (Fig 5). She has undergone follow-up for more than 2 years without recurrence.
Fig 4.
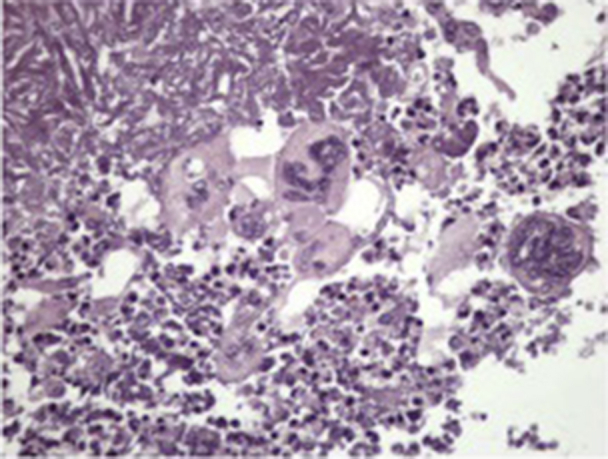
Phaeohyphomycosis: histopathologic aspects of case 4. (Original magnification: ×40.)
Fig 5.
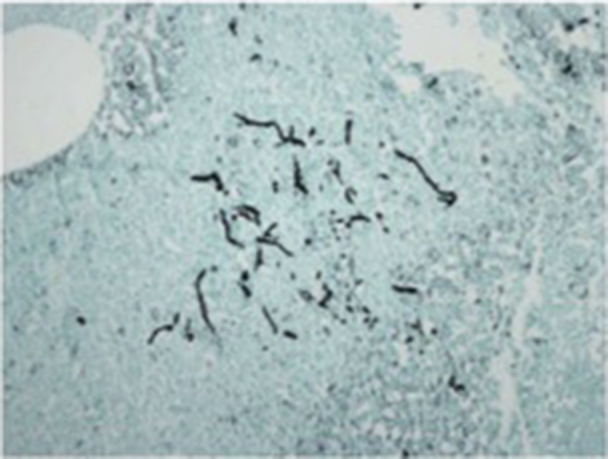
Phaeohyphomycosis: Grocott stain in case 4. (Original magnification: ×40.)
Case 5
A 42-year-old male retired policeman presented with an asymptomatic hyperkeratotic tumor on his right leg that evolved 11 months after cardiac transplantation. His immunosuppressive medications included mycophenolate mofetil, tacrolimus, and prednisone. Direct microscopy of the biopsy specimen found dematiaceous filamentous fungi (Fig 6), and fungal culture yielded Exophiala sp. Histopathology found a cystic structure with multinucleate giant cells, and dematiaceous filamentous fungi were seen on Fontana-Masson stain. Surgical excision was performed. Itraconazole, 200 mg twice a day, was started before surgery and maintained for 4 months. He has undergone follow-up for more than 2 years without recurrence.
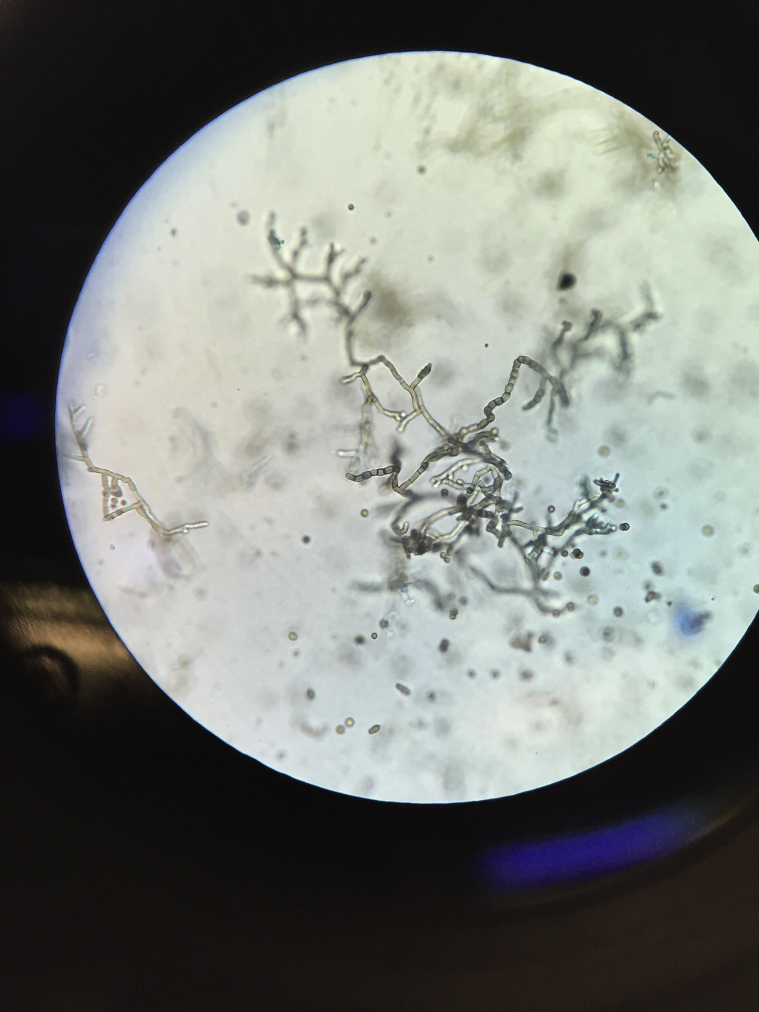
Fig 6.
Phaeohyphomycosis: direct microscopy in case 5. (Original magnification: ×20.)
Case 6
A 34-year-old female hair stylist presented with a verrucous plaque between her first and second right toes that had grown 10 months after kidney transplantation (Fig 7). Her immunosuppressive medications included tacrolimus, mycophenolate mofetil, and prednisone. Direct examination of the biopsy specimen found dematiaceous filamentous fungi, and microscopic study of culture found Exophiala sp. Histopathologic analysis found inflammatory infiltrate with multinucleated giant cells. Dematiaceous hyphae were seen through Fontana-Masson stain. The patient refused treatment and became lost to follow-up.
Fig 7.

Phaeohyphomycosis: clinical aspect of case 6.
Case 7
A 43-year-old male mason presented with asymptomatic erythematous plaques on his right leg and on the index finger of his left hand that had grown 16 months after cardiac transplantation (Fig 8). His immunosuppressive medications included mycophenolate mofetil, tacrolimus, and prednisone. Direct examination of the biopsy specimens found dematiaceous fungi, and microscopic analysis of culture found Exophiala sp. Histology confirmed the presence of fungal structures along with a granulomatous reaction. All lesions were surgically removed. In addition, the patient was treated with 200 mg twice a day itraconazole for 6 months, which had started just before surgery. The tacrolimus dose was adjusted accordingly. He has undergone follow-up for more than 2 years without recurrence.
Fig 8.

Phaeohyphomycosis: clinical aspect of case 7.
Conclusions
Phaeohyphomycosis is a group of rare opportunistic fungal infections predominantly affecting the skin, although systemic disease can occur.1, 2, 3, 4 The incidence of phaeohyphomycosis in OTR is approximately 9%, and disease usually occurs in the first few years after transplant.1, 2, 8 Phaeohyphomycosis developed in all of our patients within the first 2 years after transplant.
The incidence of phaeohyphomycosis seems to be increasing as a result of increasing numbers of OTRs and scientific advances made in immunosuppressant medications.4, 5, 6, 8 Regarding the specific immunosuppressant drug, it seems that calcineurin inhibitors such as tacrolimus are more associated with greater susceptibility to fungal infections, which later can become recurrent.1, 4, 5, 7 All of our patients were taking this medication.
Although it has been published that phaeohyphomycosis is more frequent in kidney transplant recipients,1, 4, 6, 7, 8, 10 we did not find a statistical difference between kidney and heart transplants in our series. This finding may be owing to the limited number of patients. However, we stress that all patients, regardless of the type of organ received, were under heavy immunosuppressive therapy.
Diagnosis of phaeohyphomycosis is complicated by its highly variable clinical presentation.1, 2, 3, 4, 5, 6, 7 In our patients, the diagnosis was based on clinical, microbiologic, and histopathologic studies. We observed a wide spectrum of clinical lesions including nodules, cysts, tumors, and verrucous plaques, mostly with subcutaneous involvement. The diversity of lesions presented in this series may reflect the differences in disease progression, variable host response, and degree of the immunosuppression.
Despite that there are more than 100 species of fungi associated with this disease, there is still no correlation between the etiologic agent and morphology of lesions.3, 7, 8 Exophiala sp was the only agent identified in this group of OTRs. This species is ubiquitous in nature and typically causes infections via traumatic implantation.9, 10 All of our patients had lesions on the limbs, which can be attributed to direct inoculation of the fungus into damaged skin after contact with a contaminated fomite or plant.
The treatment of phaeohyphomycosis is a challenging issue, as there is no standardized treatment and a high possibility of dangerous drug-drug interactions.1, 4, 6, 7 Surgery is likely the best treatment for well-circumscribed lesions, but additional medical treatment is recommended to avoid local sporotrichoid dissemination and to treat concomitant subclinical lesions.4, 7, 10 In the selected patients, a cure can be achieved by surgery alone as could be seen in case 4. However, we do believe that surgery can be an important adjuvant therapeutic method that should be associated whenever possible with antifungal medications.
Itraconazole was the antifungal medication used in most of our patients and was associated with high cure rate. Itraconazole, which is fungistatic and inhibits ergosterol synthesis, seems to be the most effective agent, especially against Exophiala sp.9, 10
One of the most important points to consider in the use of broad-spectrum azoles in OTRs is that these drugs are strong cytochrome CYP3A4/5 inhibitors and may cause major drug-drug interactions with calcineurin and mammalian target of rapamycin (mTOR) inhibitors.1, 4, 6 Because these immunosuppressive drugs are characterized by a narrow therapeutic window, these drug-drug interactions could lead to clinical complications as also clearly seen in the first case. It is important to closely monitor tacrolimus concentrations and be on the look out for signs of drug-related toxicity.
Because of the increased incidence of phaeohyphomycosis in OTRs, it is important that all clinicians involved in solid organ transplants always consider the possibility of this disease in allograft recipients with skin lesions. The high degree of clinical suspicion is essential to establish the correct diagnosis and to start treatment promptly to avoid serious complications and organ rejection.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Vasquez-del-Mercado E., Lammoglia L., Arenas R. Subcutaneous phaeohyphomycosis due to Curvularia lunata in a renal transplant patient. Rev Iberoam Micol. 2013;30(2):116–118. doi: 10.1016/j.riam.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 2.Isa-Isa R., Garcia C., Isa M., Arenas R. Subcutaneous phaeohyphomycosis (mycotic cyst) Clin Dermatol. 2012;30(4):425–431. doi: 10.1016/j.clindermatol.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 3.Pereiro M., Jr., Pereiro Ferreiros M.M., De Hoog G.S., Toribio J. Cutaneous infection caused by Alternaria in patients receiving tacrolimus. Med Mycol. 2004;42(3):277–282. doi: 10.1080/13693780310001610047. [DOI] [PubMed] [Google Scholar]
- 4.Vermeire S.E., de Jonge H., Lagrou K., Kuypers D.R. Cutaneous phaeohyphomycosis in renal allograft recipients: report of 2 cases and review of the literature. Diagn Microbiol Infect Dis. 2010;68(2):177–180. doi: 10.1016/j.diagmicrobio.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 5.Sudduth E.J., Crumbley A.J., Farrar W.E. Phaeohyphomycosis due to Exophiala species: clinical spectrum of disease in humans. Clin Infect Dis. 1992;15:639–644. doi: 10.1093/clind/15.4.639. [DOI] [PubMed] [Google Scholar]
- 6.Salido-Vallejo R., Linares-Sicilia M.J., Garnacho-Saucedo G. Subcutaneous phaeohyphomycosis due to Alternaria infectoria in a renal transplant patient: surgical treatment with no long-term relapse. Rev Iberoam Micol. 2014;31(2):149–151. doi: 10.1016/j.riam.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Cunha D., Amaro C., Vieira M.R. Phaeohyphomycosis caused by Alternaria infectoria presenting as multiple vegetating lesions in a renal transplant patient. Rev Iberoam Micol. 2012;29(1):44–46. doi: 10.1016/j.riam.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Hsu C., Chang S., Lee P., Chao S. Cutaneous alternariosis in a renal transplant recipient: A case report and literature review. Asian J Surg. 2015;38:47–57. doi: 10.1016/j.asjsur.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Gold W.L., Vellend H., Salit I.E. Successful treatment of systemic and local infection due to Exophiala species. Clin Infect Dis. 1994:339–341. doi: 10.1093/clinids/19.2.339. [DOI] [PubMed] [Google Scholar]
- 10.McCown H.F., Sahn E.E. Subcutaneous phaeohyphomycosis and nocardiosis in a kidney transplant patient. J Am Acad Dermatol. 1997;36:863–866. doi: 10.1016/s0190-9622(97)70042-2. [DOI] [PubMed] [Google Scholar]