Abstract
Background
In 2001, calculations in models based on atomic bomb survivors indicated that children exposed to ionizing radiation by computed tomography (CT) would be expected to have an increased risk of cancer. This led to the issuance of new recommendations in Germany concerning CT in children.
Methods
We analyzed data from the German pediatric CT cohort study together with data on children from a large general statutory health insurance provider (AOK) in order to characterize the secular trend in the use of CT in Germany. We used information from the Picture Archiving and Communication System (PACS) to estimate individual organ doses per scan and their development over time.
Results
The number of CT scans performed on children in Germany each year declined by 29% from 2006 to 2012. Over the same period, younger children were exposed to lower organ doses during CT scanning, although some organ doses were higher in neonates than in older children. The highest organ doses were in the 7.6 to 12.5-year-old age group and affected the brain (37.12 mGy ± 19.68 mGy) and the lenses (41.24 mGy ± 20.08 mGy). In every age group, the organ doses declined from year to year. With approximately 21 000 children aged 0–13 undergoing CT each year (extrapolated from insurance data of 2008), one can expect 2.3 [-1.7; 6.3] additional new cases of leukemia and 1 [-2.3; 4.0] additional new tumor of the central nervous system to arise each year.
Conclusion
In view of the risks, children should undergo CT only for the indications listed by the German Commission on Radiological Protection (Strahlenschutzkommission). Further epidemiological studies are needed for estimation of the risk associated with the use of newer CT technology.
Computed tomography (CT) is an indispensable tool in modern medical diagnosis. The use of CT has grown continuously since its introduction in the 1970s (1– 3). Despite the benefits, however, CT entails exposure to ionizing radiation. This is a risk factor for cancer, and the danger is highest after exposure in childhood (4).
The average radiation exposure for residents of Germany is ca. 4 mSv per annum, half of which (1.9 mSv) comes from medical diagnostic procedures (5). CT scans produce much higher doses per examination (1.7–16.4 mSv) than conventional radiographic techniques (<0.01–1.1 mSv) (5). The proportion of total exposure due to CT in Germany has risen in recent years, and currently CT accounts for ca. 60% of the radiation exposure from diagnostic examinations (5).
Beginning in 1999, a number of projects were carried out in the framework of the Concerted Action for CT Dose Reduction (Konzertierte Aktion Dosisreduktion CT) (6). In 2006 the German Commission on Radiological Protection issued new recommendations for CT examinations of children (7). According to these recommendations, sonography and magnetic resonance imaging should take priority over CT in all but exceptional circumstances. When CT has to be used, the dose should be the minimum required to achieve the aim of the examination. Moreover, the apparatus and protocols must be adapted to the pediatric patient (7).
As early as 2001, model calculations based on data from atom bomb survivors indicated that the risk of developing cancer after exposure to ionizing radiation is higher in childhood (8). Cohort studies from Great Britain (9), Australia (10), Taiwan (11), France (12), and Germany (13) published since 2012 (table 1) show an elevated risk of cancer following exposure to ionizing radiation via CT in childhood and adolescence. Increased risks of leukemia and brain tumors were reported (9– 11). The methods and results of these studies have been the subject of criticism (12– 17), among other reasons because the exposed children may have a higher risk of cancer owing to their underlying disease and because of the wide variation in the definition of the latency period between CT exposure and cancer occurrence (18). The French (12) and German (13) studies, in common with a new study from England (14), included previous illnesses in their analyses and found that the risks, albeit raised, were much lower than in previous investigations.
Table 1. Comparison of risk estimators in published cohort studies of cancer risk following computed tomography (CT) in childhood.
| Country (study) | Year | Study population | Risk estimator | Comparison | Leukemia | Brain/CNS tumors | ||
| Cases | Risk estimator [95% CI] | Cases | Risk estimator [95% CI] | |||||
| Great Britain (9) | 2012 | 178 604 | RR | 0–5 versus 50 mGy | 74 | 3.18 [1.46; 6.94] |
135 | 2.82 [1.33; 6.03] |
| Australia (10) | 2013 | 10 939 680 | IRR | CT versus no CT | 211 | 1.23 [1.08; 1.41] |
283 | 2.13 [1.88; 2.41] |
| Taiwan (11) | 2014 | 122 086 | HR | Head CT versus no CT | 17 | 1.9 [0.82; 4.40] |
30 | 2.56 [1.44; 4.45] |
| France (12) | 2015 | 67 274 | RR* | CT versus no CT | 25 | 1.57 [0.21; 2.93] |
27 | 1.22 [0.84; 1.61] |
| Germany (13) | 2015 | 44 584 | SIR | CT versus general population | 12 | 1.72 [0.89; 3.01] |
7 | 1.35 [0.54; 2.78] |
| Great Britain (14) | 2016 | 178 254 | RR* | CT versus no CT | 67 | 1.20 [0.89; 1.89] |
107 | 1.10 [1.02; 1.26] |
*Our calculations (18);
CI, confidence interval; HR, hazard ratio; IRR, incidence rate ratio; RR, relative risk; SIR, standardized incidence ratio
All of these studies used retrospectively acquired data, so the current risks are difficult to estimate. Assuming that the recommendations of the German Commission on Radiological Protection are followed, two hypotheses for exposure of pediatric patients emerge: (a) the younger the age group, the more the frequency of CT scanning should decrease, and the rate should go down with the passage of time; (b) the doses used for the different CT examinations should decrease with time.
The aim of this article is to assess the elevated cancer risks described in the epidemiological studies with regard to:
The frequency and distribution of pediatric CT examinations
The radiation dose entailed by CT.
Methods
The following analyses are based on figures from the Scientific Institute of the AOK, a large German general statutory health insurance provider (WIdO) (18), and data from the German cohort study KiCT (a study on the risk of cancer incidence in children after exposure to ionizing radiation from computed tomography) (13).
AOK data
We extracted from the AOK data for the period 1 January 2006 to 31 December 2012 the details of all insurees for whom at least one CT examination was billed according to the standard German EBM (Uniform Value Scale) or OPS (Classification of Operations and Procedures) criteria for medical services and who were not older than 12 years at the time of examination. The age in years at time of examination was pre-aggregated into <1, 1 to ≤ 5, and 6 to ≤ 12 for reasons of data protection. The numbers of patients and CT examinations were extrapolated to the German residential population matched for age and sex, and CT scans per 10 000 insurees were calculated. This yields the number of CT examinations per 10 000 insurees for the group of all insurees (18). For comparison with the data of our cohort study we also present the data for all AOK insurees up to the age of 12 years who had at least one CT examination in 2008 and who did not have any kind of cancer in the year of investigation (etable 1).
eTable 1. EBM codes, OPS codes, and diagnoses.
| EBM and OPS codes included in analysis | |
| Catalogue | Codes |
| EBM | 34310 bis 34344, 34350–34351 |
| OPS | 3–20, 3–22, 3–24, 3–26, 3–72, 3–73, 3–75 |
| EBM and OPS codes and diagnoses that led to exclusion from subanalysis | |
| Catalogue | Codes |
| ICD-10 | C00-D48.9 |
| EBM | 25210, 25211, 25213, 25320–25323, 25330–25333, 34360 |
| OPS | 1940, 1941, 3708.0, 3709.0, 370c.1, 3762, 5015.0, 5015.1, 5015.3, 5015.4, 5016.0, 5016.2, 5016.4, 5016.6, 5017.1, 5035.0, 5035.2, 5035.4, 5035.6, 5399.5–5399.7, 5399.b-5399.d, 5492.02, 5506, 5547, 5591.1, 5651.9**, 5820.2**, 5821.15, 5821.29, 5821.33, 5821.43, 5821.53, 5821.6, 5821.63, 5821.e, 5821.f4, 5822.9**, 5839.8, 5852.8**, 5852.9**, 6003.6, 852, 853, 854, 8600, 8601, 8602, 8603, 8918, 5410.00, 5410.01, 5410.10, 5410.11, 5411.00, 5411.01, 5411.20, 5411.22, 5411.23, 5411.30, 5411.31, 5411.40, 5411.41, 5411.50, 5411.51, 8542, 8543, 8544.0, 8544.1, 8547.0–8547.2, 8802.50–8802.52, 8805.00–8805.02, 8805.20, 8805.22, 8805.23, 8805.30, 8805.31, 8805.40, 8805.41, 8805.50, 8805.51, 8805.6 |
EBM, Uniform Value Scale (Physicians' Fee Schedule); OPS, Classification of Operations and Procedures; ICD-10, International Statistical Classification of Diseases and Related Health Problems
KiCT-RIS data
From the radiological information systems (RIS) of 20 German hospitals we extracted data for all patients under 15 years of age who had undergone at least one CT scan within the period 1 January 1980 to 31 December 2010 and were resident in Germany at the time of examination (13). The cohort was compared with the data of the German Childhood Cancer Registry (GCCR) (19). Because exposure to ionizing radiation does not immediately lead to cancer, we defined a latency period of 2 years (13). The latency period is the symptom-free interval between the first exposure to a noxa and the occurrence of the first symptoms of the disease caused by the noxa. Accordingly, persons in whom the disease arises within the latency period and those for whom the end of the latency period falls outside the study period are excluded from analysis.
KiCT-PACS data
From the picture archiving and communication systems (PACS) of 18 of the 20 hospitals we used the software PerMoS (20) to select all CT examinations of the cohort members between 1997 and 2013 at the time of data acquisition and extracted technical parameters from the Digital Imaging and Communications in Medicine (DICOM) headers (21). After adjustment of the extracted data (e.g. exclusion of reconstructions) organ doses were calculated using the National Cancer Institute Dosimetry System for CT (NCICT beta version 2.2) (22), which features conversion factors for all established CT models and pediatric hybrid phantoms (models of the human body from real data and mathematical models) (23).
To estimate the extent to which the KiCT cohort was representative, the distribution of some characteristics was compared with the projected health insurance data. The reported age groups differ for technical reasons and were adjusted as far as possible. The KiCT-RIS age groups differ from those of the AOK because the data sets were compiled for internal analyses. The KiCT-PACS age groups are oriented on the hybrid phantoms. (Figures 1 and 2) were generated with R (Version 3.2.5; R Development Core Team, 2013), while all other analyses were conducted using SAS (Vers. 9,4, SAS Institute Inc.).
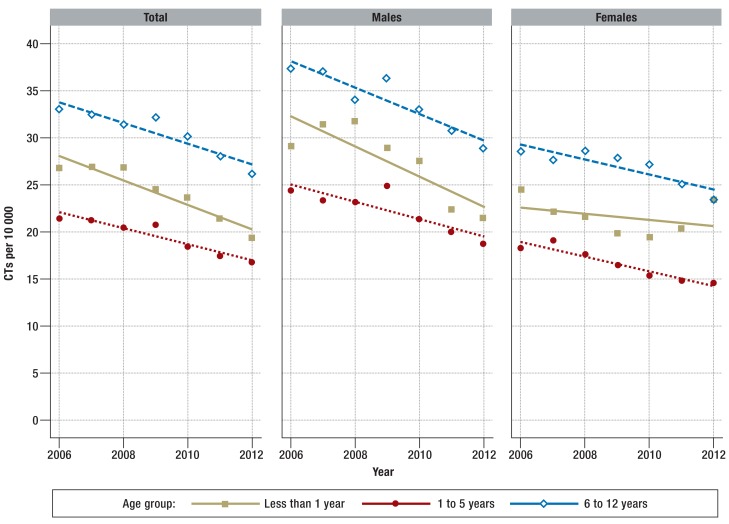
Figure 1.
Computed tomography examinations (CTs) in children per 10 000 insured persons from 2006 to 2012, by age and sex
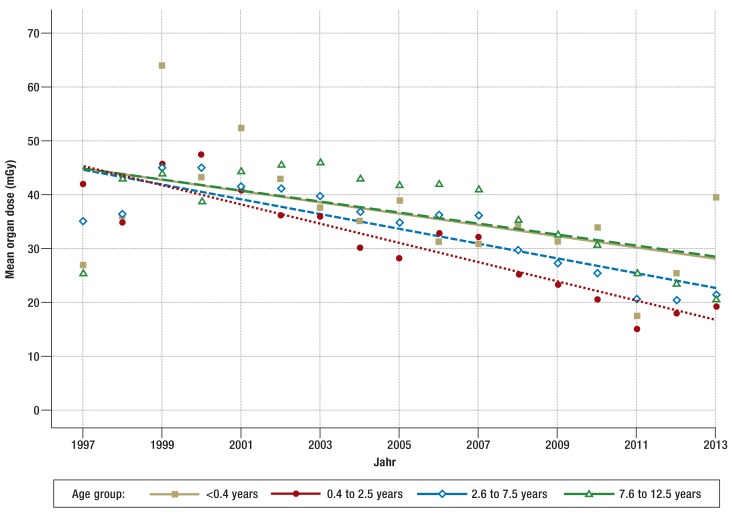
Figure 2.
Mean organ dose to the brain on computed tomography of the head by age group from 1997 to 2013, with regression lines (KiCT-PACS, n = 16 518).
KiCT, study on the risk of cancer incidence in children after exposure to ionizing radiation from computed tomography; PACS, picture archiving and communication system
Results
CT exposure
Data on a total of 50 692 insured persons under 13 years of age (subanalysis 2008: 7400 insurees) were taken from the AOK records. Age- and sex-adjusted extrapolation to the German residential population reveals ca. 35 000 examinations per annum. The extrapolated figures show a 29% decrease in CT examinations from 40 757 in 2006 to 28 933 in 2012.
Figure 1 presents the number of CT scans per 10 000 insured persons by age group. The number of examinations decreases for both sexes in each age group from 2006 to 2012.
The KiCT study included 44 584 children with 71 073 CT scans from KiCT-RIS and 13 238 children with 26 212 CT scans from KiCT-PACS (table 2). In KiCT-RIS 15% of the originally included children were excluded because of an existing cancer (14).
Table 2. Numbers of persons and CT scans by sex and age at time of examination in the AOK and KiCT data sets.
| AOK*1, 2 | KiCT-RIS | KiCT-PACS | |||||
| Persons | CTs | Persons | CTs | Persons | CTs | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Study population | 20 864 (100) | 28 993 (100) | 44 584 (100) | 71 073 (100) | 13 238 (100) | 26 212 (100) | |
| Period | 2008 | 1983–2008 | 1997–2013 | ||||
| Age range (years) | 0–12 | 0–13 | 0–12.5 | ||||
| Sex | Male | 12 019 (58) | 16 899 (58) | 26 146 (59) | 41 896 (59) | 7967 (60) | 15 816 (60) |
| Female | 8 845 (42) | 12 093 (42) | 18 387 (41) | 29 100 (41) | 5271 (40) | 10 396 (40) | |
| Unknown | – | – | 51 (0) | 77 (0) | – | – | |
| Age at CT*3 | Age category | ||||||
| 1 | – | < 1: 2547 (9) | – | < 1: 7148 (10) | – | < 0.4: 1174 (4) | |
| 2 | – | 1 ≤ 5: 7844 (27) | – | 1 ≤ 4: 18 822 (26) | – | 0.4 ≤ 2.5: 5060 (24) | |
| 3 | – | 6 ≤ 12: 18 602 (64) | – | 5 ≤ 9: 20 913 (29) | – | 2.6 ≤ 7.5: 9309 (36) | |
| 4 | – | – | – | 10 ≤ 13: 24 190 (34) | – | 7.6 ≤ 12.5: 10 669 (41) | |
*1Estimated for the German residential population, adjusted for sex and age, on the basis of data from persons insured by the AOK in the year 2008 after exclusion of persons receiving cancer-associated services in the billing year
*2Because these are extrapolated data, the totals for the individual AOK age groups may add up to less than the overall number of examinations.
*3Different age categories (1– 4) for AOK, KiCT-RIS, and KiCT-PACS
CT, computed tomography; KiCT, study on the r isk of cancer incidence in children after exposure to ionizing radiation from CT; RIS, radiological information systems;
PACS, picture archiving and communication system
In 2008, extrapolated to the German residential population, 36 436 CT examinations in 24 760 patients were billed. Of these patients, 15.7% (3896 patients, 7443 examinations) underwent CT in the course of cancer diagnosis and were therefore excluded. The extrapolated sex and age distribution were similar to those in KiCT-RIS. The age distribution in the KiCT-PACS data diverges from the other data sets.
All data sources showed that boys underwent CT more often than girls and that the head was most commonly examined. Scans of the head and neck made up 65 to 69% of all CT examinations. The chest and abdomen were examined in 13 to 26% of cases (etable 2). However, the numbers of head CT scans as a proportion of the total decreased with increasing age.
eTable 2. Distribution of exposed body regions by age.
|
Body region examined |
AOK by age (years) | KiCT-RIS by age (years) | KiCT-PACS by age (years) | |||||||||||
| < 1 | 1 ≤ 6 | 6 ≤ 12 | ∑ | < 1 | 1 ≤ 5 | 5 ≤ 10 | 10 ≤ 13 | ∑ | < 0.4 | 0.4 ≤ 2.5 | 2.6 ≤ 7.5 | 7.6 ≤ 12.5 | ∑ | |
| Head (%) | 82 | 70 | 62 | 66 | 71 | 73 | 67 | 58 | 66 | 52 | 69 | 64 | 61 | 63 |
| Neck (%) | 1 | 2 | 1 | 1 | 1 | 3 | 4 | 4 | 3 | 2 | 1 | 3 | 2 | 2 |
| Chest (%) | 9 | 8 | 6 | 7 | 16 | 11 | 10 | 11 | 11 | 30 | 18 | 19 | 19 | 19 |
| Abdomen (%) | 3 | 6 | 6 | 6 | 3 | 3 | 5 | 6 | 5 | 7 | 5 | 6 | 6 | 6 |
| Pelvis (%) | 0 | 3 | 2 | 2 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 1 | 2 | 1 |
| Limbs (%) | 0 | 1 | 10 | 6 | 0 | 1 | 3 | 8 | 4 | 1 | 0 | 1 | 1 | 1 |
| Whole body* (%) | 2 | 8 | 11 | 9 | 3 | 5 | 6 | 7 | 6 | 9 | 6 | 8 | 9 | 8 |
| Unknown (%) | 3 | 2 | 2 | 2 | 4 | 3 | 4 | 5 | 4 | 0 | 0 | 0 | 0 | 0 |
| ∑ | 9 | 27 | 64 | 100 | 10 | 26 | 29 | 34 | 100 | 4 | 19 | 36 | 41 | 100 |
*All examinations in which more than one region of the body was exposed. KiCT, s tudy on the r isk of cancer incidence in children after exposure to ionizing radiation from computed tomography; RIS, radiological information system; PACS, picture archiving and communication system
Organ dose
The absorbed radiation dose could be reconstructed for 26 212 examinations at 18 of the hospitals in the cohort study for the period from 1997 to 2013. In head CT the highest organ doses were recorded for the brain and for the lenses of the eyes (table 3). The mean organ doses per CT scan are lower for children aged 0.4 to 2.5 years than for newborns but then rise with increasing age. The organ dose for the thyroid gland is highest in newborns, at 7.04 mGy per examination. For thoracic CT the mean organ doses for bone marrow, thyroid gland, lung, breast, and heart wall increase with age. For example, the mean bone marrow dose is 1.6 mGy for newborns but 2.1 mGy in the highest age category. The mean organ dose for the large intestine on abdominal CT varies between 6 and 13 mGy.
Table 3. Organ doses for selected regions of the body by age (KiCT-PACS data set).
| Mean organ dose in mGy (standard deviation) | |||||
| Age in years | |||||
| Body region | Organ | < 0.4 | 0.4 ≤ 2.5 | 2.6 ≤ 7.5 | 7.6 ≤ 12.5 |
|
Head (n = 16 518) |
Bone marrow | 10.8 (7.4) | 11 (7.47) | 11.43 (6.95) | 7.2 (3.98) |
| Brain | 34.72 (23.8) | 28.13 (19.21) | 32.78 (19.28) | 37.12 (19.68) | |
| Lens of eye | 36 (23.6) | 30.26 (18.86) | 36.78 (20.15) | 41.24 (20.08) | |
| Thyroid gland | 7.04 (5.45) | 3.37 (2.65) | 3.18 (2.09) | 3.32 (2.36) | |
|
Chest (n = 5032) |
Bone marrow | 1.62 (3.5) | 1.73 (2.46) | 1.53 (2.29) | 2.11 (2.69) |
| Thyroid gland | 3.77 (7.31) | 4.95 (6.76) | 7.19 (9.61) | 6.06 (7.06) | |
| Lung | 4.53 (9.33) | 5.38 (7.49) | 7.22 (11.11) | 8.4 (10.98) | |
| Breast* | 3.9 (7.38) | 4.82 (7.1) | 6.38 (11.53) | 7.1 (8.03) | |
| Heart wall | 4.7 (9.69) | 5.44 (7.6) | 7.53 (11.88) | 8.72 (11.52) | |
|
Abdomen (n = 1457) |
Bone marrow | 2.67 (3.22) | 1.87 (2.29) | 2.25 (2.36) | 3.32 (3.1) |
| Breast* | 1.28 (1.15) | 2.08 (2.21) | 8.33 (8.64) | 1.28 (1.15) | |
| Large intestine | 13.36 (20.19) | 6.06 (7.17) | 10.9 (11.42) | 13.2 (13.27) | |
| Ovaries* | 6.63 (11.82) | 5.52 (6.48) | 8.82 (9.69) | 7.61 (7.55) | |
| Testicles* | 1.46 (2.05) | 0.62 (0.86) | 0.82 (0.91) | 0.64 (0.62) | |
*Calculated only for males or females respectively
KiCT, s tudy on the r isk of cancer incidence in children after exposure to ionizing radiation from computed tomography; PACS, picture archiving and communication system
All organ doses are becoming progressively lower. Figure 2 shows the change in the mean brain dose for CT of the head between 1997 and 2013.
Risk assessment
Thirty-nine cases of cancer occurring at least 2 years after the first known CT examination were registered in the KiCT cohort: 12 leukemias, 7 CNS tumors, 9 solid tumors, and 11 lymphomas (13).
Data on the same age group in the German residential population indicate that the expected number of cases in the KiCT cohort would be 7 leukemias and 5.2 CNS tumors. Leukemia thus occurred 1.72 times more often than expected (observed: 12) and CNS tumors 1.35 times more often (observed: 7) (13). Therefore, 5 leukemias and 1.8 new CNS tumors could have been caused by CT. On the assumption that each year ca. 21 000 children under 13 years of age are exposed to CT (estimation based on the AOK data from 2008), 2.3 additional cases of leukemia (95% confidence interval [CI] [-1.7; 6.3]) and 1 additional CNS tumor (95% CI [-2.3; 4.0]) per annum can be expected. According to the GCCR, among the 10.5 million children under age 15 resident in Germany in 2014 there were 1657 registered cases of cancer, including ca. 584 leukemias (5 836 in 10 years) and 435 CNS tumors (4 347 in 10 years). Our estimates therefore indicate that 0.4% of the leukemias and 0.2% of the CNS tumors in German children under 15 years of age could be associated with CT examinations.
Discussion
The healthcare data presented here show an overall decrease in the number of CT examinations in children under 13 between 2006 and 2012, but with variations by sex and age. The numbers of CT examinations per 10 000 children and adolescents with health insurance decreased in all age groups. The difference between girls and boys stayed almost constant. The reported age distribution of the patients is similar to those in the KiCT study and an earlier investigation of pediatric CT (6). Although the cohort was recruited exclusively from hospital patients, the health insurance providers' data cover the whole spectrum of health care, both in and out of the hospital. The good agreement may be attributable to the fact that almost all of the CT examinations in children under 5 years of age were carried out on an inpatient basis (18). The proportion of out-of-hospital scans rises with increasing age.
The head is the part of the body most frequently exposed to radiation from CT, probably owing to the frequency of trauma as indication. In this context, the AOK data showed that the ICD-10 diagnostic codes S00 to S09 (head injury) were assigned in 24% of the CT scans billed in children under 13.
Our estimates show that the highest organ doses are found for CT of the head. The dose for the lens of the eye was up to 41 mGy in children aged 7.6 to 12.5 years. We observed an overall dependence of dose on age and time. The organ dose for the thyroid gland is more than twice as high in newborns as in any other age group. This may be attributable to the overranging effect (additional rotations at the beginning and end of spiral CT). For example, an increase in radiation exposure of at least 33% is assumed for a newborn undergoing thoracic CT with a 12-cm scan area, a 4-cm-wide detector, and a pitch factor of 1 (24). The decrease in organ doses with time can be attributed to the use of modern scanners and the development of settings optimized for children. It remains unclear whether this positive trend observed for the 18 participating hospitals can be generalized. Moreover, the developments in out-of-hospital CT are not covered by our cohort study. The proportion of old scanners could be higher outside the hospital setting.
The results for all organs are comparable with other estimates of organ dose for the same period (from 2000 onward). The reported average doses received by the patient during head CT are approximately 30 mGy for the brain and around 5 mGy for the bone marrow, with variation among age groups (25– 29). Our estimated doses are somewhat higher, but the doses in the other studies were averaged from smaller numbers of examinations.
We availed ourselves of data from the German KiCT cohort study and AOK records to investigate trends in the use of CT in children living in Germany. The similarity of the results despite the different nature of the sources is striking. Comparability was hampered by the different age groups in the two data sets, but the findings point in the same direction.
The data from the AOK are not representative for all persons with health insurance. In comparison with those insured by other public and private providers, AOK members are of lower socioeconomic status and a higher proportion of them have a migration background (30). The estimation of usage of medical services can be viewed as a sufficiently good approximation for Germany (31). Looking at Germany as a whole, however, analyses of the data of individual health insurance providers cannot readily be extrapolated to the general population (30). We matched our cohort study against a national socioeconomic index of multiple deprivation, which contains for example the proportion of the population out of work and the proportion without skills, and showed that more CT examinations are performed on children from socioeconomically disadvantaged regions (32), so that relying on AOK data may result in overestimation of CT use. However, no data sets containing records from more than one health insurance provider were available.
For 35 195 CT examinations from the KiCT study in the period 1997 to 2013 we were able to calculate the individual dose. For the remaining over 50% of the scans, however, this was not possible because of the absence of PACS parameters. We are currently working on various ways of reconstructing the doses for these examinations and merging PACS and RIS data (33). This makes it possible to carry out dose-related evaluation of the KiCT data. We intend then to perform a detailed assessment of the risk which will form part of the pooled European cohort study EpiCT (34).
In the KiCT study, children who underwent CT under the age of 13 years were found to have twice as many leukemias and 35% more CNS tumors than the same age segment of the general residential population. Assuming a causal relationship, this means approximately three additional cases of childhood cancer per annum (= 0.2% of all tumors in children). It must be emphasized that there is still uncertainty regarding the duration of risk after a single exposure to ionizing radiation and the extent to which the possible risk can be delimited from that due to further CT examinations or other exposures. No risk estimators exist for other radiation-associated diseases. Given the high frequency of head CT, however, in future the CT-related organ doses for the lens of the eye should be recorded more accurately and monitored whenever appropriate. There are no scientific data to show how many lives are saved with the help of CT. As long as CT is restricted to the indications recommended by the German Commission on Radiological Protection (35), however, it can be assumed that the benefit far outweighs the risks and that the number of new cases of disease caused by exposure to radiation will decrease. Further epidemiological studies are needed to confirm this assumption and provide more accurate estimates of the risks involved with the use of modern CT scanners.
Supplementary Material
Key Messages.
The number of pediatric computed tomography (CT) examinations performed in Germany decreased during the period 2006 to 2012.
A large number of the pediatric CT examinations are scans of the head, but the proportion decreases with increasing age.
The highest organ doses with head CT are found in the brain and the lens of the eye.
The organ doses with head CT fell between 1997 and 2013.
Among the ca. 10.5 million children under 15 years of age resident in Germany in 2014, 584 cases of leukemia and 435 CNS tumors occurred. The risk estimators of the German KiCT cohort study indicate that 0.4% of the leukemias and 0.2% of the CNS tumors could be associated with CT.
Acknowledgments
Translated from the original German by David Roseveare
The authors are grateful to the members of the KiCT Study Group for their committed support. The KiCT Study Group comprises Thomas Albrecht (Institute for Radiology and Interventional Therapy, Vivantes, Neukölln Hospital), Maren Asmussen (Central Institute for Diagnostic Radiology, Municipal Hospital Karlsruhe), Jörg Barkhausen (Department of Radiology and Nuclear Medicine, University Hospital Schleswig Holstein, Campus Lübeck), Lars Daniel Berthold (Institute for Diagnostic and Interventional Radiology, Hanover School of Medicine), Ajay Chavan (Department of Diagnostic and Interventional Radiology, Oldenburg Hospital GmbH), Michael Forsting (Institute for Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen), Bettina Gerste (Scientific Institute of the AOK [WIdO]), Karsten Jablonka (Department of Diagnostic Radiology and Nuclear Medicine, Bremen Hospital - Central), Andreas Jahnen (Luxembourg Institute of Science and Technology), Mathias Langer (Department of Radiology, University Hospital Freiburg), Michael Laniado (Institute and Hospital for Diagnostic Radiology, University Hospital Carl Gustav Carus Dresden), Joachim Lotz (Institute for Diagnostic and Interventional Radiology, Faculty of Medicine, University of Göttingen), Hans-Joachim Mentzel (Institute for Diagnostic and Interventional Radiology, University Hospital Jena), Oliver Rompel (Radiological Institute, University Hospital Erlangen), Jürgen F. Schäfer (Department of Diagnostic and Interventional Radiology, University Hospital Tübingen), Joachim Schlick (Institute for Radiology and Neuroradiology, Nuremberg Hospital South), Karl Schneider and Michael Seidenbusch (Institute for Clinical Radiology, University Hospital Munich, Dr. von Hauner Children's Hospital), Claudia Spix (German Childhood Cancer Registry at the Institute for Medical Biostatistics, Epidemiology and Informatics (IMBEI), Faculty of Medicine, Johannes Gutenberg University of Mainz), Birgit Spors (Pediatric Radiology, Charité – University Medicine Berlin), Gundula Staatz and Peter Mildenberger (Department of Diagnostic and Interventional Radiology, Faculty of Medicine, University of Mainz), Thomas Vogl (Institute for Diagnostic and Interventional Radiology, University Hospital, Johann Wolfgang Goethe University of Frankfurt/Main), Joachim Wagner (Institute for Radiology and Interventional Therapy, Vivantes, Friedrichshain Hospital), and Gerald Weisser (Institute for Clinical Radiology and Nuclear Medicine, University Hospital Mannheim).
This original article contains parts of the doctoral thesis of Roman Pokora.
Footnotes
Conflict of interest statement
Roman Pokora has received payments for authorship or coauthorship of a publication on a related topic from Schattauer Publishers.
The remaining authors declare that no conflict of interest exists.
References
- 1.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) United Nations. New York: 2010. Sources and effects of ionizing radiation. UNSCEAR 2008 Report to the General Assembly, with scientific annexes Vol 1. Annex A Medical radiation exposures. Sources; pp. 23–220. [Google Scholar]
- 2.Muhogora WE, Ahmed NA, AlSuwaidi JS, et al. Paediatric CT examinations in 19 developing countries: frequency and radiation dose. Radiat Prot Dosimetry. 2010;140:49–58. doi: 10.1093/rpd/ncq015. [DOI] [PubMed] [Google Scholar]
- 3.Brenner DJ, Hall EJ. Computed tomography-an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 4.IARC Working Group, Ionizing Radiation, Part 1. X-and Gamma (g)-Radiation, and Neutrons, IARC monog. Lyon. International Agency for Research on Cancer. 1999 [Google Scholar]
- 5.Bundesamt für Strahlenschutz (BfS) Bonn; 2015. Umweltradioaktivität und Strahlenbelastung. Jahresbericht 2013 Bundesministerium für Umwelt, Naturschutz, Bau und Reaktorsicherheit (BMUB) pp. 1–362. [Google Scholar]
- 6.Galanski M, Nagel HD, Stamm G. Medizinische Hochschule. Hannover: 2006. Pädiatrische CT-Expositionspraxis in der BRD: Ergebnisse 2005/06; pp. 1–57. [Google Scholar]
- 7.Strahlenschutzkommission (SSK) Bildgebende Diagnostik beim Kind - Strahlenschutz , Rechtfertigung und Effektivität - Empfehlung der Strahlenschutzkommission. Verabschiedet in der 208. Sitzung der Strahlenschutzkommission am 11./12. Juli 2006: 1-14. www.ssk.de/SharedDocs/Beratungsergebnisse_PDF/2006/BildgebendeDiagnostik_Kind.pdf?__blob=publicationFile (last accessed on 12 August 2016) [Google Scholar]
- 8.Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am J Roentgenol. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 9.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mathews JD, Forsythe AV, Brady Z, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346 f2360. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang WY, Muo CH, Lin CY, et al. Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer. 2014;110:2354–2360. doi: 10.1038/bjc.2014.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Journy N, Rehel JL, Ducou Le Pointe H, et al. Are the studies on cancer risk from CT scans biased by indication? Elements of answer from a large-scale cohort study in France. Br J Cancer. 2015;112:185–193. doi: 10.1038/bjc.2014.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krille L, Dreger S, Schindel R, et al. Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: results from a German cohort study. Radiat Environ Biophys. 2015;54:1–###12. doi: 10.1007/s00411-014-0580-3. [DOI] [PubMed] [Google Scholar]
- 14.Berrinton de Gonzales A, Salotti JA, McHugh K, et al. Relationship between paediatric CT scans and subsequent risk of leukaemia and brain tumours: assessment of the impact of underlying conditions. Br J Cancer. 2016;114:388–394. doi: 10.1038/bjc.2015.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh L, Shore R, Auvinen A, Jung T, Wakeford R. Risks from CT scans—what do recent studies tell us? J Radiol Prot. 2014;34 doi: 10.1088/0952-4746/34/1/E1. [DOI] [PubMed] [Google Scholar]
- 16.United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) United Nations. New York; 2013. Sources, effects and risks of ionizing radiation. UNSCEAR 2013 Report to the General Assembly with Scientific Annexes. Vol 2. Scientific Annex B. Effects of radiation exposure of children; pp. 5–###269. [Google Scholar]
- 17.National Council on Radiation Protection and Measurements (NCRP) Unscertainties in the estimation of radiation risks and probability of disease causation. Bethesda, MD: NCRP Report No171. 2012:1–418. [Google Scholar]
- 18.Pokora R, Gerste B, Staatz G, Günster C, Blettner M. Pädiatrische CT- und MRT-Untersuchungen in Deutschland: Zeitliche Trends der Versorgung 2006-2012 Versorgungs-Report 2015/2016. Schwerpunkt: Kinder und Jugendliche. In: Klauber J, Günster C, Gerste B, Robra B, Schmacke N, editors. Schattauer. Stuttgart; 2015. pp. 239–264. [Google Scholar]
- 19.Kaatsch P, Spix C. German childhood cancer registry—annual report 2010 (1980-2010) Mainz, Germany. 2011 [Google Scholar]
- 20.Jahnen A, Kohler S, Hermen J, Tack D, Back C. Automatic computed tomography patient dose calculation using DICOM header metadata. Radiat Prot Dosimetry. 2011;147:317–320. doi: 10.1093/rpd/ncr338. [DOI] [PubMed] [Google Scholar]
- 21.Krille L, Zeeb H, Jahnen A, et al. Computed tomographies and cancer risk in children: a literature overview of CT practices, risk estimations and an epidemiologic cohort study proposal. Radiat Environ Biophys. 2012;51:103–111. doi: 10.1007/s00411-012-0405-1. [DOI] [PubMed] [Google Scholar]
- 22.Lee C, Kim KP, Bolch WE, Moroz BE, Folio L. NCICT: a computational solution to estimate organ doses for pediatric and adult patients undergoing CT scans. J Radiol Prot. 2015;35:891–909. doi: 10.1088/0952-4746/35/4/891. [DOI] [PubMed] [Google Scholar]
- 23.International Commission on Radiological Protection (ICRP) Basic anatomical and physiological data for use in radiological protection reference values - ICRP Publication 89. Ann ICRP. 2002;32:3–4. [PubMed] [Google Scholar]
- 24.Stöver B, Rogalla P. CT-Untersuchungen bei Kindern. Radiologe. 2008;48:243–248. doi: 10.1007/s00117-007-1600-y. [DOI] [PubMed] [Google Scholar]
- 25.Meulepas JM, Ronckers CM, Smets AM, et al. Leukemia and brain tumors among children after radiation exposure from CT scans: design and methodological opportunities of the Dutch Pediatric CT Study. Eur J Epidemiol. 2014;29:293–301. doi: 10.1007/s10654-014-9900-9. [DOI] [PubMed] [Google Scholar]
- 26.Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167:700–707. doi: 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim KP, Berrington de González A, Pearce MS, et al. Development of a database of organ doses for paediatric and young adult CT scans in the United Kingdom. Radiat Prot Dosimetry. 2012;150:415–426. doi: 10.1093/rpd/ncr429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bernier MO, Rehel JL, Brisse HJ, et al. Radiation exposure from CT in early childhood: a French large-scale multicentre study. Br J Radiol. 2012;85:53–60. doi: 10.1259/bjr/90758403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suliman II, Khamis HM, Ombada TH, Alzimami K, Alkhorayef M, Sulieman A. Radiation exposure during paediatric CT in Sudan: CT dose, organ and effective doses. Radiat Prot Dosimetry. 2015;167:513–518. doi: 10.1093/rpd/ncu321. [DOI] [PubMed] [Google Scholar]
- 30.Hoffmann F, Koller D. Verschiedene Regionen, verschiedene Versichertenpopulationen? Soziodemografische und gesundheitsbezogene Unterschiede zwischen Krankenkassen. Das Gesundheitswes. 2015 doi: 10.1055/s-0035-1564074. EFirst. DOI: 10.1055/s-0035-1564074. [DOI] [PubMed] [Google Scholar]
- 31.Jaunzeme J, Eberhard S, Geyer S. Wie „repräsentativ“ sind GKV-Daten? Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:447–454. doi: 10.1007/s00103-012-1626-9. [DOI] [PubMed] [Google Scholar]
- 32.Dreger S, Krille L, Maier W, et al. Regional deprivation and non-cancer related computed tomography use in pediatric patients in Germany: cross-sectional analysis of cohort data. PLoS One. 2016;11 doi: 10.1371/journal.pone.0153644. e0153644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thierry-Chef I, Dabin J, Friberg EG, et al. Assessing organ doses from paediatric CT scans-a novel approach for an epidemiology study (the EPI-CT study) Int J Environ Res Public Health. 2013;10:717–728. doi: 10.3390/ijerph10020717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Basea M, Pearce MS, Kesminiene A, et al. EPI-CT: design, challenges and epidemiological methods of an international study on cancer risk after paediatric and young adult CT. J Radiol Prot. 2015;35:611–628. doi: 10.1088/0952-4746/35/3/611. [DOI] [PubMed] [Google Scholar]
- 35.Strahlenschutzkommission (SSK) Orientierungshilfe für bildgebende Untersuchungen. www.ssk.de/SharedDocs/Beratungsergebnisse_PDF/2008/Orientierungshilfe.pdf?__blob=publicationFile (last accessed on 12 August 2016) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.