Abstract
Background:
We aimed to analyze the effect of nursing strategies on patients with chronic renal failure (CRF) undergoing maintenance hemodialysis (MHD) treatment by puncturing on arteriovenous fistula (AVF).
Methods:
Ninety-two patients with chronic renal failure undergoing maintenance hemodialysis (MHD) between Jan 2014 and Jan 2015 were included in the study (all undergoing AVF, dialysis for 2–3 sessions per week, 4–5 h per session) and randomly divided into control group and observation group. Patients in control group were given standard nursing care and patients in observation group were given professional nursing of internal fistula. The complication rate and dysfunction rate during internal fistula perioperative period, fistula usage time and effect on life quality of patients of these two groups were compared (during 18-month follow-up).
Results:
The complication rate and dysfunction rate during internal fistula perioperative period of the observation group were significantly lower than that of the control group, and the difference was statistically significant (P<0.05). The median time of internal fistula usage was significantly prolonged, and the health index, emotion index and psychology index quality-of-life in the observation group were significantly higher than that of the control group (P<0.05).
Conclusion:
Professional nursing strategies of internal fistula can prolong service time, decrease complications and improve life quality for patients undergoing maintenance hemodialysis treatment via arteriovenous fistula.
Keywords: Chronic renal failure, Arteriovenous fistula (AVF), Maintenance hemodialysis (MHD), Dysfunction rate, Quality-of-life (QOL)
Introduction
An increasing proportion of patients with chronic renal failure are given maintenance hemodialysis (MHD), which significantly improves renal function and life quality and prolongs survival time (1). Arteriovenous fistula (AVF) is the optimal vascular access of MHD, having many advantages such as little trauma, easy to puncture, sufficient blood flow and low infection rate (2).
In the first two years of dialysis, the percentage of admission caused by complication of hemodialysis access was high as 72.0%, occupying 20.5% of the admission caused by end-stage renal disease (3). During the process of internal fistula usage, repeatedly puncturing at the same place may cause blood vessel injury, fibrosis, hardening blood vessel and narrowing lumen and influence quantity of blood flow; moreover, fixed puncture point may also cause errhysis and psudoaneurysm; slow blood flow inside the aneurysm may cause thrombus and large aneurysm may have rupture and bleeding and infection (4). Because there are few blood vessels available for fistulizaition, protecting AVF well is particularly important for prolonging usage time and improve MHD effect (5).
The aim of the present study was to investigate the effect of nursing strategies on patients with CRF undergoing MHD treatment by puncturing on AVF.
Methods
Ninety-two patients with chronic renal failure first undergoing AVF, hospitalized in Ji’nan Municipal Organs Hospital (Ji’nan, Shandong Province, China) between Jan 2014 and Jan 2015, were concluded into the study, with vascular congenital malformation, puncture failure, poor compliance and no follow-up excluded.
After the approval of the Ethics Committee of the hospital and informed consent of patients and relatives, the cases were randomly divided into control group and observation group according to time sequence of admission, each of 46 cases.
Control group: Twenty-nine males, 17 females; ranged from 42–73 yr old, (average 56.7±13.2 yr old); serum creatinine 623–1524 μmol/L, (average 823.6±74.9 μmol/L).
Observation group: Twenty-eight males, 18 females; ranged from 43–74 yr old, (average 56.8±12.5 yr old); serum creatinine 664–1397 μmol/L, (average 815.4±66.5 μmol/L). Sex, age and creatinine level of the two groups were not significantly different (P<0.05).
Patients in control group were given with routine nursing, specifics were as follows: selected blood vessels with soft texture, large diameter, few branches, superficial vasculature and smooth blood flow for AVF operation, non-idiomatic body side radial artery - cephalic vein or brachial artery - cephalic vein preferred; surgical method was side-to-side or end-to-side anastomosis; the anticoagulation was unfractionated heparin or low molecular heparin; the dialysis frequency was 2–3 times per week for 4–5 h per time; the puncture needle was 16 G; quantity of blood flow was 200–280 mL/min. Nursing methods included psychological nursing, health education, nursing during fistula usage period, disease observation and diet and exercise guiding during hemodialysis period.
Patients in observation group were given professional nursing strategies of inter fistula, specifics as follows:
Avoided invasive manipulation or treatment on limbs of fistulization (6), such as blood drawing and venous transfusion; patients having a history of subclavian vein catheterization needed venography to show patency degree of vein blood vessels; blood pressure needed to be maintained among 130–140/80–90 mmHg to avoid postoperative thrombosis induced by hypotension. Corrected severe hypertension, hyperlipemia, edema, blood hyperviscosity and blood coagulation disorders, and encouraged patients to do handgrip exercise.
Did well the nursing before internal fistula usage (7), regulated indoor temperature to about 25 °C to avoid vasoconstriction caused by cold stimulation; kept the clothes and sleeves loose and the surgical dressing not too tight, avoided roll bandage; raising the affected limb was good for venous return and decreasing tissue edema; kept close observation of the wound and internal fistula situation for 3–4 times per day to see whether the wound had errhysis, effusion, red and swollen and whether the internal fistula had vibration, pulse and vascular murmur, if there were any abnormality, reported it to doctors and handled it with responding action; promoted the maturity of internal fistula, doing grasp movement exercise early, local hot compress and physical therapy were conducive to the rapid maturity of inter fistula.
The maturation period of inter fistula generally need 1–6 months, and it could be punctured for use when quantity of blood flow exceeded 600 mL/min. During first-use stage, the internal fistula was not fully mature and the vascular wall was relatively thin, which may cause injury and tear to form hematoma and influencing further usage. The puncture point should be chelidon; ordinary veins were used as blood passage; selected appropriate puncture point after the maturity of internal fistula; used the internal fistula systematically (8). The puncture point of artery should be 5 cm away from the anastomotic stoma, and the distance between the two points should ≥10 cm to decrease recirculation if they were punctured on the same blood vessel to be artery and vein respectively; the puncture needle should be 16 G, starting from 200 ml/min, the quantity of blood flow increased little by little after the maturity of the internal fistula. Strengthened the inspection tour and kept close observation to see whether the puncture point had errhysis and whether the needle had displacement and extrusion after the hemodialysis began; observed the blood pressure change and measured it every 30 min to prevent fistula obstruction caused by hypotension; observed whether the quantity of blood flow was sufficient. After the accomplishment of hemodialysis, rolled the square gauze and put it onto the puncture point, kept the vertical axis of the square gauze in correspondence with that of the puncture point, pressed the square gauze lightly and slowly pulled out the needle head; after the needle head got out of the blood vessel, rapidly intensified the pressure and fixed it with adhesive tape, at the same time determined whether to use elastic cord depending on individual factors, but the pressure should not cause bleeding and be suitable for the touch of vascular pulsation and vibration. Half an hour after withdrawing the needle, removed the elastic cord, ordered patients to examine the vibration and murmur of internal fistula every day during the dialysis period and report to doctors immediately if there were any informality such as pulse, weakening vibration and aching feelings.
Took precautions against fistula infection (9), the dialysis room should be given disinfection by ultraviolet light every day and equipped with air cleaner, and the floor should be mopped with disinfectant. Well hygienic propaganda and education, ordered patients to keep the puncture point skin clean and dry, pasted with waterproof adhesive tape when patients needed a shower or swim. If the puncture point got red and swollen, harden or the patient felt aching, doctors should change the puncture point immediately and handle it with appropriate action. Ordered patients to do local exercise of finger movements 3–5 d after the operation and “fistula exercises” to promote the maturity of internal fistula (10).
Observation indexes
The complication rate and dysfunction rate compared during internal fistula perioperative period, fistula usage time and effect on life quality of patients of these two groups. SF-36 scale used to evaluate life quality. The observation indexes were divided into three parts: health index, emotion index and psychology index.
Statistical Methods
SPSS 19.0 statistical software (Chicago, IL, USA) was used for recording and analysis. Quantitative data was expressed as mean ± standard deviation, and the comparison between groups was made by t test; qualitative data were expressed by percentage (%) and the comparison between groups was made by adopting χ2 test; fistula usage time was analyzed with Kaplan-Meier method; P<0.05 was considered to be statistically significant.
Results
Comparison of complication rate and dysfunction rate during internal fistula perioperative period
The two groups were followed up for about 18 months. The complication rate and dysfunction rate during internal fistula perioperative period of the observation group were significantly lower than that of the control group, and the difference was statistically significant (P<0.05) (Table 1).
Table 1:
Comparison of complication rate and dysfunction rate during internal fistula perioperative period [percent (%)]
| Group | Case | Hematoma | Infection | Blockage | Hemangioma | others | Complication rate | Dysfunction rate |
|---|---|---|---|---|---|---|---|---|
| Control group | 46 | 6 | 3 | 4 | 2 | 2 | 17 (37.0) | 16 (34.8) |
| Observation group | 46 | 3 | 1 | 2 | 1 | 1 | 8 (17.4) | 7 (15.2) |
| χ2 | 4.449 | 4.696 | ||||||
| P | 0.035 | 0.030 |
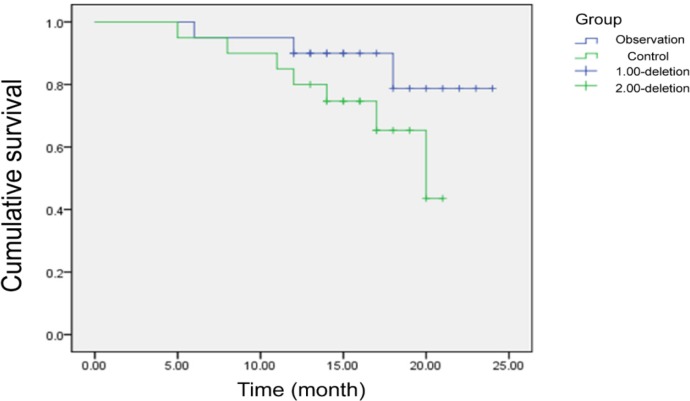
Fig. 1:
K-M analysis of fistula usage time
Comparison of fistula usage time and life quality of patients
The fistula usage median time of the observation group was longer than 20 months whereas that of the control group was 20 months, and the difference was statistically significant (Log Rank examination χ2=10.623, P<0.001) (Table 1). The three marks of health index, emotion index and psychology index in life quality of the observation group were significantly higher than that of the control group, and the difference was statistically significant (P<0.05) (Table 2).
Table 2:
Comparison of life quality of patients (scores)
| Group | Health index | Emotion index | Psychology index |
|---|---|---|---|
| Control group | 15.3±4.2 | 60.5±8.4 | 9.4±2.2 |
| Observation group | 6.6±3.3 | 39.7±7.6 | 4.6±1.3 |
| t | 7.528 | 6.349 | 6.434 |
| P | <0.001 | <0.001 | <0.001 |
Discussion
The present study emphasized correct puncture technique through professional nursing strategies of internal fistula and patient-orientation, adopted actively existing high-risk factor of arteriovenous fistula dysfunction in multiple ways, increased knowledge of patient’s internal fistula protection and valued nursing procedures. The complication rate and dysfunction rate during internal fistula perioperative period of the observation group were significantly lower than that of the control group; the median time of internal fistula usage was significantly prolonged; the three marks of health index, emotion index and psychology index in life quality of the observation group were significantly higher than that of the control group. The differences were statistically significant.
Among patients needing fistulation, 97.9% of them needed psychological support and 95.7% of them paid much attention to surgical procedures, surgical methods, pains during operation and recovery time after operation (11). As a result, patients should be treated with kind and patient attitude in the nursing process and given individualized explanation, comfort and encouragement according to their age, educational level and cognition degree of disease so that they can ease misgivings and actively cooperate with doctors’ treatment. Dysfunction of internal fistula was the main cause for insufficient dialysis of patients, increasing admission rate and death rate.
About 52.63% of internal fistulas got blocked and needed reconstruction in the first year of usage (12). The reasons suggested for the observation: i) Puncture technique (8). Strictly conducting sterile operation was the most fundamental principle and the puncture point should be selected designedly; the intravenous needle should puncture toward the heart, and the arterial needle should puncture toward the anastomotic stoma; rope-ladder puncture technique was the first choice, should not use the method of fixed point; puncture angle had oblique puncture and straight puncture. Fixation method was an important segment of the whole puncture process; inappropriate fixation may cause needle rolling and slipping and pinpoint prickling, of which the main failure reasons were inappropriate technique of pasting adhesive tapes and it’s inappropriate length and width (13); ii) Hypotension, main cause for fistula acute blockage (14), may be resulted from inadequate estimation of patient’s body mass, diarrhea and hypoglycemia; iii) Own vessels, diabetes, arteriosclerosis, hyperlipidemia and high blood viscosity (15) ; iv) Infection of internal fistula may cause vascular intimal injury, activate growth factors, form fibrous tissue and lead to narrowing blood vessels; (v) Patient’s inadequate knowledge of internal fistulas and psychological status.
Limitations also existed in this study, for example, only 92 patients were enrolled in the study, thus the effects of our nursing strategy on CRF patients undergoing MHD treatment required to be explored by further study with a large sample size.
Conclusion
Professional fistula nursing strategy could prolong its service time, decrease complications and improve life quality.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgements
This study received no financial support. The authors declare that there is no conflict of interests.
References
- 1.Wang AY, Sherrington C, Toyama T, Gallagher M, Cass A, et al. (2016). Muscle strength, mobility, quality of life and falls in patients on maintenance haemodialysis: A prospective study. Nephrology (Carlton), 2. [DOI] [PubMed] [Google Scholar]
- 2.Chang HH, Chang YK, Lu CW, Huang CT, Chien CT, Hung KY, Huang KC, Hsu CC. (2016). Statins Improve Long Term Patency of Arteriovenous Fistula for Hemodialysis. Sci Rep, 6: 22197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robson JP., JR (2013). A review of hemodialysis vascular access devices: improving client outcomes through evidence-based practice. J Infus Nurs, 36: 404–10. [DOI] [PubMed] [Google Scholar]
- 4.Wilson B, Harwood L, Oudshoorn A. (2013). Moving beyond the “perpetual novice”: understanding the experiences of novice hemodialysis nurses and cannulation of the arteriovenous fistula. CANNT J, 23: 11–8. [PubMed] [Google Scholar]
- 5.Sousa CN, Figueiredo MH, Dias VF, Teles P, Apóstolo JL. (2015). Construction and validation of a scale of assessment of self-care behaviours anticipatory to creation of arteriovenous fistula. J Clin Nurs, 24: 3674–80. [DOI] [PubMed] [Google Scholar]
- 6.Huang JL, Jang JF, Lee KF, Shie YT, Jin MH. (2015). A Project to Reduce the Occlusion Rate in Hemodialysis Arteriovenous Access. Hu Li Za Zhi, 62: 13–20. [DOI] [PubMed] [Google Scholar]
- 7.Pellejero Palacio S, Lorente Martín S, Palomo García M, Rodriguez-Garcia J. (2014). [Health education to patients undergoing arteriovenous fistula]. Rev Enferm, 37: 34–40. [PubMed] [Google Scholar]
- 8.Adib-Hajbagheri M, Molavizadeh N, Alavi NM, Abadi MH. (2014). Factors associated with complications of vascular access site in hemodialysis patients in Isfahan Aliasghar hospital. Iran J Nurs Midwifery Res, 19: 208–14. [PMC free article] [PubMed] [Google Scholar]
- 9.Sousa CN, Teles P, Dias VF, Apóstolo JL, Figueiredo MH, Martins MM. (2014). Physical examination of arteriovenous fistula: The influence of professional experience in the detection of complications. Hemodial Int, 18: 695–9. [DOI] [PubMed] [Google Scholar]
- 10.Allon M, Robbin ML. (2002). Increasing arteriovenous fistulas in hemodialysis patients: Problems and solutions. Kidney Int, 62:1109–1124. [DOI] [PubMed] [Google Scholar]
- 11.Preljevic VT, Osthus TB, Sandvik L, Opjordsmoen S, Nordhus IH, Os I, Dammen T. (2012). Screening for anxiety and depression in dialysis patients: Comparison of the Hospital Anxiety and Depression Scale and the Beck Depression Inventory. J Psychosom Res, 73:139–144. [DOI] [PubMed] [Google Scholar]
- 12.Sousa CN, Apóstolo JL, Figueiredo MH, Martins MM, Dias VF. (2014). Interventions to promote self-care of people with arteriovenous fistula. J Clin Nurs, 23: 1796–802. [DOI] [PubMed] [Google Scholar]
- 13.Delfosse F, Boyer J, Lemaitre V, Inghels Y. (2012). Disconnection of arteriovenous fistula: standardize the coverage of the hemorragic risk. Nephrol Ther, 8: 23–34. [DOI] [PubMed] [Google Scholar]
- 14.Vahedian J, Jalayifar AM, Keramati MR, Nabavizadeh F, Vahedian M. (2012). Primary success of bifurcated vein patch arteriovenous fistula and Brescia-Cimino methods. Iran J Kidney Dis, 6: 124–8. [PubMed] [Google Scholar]
- 15.Murphy F. (2011). The ongoing challenges with renal vascular access. Br J Nurs, 20(4):S6, S8,, S10 passim. [DOI] [PubMed] [Google Scholar]