Abstract
Objectives
To assess the quality of life (QoL) of children suffering from juvenile idiopathic arthritis (JIA) in Poland, to compare QoL of children with JIA and healthy children, and to compare children’s and parents’ assessments of QoL.
Material and methods
The KIDSCREEN-52 questionnaire (children’s and parents’ version) was used to assess the quality of life. The QoL in JIA patients and healthy peers from European and Polish reference groups was compared by the t-test. The Bland-Altman method was used to evaluate child and parent assessment agreement.
Results
Eighty-nine questionnaires were obtained from children (median age: 14 years; 62% female; JIA history longer than 1 year) and 84 questionnaires from parents. The QoL of JIA patients was lower than in healthy peers from the European reference group in terms of physical well-being (p < 0.001), psychological well-being (p = 0.011), autonomy (p < 0.001) and social support and peers (p < 0.001). The QoL of JIA patients compared with the QoL of children from the Polish reference group was lower only in terms of physical well-being (p < 0.001), whereas it was higher in terms of moods and emotions (p = 0.023), parent relations and home life (p = 0.005) and financial resources (p < 0.001). In most terms the assessment performed by the parent was lower than the child’s. The most significant differences were observed for physical well-being (p < 0.001), psychological well-being (p = 0.016), and self-perception (p = 0.013).
Conclusions
The present study is the first assessment of QoL of JIA children in Poland. In our study the quality of life in JIA children was lower than in healthy peers. Discrepancies between the assessment of the child’s QoL performed by the child and the parent were found. Both assessments should be taken into account in clinical practice as well as in research studies.
Keywords: quality of life, juvenile idiopathic arthritis, KIDSCREEN
Introduction
The World Health Organization defines health as “a state of complete physical, mental and social well-being” [1]. Clinical studies and everyday medical practice focus on the analysis of somatic symptoms and the effects of their treatment, omitting the mental and social aspects. Guidelines for the treatment of chronic diseases rarely include issues relating to the mental and social dimension of patients’ life.
According to the holistic approach to man, the term “health-related quality of life” that appeared in the early 1990s does not relate only to subjective assessments based on the results of laboratory and imaging studies, but underlines the value of subjective assessment performed by the patient for the analysis of treatment outcomes [2]. Many authors demand that the study on the quality of life of the patients should be included in the clinical studies’ protocol and in the monitoring of treatment outcomes [3, 4].
The quality of life is particularly important for patients suffering from chronic diseases, including juvenile idiopathic arthritis (JIA). Juvenile idiopathic arthritis, known also as juvenile rheumatoid arthritis, is the most common form of chronic arthritis in children and adolescents, which affects the physical as well as emotional and sociological well-being of approximately 1 in 1000 children under the age of 16 years [5]. The disease causes pain, morning stiffness, and fatigue affecting normal lifestyle of children and their parents. Diagnostic procedures, stays in hospital, and side effects induced by drugs used in JIA treatment are sources of additional stress.
The current guidelines for the treatment of individual clinical manifestations of juvenile idiopathic arthritis focus on the “treat to target” concept. The main objective is to attain clinical remission of the disease activity defined as a parent- and child-acceptable symptom state [6].
Besides clinical parameters, the most frequently used instruments to assess the functional status include the Childhood Health Assessment Questionnaire (CHAQ), which evaluates the disability and the severity of pain in 8 domains (30 questions), and the Childhood Health Questionnaire (CHQ), which assesses the quality of life of children in terms of overall health, general and everyday physical functions, pain, behaviour, mood, self-esteem, emotional impact on parents and limitations of family activities.
The Juvenile Arthritis Quality of Life Questionnaire (JAQQ), less popular than the CHQ, was developed to study the quality of life of children suffering from JIA. It includes the VAS pain scale and 74 questions that define in 4 domains gross and fine motor skills, psychosocial functions as well as systemic reactions [7].
In the years 2001–2004 in 13 European countries, including Poland, the KIDSCREEN research project on the measurement of the health-related quality of life in children and adolescents was carried out. The project was financed by the European Union. An operational definition, underlining that the quality of life (QoL) has many different dimensions, was developed for the purpose of the project. According to the definition, the quality of life can be viewed as a “psychological construct which describes the physical, mental, social, psychological, and functional aspects of wellbeing and function from the patient perspective” [8].
The outcome of the project was 6 questionnaires in each language version: a long version with 52 questions, a medium version with 27 questions, and a short version with 10 questions (each version available for child and parent/caregiver). The questionnaires fulfil all methodology requirements for this type of research tool, including unidimensionality, internal consistency, reliability and validity. Questionnaires are designed for healthy and chronically ill children and adolescents aged between 8 and 18 years. The 52-item questionnaire measures health-related quality of life (HRQoL) across ten dimensions: physical well-being, psychological wellbeing, moods and emotions, self-perception, autonomy, parent relation and home life, financial resources, social support and peers, school environment, and social acceptance.
The aim of this study was to analyse the QoL of JIA patients in Poland, based on the assessment performed by children and their parents, to compare QoL of children with JIA and healthy children, and to compare children’s and parents’ assessments of QoL.
Material and methods
The KIDSCREEN-52 questionnaire was used to assess health-related quality of life in children suffering from JIA. The study was conducted from July 2014 to June 2015 among children and their parents in the paediatric outpatient clinic of the Institute of Rheumatology (at present: the National Institute of Geriatrics, Rheumatology and Rehabilitation) in Warsaw, Poland. The inclusion criteria were age from 8 to 18 years and JIA history longer than 1 year. The questionnaires were completed anonymously. The study was approved by the Ethics Committee of the Institute of Rheumatology in Warsaw, Poland.
The questionnaire included 52 items divided into 10 domains (Table I).
Table I.
Description of quality of life domains in KIDSCREEN-52 questionnaire
| KIDSCREEN domain | Number of items | Domain content | |
|---|---|---|---|
| 1 | Physical well-being | 5 | physical activity level, energy and fitness |
| 2 | Psychological well-being | 6 | positive emotions and satisfaction with life |
| 3 | Moods & emotions | 6 | depressive moods and stressful feelings |
| 4 | Self-perception | 5 | satisfaction with appearance and clothes |
| 5 | Autonomy | 5 | opportunity to create social and leisure time |
| 6 | Parent relation & home life | 6 | relationship with parents and atmosphere at home |
| 7 | Financial resources | 3 | availability of financial resources |
| 8 | Social support & peers | 6 | relationship with other children |
| 9 | School environment | 6 | feelings about school: learning, concentration, relationship with teachers |
| 10 | Bullying (social acceptance) | 3 | rejection by peers |
The questions related to the last week. The respondents replied to the questions on a 5-point Likert scale. The questions on frequency could be answered as follows: 1 – never, 2 – seldom, 3 – sometimes, 4 – often, 5 – always. The questions on feelings intensity had the following options: 1 – not at all, 2 – slightly, 3 – moderately, 4 – very, 5 – extremely. The outcome of the study was the sum of all scores on a given scale. Some of the questions (negatively formulated) had to be reverse-coded while calculating the results. The larger the sum of scores, the higher is quality of life. According to the KIDSCREEN handbook the total raw scores from the ten dimensions were converted into T values with a mean of 50 and a standard deviation (SD) of 10. T values of the study (T-JIA) were compared to T values of the European general population (T-Eur) and T values of the Polish population (T-Pol) presented in the KIDSCREEN handbook [9].
All questionnaire variables were expressed as the mean and standard deviation (SD). Comparisons of the study results and reference data were conducted using the t-test. Normality of variables’ distribution was checked by the Shapiro-Wilk test. Some of the variables (5 from 20) were not normally distributed. However, to allow data comparisons with results of other studies and because of a reasonably large sample size we decided to use the t-test and mean and SD values for all variables. The effect of JIA’s influence on HRQoL was calculated by Cohen’s d effect size coefficient defined by the difference between means divided by standard deviation. The effect size coefficient d > 0 indicates higher HRQoL in JIA children than in children from the reference group, while conversely d < 0 indicates lower HRQoL in JIA children than in the reference group. Values of d ≈ 0.2 indicate a small, d ≈ 0.5 a medium and d ≥ 0.8 a large effect.
The assessment agreement between children and parent assessment was evaluated by the Bland-Altman method (mean difference and 95% limits of agreement for each comparison were calculated) and paired t-test. In all calculations a p value of less than 0.05 was considered statistically significant.
All analyses were conducted using STATISTICA software, version 10.0.
Results
Eighty-nine questionnaires completed by children and 84 questionnaires completed by parents/caregivers were obtained. Fifty-five girls (62%) and 34 boys (38%) participated in the study. The median age was 14 years (interquartile range: 11–16).
The caregiver questionnaires were most often completed by the parents: 58 mothers (69%) and 21 fathers (25%). Only 5 questionnaires (6%) were completed by other caregivers.
Quality of life assessment made by child
The quality of life assessed by the children in all 10 domains is presented in Table II. The T value of children with JIA (T-JIA) was compared with European (T-Eur) and Polish (T-Pol) reference values [9]. HRQoL values for JIA patients in comparison with reference values for European children were significantly lower in 4 out of 10 domains: physical well-being, psychological well-being, autonomy and social support & peers (Cohen’s d: –0.8, –0.3, –0.4 and –0.6, respectively). However, in comparison with reference values for Polish children, these values were lower in one domain only: physical well-being (Cohen’s d: –0.7), whereas in 3 domains – moods & emotions, parent relations & home life and financial resources – T-JIA values were higher than Polish reference values.
Table II.
KIDSCREEN-52 child scores; comparison between JIA children (T-JIA) and European general population of healthy children (T-Eur) and Polish general population of healthy children (T-Pol)
| Children | n | T-JIA mean (SD) | T-JIA – T-Eur | T-JIA – T-Pol | ||||
|---|---|---|---|---|---|---|---|---|
| difference | p | effect size | difference | p | effect size | |||
| Physical well-being | 89 | 42.23 (9.28) | –7.77* | < 0.001 | –0.8 | –6.81* | < 0.001 | –0.7 |
| Psychological well-being | 89 | 46.78 (11.66) | –3.22* | 0.011 | –0.3 | 1.30 | 0.297 | 0.1 |
| Moods & emotions | 89 | 51.43 (10.72) | 1.43 | 0.210 | 0.1 | 2.63* | 0.023 | 0.3 |
| Self-perception | 88 | 49.34 (9.77) | –0.66 | 0.526 | –0.1 | 0.70 | 0.505 | 0.1 |
| Autonomy | 88 | 46.37 (8.44) | –3.63* | < 0.001 | –0.4 | –0.09 | 0.917 | 0.0 |
| Parent relation & home life | 89 | 49.85 (10.24) | –0.15 | 0.891 | 0.0 | 3.15* | 0.005 | 0.3 |
| Financial resources | 88 | 48.41 (9.43) | –1.59 | 0.117 | –0.2 | 4.73* | < 0.001 | 0.5 |
| Social support & peers | 89 | 44.09 (10.61) | –5.91* | < 0.001 | –0.6 | –1.23 | 0.277 | –0.1 |
| School environment | 87 | 47.75 (10.25) | –2.25* | 0.043 | –0.2 | 1.56 | 0.160 | 0.2 |
| Bullying | 88 | 51.91 (8.98) | 1.91* | 0.049 | 0.2 | 3.03 | 0.305 | 0.3 |
Statistically significant differences, p < 0.05.
Quality of life assessment made by parent/caregiver
Quality of life assessment made by parent/caregiver is presented in Table III. The largest difference between European reference values and T-JIA was observed for physical well-being (d = –1.7). Also significantly lower T-JIA values (compared with T-Eur values) were obtained for psychological well-being, self-perception, financial resources, social support & peers, and school environment. As to the comparison with the Polish reference group, significantly lower T-JIA values were observed for physical well-being and social support & peers, whereas significantly higher values in JIA patients, compared with healthy Polish peers, were observed for autonomy, parent relation & home life and financial resources.
Table III.
KIDSCREEN-52 parent scores; comparison between scores of parents of children with JIA (T-JIA) and European general population of parents of healthy children (T-Eur) and Polish general population of parents of healthy children (T-Pol)
| Parents/caregivers | n | T-JIA mean (SD) | T-JIA – T-Eur | T-JIA – T-Pol | ||||
|---|---|---|---|---|---|---|---|---|
| difference | p | effect size | difference | p | effect size | |||
| Physical well-being | 80 | 32.70 (7.76) | –17.30* | < 0.001 | –1.7 | –12.89* | < 0.001 | –1.3 |
| Psychological well-being | 83 | 44.79 (12.47) | –5.21* | < 0.001 | –0.5 | 1.39 | 0.314 | 0.1 |
| Moods & emotions | 84 | 51.19 (11.63) | 1.19 | 0.351 | 0.1 | 1.46 | 0.253 | 0.1 |
| Self-perception | 84 | 47.33 (9.06) | –2.67* | 0.008 | –0.3 | –1.41 | 0.159 | –0.1 |
| Autonomy | 84 | 47.82 (10.86) | –2.18 | 0.069 | –0.2 | 2.50* | 0.038 | 0.2 |
| Parent relation & home life | 81 | 51.17 (11.60) | 1.17 | 0.367 | 0.1 | 3.84* | 0.004 | 0.4 |
| Financial resources | 79 | 47.01 (9.48) | –2.99* | 0.006 | –0.3 | 5.85* | < 0.001 | 0.6 |
| Social support & peers | 77 | 41.76 (10.33) | –8.24* | < 0.001 | –0.8 | –3.00* | 0.013 | –0.3 |
| School environment | 79 | 46.11 (9.47) | –3.89* | < 0.001 | –0.4 | 1.01 | 0.304 | 0.1 |
| Bullying | 83 | 51.08 (9.44) | 1.08 | 0.301 | 0.1 | 1.69 | 0.107 | 0.2 |
Statistically significant differences, p < 0.05.
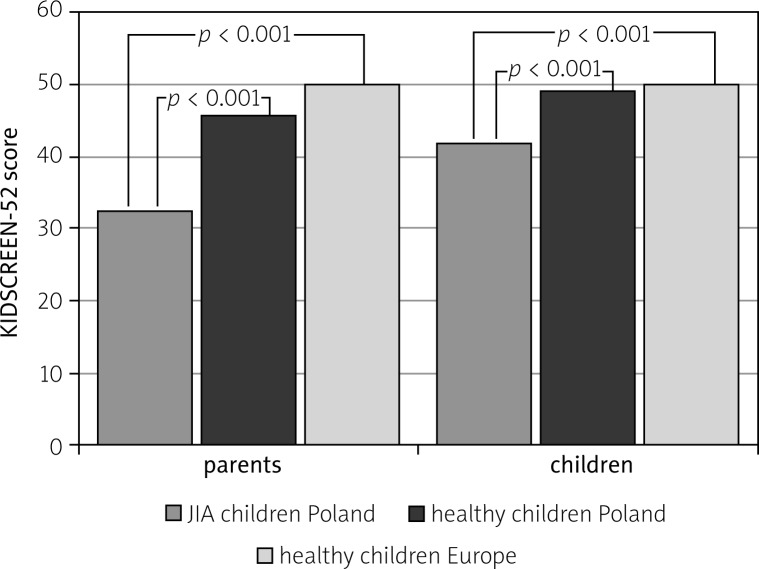
Physical well-being scores for JIA children, healthy children from Poland and healthy children from Europe in evaluation of children and parents are presented in Figure 1.
Fig. 1.
Physical well-being scores of KIDSCREEN-52 in JIA children and healthy peers in Poland and Europe, children and parents assessments.
Comparison of child’s and parent’s results
The assessment of the quality of life performed by the child differs from the assessment of child’s quality of life performed by the parent. In most dimensions the quality of the child’s life was assessed as lower by the parent than by the child. The differences were particularly noticeable in the following dimensions: physical well-being (p < 0.001), psychological well-being (p = 0.016), self-perception (p = 0.013), social support & peers (p = 0.031), and school environment (p = 0.040) (Table IV, Fig. 2).
Table IV.
Child and parent assessment agreement of child’s quality of life
| Dimension | n | Child [mean] | Parent [mean] | Difference | p |
|---|---|---|---|---|---|
| physical well-being | 79 | 43.08 | 32.64 | –10.44* | < 0.001 |
| psychological well-being | 82 | 47.43 | 44.48 | –2.95* | 0.016 |
| moods & emotions | 83 | 52.33 | 50.95 | –1.38 | 0.182 |
| self-perception | 82 | 49.72 | 47.28 | –2.44* | 0.013 |
| autonomy | 82 | 46.62 | 47.89 | 1.27 | 0.299 |
| parent relation & home life | 80 | 50.39 | 51.22 | 0.83 | 0.537 |
| financial resources | 77 | 48.75 | 46.93 | –1.82 | 0.112 |
| social support & peers | 76 | 44.63 | 41.72 | –2.91* | 0.031 |
| school environment | 77 | 48.36 | 45.95 | –2.41* | 0.040 |
| bullying | 82 | 52.13 | 50.98 | –1.15 | 0.337 |
Statistically significant differences, p< 0.05
Fig. 2.
Bland-Altman plots of child and parent assessment agreement for the following dimensions: physical well-being, psychological well-being, self-perception, social support & peers. Average value of the child and the parent assessment is presented on horizontal axis, whereas the difference between assessment values is presented on vertical axis. Mean assessment difference (bias) and the limits of agreement (–1.96*SD and +1.96*SD) are also presented.
Limitations of study
The present study was single-centred. The respondents replied to the questionnaire anonymously, which made it impossible to juxtapose the obtained data with their domicile, social and financial status. No clinical data on the severity of the disease, exact duration and treatment were obtained.
Discussion
To the best of our knowledge, the present study is the first analysis of the quality of life of children and adolescents suffering from JIA in Poland. In 2007 an international study on the quality of life of children with JIA was published, in which 30 children from Poland participated. However, the results were presented for the whole study group that included children from several Central and Eastern European countries, without dividing them into particular countries [10]. In 2010 a study on social adaptation and coping with the disease of children suffering from chronic rheumatic disease was conducted [11]. However, all quality of life dimensions of children with JIA have not been studied yet using dedicated questionnaires.
In the present study the value of children’s HRQoL was lower than in healthy children from the European reference group. This result is consistent with the results of studies conducted in other countries [12, 13]. In this study the lowest quality of life values compared with the healthy population of children from the reference group, both European and Polish, were observed in the physical well-being dimension. The questionnaire items in this dimension referred to general health, physical activity, and ability to run or ride a bike. The results of the study correspond with results of other researchers. Much lower quality of life in children with JIA in comparison with healthy children, especially in terms of functional ability, was observed by Haverman [14], during a study conducted in the Netherlands in 2010. A study carried out in the UK by Shaw et al. showed that the difficulties with regular physical activity constitute the greatest issue for half of the adolescents with JIA [7]. Kwon et al. [15] reported a high negative correlation (r = –0.74) between functional ability and overall HRQoL among adolescents with JIA.
We also revealed that QoL of JIA children in comparison with European data is lower in other dimensions: autonomy, social support and peers and school environment. This finding may significantly contribute to the management of young patients. Combining physical rehabilitation with programmes supporting social skills and improving communication with peers might constitute an important element that could improve QoL. The synthesis of many studies on the QoL of children with JIA carried out by Tong et al. [13] states: “Although physical therapy was believed to be important, children suggested exercises needed to be enjoyable and integrated among their other priorities, including school commitments. Children need ongoing access to psychosocial and educational support to promote adjustment and coping”. Békési [16], on the other hand, describes the positive influence of integration-recreational camps for chronically ill children on their quality of life, particularly in terms of self-perception.
The comparison of quality of life of JIA children with Polish reference data indicated lower values in children with JIA only in the physical domain. Significantly higher quality of life results in children with JIA, in comparison with healthy children, occurred in the following dimensions: moods and emotions, parent relation and home life, and financial resources. It might be the result of pampering ill children. The parents of children suffering from chronic disease dedicate more time to sick children, often at the expense of healthy siblings [17, 18], trying to satisfy their emotional and financial needs in order to compensate them for the distress relating to the disease [19]. On the other hand, Chaves et al. [20] noted that fulfilling the wishes of ill children results in the improvement of parents’ quality of life.
The KIDSCREEN-52 questionnaire was used in a study on the quality of life of children suffering from diabetes in Poland in 2010. The value of quality of life in the physical well-being dimension was slightly higher in children with diabetes (mean = 43.14) than in children with JIA in the present study (mean = 42.23). The values in other dimensions were similar or lower than in children with diabetes [21].
Another interesting result of the present study is the comparison of QoL assessment carried out by the child and the parent. The assessments differ in most dimensions. Particular differences were noted in the case of physical well-being, psychological well-being, social support & peers and self-perception. The quality of life assessed by the parent was lower than the quality of life assessed by the child. The results of studies carried out by other authors are inconclusive. Some authors found a high level of parent-child assessment agreement [22, 23], whereas others indicate many discrepancies [12, 24–26]. In the study by Brunner et al. [22] in most dimensions relating to physical health and disability level the parent-child assessment agreement was high, whereas in the dimensions relating to emotional functioning, worry and communication the level of agreement was low. Similarly, Lal et al. [23] found a high level of assessment agreement in terms of functional ability and only moderate agreement of pain and well-being assessments. These results would confirm the thesis that it is particularly difficult for parents to assess the psychological, social and emotional state of their children. However, the results of the study carried out by April et al. [24] were different: high assessment agreement was demonstrated for pain level, psychosocial function and systemic symptoms, whereas low assessment agreement was demonstrated for gross and fine motor functions. The study by Palermo et al. [25] described the discrepancies between the assessment of pain level and disability carried out by the parent and the child.
The discrepancy between the assessment carried out by the child and by the parent is an important issue, because the parent usually participates in the therapeutic process. The question is, whose assessment is more credible, the child’s or parent’s, and whose assessment should the physician trust? Some authors incline towards greater consideration of the child’s assessment because of the subjectivity of QoL assessment [27, 28]. It is, however, worth noting that the analysed parameters, such as pain or mood, are by definition subjective. As there is no tool allowing for the objective validation of the accuracy of particular assessments and, as mentioned above, parents play a fundamental role in the treatment of JIA patients, it seems appropriate to take into account both assessments. Eiser and Varni [29] and Vetter et al. [30] are of a similar opinion, underlining that the discrepancies between the child’s and parent’s assessment do not constitute a methodological mistake, but the perception of the same issue from two, equally important, perspectives. Therefore both assessments should be taken into consideration in clinical practice as well as in research studies.
One of the main objectives in the treatment of chronically ill patients is to improve their quality of life. It is still necessary to explain how the changes in clinical parameters influence the change in the quality of life. It appears that a medicine that slows down the disease activity should automatically improve the quality of life. This thesis, however, was not confirmed by Seid et al. [31], who determined that an innovative treatment with outstanding effects in slowing down JIA progression did not cause significant improvement in the children’s quality of life.
Conclusions
The results of the first study on the quality of life in children and adolescents with juvenile idiopathic arthritis in Poland were presented. In our study the quality of life in JIA children was lower than in healthy peers. A discrepancy between the quality of life assessment performed by the child and by the parent was observed: the parents’ assessments were lower. It indicates the necessity to take both assessments into consideration in further studies and clinical practice. It is necessary to monitor the quality of life of JIA patients. The quality of life assessment should constitute an inherent parameter in the assessment of the effectiveness of treatment used in children with inflammatory rheumatic diseases.
Acknowledgements
The study was supported from the statutory funds of the Rheumatology Institute (at present: the National Institute of Geriatrics, Rheumatology and Rehabilitation), Warsaw, Poland.
We would like to thank Mrs. Sylwia Ostrowska, Jolanta Dylewska and Marta Ługowska for assistance with questionnaires’ distribution.
The authors declare no conflict of interest.
References
- 1.Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference; 19–22 June, 1946; New York. signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948. [Google Scholar]
- 2.Oleś M. Jakość życia dzieci i młodzieży w zdrowiu i w chorobie. Lublin: Wydawnictwo KUL; 2010. [Google Scholar]
- 3.Luca NJ, Feldman BM. Health outcomes of pediatric rheumatic diseases. Best Pract Res Clin Rheumatol. 2014;28:331–350. doi: 10.1016/j.berh.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Calvert M, Blazeby J, Altman DG, et al. Reporting of patientreported outcomes in randomized trials: the CONSORT PRO extension. JAMA. 2013;309:814–822. doi: 10.1001/jama.2013.879. [DOI] [PubMed] [Google Scholar]
- 5.Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet. 2007;369:767–778. doi: 10.1016/S0140-6736(07)60363-8. [DOI] [PubMed] [Google Scholar]
- 6.Consolaro A, Negro G, Lanni S, et al. Toward a treat-to-target approach in the management of juvenile idiopathic arthritis. Clin Exp Rheumatol. 2012;30(4 Suppl 73):S157–S162. [PubMed] [Google Scholar]
- 7.Shaw KL, Southwood TR, Duffy CM, McDonagh JE. Healthrelated quality of life in adolescents with juvenile idiopathic arthritis. Arthritis Rheum. 2006;55:199–207. doi: 10.1002/art.21852. [DOI] [PubMed] [Google Scholar]
- 8.Ravens-Sieberer U, Gosch A, Rajmil L, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res. 2005;5:353–364. doi: 10.1586/14737167.5.3.353. [DOI] [PubMed] [Google Scholar]
- 9.The KIDSCREEN Group Europe. Handbook. Lengerich: Pabst Science Publishers; 2006. The KIDSCREEN Questionnaires – Quality of life questionnaires for children and adolescents. [Google Scholar]
- 10.Gutiérrez-Suárez R, Pistorio A, Cespedes Cruz A, et al. Pediatric Rheumatology International Trials Organisation (PRINTO). Health-related quality of life of patients with juvenile idiopathic arthritis coming from 3 different geographic areas. The PRINTO multinational quality of life cohort study. Rheumatology (Oxford) 2007;46:314–320. doi: 10.1093/rheumatology/kel218. [DOI] [PubMed] [Google Scholar]
- 11.Dobrucka-Janeczek I, Rutkowska-Sak L. Osobowość i przystosowanie dzieci chorych na przewlekłe choroby reumatyczne. Reumatologia. 2012;50:211–218. [Google Scholar]
- 12.Sawyer MG, Whitham JN, Roberton DM, et al. The relationship between health-related quality of life, pain and coping strategies in juvenile idiopathic arthritis. Rheumatology (Oxford) 2004;43:325–330. doi: 10.1093/rheumatology/keh030. [DOI] [PubMed] [Google Scholar]
- 13.Tong A, Jones J, Craig JC, et al. Children’s experiences of living with juvenile idiopathic arthritis: a thematic synthesis of qualitative studies. Arthritis Care Res (Hoboken) 2012;64:1392–1404. doi: 10.1002/acr.21695. [DOI] [PubMed] [Google Scholar]
- 14.Haverman L, Grootenhuis MA, van den Berg JM, et al. Predictors of health-related quality of life in children and adolescents with juvenile idiopathic arthritis: results from a Web-based survey. Arthritis Care Res (Hoboken) 2012;64:694–703. doi: 10.1002/acr.21609. [DOI] [PubMed] [Google Scholar]
- 15.Kwon HJ, Kim YL, Lee SM. Relation between functional ability and health-related quality of life of children with juvenile rheumatoid arthritis. J Phys Ther Sci. 2015;27:837–840. doi: 10.1589/jpts.27.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Békési A, Török S, Kökönyei G, et al. Health-related quality of life changes of children and adolescents with chronic disease after participation in therapeutic recreation camping program. Health Qual Life Outcomes. 2011;9:43. doi: 10.1186/1477-7525-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharpe D, Rossiter L. Siblings of children with a chronic illness: a meta-analysis. J Pediatr Psychol. 2002;27:699–710. doi: 10.1093/jpepsy/27.8.699. [DOI] [PubMed] [Google Scholar]
- 18.Besier T, Hölling H, Schlack R, et al. Impact of a family-oriented rehabilitation programme on behavioural and emotional problems in healthy siblings of chronically ill children. Child Care Health Dev. 2010;36:686–695. doi: 10.1111/j.1365-2214.2010.01085.x. [DOI] [PubMed] [Google Scholar]
- 19.Hentinen M, Kyngäs H. Factors associated with the adaptation of parents with a chronically ill child. J Clin Nurs. 1998;7:316–324. doi: 10.1046/j.1365-2702.1998.00154.x. [DOI] [PubMed] [Google Scholar]
- 20.Chaves C, Hervas G, Vazquez C. Granting wishes of seriously ill children: Effects on parents’ well-being. J Health Psychol. 2016;21:2314–2327. doi: 10.1177/1359105315576348. [DOI] [PubMed] [Google Scholar]
- 21.Oleś M. Subiektywna jakość życia u nastolatków przewlekle chorych – analiza na przykładzie cukrzycy typu 1. Psychologia Jakości Życia. 2010;9:21–45. [Google Scholar]
- 22.Brunner HI, Klein-Gitelman MS, Miller MJ, et al. Health of children with chronic arthritis: relationship of different measures and the quality of parent proxy reporting. Arthritis Rheum. 2004;51:763–773. doi: 10.1002/art.20689. [DOI] [PubMed] [Google Scholar]
- 23.Lal SD, McDonagh J, Baildam E, et al. Agreement between proxy and adolescent assessment of disability, pain, and well-being in juvenile idiopathic arthritis. J Pediatr. 2011;158:307–312. doi: 10.1016/j.jpeds.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.April KT, Feldman DE, Platt RW, et al. Comparison between Children with Juvenile Idiopathic Arthritis (JIA) and their parents concerning perceived Quality of Life. Qual Life Res. 2006;15:655–661. doi: 10.1007/s11136-005-3690-1. [DOI] [PubMed] [Google Scholar]
- 25.Palermo TM, Zebracki K, Cox S, et al. Juvenile idiopathic arthritis: parent-child discrepancy on reports of pain and disability. J Rheumatol. 2004;31:1840–1846. [PubMed] [Google Scholar]
- 26.Vanoni F, Suris JC, von Scheven-Gête A, et al. The difference of disease perception by juvenile idiopathic arthritis patients and their parents: analysis of the JAMAR questionnaire. Pediatr Rheumatol Online J. 2016;14:2. doi: 10.1186/s12969-015-0063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheffler LC, Hanley C, Bagley A, et al. Comparison of self-reports and parent proxy-reports of function and quality of life of children with below-the-elbow deficiency. J Bone Joint Surg Am. 2009;91:2852–2859. doi: 10.2106/JBJS.H.01108. [DOI] [PubMed] [Google Scholar]
- 28.Yi-Frazier JP, Hilliard ME, Fino NF, et al. Whose quality of life is it anyway? Discrepancies between youth and parent health-related quality of life ratings in type 1 and type 2 diabetes. Qual Life Res. 2016;25:1113–1121. doi: 10.1007/s11136-015-1158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eiser C, Varni JW. Health-related quality of life and symptom reporting: similarities and differences between children and their parents. Eur J Pediatr. 2013;172:1299–1304. doi: 10.1007/s00431-013-2049-9. [DOI] [PubMed] [Google Scholar]
- 30.Vetter TR, Bridgewater CL, McGwin G., Jr An observational study of patient versus parental perceptions of health-related quality of life in children and adolescents with a chronic pain condition: who should the clinician believe? Health Quality of Life Outcomes. 2012;10:85. doi: 10.1186/1477-7525-10-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seid M, Opipari L, Huang B, et al. Disease control and health-related quality of life in juvenile idiopathic arthritis. Arthritis Rheum. 2009;61:393–399. doi: 10.1002/art.24477. [DOI] [PMC free article] [PubMed] [Google Scholar]