Abstract
Background:
Use of valid criteria for evaluation of patients admitted to intensive care unit (ICU) is essential to assess the quality of services provided. This study was conducted to evaluate admission, mean and the highest Sequential Organ Failure Assessment (SOFA) scores in predicting mortality and outcome of patients admitted to the ICU.
Methods:
This prospective observational study was conducted on 300 patients admitted to the ICU of Imam Khomeini Hospital, Sari, Iran, in 2015. The SOFA tool was applied at the beginning of the admission of patients in the ICU and then every 24 hours. Functions of six vital organs were recorded on a daily basis for scoring with SOFA. Demographic profile, the main diagnosis leading to hospitalization in the ICU, previous interventions, complications and hospital outcomes were recorded for each patient. The patients’ admission, mean and highest SOFA scores were also evaluated and recorded during the study period. These scores were compared between deceased and survived patients. ROC curve determined the best cut-off point of score calculated.
Results:
Among all 300 patients who were enrolled in the study, 189 (63%) cases were males. Trauma was the most common cause of hospitalization and mortality. Thirty point seven percent of 92 deceased patients needed to intubation. Mean length of ICU and hospital stay were significantly longer for deceased patients than the survivors (P <0.001). The admission, mean and highest SOFA scores were 11.72, 16.38 and 16.45 in deceased patients, as well as 6.52, 5.82 and 6.5 in survived patients, respectively. The area under the curve (AUC) for the admission, mean and highest SOFA scores were 0.875, 0.988 and 0982, respectively. All three models were able to predict the outcome of patients significantly (P <0.0001). The cut-off point of 10.6 for the mean SOFA had the highest sensitivity and specificity in predicting mortality.
Conclusion:
The results of this study showed that the mean SOFA score had the highest sensitivity and specificity in prediction of ICU mortality. Therefore, this criterion is a valuable indicator to better predictions of mortality and morbidity rate in the ICU patients, which can lead to appropriate health care and therapeutic interventions in these patients.
Keywords: Sequential Organ Failure, SOFA Score, Intensive Care, Mortality
1. INTRODUCTION
Intensive care includes all critical cares depend on the patient’s life under supervision of the more experienced and more highly qualified physicians and nurses using advanced equipment and facilities (1, 2). Multiple organ dysfunction syndrome (MODS) is the last step in severely ill patients, which occurs following infection and septic shock, tissue damage, excessive hemorrhage, ischemia and severe inflammation (3, 4). Entanglement of various organs including the liver, kidney, lung, gastrointestinal system, and central nervous system (CNS) in the MODS is evident as slight to progressive damages such as pulmonary hypertension, renal failure, gastritis, pancreatitis, encephalopathy, and acid-base and electrolyte disorders. In previous studies has been indicated that the MODS has a poor prognosis and a direct relationship with the organs involved, so that mortality will be higher with more organs involved (4-6).
Nowadays, the standard scoring systems determine the severity of illness and the probability of mortality in patients hospitalized in the intensive care units (ICUs) (7, 8). Currently, there are different methods to predict patient outcomes, but four of them are more reliable accredited by most references, including Acute Physiology and Chronic Health Evaluation (APACHE II, III, IV), the Simplified Acute Physiology Score (SAPS), the Mortality Prediction Model (MPM) and the Sequential Organ Failure Assessment (SOFA) (7-9).
SOFA score (0–4 points) is determined for each one of the six organ systems (neurologic, respiratory, cardiovascular, renal, hepatic, and hematologic) (10-12). The advantages of the SOFA compared to the other three abovementioned methods are high discriminatory power and calibration, no need for computer software and operator, the simplicity of collecting information and low cost (10). The three APACHE II, MPM and SAPS models are required to investigate a large number of variables (14, 15 and 17 respectively), whereas the SOFA uses only six variables. In addition, it is possible to review information on a daily basis or every 48 hours in the SOFA model, while only at the first 24 hours in the three other models (4, 13).
The SOFA is more preferable compared to three other systems by taking two principles of the accurate assessment of the mortality outcome and the ease of usability of the tool due to the high cost and the long lead-time to data collection in critically ill patients (14). Because of serial evaluation of the SOFA score, parameters called mean SOFA (the mean SOFA scores during hospitalization) and highest SOFA (the highest SOFA score during the length of stay) are assessed, which their relationship with the morbidity and mortality has been clearly expressed in some studies (14-15). Benefiting from a valid indicator is essential to evaluate patients admitted to the ICU for having accurate judgment about the quality of services provided, while many hospitals use traditional methods to assess patients (8).
Therefore, this study aimed to use and evaluate the SOFA scoring tool (the admission, mean and highest SOFA scores) in prediction of ICU mortality.
2. METHODS
This prospective observational study was performed on 300 patients admitted to the ICU of a teaching hospital affiliated to the Mazandaran University of Medical Sciences (Imam Khomeini hospital), Sari, Iran in 2015. Approval of the institutional review board was obtained. The exclusion criteria were patients younger than 18 years, mortality in less than four hours in the ICU, hospitalization less than 24 hours in the ICU, cardiopulmonary resuscitation (CPR) before admission in the ICU, and readmission to the ICU. The SOFA tool was used at the admission of patients in the ICU and then every 24 hours. Functions of six vital organs were evaluated and recorded on a daily basis; as respiratory system with the PO2/FiO2, cardiovascular system with the mean arterial pressure (MAP) and the need for vasoactive drugs, hematologic system by measuring platelets levels, hepatic system by measuring total bilirubin level, neurologic system with the glasgow coma scale (GCS) score and renal system with the levels of creatinine and urine output. The SOFA score for a patient is the sum of scores of all organs. Each organ is scored from zero to four, and the total score is between zero to 24. Organ dysfunction is characterized by the scores of 1-2, and organ failure with the scores of 3-4. The daily scores were presented to physicians to be informed of the status of the organs function to start a new therapeutic strategy for the patient, if necessary. The scores at the beginning of the admission in the ICU, and the mean scores of all hospitalization days in the ICU, and the highest score during the hospitalization period were evaluated for comparison between deceased and survived patients. Moreover, demographic profile, the main diagnosis leading to hospitalization in the ICU, previous interventions, complications and hospital outcomes were recorded for each patient. Mean and standard deviation were used to describe quantitative data and the number (percentage) for qualitative variables. After describing data using central and dispersion indicators, data were analyzed using correlation between variables. ROC curve determined the best cut-off point.
3. RESULTS
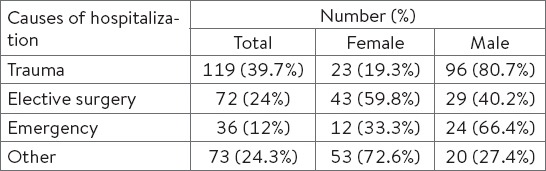
In this study, 300 patients hospitalized in the intensive care unit were enrolled, including 189 (63%) males and 111 (37%) females. The mean age was 44±20 years for males and 46±18 years for females, the age difference between the two groups was not statistically significant (P >0.05). Sex had a significant effect on the cause of admission, so that more males were hospitalized for trauma that this difference was statistically significant (P <0.0001). As shown in Table 1, the most common cause of hospitalization was related to trauma, with a prevalence of 37.9%.
Table 1.
Frequency of causes of hospitalization in intensive care unit (ICU)
From total amount 133 (44.3%) of cases had underlying diseases. History of underlying disease in females was more than males (P <0.0001). Ninety-two of the 300 patients died. The relative frequency of mortality between males and females had no statistically significant difference (P =0.154). The death occurred in 55 (41.1%) patients with a history of underlying disease, while was 37 (22%) among those did not any underlying diseases (P <0.0001). Twenty-six deceased patients had a previous history of hospitalization. In addition, the greatest cause of mortality in patients was trauma. One hundred ninety-five patients required intubation, which 104 (53.3%) of them survived. 30.7% of 92 deceased patients required intubation. Four patients needed re-intubation that had been done 12, 11, 5 and 4 hours later and all four patients were also in the deceased group. In terms of the need for intubation, no statistically significant difference was observed between the two groups (P =0.993).
The mean length of hospitalization in the ICU in deceased patients was almost 2 times of survived ones and this difference was statistically significant (P <0.001) (Table 2).
Table 2.
Number of hospitalization days of deceased and survived patients in the hospital and the ICU
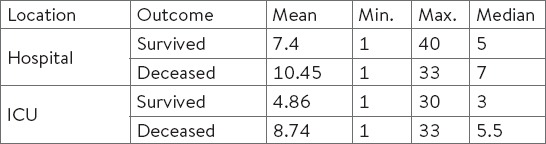
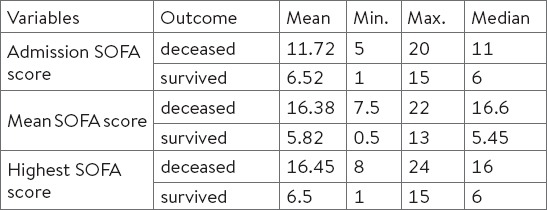
The time of death after admission to the ICU was at least 1 day and maximum 33 days, with an average of 9.9±7.4 days. The admission, mean and highest SOFA scores in deceased and survived patients have been shown in Table 3.
Table 3.
The admission, mean and highest SOFA scores in the ICU patients during the study period in the deceased and survived patients
The best estimate of mortality was related to the highest SOFA score. The discriminatory power was measured using receiver-operating characteristic (ROC) curve. The area under the curve (AUC) for SOFA scores of patients at the time of admission to the ICU (0.875, 95% CI: 0.835 to 0.915), mean SOFA (0.988, 95% CI: 0.978 to 0.999) and the highest SOFA score (0.982, 95% CI: 0.97 to 0.993) have been presented in Table 4.
Table 4.
Comparison of the sensitivity and specificity in three models of SOFA scores in estimating mortality rate. PPV: positive predictive values, NPV: negative predictive values

All three models were able to predict patient outcomes significantly (P <0.0001). As Figure 1 shows, cut-off point of 10.6 for the mean SOFA had the highest sensitivity and specificity in predicting ICU mortality. According to the ROC curve, the mean SOFA was the best method to predict patient outcomes, significantly better than the other two models.
Figure 1.
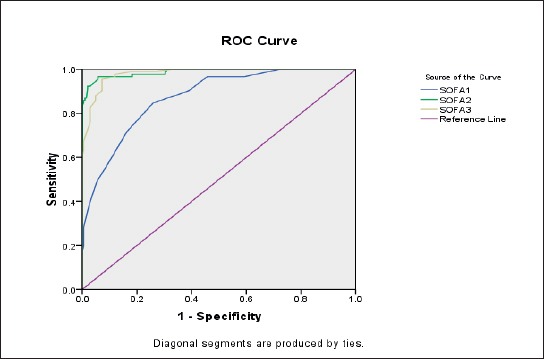
Comparison of ROC curve to predict mortality rate
4. DISCUSSION
The findings of this study showed that although all three assessment models of SOFA scores were significantly able to predict patient outcomes, but the mean SOFA had the highest sensitivity and specificity compared to the other two models. The SOFA scoring system seeks the status of patients during hospitalization in the ICU. The prediction of patient outcomes and mortality by the SOFA scoring system has been started since 1986. The SOFA tool is one of several scoring systems in the ICU, which determines the extent or rate of organ dysfunction and predicts patients’ mortality. This scoring is based on six different points, one each for the respiratory, cardiovascular, hepatic, hematologic, renal and neurological systems (10, 14-16). It assists physicians, nurses and other health care providers in estimating the risk of morbidity and mortality (8, 10, 17).
To the best of our knowledge, this is the first study in Iran which evaluated the association of patient outcomes with the first day SOFA, mean-SOFA, and highest-SOFA scores. In Iran, other tools have been frequently used to predict patient outcomes; for example, Fallahinia et al. used the SAPS III tool to predict patient outcomes (18). In the present study, the mean SOFA score was the best predictor for mortality, while in other assessment models such as MPM, SAPS and APACHE, other researchers observed that the best time to estimate hospital mortality is more feasible in the first days of hospitalization (19-20).
In the present study, trauma was the most common cause of hospitalization in the ICU, which this rate was greater in males than females. Various geographical areas have different disease outbreaks and reasons for hospitalization. In the study of Johnson et al., the most common cause of hospitalization was the infections and lung problems (21). In the present study, the mortality rate was 30.6%, and there was no significant difference between males and females. This percentage has been reported differently in the diverse ICUs in other studies; for example, 1 percent in a study of Raksakietisak et al. (22), 23.9 percent by Haddadi et al. (23), 59 percent by Vosylius et al. (24) and 59 percent by Johnson et al. (21).
Forty one percent of the patients died due to underlying disease, like the study of Raksakietisak et al. which the most frequent underlying diseases was related to blood pressure (38.2 %) and heart disease (28.5 %) (22). In a study of Vosylius et al. in Lithuania, the most functional defects were the cardiovascular, renal and nervous systems (24). In our study, the most common cause of mortality was due to trauma, but Raksakietisak et al. reported arrhythmias, hemorrhagic shock and ischemic heart disease as the common causes of mortality (22) and Vosylius announced cardiovascular and nervous systems as most common causes (24).
In all three models evaluated in our study, the SOFA score (admission, mean and highest) was significantly greater in the deceased group compared with survivors, which the results are in line with most of the studies carried out in the world. In the study by Vosylius et al. the SOFA score in the first and third days of hospitalization was significantly higher for the deceased patients and organ dysfunction score was significantly greater in the deceased group than in the survived patients (24). In the study of Johnson et al. the mean SOFA score was 12±3.9 for all ICU patients. The mean SOFA score was 14.4±3.9 for medical deceased patients and 8.2±3.9 for surgical deceased patients. The highest SOFA score has progressively amplified by increasing hospitalization in the ICU. They observed poor prediction of patient outcomes due to MODS on the first day of stay in the ICU. Similar to our findings, the prediction of patient outcomes through admission SOFA is weaker than in the other two models (21).
In the study of Haddadi et al., the mean and highest SOFA scores for the ICU patients with hospital-acquired infection during the six days of hospitalization were 8.28 and 48, respectively. The SOFA score of 12.3 with confidence interval between 2.33 and 64.91 had the best prediction (23). Ferreira et al. said that the SOFA score on second day was more efficient than admission SOFA score (25).
Most studies, like our work, claim poor predictive power for the admission SOFA score. Haddadi et al. reported that AUC for SOFA was 0.718 on the last day (23). Peres Bota et al. revealed that the AUC for the admission SOFA was 0.73 (4). Khwannimit et al. obtained 0.879 and 0.907 for the AUC of the first day and highest SOFA scores, respectively (13) and the accuracy of the admission SOFA tool was weaker as our study. In the study of Zygun et al. in Canada, the AUC for the admission and highest SOFA were 0.67 and 069, respectively (26).
In the study of Vosylius et al. admission, highest and mean SOFA had significant relationship with the patient mortality. They reported that the highest and admission SOFA scores greater than 11 or mean SOFA scores more than 5 predict over 80% of mortality (24).
Majority of studies have claimed that the SOFA score has suitable discriminatory power as well as higher sensitivity and specificity in determining the outcome of patients admitted to the ICU, and they proved poor ability to accurate measurement of patient outcomes on the first day; while the discriminatory power improves with increasing duration of stay in the ICU.
It has been shown that predicting patients’ outcome based on the AUC for the SOFA score on the first and third days was perfect for functioning of all organs, but the admission SOFA score was not very helpful for the analysis of patient outcomes (4). Moreover, it has been revealed that the results of SOFA scoring have been as efficient as of Apache III models. Despite the fact that the calculation of the SOFA score is easier and it does not dependent on early diagnosis during hospitalization (27).
5. CONCLUSION
The findings of this study showed that the mean SOFA score of the patients during ICU stay had the highest sensitivity and specificity in predicting their mortality. Therefore, this criterion is a valuable indicator to better predictions of mortality and morbidity in ICU patients, which can lead to appropriate health care and therapeutic interventions in these patients.
• Acknowledgement:
The financial support of Research Deputy of Mazandaran University of Medical Sciences is gratefully acknowledged. Also, the authors wish to thank all critical care nurses working in ICUs OF Imam Khomeni hospital, Sari, and patient’s family for their tremendous cooperation and support.
REFERENCES
- 1.Weil MH, Tang W. From intensive care to critical care medicine: a historical perspective. Am J Respir Crit Care Med. 2011;183(11):1451–3. doi: 10.1164/rccm.201008-1341OE. [DOI] [PubMed] [Google Scholar]
- 2.Ahanchian MR, Emami Zeydi A, Armat MR. Conflict management styles among Iranian critical care nursing staff: a cross-sectional study. Dimens Crit Care Nurs. 2015;34(3):140–5. doi: 10.1097/DCC.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 3.Murray MJ, Coursin DB. Multiple organ dysfunction syndrome. Yale J Biol Med. 1993;66(5):501–10. [PMC free article] [PubMed] [Google Scholar]
- 4.Peres Bota D, Melot C, Lopes Ferreira F, Nguyen Ba V, Vincent JL. The Multiple Organ Dysfunction Score (MODS) versus the Sequential Organ Failure Assessment (SOFA) score in outcome prediction. Intensive Care Med. 2002;28(11):1619–24. doi: 10.1007/s00134-002-1491-3. [DOI] [PubMed] [Google Scholar]
- 5.Nair R, Bhandary NM, D’Souza AD. Initial Sequential Organ Failure Assessment score versus Simplified Acute Physiology score to analyze multiple organ dysfunction in infectious diseases in Intensive Care Unit. Indian J Crit Care Med. 2016;20(4):210–5. doi: 10.4103/0972-5229.180041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marshall JC, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ. Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med. 1995;23(10):1638–52. doi: 10.1097/00003246-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Keegan MT, Gajic O, Afessa B. Severity of illness scoring systems in the intensive care unit. Crit Care Med. 2011;39(1):163–9. doi: 10.1097/CCM.0b013e3181f96f81. [DOI] [PubMed] [Google Scholar]
- 8.Afessa B, Gajic O, Keegan MT. Severity of illness and organ failure assessment in adult intensive care units. Crit Care Clin. 2007;23(3):639–58. doi: 10.1016/j.ccc.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Wong EG, Parker AM, Leung DG, Brigham EP, Arbaje AI. Association of severity of illness and intensive care unit readmission: A systematic review. Heart Lung. 2016;45(1):3–9.e2. doi: 10.1016/j.hrtlng.2015.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janssens U, Graf C, Graf J, Radke PW, Königs B, Koch KC, et al. Evaluation of the SOFA score: a single-center experience of a medical intensive care unit in 303 consecu tive patients with predominantly cardiovascular disorders. Sequential Organ Failure Assessment. Intensive Care Med. 2000;26(8):1037–45. doi: 10.1007/s001340051316. [DOI] [PubMed] [Google Scholar]
- 11.Matsumura Y, Nakada TA, Abe R, Oshima T, Oda S. Serum procalcitonin level and SOFA score at discharge from the intensive care unit predict post-intensive care unit mortality: a prospective study. PLoS One. 2014;9(12):e114007. doi: 10.1371/journal.pone.0114007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain S, Guleria K, Suneja A, Vaid NB, Ahuja S. Use of the Sequential Organ Failure Assessment score for evaluating outcome among obstetric patients admitted to the intensive care unit. Int J Gynaecol Obstet. 2016;132(3):332–6. doi: 10.1016/j.ijgo.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Khwannimit B. Serial evaluation of the MODS, SOFA and LOD scores to predict ICU mortality in mixed critically ill patients. J Med Assoc Thai. 2008;91(9):1336–42. [PubMed] [Google Scholar]
- 14.Anami EH, Grion CM, Cardoso LT, Kauss IA, Thomazini MC, Zampa HB, Bonametti AM, Matsuo T. Serial evaluation of SOFA score in a Brazilian teaching hospital. Intensive Crit Care Nurs. 2010;26(2):75–82. doi: 10.1016/j.iccn.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 15.Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–800. doi: 10.1097/00003246-199811000-00016. [DOI] [PubMed] [Google Scholar]
- 16.Acharya SP, Pradhan B, Marhatta MN. Application of “the Sequential Organ Failure Assessment (SOFA) score” in predicting outcome in ICU patients with SIRS. Kathmandu Univ Med J (KUMJ) 2007;5(4):475–83. [PubMed] [Google Scholar]
- 17.Donabedian A. Evaluating the Quality of Medical Care. Milbank Q. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falahinia Gh, Oshvandi K, Farhanchi A, Moghimbeigi A, Zareian A. Comparing performance of the intensive care units based on the mortality rate and structural standards in educational hospitals. J Crit Care Nurs. 2014;7(1):e6882. [Google Scholar]
- 19.Salluh JI, Soares M. ICU severity of illness scores: APACHE, SAPS and MPM. Curr Opin Crit Care. 2014;20(5):557–65. doi: 10.1097/MCC.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 20.Castella X, Artigas A, Bion J, Kari A. A comparison of severity of illness scoring systems for intensive care unit patients: results of a multicenter, multinational study. The European/North American Severity Study Group. Crit Care Med. 1995;23(8):1327–35. doi: 10.1097/00003246-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Johnson S, AVR S. Comparison of Different Scoring Systems Used in the Intensive Care Unit. J Pulm Respir Med. 5:276. [Google Scholar]
- 22.Raksakietisak M, Toomtong P, Vorakitpokatorn P, Sengleulur A, Sunjohndee M. TISS 28 or SOFA: good predicting factors for admission in a surgical intensive care unit longer than 24 hours. J Med Assoc Thai. 2006;89(5):648–56. [PubMed] [Google Scholar]
- 23.Haddadi A, Ledmani M, Gainier M, Hubert H, Tagne J, Micheaux PLD. Comparing the APACHE II, SOFA, LOD, and SAPS II scores in patients who have developed a nosocomial infection. Bangladesh Crit Care J. 2014;2(1):4–9. [Google Scholar]
- 24.Vosylius S, Sipylaite J, Ivaskevicius J. Determinants of outcome in elderly patients admitted to the intensive care unit. Age Ageing. 2005;34(2):157–62. doi: 10.1093/ageing/afi037. [DOI] [PubMed] [Google Scholar]
- 25.Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754–8. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 26.Zygun Zygun DA, Laupland KB, Fick GH, Sandham JD, Doig CJ. Limited ability of SOFA and MOD scores to discriminate outcome: a prospective evaluation in 1,436 patients. Can J Anaesth. 2005;52(3):302–8. doi: 10.1007/BF03016068. [DOI] [PubMed] [Google Scholar]
- 27.Markgraf R, Deutschinoff G, Pientka L, Scholten T, Lorenz C. Performance of the score systems Acute Physiology and Chronic Health Evaluation II and III at an interdisciplinary intensive care unit, after customization. Crit Care. 2001;5(1):31–6. doi: 10.1186/cc975. [DOI] [PMC free article] [PubMed] [Google Scholar]


