Abstract
Background
Lipomas are benign mesenchymal tumors composed of mature adipocytes. They are classified according to their histological pattern and their etiology remains unclear. Objectives: To present two cases and review the literature.
Material and Methods
A search was conducted in the Medline / PubMed and Scielo data bases of the last 10 years (2004-2014) with the keywords “ intraoral lipoma OR oral cavity lipoma”.
Results
46 articles with 95 cases (56 women and 39 men) were reviewed. The average age was found to be 52.28 years (52.28 ± 18.55); and most of them occurred between the 4th and 6th decade of life. Lipomas occur mostly in the buccal mucosa (n = 36, 37.9%), followed by the tongue (n = 23, 24.2%) and other locations (n = 36, 37.9%). The most common histologic pattern was simple lipomas (n = 40, 42%), followed by fibrolipomas (n = 18, 18.9%) and other types (n = 37, 39.1%). The average tumor size was 19.77 ± 16.26mm.
Conclusions
Lipomas are a relatively rare finding in the oral cavity. Surgical excision is the treatment of choice and recurrence is not expected.
Key words:Benign oral tumor, oral lipoma, lipoma, oral cavity.
Introduction
Lipoma is a benign mesenchymal tumor composed of mature adipocytes (1,2). They are common in the head and neck region, but their appearance in the oral cavity is uncommon. Only 1-5% of the lesions are located in this area (3,4); representing 2.2% of all lipomas (3). The most common areas are the buccal mucosa, lips, tongue, palate,vestibule, floor of the mouth and retromolar area (5).
Clinically they are well circumscribed, painless and slow growing tumors (6-8). Their etiology and pathogenesis are not clear, even though factors like mechanical, endocrine, inflammatory (6,8-10), hypercholesterolemia and obesity (11,12), radiation (11) as well as chromosomal abnormalities (3,9,13) have been considered. Histologically they can be classified as simple lipoma, fibrolipoma, spindle cell lipoma, intramuscular lipoma, chondrolipoma, pleomorphic lipoma, myxoid lipoma, angiolipoma and sialolipoma (3,6,14).
The most accepted treatment is surgical excision, but medical management has also been proposed (4,5). Recurrence is rare (4).
In this paper we present a review of the literature of the past 10 years and two clinical cases.
Material and Methods
A literature review of the last 10 years (2004)-(2014)in the Medline_Pubmed database and ScIELO (Scientific Electronic Library Online) was done using the keywords ”intraoral lipoma OR oral cavity lipoma”. Selection criteria included literature reviews, case series and case reports in humans; in English and in Spanish. Articles which did not include intraoral lipomas or information about sex, age and/or size and lipomas localized in the parotid gland were eliminated. The papers reviewed specifically analyze the number of cases, sex, age, location, size and histological pattern.
In this review we present two cases of lipoma.
Results
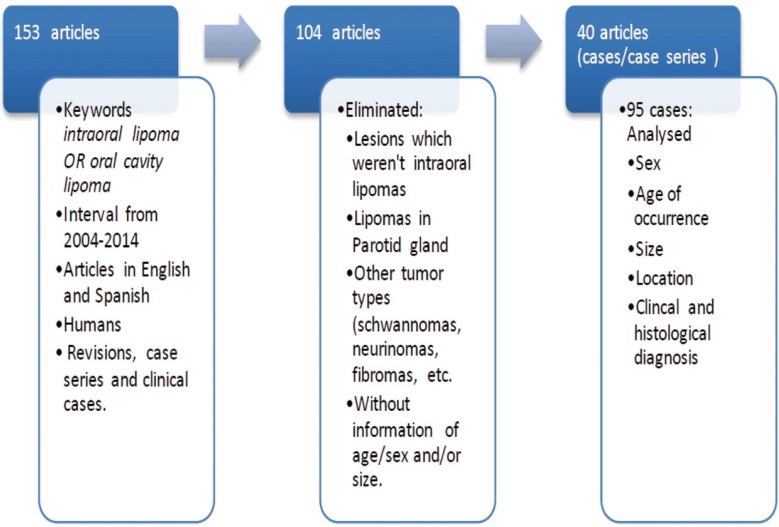
157 articles were initially found, which after the application of the selection criteria were reduced to 40 case series and clinical case reports which included a total of 95 intraoral lipomas (Fig. 1). Table 1 summarizes the most significant data obtained from each article (1-40).
Figure 1.
Flow chart with the selection criterion for the inclusion of selected publications.
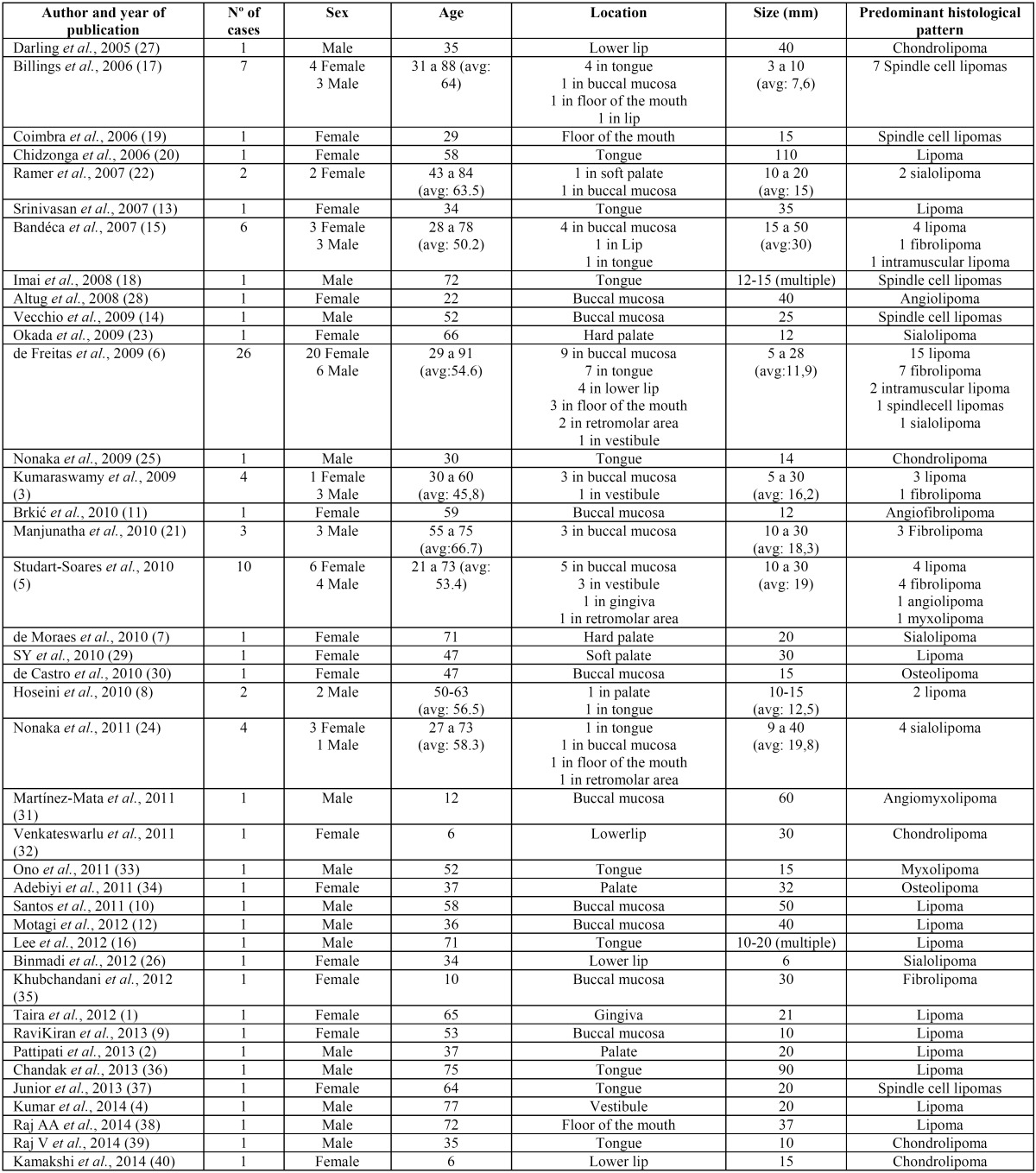
Table 1. Articles reviewed with their most significant data.
With regards to sex distribution, 56 cases were found in women (58.9%), 39 in men (42.2%). The average age was found to be 52.28 years (52.28 ± 18.55); and it is noteworthy that the majority of lesions occurred in the fourth and sixth decade of life.
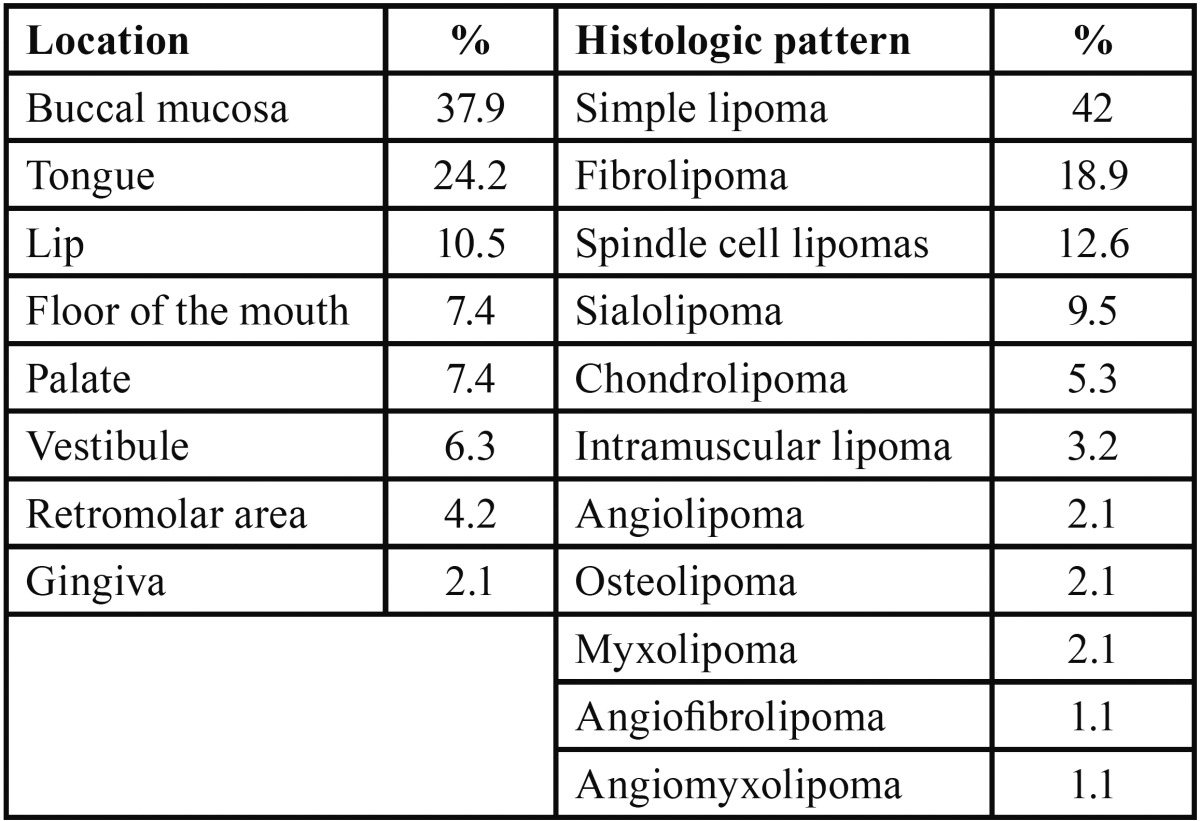
The most common region for the occurrence was the buccal mucosa (n=36, 37.9%), followed by the tongue (n=23, 24.2%), lip (n=10, 10.5%), palate (n=7, 7.4%), floor of the mouth (n=7, 7.4%), vestibule (n=6, 6.3%), retromolar area (n=4, 4.2%) and gingiva (n = 2, 2.1%) ( Table 2).
Table 2. Location and histologic pattern.
Regarding the histological type, the most common pattern was simple lipomas (n=40, 42%), fibrolipomas (n=18, 18.9%), followed by spindle cell lipoma (n=12, 12.6 %), sialolipomas (n=9, 9.5%), chondrolipomas (n=5, 5.3%), intramuscular lipomas (n=3, 3.2%), angiolipomas (n=2, 2.1% ), osteolipomas (n=2, 2.1%), myxolipomas (n=2, 2.1%), angiofibrolipomas (n=1, 1.1%) and angiomyxolipomas (n=1, 1.1%) ( Table 2).
With reference to the size of lipomas reviewed, the average size was recorded to be 19.77 ± 16.26 mm and two of the lesions were multiple.
-Case report nº 1
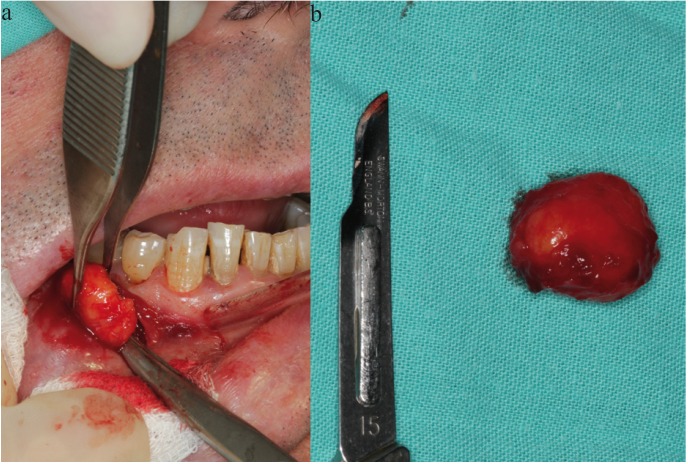
We report a case of a 61 year old man with an accidental finding of a lesion; a single painless swelling in the right lower vestibule. Clinical examination revealed a mass of 1.6x1.7cm, soft, mobile, not attached to deeper planes and covered by mucosa which appeared normal but with a slight yellowish color. No neurological defects were demonstrated despite its location near the mental foramen, and cervical lymphadenopathy couldn’t be palpated (Fig. 2).
Figure 2.
Submucosal mass in the left mandibular vestibule.
A differential diagnosis of lipoma was given, which was confirmed with fine needle aspiration cytology (FNAC). The lesion was enucleated under local anesthesia with articaine 1: 100,000 4%, followed by incision, dissection, excision and suture using Vicryl® 3/0. Macroscopically itwas an encapsulated lesion, easily enucleable and yellowish in color (Fig. 3a). Histological examination at 40x magnification (H & E, Hematoxylin & Eosin) showed adipocytes and a well circumscribed tumor with a thin fibrous capsule.
Figure 3.
a) Exposing the mass. b) Macroscopic image of the surgically excised tissue.
The postoperative period was uneventful and no recurrence was seen after 1 year of follow-up. The definitive diagnosis was confirmed to be lipoma, similar to clinical diagnosis (Fig. 3b).
-Case report nº 2
The second case is of an 89-year-old female with a nodular lesion on the left lingual border with a diameter of 1.2 cm and unknown time of evolution. The lesion was asymptomatic, well defined, smooth with soft consistency and with anormal lingual mucosal surface.
A presumptive diagnosis of fibroma was made. An excisional biopsy and enucleation of the lesion was performed. Macroscopically an encapsulated and yellowish lesion was observed. The definitive diagnosis was lipoma and there was no recurrence.
Histological examination with H & E staining revealed mature fat cells that differed little in microscopic appearance from the surrounding normal fatty tissue. The epithelium was found to be stratified squamous parakeratinized epithelium and fibrocellular connective tissue stroma, having abundant groups of oval cells with vacuolated peripheral nuclei planes, resembling adipocytes, characteristic of lipoma.
Discussion
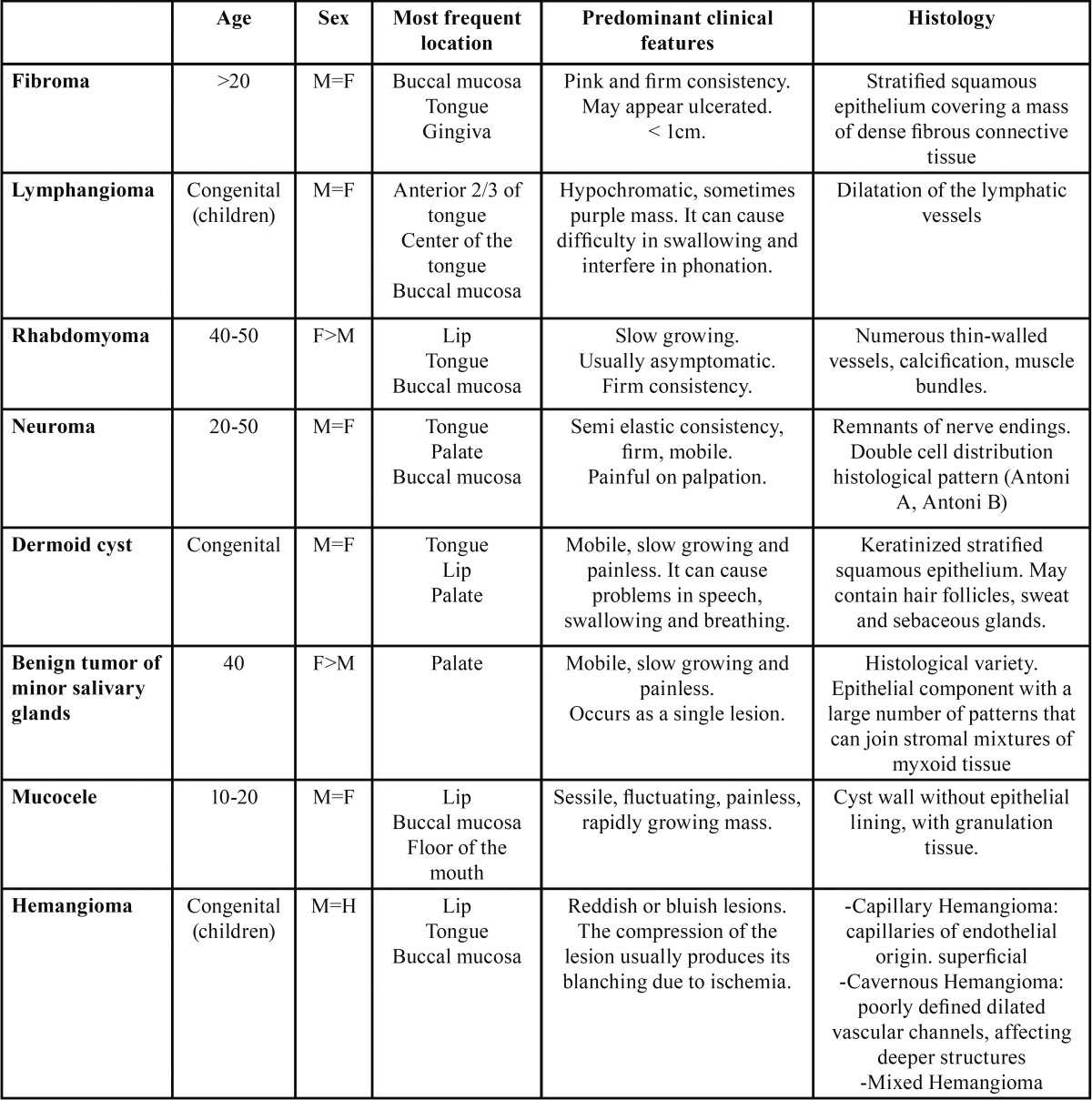
While intraoral lipomas are relatively uncommon (1,4,7,8,15,16), their clinical diagnosis is easy due to their yellowish color, and their usual location superficially near the mucosa (1). The differential diagnosis includes fibroma, dermoid cyst, minor salivary gland tumors, mucocele, hemangioma, lymphangioma, rhabdomyoma or neuroma (4,17) ( Table 3). Depending on its location, a herniated buccal fat of pad should also be kept in mind while performing a differential diagnosis (3).
Table 3. Differential diagnosis of intraoral lipoma.
The majority of cases are solitary tumors. The literature shows that only 5% occur as multiple lesions (4,13,16,18). We found 2 cases of multiple lipomas in our review (16,18). When they occur as multiple lesions they may be associated with syndromes such as neurofibromatosis, Gardner’s syndrome, Dercum’s disease, familial multiple lipomatosis, Proteus syndrome or Pai syndrome (4).
We have already mentioned that the etiology is unknown, but two main theories have been established. (i) The “Hypertrophy theory”, which states that obesity and inadvertent growth of adipose tissue may contribute to their formation. This theory is less convincing at explaining the lesions that occur in areas lacking pre-existing adipose tissue (4). (ii) The “Metaplasia theory” suggests that the lipomatous development occurs due to aberrant differentiation of mesenchymal cells in lipoblasts (3,4,19). Other mechanisms such as trauma, infection, chromosomal abnormalities or hormonal imbalances have also been proposed (3,6,11).
According to the literature,the most common sites of this type of tumor are the buccal mucosa and the tongue (20,21). Studart-Soares et al. (5), revised 450 intraoral lipomas between 1966 and 2009, and the most common site was found to be buccal mucosa (n=174; 38.7%), followed by vestibule (n=35; 7.8%), retromolar area (n=21; 4.7%), and other sites (n=220; 48.8%). Taira et al. (1), studied 207 cases published between 1987 and 2004, andalso found the buccal mucosa to be the most prominent site (n=84, 40.6%), followed by tongue (n=37, 17.9%), lip (n=26, 12.6%), and other areas (n=60, 28.9%). With respect to the histology, the sialolipoma variety is generally encountered in minor salivary glands (22-24). Our review also found the buccal mucosa to be the most common site for lipoma (n=38; 34.9%), in accordance with the literature.
With respect to the sex distribution in 450 cases studied by Studart-Soares et al. (5), 256 were males (52.2%) and 234 were females (47.8%). The tendency was similar in the review conducted by Taira et al. (1). On the other hand, in the study of 26 cases by Freitas et al. (6), 20 were females (76.92%) and 6 were males (23.8%). In our revision, we found a female predilection with 56 cases in females (58.9%), as compared to 39 males (41.1%). Thus, if we rely on the literature, there is practically no difference in distribution between the sexes, with a male to female ratio of 1:1.2 (4). With respect to the age of distribution, all the articles we studied seemed to coincide with our revision, with the majority of the lipoma cases occurring between the 4th and 6th decade of life (1,5).
Histologically, lipomas are classified based on the matrix and the properties of tumor cells: Simple lipoma, fibrolipoma, spindle cell lipoma, intramuscular lipoma, angiolipoma, chondrolipoma, pleomorphic lipoma, myxoid lipoma and sialolipoma (3,17,25,26). Studart-Soares et al. (5) investigated the histological type of 390 cases, in which the most common histologic pattern was simple lipoma (n=229, 48.7%), followed by fibrolipomas (n=103, 26.4%), myxolipoma (n=9, 2.3%), angiolipomas (n=4, 1%) and others (n=45, 11.5%). Taira et al. (1), analyzed the histological pattern of 113 cases in their study; and the prevalence of various histological types in descending order were simple lipomas (n=78, 69%), fibrolipomas (n=31, 27.4%) and others (n=4, 3.5%). This trend coincides with the one we found in this review; we found predominance of simple lipomas (n=40, 42%), followed by fibrolipomas (n=18, 18.9%), spindle cell lipomas (n=12, 12.6%) and finally other histological types (n = 25, 26.3%).
The size of lipomas varies greatly, although most of the lesions are less than 10mm (3), reaching up to 11cm in diameter (20). In this review, the average size was 19.77mm, the largest recorded lesion being 110 mm.
The treatment of choice is surgical excision. No recurrence has been described, although it may occur in the case of infiltrating lipomas basically due to an inadequate excision combined with a non-encapsulated lesion. Malignant transformation hasn’t been described either (4). Medical management of lipomas has also been proposed which involves injecting steroids to cause atrophy of adipose tissue. Lesions which are less than 2.5cm in diameter show a better prognosis. The injection of a mixture of 1:1 parts lidocaine with triamcinolone acetonideis repeated once a month. The average volume used ranges from 1 to 3 ml depending on the size of the tumor. Liposuction is also used using a 16-gauge needle in average (4 to 10 cm) or large-sized (> 10cm) tumors (4). In this review all lipomas were treated by surgical excision and none of them showed any recurrence.
References
- 1.Taira Y, Yasukawa K, Yamamori I, Iino M. Oral lipoma extending superiorly from mandibular gingivobuccal fold to gingiva: a case report and analysis of 207 patients with oral lipoma in Japan. Odontology. 2012;100:104–8. doi: 10.1007/s10266-011-0027-0. [DOI] [PubMed] [Google Scholar]
- 2.Pattipati S, Kumar MN, Ramadevi, Kumar BP. Palatal lipoma: a case report. J ClinDiagn Res. 2013;7:3105–6. doi: 10.7860/JCDR/2013/7886.3682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumaraswamy S, Madan N, Keerthi R, Shakti S. Lipomas of oral cavity: case reports with review of literature. J Maxillofac Oral Surg. 2009;8:394–7. doi: 10.1007/s12663-009-0096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar LK, Kurien NM, Raghavan VB, Menon PV, Khalam SA. Intraoral lipoma: a case report. Case Rep Med. 2014;2014:480130. doi: 10.1155/2014/480130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Studart-Soares EC, Costa FW, Sousa FB, Alves AP, Osterne RL. Oral lipomas in a Brazilian population: A 10-year study and analysis of 450 cases reported in the literature. Med Oral Patol Oral Cir Bucal. 2010;15:e691–6. doi: 10.4317/medoral.15.e691. [DOI] [PubMed] [Google Scholar]
- 6.de Freitas MA, Freitas VS, de Lima AA, Pereira FB Jr, dos Santos JN. Intraoral lipomas: a study of 26 cases in a Brazilian population. Quintessence Int. 2009;40:79–85. [PubMed] [Google Scholar]
- 7.de Moraes M, de Matos FR, de Carvalho CP, de Medeiros AM, de Souza LB. Sialolipoma in minor salivary gland: case report and review of the literature. Head Neck Pathol. 2010;4:249–52. doi: 10.1007/s12105-010-0187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoseini AT, Razavi SM, Khabazian A. Lipoma in oral mucosa: two case reports. Dent Res J. 2010;7:41–3. [PMC free article] [PubMed] [Google Scholar]
- 9.RaviKiran A, PurnachandraraoNaik N, Samatha Y, VijayKumar A, KalyanKumar D. Intraoral lipoma: a rare case report and review of literature. J ClinDiagn Res. 2013;7:3090–1. doi: 10.7860/JCDR/2013/6845.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santos LC, Wanderley Rocha SM, Carvalho CN, Oliveira EP, Neves DF. Intraoral lipoma: an atypical case. Braz J Otorhinolaryngol. 2011;77:676. doi: 10.1590/S1808-86942011000500024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brkić A, Ozçamur C, Gürkan-Köseoğlu B, Olgac V. Angiofibrolipoma of the buccal mucosa: a case report. J Oral Sci. 2010;52:173–6. doi: 10.2334/josnusd.52.173. [DOI] [PubMed] [Google Scholar]
- 12.Motagi A, Aminzadeh A, Razavi SM. Large oral lipoma: Case report and literature review in Iran. Dent Res J. 2012;9:350–2. [PMC free article] [PubMed] [Google Scholar]
- 13.Srinivasan K, Hariharan N, Parthiban P, Shyamala R. Lipoma of tongue - A rare site for a rare site for a common tumour. Indian J Otolaryngol Head Neck Surg. 2007;59:83–4. doi: 10.1007/s12070-007-0027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vecchio G, Amico P, Caltabiano R, Colella G, Lanzafame S, Magro G. Spindle cell/pleomorphic lipoma of the oral cavity. J Craniofac Surg. 2009;20:1992–4. doi: 10.1097/SCS.0b013e3181bd2dad. [DOI] [PubMed] [Google Scholar]
- 15.Bandéca MC, de Pádua JM, Nadalin MR, Ozório JE, Silva-Sousa YT, da Cruz Perez DE. Oral soft tissue lipomas: a case series. J Can Dent Assoc. 2007;73:431–4. [PubMed] [Google Scholar]
- 16.Lee SH, Yoon HJ. Bilateral asymmetric tongue classic lipomas. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:15–8. doi: 10.1016/j.tripleo.2011.07.045. [DOI] [PubMed] [Google Scholar]
- 17.Billings SD, Henley JD, Summerlin DJ, Vakili S, Tomich CE. Spindle cell lipoma of the oral cavity. Am J Dermatopathol. 2006;28:28–31. doi: 10.1097/01.dad.0000189615.13641.4b. [DOI] [PubMed] [Google Scholar]
- 18.Imai T, Michizawa M, Shimizu H, Imai T, Yamamoto N, Yura Y. Bilateral multiple spindle cell lipomas of the tongue. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2008;106:264–9. doi: 10.1016/j.tripleo.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 19.Coimbra F, Lopes JM, Figueiral H, Scully C. Spindle cell lipoma of the floor of the mouth. A case report. Med Oral Patol Oral Cir Bucal. 2006;11:401–3. [PubMed] [Google Scholar]
- 20.Chidzonga MM, Mahomva L, Marimo C. Gigantic tongue lipoma: a case report. Med Oral Patol Oral Cir Bucal. 2006;11:437–9. [PubMed] [Google Scholar]
- 21.Manjunatha BS, Pateel GS, Shah V. Oral fibrolipoma-a rare histological entity: report of 3 cases and review of literature. J Dent. 2010;7:226–31. [PMC free article] [PubMed] [Google Scholar]
- 22.Ramer N, Lumerman HS, Ramer Y. Sialolipoma: report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:809–13. doi: 10.1016/j.tripleo.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 23.Okada H, Yokoyama M, Hara M, Akimoto Y, Kaneda T, Yamamoto H. Sialolipoma of the palate: a rare case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:571–6. doi: 10.1016/j.tripleo.2009.05.045. [DOI] [PubMed] [Google Scholar]
- 24.Nonaka CF, Pereira KM, de Andrade Santos PP, de Almeida Freitas R, da Costa Miguel MC. Sialolipoma of minor salivary glands. Ann Diagn Pathol. 2011;15:6–11. doi: 10.1016/j.anndiagpath.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Nonaka CF, Miguel MC, de Souza LB, Pinto LP. Chondrolipoma of the tongue: a case report. J Oral Sci. 2009;51:313–6. doi: 10.2334/josnusd.51.313. [DOI] [PubMed] [Google Scholar]
- 26.Binmadi NO, Chaisuparat R, Levy BA, Nikitakis NG. Sialolipoma of the lower lip: case report and literature review. Open Dent J. 2012;6:208–11. doi: 10.2174/1874210601206010208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Darling MR, Daley TD. Intraoral chondroid lipoma: a case report and immunohistochemical investigation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:331–3. doi: 10.1016/j.tripleo.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Altug HA, Sahin S, Sencimen M, Dogan N, Erdogan O. Non-infiltrating angiolipoma of the cheek: a case report and review of the literature. J Oral Sci. 2009;51:137–9. doi: 10.2334/josnusd.51.137. [DOI] [PubMed] [Google Scholar]
- 29.SY A, Nao EEM, Ndiaye M, Taddio JM, Pegbessou EP, Ndiaye C. Lipoma of the soft palate: A rare anatomoclinical entity. Eur Ann Otorhinolaryngol Head Neck Dis. 2012;127:151–2. doi: 10.1016/j.anorl.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 30.de Castro AL, de Castro EV, Felipini RC, Ribeiro AC, Soubhia AM. Osteolipoma of the buccal mucosa. Med Oral Patol Oral Cir Bucal. 2010;15:347–9. doi: 10.4317/medoral.15.e347. [DOI] [PubMed] [Google Scholar]
- 31.Martínez-Mata G, Rocío MF, Juan LE, Paes AO, Adalberto MT. Angiomyxolipoma (vascular myxolipoma) of the oral cavity. Report of a case and review of the literature. Head Neck Pathol. 2011;5:184–7. doi: 10.1007/s12105-011-0241-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Venkateswarlu M, Geetha P, Srikanth M. A rare case of intraoral lipoma in a six year-old child: a case report. Int J Oral Sci. 2011;3:43–6. doi: 10.4248/IJOS11008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ono S, Rana M, Takechi M, Ogawa I, Okui G, Mitani Y. Myxolipoma in the tongue - a clinical case report and review of the literature. Head Neck Oncol. 2011;3:50. doi: 10.1186/1758-3284-3-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adebiyi KE, Ugboko VI, Maaji SM, Ndubuizu G. Osteolipoma of the palate: Report of a case and review of the literature. Niger J Clin Pract. 2011;14:242–4. doi: 10.4103/1119-3077.84029. [DOI] [PubMed] [Google Scholar]
- 35.Khubchandani M, Thosar NR, Bahadure RN, Baliga MS, Gaikwad RN. Fibrolipoma of buccal mucosa. Contemp Clin Dent. 2012;3:112–4. doi: 10.4103/0976-237X.95119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chandak PS, Pandilwar K, Chandak T, Mundhada R. Huge lipoma of tongue. Contemp Clin Dent. 2012;3:507–9. doi: 10.4103/0976-237X.107457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Junior OC, de Aguilar EC, Sartori JH, Lima fdeO. Spindle cell lipoma of the tongue: A case report of unusual occurrence. J Oral Maxillofac Pathol. 2013;17:148. doi: 10.4103/0973-029X.110730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raj AA, Shetty PM, Yadav SK. Lipoma of the floor of the mouth: report of an unusually large lesion. J Maxillofac Oral Surg. 2014;13:328–31. doi: 10.1007/s12663-011-0204-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Raj V, Dwivedi N, Sah K, Chandra S. Chondrolipoma: report of a rare intra oral variant with review of histiogenic concepts. J Maxillofac Oral Pathol. 2014;18:276–80. doi: 10.4103/0973-029X.140785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.G K, Pi Y. Chondrolipoma of the lower lip: A case report. J ClinDiagn Res. 2014;8:FD07–8. doi: 10.7860/JCDR/2014/7634.4461. [DOI] [PMC free article] [PubMed] [Google Scholar]