After blunt polytrauma the cervical spine may be injured in 2-12% of patients,1-3 and injuries of the head and neck are associated in up to one third of cases.4,5 The presence of a head injury is important as it is the strongest independent risk factor for injury of the cervical spine (relative risk 8.56) and may also prevent meaningful clinical evaluation and exclusion of cervical injury.
Before the advanced trauma life support guidelines7 it had been suggested that among patients with a cervical spine injury, a delayed or missed diagnosis was associated with 10 times the rates of permanent neurological sequelae.8 Modern trauma care appropriately assumes that injury is present until it is excluded. Conscious trauma patients who are able to report symptoms and meet the criteria detailed in box 1 may generally be regarded as having a stable cervical spine. The strict application of such criteria may be more sensitive than routine screening radiographs.9-11
These criteria will not allow clinical exclusion of injury among most patients with multiple injuries. Patients rendered unconscious and requiring intubation, receiving analgesia or sedation, or with a serious head injury are not appropriate for the clinical exclusion of cervical spine injury. The strategy for the evaluation of such patients may lie anywhere between the following two modalities.
Firstly, prolonged immobilisation and a semirigid cervical collar may be used, with clinical evaluation on the return of an “adequate” level of consciousness (many clinicians believe that this is the only reliable way to exclude occult ligamentous injury). This is often associated with serious complications of prolonged immobilisation and application of the cervical collar, detailed in figure 1 and box 2. In addition, this form of evaluation in a previously unconscious patient has not been studied reliably. In one series, 2% of injuries were missed among “fully conscious” patients.12
Fig 1.
Pressure sores related to immobilisation. The elderly patient shown here died principally because of the consequences of his deep and extensive pressure ulcer. He had no spinal injury. The application of a spinal board and prolonged supine positioning were important risk factors
Box 1: Clinical exclusion of cervical spine injury
After blunt polytrauma the patient's cervical spine may be regarded as stable if:
Glasgow coma score is 15 and the patient alert and orientated
The patient has not consumed any intoxicants or drugs
No serious distracting injuries are present
No signs or symptoms become apparent on cervical examination—that is,
No midline tenderness or pain
No impairment to full range of active movement
No referable neurological deficit
The reliability and performance of these criteria requires experience, judgment, and strict application by the clinician.
Summary points
Prolonged immobilisation and use of a cervical collar are associated with notable morbidity and mortality, most commonly secondary to cutaneous pressure necrosis in the occipital, sacral, or heel areas
No consensus exists with regard to the optimal evaluation of an unconscious patient with multiple injuries who has a possible injury of the cervical spine
Plain radiography and directed computed tomography allow exclusion of cervical spine injury with > 99% sensitivity in unconscious patients
Computed tomography of the entire neck further reduces the risk of missing an injury of the cervical spine
There is little evidence that the routine use of magnetic resonance imaging or dynamic fluoroscopy is superior to radiographs and computed tomography in excluding cervical spine injury
The risks of prolonged immobilisation, beyond 48-72 hours, are poorly appreciated and exceed those of a serious missed cervical spine injury after normal plain radiography and computed tomography imaging
Secondly, in patients who remain unconscious, clinical examination may be forgone and imaging alone relied on. Traditional teaching claims that a potentially unstable ligamentous injury of the cervical spine, without an associated fracture, cannot be shown directly by plain films or computed tomography. Many studies challenge this.2,3,20,21
The lack of consensus regarding optimal evaluation applied to the common scenario of “clearing” the cervical spine in the intensive care unit, emergency department, or operating department is striking. In 2002 our intensive care unit cared for 183 unconscious patients with multiple injuries and experienced this clinical dilemma every other day. Across the United Kingdom an estimated 100 head injuries per 100 000 population occur per year.22 Our survey of Northern Ireland's intensivists and trauma surgeons showed diverse practices. Worryingly, 12.5% of clinicians believed that plain radiography was adequate to exclude cervical injury, and the advanced trauma life support concept of a “generic expert” to provide standardised evaluation and “clearance” of cervical spine injury is a myth.14 Other workers have shown that 48% of UK intensive care units23 and 12-16% of American specialists24 were prepared to clear an unconscious patient's cervical spine by using a solitary lateral plain radiograph.
We reviewed the complications of spinal immobilisation and the performance of the common imaging modalities, and we examined established management protocols, to present an evidence based, clinically applicable protocol designed to facilitate the early identification or exclusion of cervical spine injury. The aims of the protocol include reducing the notable morbidity and mortality associated with prolonged spinal precautions among unconscious patients with multiple injuries.
Methods
The sources for this review were Medline 1960-2004, Embase, PubMed, and the Cochrane Library. We used the medical subject headings “cervical spine and cord injury”, “cervical collar”, “spinal precautions and immobility”, “plain radiography”, “computed tomography”, “magnetic resonance imaging and dynamic fluoroscopy” and combinations thereof. We searched all reference lists and review articles for additional works, and we contacted our regional specialists in anaesthesia, intensive care medicine, radiology, orthopaedics, and neurosurgery. We also visited two websites, www.east.org and www.trauma.org, to gather information.
Box 2: Complications of prolonged immobilisation and spinal precautions
Cutaneous pressure ulceration
This is common and increases with prolonged use of collars, particularly after 48-72 hours, and may occur in up to 55% of patients.13 The requirement for skin grafting has been reported by 18.8% of specialists,14 and our unit has experienced septic shock and infected cervical prostheses after operative fixation have been reported in our unit. “Bed sores” require prolonged time to heal—each ulcer costing $30 000 (£17 000; €25 000) (fig 1).15
Elevated intracranial pressure and venous obstruction
This may produce secondary ischaemic brain injury; up to one third of patients with multiple injuries have a head injury.4,5
Difficult intubation and loss of the airway
Tracheostomy is often delayed and performed surgically rather than as a percutaneous procedure.
Difficulty in obtaining central venous access
Subsequent poor line care is associated with increased catheter related septicaemia.
Inability to provide good oral care
Has been linked to bacteraemia and sepsis.
Failed enteral nutrition
Supine positioning and immobility increase enteric failure to reach nutritional targets and requirement for parenteral nutrition. Gastrointestinal bacterial translocation is a proposed complication.
Gastrostasis, reflux, and pulmonary aspiration
Gastrostasis, reflux, and pulmonary aspiration are promoted by a static supine position resulting in ventilator associated pneumonia; prolonged ventilation and intensive care stay; and increasing morbidity, mortality, and costs. Among elderly patients with cervical spine injuries, 26.8% died during treatment, principally due to respiratory complications.16
Restricted physiotherapy regimens
Such restrictions result in an increased risk of ventilator associated pneumonia and thromboembolism.
Thromboembolism
Deep venous thrombosis may occur, with an incidence of 2.1%.17
Increased risk of cross infection
Log rolling (requiring at least four staff) makes barrier nursing a practical impossibility and cross contamination is demonstrably higher, affecting the entire intensive care unit, theatre population, and hospital population.18,19
Complications of spinal immobilisation
A cornerstone in the management of unconscious patients with multiple injuries is the avoidance of displacing potentially unstable spinal injuries with resultant secondary neurological compromise. “Spinal precautions” may include spinal boards for transfer, prolonged nursing in a supine position on a firm mattress, the application of cervical collars, lateral restraints, head tapes, and surgical stabilisation of identified injuries as indicated. The benefit conferred by routine application of some of these elements, particularly spinal boards25 and cervical collars,26 has been questioned.
Box 3: Existing management guidelines and protocols
Advanced trauma life support guidelines and cervical spine injury
“For patients who are comatose, have an altered level of consciousness, or are too young to describe their symptoms: all such patients should at least have a lateral and AP c-spine x-ray. Whenever possible, an open-mouth view also should be obtained. If the entire c-spine can be visualised and is found to be normal, the collar can be removed after appropriate evaluation by a neurosurgeon or orthopaedic surgeon.... When in doubt, leave the collar on... a cervical computed tomography scan can be obtained somewhat later.”7 These guidelines offer little guidance beyond performing plain radiographs and the involvement of a specialist and this seriously undermines their usefulness in patients in intensive care, given the lack of consensus among individual clinicians.14,23,24
Eastern Association for the Surgery of Trauma (EAST) guidelines
“A three view spine series supplemented by thin cut axial computed tomography images with sagittal reconstruction through suspicious areas or inadequately visualised areas provides a false negative rate of less than 0.1%... computed tomography alone, MRI and flexion/extension radiographs have all been shown to miss injuries and have not been shown to be more accurate....”38
There was insufficient evidence to allow level 1 recommendations, but these 1998 guidelines37 are supported by several large studies that show that plain radiographs and directed computed tomography have an overall sensitivity of well over 99%,2,3,20 challenging traditional wisdom that ligamentous injury cannot be reliably identified with these modalities.
Revised EAST guidelines and cervical spine injury
The most recent EAST guidelines were issued in 2000 and recommend dynamic fluoroscopy in unconscious patients:
“Altered mental status and return of normal mental status not anticipated for 2 days or more (eg severe traumatic or hypoxic brain injury).... Plain films... axial computed tomography images at 3mm intervals with sagittal reconstruction from the base of the occiput through C2... if normal, flexion/extension lateral cervical spine fluoroscopy....”38
The EAST 2000 recommendation for dynamic fluoroscopy was prompted by a small meta-analysis (n = 227, including five ligamentous injuries) and radically revised the 1998 estimated false negative incidence after plain radiography and directed computed tomography from < 0.1% to 2.2%.38 Our more recent and complete literature evaluation is summarised in table B on bmj.com and seriously questions the EAST 2000 inclusion of dynamic fluoroscopy.36
The more common complications of prolonged immobilisation and spinal precautions are listed in box 2. A missed spinal injury may represent a disaster for the patient and would be a well remembered adverse event in any intensive care unit. However, most of the complications of prolonged immobilisation are poorly recorded, acting synergistically to produce less apparent or attributable adverse events. Depending on the clinician's base specialty, these complications may not be recognised, and we have previously shown that only 60% of orthopaedic surgeons believed that prolonged immobilisation represented a serious risk to the patient.14 Collectively we may be ignoring the morbidity and mortality attributable to the prolonged immobilisation of large numbers of trauma patients in intensive care in order to avoid a rare scenario—namely, instability of the cervical spine despite normal appropriate imaging.
The pathogenesis of pressure ulceration of the skin is complex and multifactorial, but after 72 hours in a cervical collar cutaneous complications are common.27 Skin breakdown has been recorded in 55% of patients wearing collars for more than five days.13 Additional risk factors for cutaneous necrosis include prolonged periods of immobilisation, lack of posture change, and the use of spinal boards.28 Although pressure reducing mattresses29 or frequent posture changes30,31 reduce this incidence, both are contraindicated by “spinal precautions.” Pressure necrosis may occur rapidly,32 and there is evidence that cutaneous vasoregulation is disturbed in patients with an actual cervical spine injury.33 Spinal boards are increasingly felt to be appropriate only for extrication,34 and their use outside this setting should be limited.35 If excluding cervical spine injury by using imaging alone were to allow the early discontinuation of spinal precautions then subsequent nursing of patients in altering positions and the use of a pressure relieving mattress would almost certainly reduce morbidity and mortality.
Techniques to “clear” the cervical spine
The radiological exclusion of cervical injury has been reviewed extensively (see also table A on bmj.com).36 w1 Since clinical exclusion of cervical spine injury is unproved and often impossible in patients with multiple injuries, reliable imaging of the cervical spine is imperative.
Plain cervical radiography combined with computed tomography has a similar sensitivity to magnetic resonance imaging and dynamic fluoroscopy in detecting an unstable cervical spine injury; fewer than 1% of injuries will be missed. Combined screening with plain radiographs and directed computed tomography may have a false negative rate as low as 0.1%, and this includes serious ligamentous injuries.37 Units regularly accepting trauma patients should be able to provide a 24 hour service offering plain radiography and computed tomography. The use of magnetic resonance imaging requires a more difficult and distant transfer from intensive care in addition to all the problems of ferromagnetic compatibility for monitoring and anaesthesia.w2 w3 Magnetic resonance imaging is therefore unlikely to become routine for screening injuries of the cervical spine among critically ill patients for the foreseeable future. The use of dynamic fluoroscopy is discussed further with the 2000 guidelines of the Eastern Association for the Surgery of Trauma (EAST),38 but we believe that the technique lacks compelling evidence regarding its use in screening cervical spine injury in unconscious patients with multiple injuries. Box 3 shows existing management guidelines and protocols.
We showed that the incidence of serious ligamentous injuries identified by dynamic testing alone was 0.9% (n = 887) and, to detect one further injury beyond plain radiographs and directed computed tomography, the number needed to treat was in excess of 500 and a false negative result (0.33%) approached twice this rate.31 Scientific objections, safety concerns, and inability to confirm rotational stability all undermine the routine use of dynamic fluoroscopy.w4 A recent study found that only 4% of studies visualised the entire cervical spine.w5 Dynamic fluoroscopy is therefore probably best restricted to clinical studies in the future.
Proposed evaluation of the cervical spine in unconscious patients with multiple injuries
In the evaluation of an unconscious patient with multiple injuries who has a possible injury of the cervical spine, the principles of any screening programme (for example, sensitivity v specificity) should be weighed against the risks associated with subsequent management (such as mobilisation v spinal precautions). We believe that the notable morbidity and mortality associated with prolonged immobilisation and spinal precautions (box 2), coupled with the excellent performance of modern imaging, make it unacceptable to await clinical exclusion of cervical spine injury if the patient does not regain consciousness within 48-72 hours. Furthermore, the efficacy of a full clinical evaluation before the cervical spine is considered stable has not been confirmed in this context. Conversely, the practice of employing combinations of plain radiography (especially a solitary lateral view) while patients remain unconscious is not sufficiently sensitive and may miss 15% of actual injuries of the cervical spine.w6
Additional educational resources
Eastern Association for the Surgery of Trauma (www.east.org)—United States based, not for profit organisation to provide leadership and foster advances in the care of injured patients www.trauma.org—Provides global education, information, and communication resources for professionals in trauma and critical care Reviews of the performance of the various imaging modalities available to exclude cervical spine injury in unconscious patients with multiple injuries31,32 The Oxford protocol—See Brohi et al, 200012 and website of John Radcliffe Hospital (www.oxfordradcliffe.nhs.uk)
All existing guidelines and recommendations7,37,38 in this field remain level 2-3 recommendations, and on available evidence, plain radiographs combined with high resolution computed tomography, magnetic resonance imaging, and dynamic fluoroscopy all seem to have similar sensitivities to detect unstable cervical injuries, including pure ligamentous injuries, and miss fewer than 1% of actual cervical spine injuries after polytrauma. We believe that screening and excluding injury of the cervical spine in unconscious patients with multiple injuries by plain radiography and directed computed tomography is sufficiently sensitive and widely available to be recommended for routine use in most trauma units. The quoted risk of missing a seriously unstable injury (0.1%)37 is probably representative—that is, close to one in 1000 patients evaluated. We think that trauma units with access to a helical, multiplane, computed tomography scanner should routinely image the entire cervical spine at high resolution since the number needed to treat to detect a further injury beyond directed scanning may be only eight to 22 patients,20,21,36 and this is the standard recommended in figure 2. This is similarly a level 2-3 recommendation; an urgent need remains for an adequately powered, prospective comparison of these modalities to justify any further recommendations.
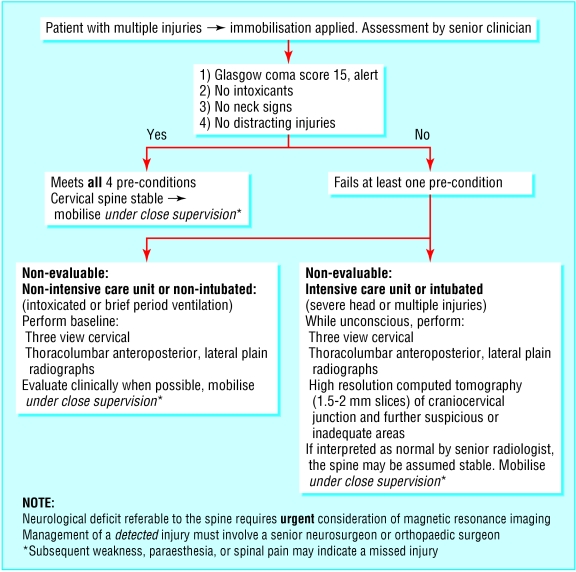
Fig 2.
Proposed algorithm to clear the cervical spine in unconscious trauma patients.
Case presentation
An elderly man was admitted to the intensive care unit with multiple broken ribs, pulmonary contusions, and a closed head injury (initial Glasgow coma score 11). Nevertheless, he made good progress and was successfully weaned from mechanical ventilation. Despite normal spinal imaging performed to the satisfaction of the fracture service, the service requested a clinical assessment, which required a conscious and competent patient before it would exclude significant spinal injury. “Spinal precautions” up to this point had included an interhospital transfer on a spinal board and use of a firm mattress in intensive care with the patient maintained in a strict supine position, and the application of a semirigid cervical collar. Lateral turning for nursing procedures required a “log roll” technique by at least four staff. By day 10 it was apparent that clinical assessment would not be possible, given the patient's ongoing neurological deficit and the effects of analgesia. At this point spinal precautions were discontinued. Unfortunately, by the same day, a large sacral ulcer became apparent, which, once debrided, occupied almost all of the patient's lower back (fig 1) and extended to bone. This ulcer was the source of repeated episodes of sepsis and required high dose opioid analgesia. This resulted in a depressed level of consciousness and pneumonia and necessitated starting mechanical ventilation again. The man died 73 days after admission to intensive care. It was decided that he would not survive the extensive reconstructive surgery he required. No spinal injury or related neurological deficit was ever detected in this patient, either before or after death.
We propose the removal of cervical collars and patients' mobilisation as a priority for management. Therefore if plain radiographs and computed tomography imaging do not show evidence of traumatic abnormality and the patient is not expected to be conscious within 48-72 hours, current evidence supports the declaration “cervical spine cleared” without further delay.
We draw attention to the routine inclusion of thoracolumbar plain radiography, where unconscious patients with multiple injuries have a compatible mechanism of injury.
Supplementary Material
 Additional tables and references are on bmj.com
Additional tables and references are on bmj.com
Contributors: CGM had the original idea, searched the literature, and wrote the main text. CGM and GGL managed the cases. EPM is guarantor.
Funding: None.
Competing interests: None declared.
References
- 1.MacDonald RL, Schwartz ML, Mirich D. Diagnosis of cervical spine injury in motor vehicle crash victims: how many X-rays are enough? J Trauma 1990;30: 392-7. [PubMed] [Google Scholar]
- 2.Chiu WC, Haan JH, Cushing BM, Kramer ME, Scalea TM. Ligamentous injuries of the cervical spine in unreliable blunt trauma patients: incidence, evaluation and outcome. J Trauma 2001;50: 457-63. [DOI] [PubMed] [Google Scholar]
- 3.Demetriades D, Charalambides K, Chahwan S, Hanpeter D, Alo K, Velmahos G, et al. Nonskeletal cervical spine injuries: epidemiology and diagnostic pitfalls. J Trauma 2000;48: 724-7. [DOI] [PubMed] [Google Scholar]
- 4.Holly LT, Kelly DF, Counelis GJ, Blinman T, McArthur DL, Cryer HG. Cervical spine trauma associated with moderate and severe head injury: incidence risk factors and injury characteristics. J Neurosurg 2002;96: S285-91. [DOI] [PubMed] [Google Scholar]
- 5.Iida H, Tachibina S, Kithara T, Horiike S, Ohwada T, Fujii K, et al. Association of head trauma with cervical spine injury, spinal cord injury or both. J Trauma 1999;46: 450-2. [DOI] [PubMed] [Google Scholar]
- 6.Blackmore CC, Emerson SS, Mann FA, Koepsell TD. Cervical spine imaging in patients with trauma: determination of fracture risk to optimize use. Radiology 1999;211: 759-65. [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons Committee on Trauma. Advanced trauma life support for doctors student course manual. Chicago: American College of Surgeons, 1997.
- 8.Reid DC, Hernderson R, Saboe L, Miller JD. Etiology and clinical course of missed spine fractures. J Trauma 1987;27: 980-6. [DOI] [PubMed] [Google Scholar]
- 9.Velmahos GC, Theodorou D, Tatevossian R, Belzbergh H, Cornwell EE 3rd, Berne TV, et al. Radiographic cervical evaluation in the alert, asymptomatic blunt trauma victim: much ado about nothing? J Trauma 1996;40: 768-74. [DOI] [PubMed] [Google Scholar]
- 10.Bachulis BL, Long WB, Hynes GD, Johnson MC. Clinical indications for cervical radiographs in the traumatized patient. Am J Surg 1987;153: 473-8. [DOI] [PubMed] [Google Scholar]
- 11.Ersoy G, Karcioglu O, Enginbas Y, Eray O, Ayrik C. Are cervical spine X-rays mandatory in all blunt trauma patients? Eur J Med 1995;2: 191-5. [DOI] [PubMed] [Google Scholar]
- 12.Brohi K, Wilson-MacDonald J. Evaluation of unstable cervical injury: a 6 year experience. J Trauma 2000;49: 76-80. [DOI] [PubMed] [Google Scholar]
- 13.Davis JW, Parks SN, CL Detlefs MD, Williams GG, Williams JL, Smith RW. Clearing the cervical spine in obtunded patients: the use of dynamic fluoroscopy. J Trauma 1995;39: 435-8. [DOI] [PubMed] [Google Scholar]
- 14.Morris CG, Mullan B. Clearing the cervical spine after polytrauma, instituting unified management for unconscious victims in the intensive care unit. Anaesthesia 2004;59: 755-61 [DOI] [PubMed] [Google Scholar]
- 15.Nawoczenski DA: Pressure sores: prevention and management. In: Buchanan LE, Nawoczenski DA, eds. Spinal cord injury—concepts and management approaches. Baltimore, Williams and Wilkins, 1987: 99-121.
- 16.Lieberman IH, Webb JK. Cervical injuries in the elderly. J Bone Joint Surg 1994;76: 877-81. [PubMed] [Google Scholar]
- 17.McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil 1999;80: 1402-10. [DOI] [PubMed] [Google Scholar]
- 18.Bauer TM, Ofner E, Just HM, Just H, Daschner FD. An epidemiological study assessing the relative importance of airborne and direct contact transmission of microorganisms in a medical intensive care unit. J Hosp Infect 1990;15: 301-9. [DOI] [PubMed] [Google Scholar]
- 19.Huebener J, Frank U, Kappstien I, et al. Influence of architectural design on nosocomial infection in intensive care units—a prospective 2 year analysis. Intensive Care Med 1989;15: 179-83. [DOI] [PubMed] [Google Scholar]
- 20.Berne JD, Velmahos GC, El-Tawil Q, Demetriades D, Asenso JA, Murray JA, et al. Value of complete cervical computed tomographic scanning in identifying cervical injury in the unevaluable blunt trauma patient with multiple injuries: a prospective study. J Trauma 1999;47: 896-902. [DOI] [PubMed] [Google Scholar]
- 21.Nunez DB, Zuluaga A, Fuentes-Bernardo DA, Rivas LA, Becerra JL. Cervical spine trauma: how much more do we learn by routinely using helical CT? Radiographics 1996;16: 1307-18. [DOI] [PubMed] [Google Scholar]
- 22.Rehabilitation of persons with traumatic brain injury. NIH Consensus Statement 1998. Oct 26-28;16: 1-41. [PubMed] [Google Scholar]
- 23.Grossman MD, Reilly PM, Gillett T, Gillett D. National survey of the incidence of cervical spine injury and approach to cervical spine clearance in US trauma centers. J Trauma 1999;47: 684-90. [DOI] [PubMed] [Google Scholar]
- 24.Gupta KJ, Clancy M. Discontinuation of cervical spine immobilisation in unconscious patients with trauma in intensive care units—telephone survey of practice in south and west region. BMJ 1997;314: 1652-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Porter KM, Allison KP. The UK emergency department practice for spinal board unloading. Is there conformity? Resuscitation 2003;58: 117-20. [DOI] [PubMed] [Google Scholar]
- 26.Morris CG, McCoy E. Cervical immobilisation collars in ICU: friend or foe? Anaesthesia 2003;58: 1051-3. [DOI] [PubMed] [Google Scholar]
- 27.Ajani AE, Cooper DJ, Scheinkestel CD, Laidlaw J, Tuxen DV. Optimal assessment of cervical spine trauma in severe nonpenetrating closed head injury: a prospective study. Anaesth Intensive Care 1998;26: 487-91. [DOI] [PubMed] [Google Scholar]
- 28.Mawson AR, Biundo JJ Jr, Neville P, Linares HA, Winchester Y, Lopez A. Risk factors for early occurring pressure ulcers following spinal injury. Am J Phys Med Rehabil 1998;67: 123-7. [DOI] [PubMed] [Google Scholar]
- 29.Kato H, Inoue T, Torii S. A new postoperative management scheme for preventing sacral pressure sores in patients with spinal cord injuries. Ann Plast Surg 1998;40: 39-43. [DOI] [PubMed] [Google Scholar]
- 30.O'Sullivan KL, Engrav LH, Maier RV, Pilcher SL, Isik FF, Copass MK. Pressure sores in the acute trauma patient: incidence and causes. J Trauma 1997;42: 276-8. [DOI] [PubMed] [Google Scholar]
- 31.Linares HA, Mawson AR, Suarez E, Biundo JJ. Association between pressure sores and immobilisation in the immediate post-injury period. Orthopedics 1987;10: 571-3. [DOI] [PubMed] [Google Scholar]
- 32.Curry K, Cassidy L. The relationship between extended periods of immobility and decubitus ulcer formation in the acutely spinal cord-injured patient. J Neurosci Nurs 1992;24: 185-9. [DOI] [PubMed] [Google Scholar]
- 33.Mawson AR, Siddiqui FH, Connolly BJ, Sharp CJ, Summer WR, Biundo JJ Jr. Sacral transcutaneous oxygen tensions levels in the spinal cord injured: risk factors for pressure ulcers? Arch Phys Med Rehabil 1993;74: 745-51. [DOI] [PubMed] [Google Scholar]
- 34.Cooke MW. Use of spinal board within the accident and emergency department. J Accid Emerg Med 1998;15: 108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hauswald M, McNally T. Confusing extrication with immobilisation: the inappropriate use of hard spine boards for interhospital transfers. Air Med J 2000;19: 126-7. [DOI] [PubMed] [Google Scholar]
- 36.Morris CG, McCoy E. Clearing the cervical spine in unconscious polytrauma victims; balancing risks and effective screening. Anaesthesia 2004;59: 464-82. [DOI] [PubMed] [Google Scholar]
- 37.EAST Ad Hoc Committee on Practice Management Guideline Development. Practice management guidelines for trauma from the Eastern Association for the Surgery of Trauma. J Trauma 1998;44: 941-6. [DOI] [PubMed] [Google Scholar]
- 38.Eastern Association for the Surgery of Trauma. Determination of cervical spine stability in trauma patients. Winston-Salem: EAST, 2000. www.east.org/tpg/chap3u.pdf (accessed 22 Jul 2004).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.