Abstract
Polybrominated diphenyl ethers (PBDEs), polychlorinated biphenyls (PCBs) and p,p′-dichlorodiphenyldichloroethylene (p,p′-DDE) have been measured in surplus serum collected in 2009 from a convenience sample of 300 Texas children (boys and girls) in the birth to 13 years of age range. Serum concentrations of traditional persistent organic pollutants such as 2,2′,4,4′,5,5′-hexachlorobiphenyl (PCB-153) and p,p′-DDE did not change consistently with age. By contrast, serum concentrations of tetra-, penta-, and hexa-BDEs were lowest in the youngest children (birth to two year old) and increased 3.0 to 7.9 times, depending on the analyte, for children in the >4 to 6 years of age group. From the apex concentration to the 10 to 13 years of age group, concentrations decreased significantly except for 2,2′,4,4′,5,5′-hexabromodiphenyl ether (PBDE-153), which also had a longer apex concentration of >4 to 8 years of age. This concentration trend for PBDE-153 is most likely due to a longer half-life of PBDE-153 than of other PBDE congeners. The observed PBDEs concentration patterns by age may be related, at least in part, to ingestion of residential dust containing PBDEs through hand-to-mouth behavior among toddlers, preschoolers, and kindergarteners. Further studies to characterize young children’s exposure to PBDEs are warranted and, in particular, to determine the lifestyle factors that may contribute to such exposures.
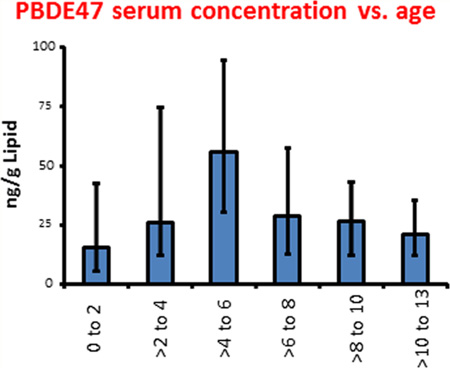
Graphical Abstract
INTRODUCTION
Polybrominated diphenyl ethers (PBDEs) are a class of brominated flame retardants. The tetra- through hexa-BDE congeners are persistent in wildlife and humans,1 are present in common food items,2 and almost universally detected in human biomonitoring studies in the United States.3–5 Three commercial preparations, identified by their average bromine content as PentaBDE, OctaBDE, and DecaBDE, have been commercially produced. The PentaBDE and OctaBDE products were voluntarily withdrawn from the US market in 2004;6 production, import, and sale of DecaBDE ended in 2013.7 Technical PentaBDE has been used in applications such as furniture and wall-to-wall carpets; the OctaBDE and DecaBDE products have been used in hard plastics such as the housing of electrical appliances.8 The detection frequency of congeners present in technical OctaBDE and DecaBDE in nonoccupationally exposed subjects is generally lower than that of congeners present in technical PentaBDE (tri- to hexa-BDEs).3–5 Animal models have shown that PBDEs may have endocrine disrupting effects on thyroid hormone production,9,10 neurotoxic effects that delay or impair motor activity as well as cognitive and behavioral functions,11–13 and estrogen/androgen hormone effects that may affect puberty onset and impair spermatogenesis.14,15 Congeners from all bromination degrees are found at higher levels in indoor dust in the United States than in other regions of the world.16
PBDEs have mainly been measured in serum collected from adults or at birth (i.e., cord serum).3–5,17 However, compared to other population groups, children may be more exposed to particulate matter in the indoor environment18 and, as a result, may also be more exposed to certain PBDEs than adults.16 Therefore, evaluating children’s exposure to PBDEs and other environmental chemicals present in indoor dust is of importance from a public health perspective.
The objectives of the current study were (1) to measure PBDEs in individual serum samples collected from children less than 1 year of age to 13 years of age, (2) to measure other structurally related persistent organic pollutants (POPs), such as polychlorinated biphenyls (PCBs) and persistent pesticides, which are compounds known to be present in indoor dust at concentrations orders of magnitude lower than PBDEs, and (3) to compare the serum concentrations of PBDEs and other POPs in these children to those of the 2003–2004 National Health and Nutrition Examination Survey (NHANES),3 a representative sample of the US general population.
MATERIALS AND METHODS
This study was reviewed and found to be exempt from informed consent requirements by the Institutional Review Board (IRB) at the University of Texas Health Science Center at Houston. The Centers for Disease Control and Prevention (CDC) IRB determined that the CDC laboratory was not engaged in research.
Sample Collection
Children sera were collected for pathology testing at the Children’s Medical Center in Dallas, Texas from August to November 2009. It is not known if these samples were collected for routine examination or if the children were being evaluated for health reasons or concerns. Due to confidentiality issues, we only had access to the child’s sex, date of birth and date of collection of the serum from which the age of the child at collection was calculated. Residual serum samples were available from children between <1 year to <13 years of age. The first 50 available samples with a volume over 0.5 mL and within the age range sought for each age group (i.e., 0 to 2; >2 to 4; >4 to 6; >6 to 8; >8 to 10; >10 to 13 years of age) were selected for POPs measurements until reaching a total number of 300 samples for the six age strata. The samples were stored at −70 °C until the time of analysis.
Chemical Analysis
The analytical method used has been published.19 Briefly, the serum samples were processed in batches of 30 including three quality control samples [human serum fortified with target analytes (2 mL)] and three method blanks. Method blanks, composed of fetal calf serum, were diluted 1:40 with water (to a final volume of 4 mL) to decrease the concentration of endogenous p,p′-DDE to a level 1 order of mangnitude below the limit of detection (LOD). Serum was weighed into 16 × 100 mm test tubes fitted with Teflon-lined silicone septa and the volume for each sample was adjusted to 4 mL with water; the amount of serum available for POPs measurements ranged from 0.12 to 2 g (median = 1.04 g). The serum samples were transferred to a liquid handler (Gilson 215; Middleton, WI) for automatic fortification of 13C12-labeled internal standards. The spiked sera were pretreated with formic acid (4 mL) and diluted with an additional 4 mL of water before solid phase extraction (SPE).19 The automated extractions were carried out overnight on a modular SPE workstation (Biotage AB; Uppsala, Sweden) followed by lipid removal using the same SPE workstation.19 Measurement of target analytes was performed using gas chromatography-isotope dilution-high resolution mass spectrometry using a DFS instrument (ThermoFisher; Bremen, Germany).19 All concentrations reported were background corrected for the median analyte amount in blank samples. The LOD was defined as the highest of the blank LOD or the lowest point in the calibration curve (0.5 pg/µL), except for PBDE-209 (5 pg/µL). The blank LOD was defined as 3 times the standard deviation of the blank samples analyzed in parallel with the study samples. All chromatographic peaks were confirmed to have a signal-to-noise ratio greater than 3. The median and range of amount (pg) of POPs detectable in blank samples and the LOD used for each analyte for which further statistical handling was performed are given in Table 1.
Table 1.
Median and Range Amount of Analytes Detectable in Method Blank Samples (pg/sample) and Limit of Detection (LOD) [pg/g serum])
| IUPAC name (abbreviation) | blank concentration (pg/sample) median (range) |
limit of detection (pg/g serum) median (range) |
|---|---|---|
| polybrominated diphenyl ethers (PBDEs) | ||
| 2,2′,4,4′-tetrabromodiphenyl ether (PBDE-47) | 6.1 (3.2–20.9) | 14.9 (7.7–127.9)a |
| 2,2′,4,4′,5-pentabromodiphenyl ether (PBDE-99) | 1.0 (0–7.1) | 4.8 (2.5–41.3)b |
| 2,2′,4,4′,6-pentabromodiphenyl ether (PBDE-100) | 0.0 (0–6.0) | 4.8 (2.5–41.3)b |
| 2,2′,4,4′,5,5′-hexabromodiphenyl ether (PBDE-153) | 0.0 (0–6.7) | 4.8 (2.5–41.3)b |
| decabromodiphenyl ether (PBDE-209) | 0.0 (0–68.7) | 82.12 (23.7–945.6)b |
| persistent pesticides and polychlorinated biphenyls (PCBs) | ||
| p,p′-dichlorodiphenyldichloroethylene (p,p′-DDE) | 0.0 (0–14.3) | 12.9 (12.5–206.6)b |
| 2,2′,4,4′,5,5′-hexachlorobiphenyl (PCB-153) | 0.0 (0–4.4) | 4.8 (2.5–41.3)b |
Limit of detection defined as signal-to-noise greater than 3.
Limit of detection defined as three times the standard deviation of method blanks analyzed in parallel with unknown samples.
Statistical Analyses
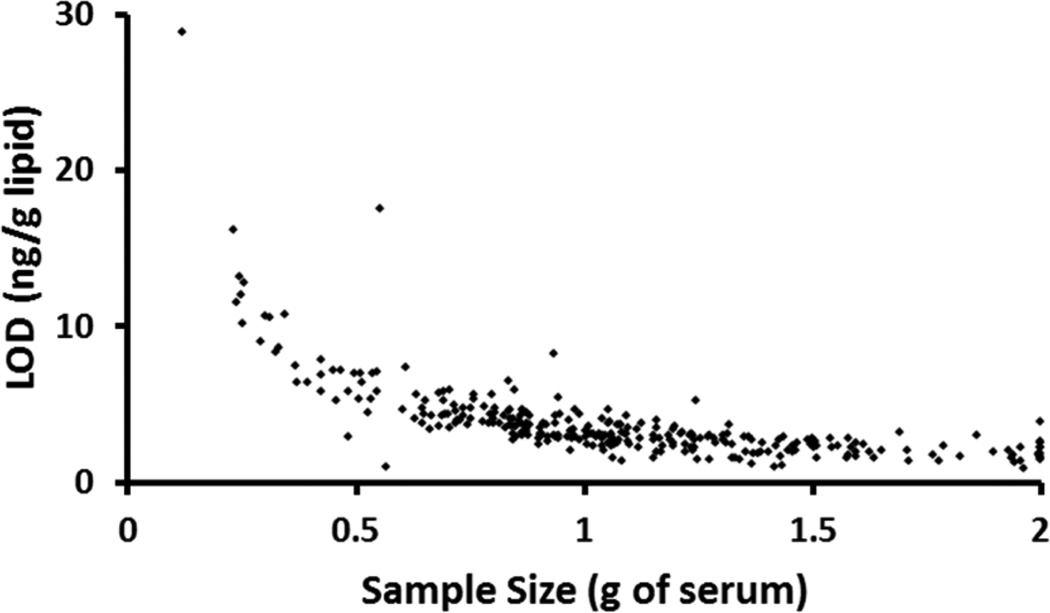
All statistical evaluation of the analytical and demographical data was performed in SAS 9.3 (SAS Institute Inc.; Cary, NC). The subjects were stratified by age groups with two-year increments with 50 subjects included in each of the six age strata. Statistical evaluation of concentration data was only performed for analytes having an overall detection frequency ≥60% (Tables 1 and 2). As expected, the LOD (Figure 1) directly depends on the available amount of serum used for analysis. Specifically, the LOD increases rapidly when the serum amount is below 0.5 g, as exemplified with 2,2′,4,4′-terabromodiphenyl ether (PBDE-47) in Figure 1. Due to this observation, the detection frequency, by analyte, for samples having a serum amount of <0.5 g was compared to the overall detection frequency (Supporting Information, Table S1). We observed no apparent bias toward an increased frequency of nondetectable concentrations for low amount samples by age strata, except for the age group >2 to 4 years of age where nine out of 50 samples had <0.5 g of available serum (Supporting Information, Table S1).
Table 2.
Detection Frequency and Selected Percentiles with 95% Confidence Interval (95%CI) of the Concentration (ng/g lipid) of Four PBDEs, PCB-153 and p,p′-DDE by Age Strata in 300 Texas Children’s Sera Collected in 2009 Showing the p-Value of the Difference in Median Concentration between the Age Group >4 to 6 Years and Other Age Groupsa
| age group (years) | detection frequency (%) |
25th (95%CI) (ng/g lipid) |
median (95%CI) (ng/g lipid) |
75th (95%CI) (ng/g lipid) |
maximum (ng/g lipid) |
p-value |
|---|---|---|---|---|---|---|
| 2,2′,4,4′-tetrabromodiphenyl ether (PBDE-47) | ||||||
| 0 to 2 | 90 | 5.5 (4.3–11.7) | 15.4 (11.6–32.1) | 42.3 (29.4–78.5) | 345 | <0.001 |
| >2 to 4 | 94 | 12.3 (5.1–18.8) | 26.1 (18–49.8) | 74.7 (47.3–132) | 1450 | <0.05 |
| >4 to 6 | 98 | 30.2 (18.9–43.4) | 55.7 (42.5–77.2) | 94.6 (70.4–144) | 314 | REF |
| >6 to 8 | 96 | 12.5 (9.5–20.9) | 28.7 (19.3–43.1) | 57.3 (41.4–115) | 1790 | <0.05 |
| >8 to 10 | 96 | 12.0 (8.6–16) | 26.35 (15.9–32.5) | 42.8 (31.5–68.8) | 361 | <0.01 |
| >10 to 13 | 100 | 11.9 (9.8–16.1) | 21.15 (15.6–23.4) | 35.4 (23.2–62.5) | 180 | <0.001 |
| 12–19 (NHANES 2003–2004)b | n/a | 14.1 (12.0–16.6) | 27.2 (22.1–33.6) | 53.6 (44.9–63.6) | 2350 | |
| 2,2′,4,4′,5-pentabromodiphenyl ether (PBDE-99) | ||||||
| 0 to 2 | 92 | 2.5 (1.2–3.4) | 3.9 (3.3–7.7) | 10.3 (5.8–22.6) | 125 | <0.001 |
| >2 to 4 | 88 | 3.0 (1.6–4.8) | 7.6 (4.6–13.2) | 23.9 (12.6–33) | 714 | <0.05 |
| >4 to 6 | 98 | 7.5 (5.1–9.7) | 13.25 (9.7–18.4) | 22.75 (17.6–44.5) | 92.7 | REF |
| >6 to 8 | 92 | 3.2 (2.1–4.6) | 6.2 (4.6–9.7) | 16.4 (9.1–35.2) | 469 | <0.05 |
| >8 to 10 | 100 | 3.4 (2.7–4.7) | 6.7 (4.7–9.2) | 12.4 (9–25.6) | 152 | <0.01 |
| >10 to 13 | 98 | 2.7 (2.2–4.5) | 5.4 (4.2–7.2) | 8.9 (7.1–13.1) | 68.6 | <0.001 |
| 12–19 (NHANES 2003–2004)b | n/a | <LOD | 5.6 | 12.8 (11.4–15.7) | 692 | |
| 2,2′,4,4′,6-pentabromodiphenyl ether (PBDE-100) | ||||||
| 0 to 2 | 60 | n/d (n/d–1.5) | 2.4 (n/d–5.9) | 8.4 (5.5–12) | 53.3 | <0.001 |
| >2 to 4 | 84 | 1.7 (0.7–5.4) | 5.95 (4.8–12.4) | 17.2 (9.5–26.4) | 1210 | <0.01 |
| >4 to 6 | 98 | 7.2 (6–9.6) | 12 (9.3–17.2) | 19.8 (16.4–33) | 78.8 | REF |
| >6 to 8 | 92 | 3.3 (2.3–5.6) | 8.3 (5.4–11) | 17 (10.9–27.4) | 781 | 0.097 |
| >8 to 10 | 90 | 2.7 (1.6–4.1) | 6.1 (3.7–8.4) | 9.8 (7.8–15.9) | 76.9 | <0.001 |
| >10 to 13 | 84 | 2.7 (n/d–3.8) | 4.55 (3.8–5.9) | 8.8 (5.1–12.4) | 57.5 | <0.001 |
| 12–19 (NHANES 2003–2004)b | n/a | 2.6 (2.2–3.1) | 4.8 (3.8–6.1) | 9.4 (7.9–12.8) | 365 | |
| 2,2′,4,4′,5,5′-hexabromodiphenyl ether (PBDE-153) | ||||||
| 0 to 2 | 70 | 1.0 (n/d–1.9) | 3.3 (1.6–5.7) | 6.5 (5.5–11.2) | 21.7 | <0.001 |
| >2 to 4 | 82 | 1.9 (0.8–4.3) | 6.6 (4–10.1) | 10.5 (9.5–20.4) | 1390 | <0.001 |
| >4 to 6 | 98 | 7.9 (6.3–12) | 14.1 (11.8–19.9) | 25.9 (18.5–32.6) | 110 | REF |
| >6 to 8 | 96 | 5.8 (4.9–10.2) | 12.5 (10–20.7) | 31.3 (20–51.1) | 1120 | >0.5 |
| >8 to 10 | 94 | 6.1 (2.6–9.3) | 10.15 (9.2–12.8) | 19.7 (12.4–32.2) | 92 | 0.37 |
| >10 to 13 | 98 | 5.1 (3.9–7.9) | 10.85 (7.7–11.5) | 16.1 (11.4–28.8) | 61.9 | 0.28 |
| 12–19 (NHANES 2003–2004)b | n/a | 3.6 (3.0–5.2) | 7.4 (6.0–9.5) | 15.3 (11.7–19.4) | 821 | |
| decabromodiphenyl ether (PBDE-209) | ||||||
| 0 to 2 | 8 | n/d | n/d | n/d | n/d | n/d |
| >2 to 4 | 21 | n/d | n/d | n/d | n/d | n/d |
| >4 to 6 | 26 | n/d | n/d | n/d | n/d | n/d |
| >6 to 8 | 22 | n/d | n/d | n/d | n/d | n/d |
| >8 to 10 | 16 | n/d | n/d | n/d | n/d | n/d |
| >10 to 13 | 21 | n/d | n/d | n/d | n/d | n/d |
| 12–19 (NHANES 2003–2004)b | n/a | n/a | n/a | n/a | n/a | |
| p,p′-dichlorodiphenyldichloroethylene (p,p′-DDE) | ||||||
| 0 to 2 | 90 | 20.4 (7–29.3) | 36.3 (27.8–73.5) | 139.0 (65.5–317) | 6390 | >0.5 |
| >2 to 4 | 96 | 24.5 (19.8–46.2) | 63.1 (42.3–99.7) | 192.0 (89.6–499) | 2980 | >0.5 |
| >4 to 6 | 98 | 36.3 (25.4–42.8) | 50.2 (42.2–57.6) | 83.1 (56.4–162) | 643 | REF |
| >6 to 8 | 100 | 37.0 (30.4–49) | 57.7 (46.4–96.4) | 159.0 (93.6–274) | 12 400 | >0.5 |
| >8 to 10 | 100 | 44.4 (35.4–51.4) | 55.6 (51.2–81.4) | 100.0 (81.3–140) | 515 | >0.5 |
| >10 to 13 | 100 | 42.2 (38.6–53.4) | 73.0 (50.1–85.7) | 102.0 (85.7–177) | 1260 | 0.43 |
| 12–19 (NHANES 2003–2004)b | n/a | 57.7 (47.7–67.8) | 93.6 (81.0–114.0) | 167.0 (123.0–240.0) | 22 900 | |
| 2,2′,4,4′,5,5′-hexachlorobiphenyl (PCB-153) | ||||||
| 0 to 2 | 76 | 1.1 (0.4–1.4) | 2.1 (1.4–2.7) | 4.4 (2.6–7.9) | 27.5 | >0.5 |
| >2 to 4 | 64 | 0.9 (0.4–1) | 1.2 (1–2.2) | 2.5 (1.9–7.4) | 19.7 | >0.5 |
| >4 to 6 | 74 | 0.9 (n/d–1.1) | 1.5 (1–2.3) | 2.7 (1.9–4.5) | 15.7 | REF |
| >6 to 8 | 76 | 1.2 (n/d–1.5) | 2.1 (1.5–3.4) | 4.6 (3–10.8) | 24.8 | 0.22 |
| >8 to 10 | 72 | 1.2 (n/d–1.7) | 2.2 (1.5–2.5) | 3.0 (2.5–4.6) | 36.2 | >0.5 |
| >10 to 13 | 78 | 1.0 (n/d–1.4) | 1.9 (1.4–2.4) | 3.3 (2.4–5) | 20.5 | >0.5 |
| 12–19 (NHANES 2003–2004)b | n/a | 3.8 (3.17–4.15) | 5.4 (4.70–6.21) | 8.5 (7.80–9.81) | 986 | |
Percentiles were derived from the SAS procedure “Proc Lifetest” providing reversed Kaplan–Meier (rKM) estimates of left censored data.
12–19 year old subjects from the National Health and Nutrition Examination Survey (NHANES) 2003–2004.3
Abbreviations: n/a, data not available; n/d, not determined due to having >60% results below the limit of detection (LOD).
Figure 1.
Individual sample limit of detection (ng/g lipid) is dependent on the serum volume used for analysis, exemplified here with 2,2′,4,4′-tetrabromodiphenyl ether (PBDE-47). Twenty five out of 300 samples (or 8.3% of samples) had an available sample size below 0.5 g, cf. Supporting Information, Table S1.
We used reverse Kaplan–Meier estimator,20 which is a nonparametric maximum likelihood estimator for left censored data (i.e., data below the LOD), to calculate percentiles and distribution function by age strata. The reverse Kaplan–Meier estimator is recommended in preference to commonly used methods such as substituting LOD/2 or LOD/√2 for values below the LOD, assuming a known parametric distribution, or using imputation to replace the left-censored values. We used the SAS procedure “Proc Lifetest”, which provides a nonparametric estimation of percentiles of concentration for left censored data (Table 2). We used Wilcoxon test to compare sex differences and the distributional difference for each age group with the >4–6 years old age group. The 25th, 50th, and 75th percentiles with 95% confidence intervals and the maximum concentration for each age strata are given in Table 2 after combining the results from female and male children because no statistical sex difference was observed (Wilcoxon rank test; data not shown).
RESULTS
The concentrations of PBDEs (n = 11), PCBs (n = 34), and persistent pesticides (n = 9) have been determined in serum collected in 2009 from a convenience sampling of children from Texas, USA, between the ages of zero to less than 13 years. Frequencies of detection ranged from 0% to 100%, depending on the analyte. We present results only for analytes with overall detection frequency of at least 60%. The detection frequency of PBDE-209 followed the pattern of lower brominated PBDEs with the highest detection frequency (26%) in the >4–6 years age group children. The detection frequencies of PBDE-209 were 8%–21% and 16–21% for the age groups 4 years and younger and older than 6 years (Table 2), respectively. The PBDE-209 overall detection frequency was too low (<60%) to calculate median concentrations by age group.
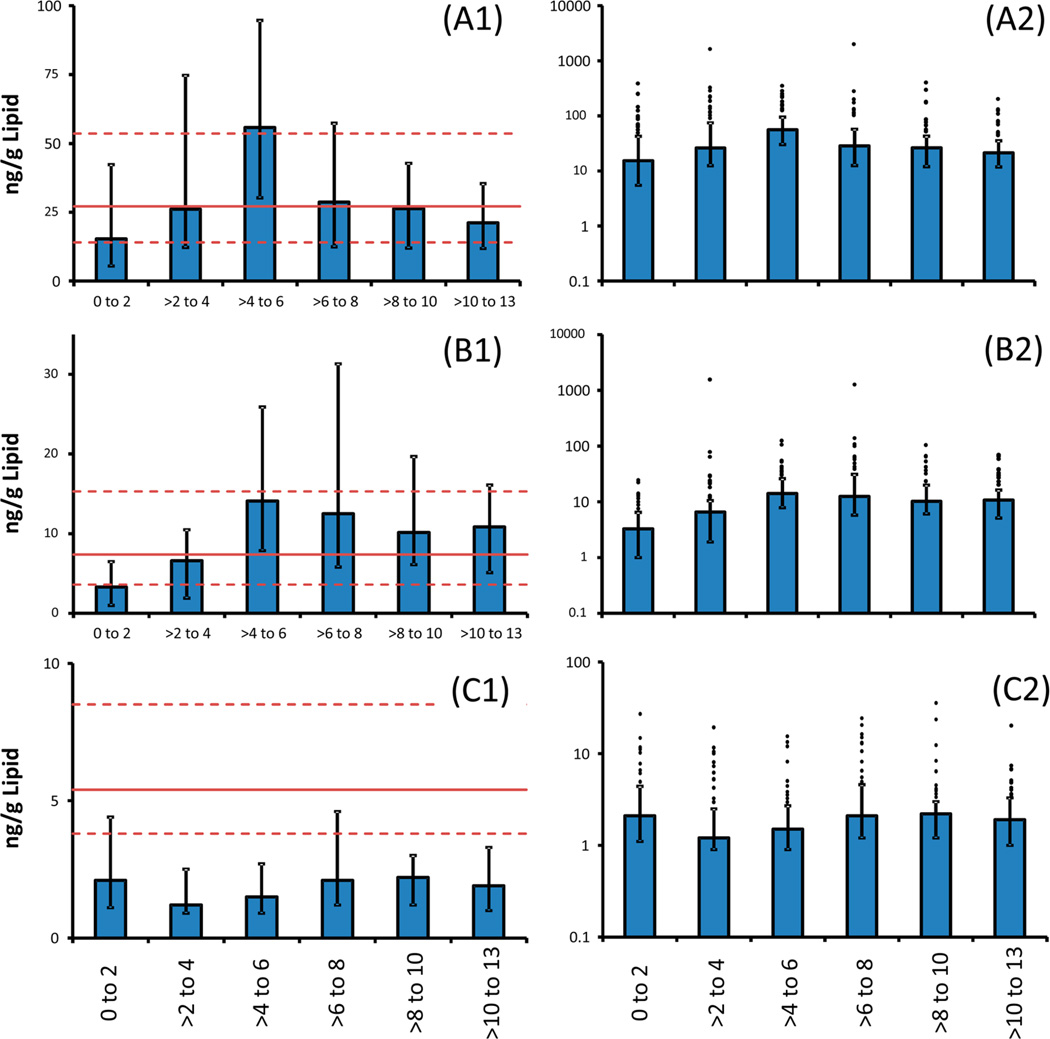
The serum concentrations of PBDE-47, PBDE-99, and PBDE-100 increased from 0 to 2 years of age and reached a maximum concentration in the age group >4–6 years, after which concentrations showed a decreasing trend (Figure 2, Table 2). Serum concentrations of PBDE-100 in children between the age groups >4–6 and >6–8 years were not significantly different (Table 2). PBDE-153 reached its peak concentration between >4 and 8 years of age, later than other PBDEs measured (Figure 2 and Table 2); the overall lower concentration of PBDE-153 in children >8 years of age was not significantly different from that in the >4–6 year old children (Table 2). On the other hand, serum concentrations of PCB-153 and p,p′-dichlorodiphenyldichoroethylene (p,p′-DDE) were similar in all age groups among these Texas children and not significantly different to the >4–6 year olds.
Figure 2.
Median concentration (ng/g lipid) of (A1) 2,2′,4,4′-tetrabromodiphenyl ether (PBDE-47), (B1) 2,2′,4,4′,5,5′-pentaBDE (PBDE-153), and (C1) 2,2′,4,4′,5,5′-hexachlorobiphenyl (PCB-153) by age group with vertical bars indicating interquartile range for Texas children’s serum collected in 2009. The horizontal red lines show the median (solid line) and 25th and 75th concentrations (dashed lines) for subjects between 12 and 19 years of age in the 2003–2004 National Health and Nutrition Examination Survey (NHANES). The median and corresponding 25th and 75th percentiles are also presented on a logarithmic scale in the bar graphs (A2, B2, and C2) with results above the 75th percentiles shown as dots above the vertical bars.
The >4–6 year old children had statistically higher medians of PBDE-47, -99, -100 than 12–19 year old adolescents from NHANES 2003–20043 assessed by comparison of the 95% confidence intervals of the medians (Table 2, Figure 2). Similarly, PBDE-153 serum concentrations were higher for both the >4–6 and >6–8 year olds than the 12–19 years old NHANES participants, but concentrations of the 0–2 year age group children were lower. On the other hand, all age groups of the Texas children had lower serum concentrations of p,p,′-DDE and PCB-153 than the 12–19 year old NHANES adolescents (Table 2, Figure 2).
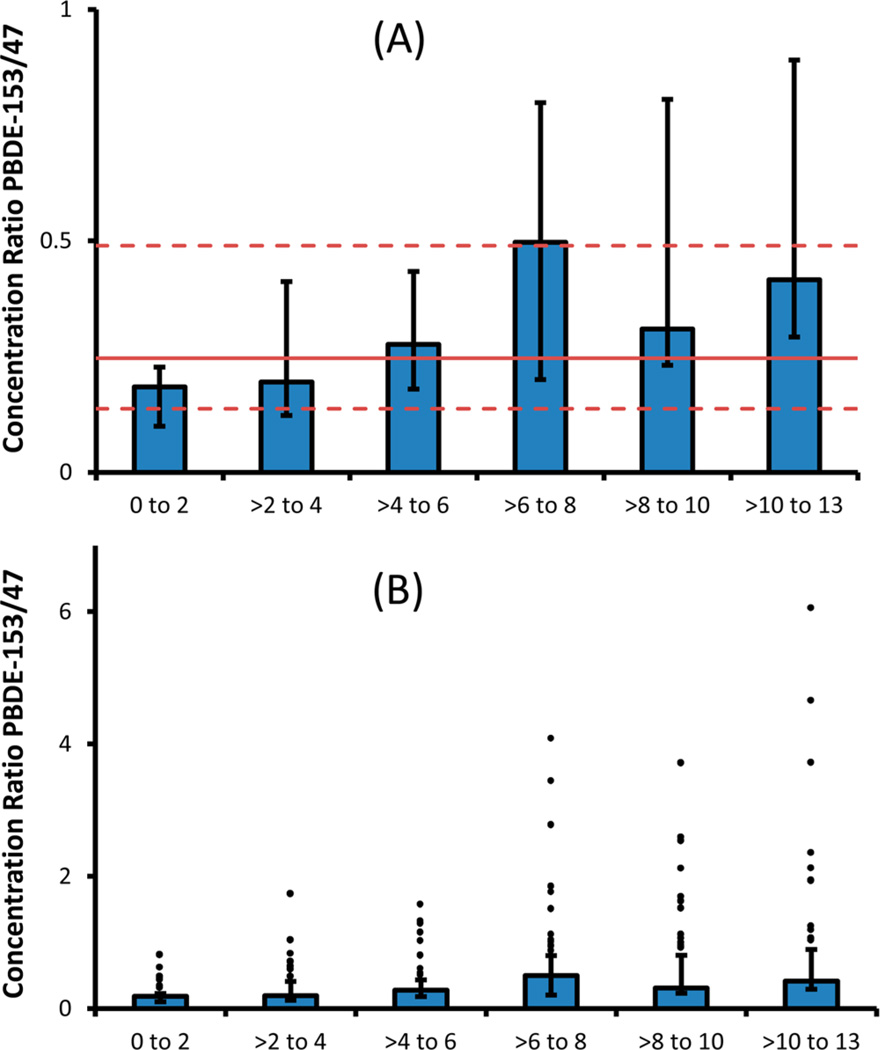
The median concentration ratio between PBDE-153 (hexaBDE) and PBDE-47 (tetraBDE), a measure of relative contribution to the overall serum concentration of these congeners, increased by age group from 0.18 (0 to <2 year olds) to 0.50 (>6 to 8 year olds), but did not change consistently among children between the age groups of >6 to 8 years and >10 to 13 years (Figure 3). Noteworthy, PBDE-153 was the dominant PBDE congener ([PBDE-153]/[PBDE-47] >1) in 0%, 2%, 10%, 15%, 17%, and 18% of the children in the 0–2, >2–4, >4–6, >6–8, >8–10, and >10–13 years age groups, respectively.
Figure 3.
(A) Median concentration ratio of 2,2′,4,4′,5,5′-hexabromodiphenyl ether (PBDE-153) and 2,2′,4,4′-tetraBDE (PBDE-47) with vertical bars indicating the 25th and 75th percentiles by age group for 300 Texas children who provided sera in 2009. The horizontal red lines indicate the median (solid line) and the 25th and 75th percentile concentrations (dashed lines) for all subjects of the 2003–2004 National Health and Nutrition Examination Survey (NHANES). (B) Representation of the data in graph (A) on a logarithmic scale indicating samples with concentration ratios above the 75th percentile as dots above the vertical bars.
DISCUSSION
We are reporting the concentrations of select PBDEs and traditional POPs in sera collected in 2009 from a convenience group of children, between the ages of zero and <13 years, who attended a medical care facility in Dallas, Texas, USA. Whether the children were at the facility for evaluation of health concerns or illness or for a routine health examination was not known. This limitation prevents us from drawing conclusions extending beyond the population studied because these children may not be representative of other children of similar ages.
Serum concentrations of the majority of PBDEs increased from birth until peaking at the age of >4 to 6 years (>4–8 years for PBDE-153). Then, for most congeners, concentrations decreased until the oldest age group examined (i.e., >10 to 13 years of age). Of interest, concentrations of PBDE-153 did not decrease significantly with age. In the youngest children, the PBDE pattern was dominated by PBDE-47, but with age, the relative contribution of PBDE-153 increased. For example, in the >6 to 8 year old children, the concentration of PBDE-153 was half that of PBDE-47. This finding and the longer period of apex concentrations of PBDE-153 compared to other PBDEs may be explained by PBDE-153 having a longer biological half-life than other congeners investigated. The assumed longer biological half-life of PBDE-153 would also explain the increasing number of older children for whom PBDE-153 was the dominating congener. However, it is worth noting that the frequency of cases where PBDE-153 was the dominating congener ranged from 0% (0–2 year old) to 18% (>10–13 year old) among the Texas children whereas for the 12 to >60 year old NHANES 2003–2004 participants, it was 9.3%. The reason for this difference is unknown, but could be due to regional differences (i.e., NHANES is a nationally representative sample of the population of the United States) or related to the fact that the NHANES samples were collected in 2003–2004, five years before these Texas children’s samples.
Dehalogenation of higher brominated congeners may produce lower brominated congeners,21 such as octa- and nona-BDEs. If dehalogenation significantly contributed to the presence of PBDE-153 in the Texas children’s sera, we could reasonably expect to observe other hexa-BDEs formed through the same methabolism pathway. However, no hexa-BDE congeners other than PBDE-154, which was present in the technical penta-BDE mixtures, were detected in the samples at a level >4% of the PBDE-153 concentration. The absence of other hexa-BDE metabolites in these children’s sera suggests that dehalogenation is unlikely to be of quantitative importance in humans. Therefore, although the possibility that some debromination occurred cannot be excluded at present, it is more likely that the presence of PBDE-153 in the children’s sera is due to exposure to PBDE-153 present in indoor dust and the increasing proportion of PBDE-153 relative to PBDE-47 is due to a longer biological half-life of PBDE-153 compared with other PBDE congeners.
Half-life estimates, obtained from occupationally exposed workers in Sweden, of higher brominated congeners are relatively short (i.e., three months for PBDE-183 (2,2′3,4,4′,5′,6-heptaBDE) and 2 weeks for PBDE-209 (decaBDE)).22 The short half-life of PBDE-20922 may explain its relatively low detection frequency (19%) in this group of Texas children. The detection frequency for PBDE-209 was lowest among the youngest children and highest for the >4 to 6 year old children. Interestingly, the detection frequency by age group of PBDE-209 exhibits a similar trend compared with that of tetra- to hexa-BDEs, suggesting that the routes of exposure to these PBDEs are similar in the Texas children.
Characterizing the determinants of young children’s exposure to PBDEs remains a research gap. For example, 12% of children between the ages of >2 and 6 years had serum concentrations of PBDE-47 over 157 ng/g lipid, the 95th percentile of NHANES 2003–2004.3 The highest concentration of PBDE-47 in the Texas children was 1790 ng/g lipid and two children had serum concentrations of PBDE-47 over 1000 ng/g lipid (6 times higher than the NHANES 2003–2004 95th percentile), corresponding to 1.3% of the children between the ages of >2 and <8 years. In NHANES 2003–2004, four persons had concentrations of PBDE-47 over 1000 ng/g lipid, corresponding to 0.2% of the national sample of over 2000 subjects between the ages of 12 years through >60 years. Together, these findings suggest that children may be more likely to experience exposures leading to serum concentrations of >1000 ng/g lipid, in addition to the elevated median concentration for the >4–6 year old children. Furthermore, a previous study that sampled from the same medical center in Texas found PBDE contamination in fetal tissue.23 This suggests the necessity to further explore the determinants of young children’s exposure during the sensitive period of gestation.
The concentration of traditional POPs such as PCBs and p,p′-DDE did not change consistently with age in the Texas children. By contrast, increasing concentrations of these contaminants were reported with increasing age in NHANES 2003–2004 adult participants3 who years ago might have experienced increased environmental exposure to these contaminants when exposures to traditional POPs were greater than today and over a longer time period. The absence of an association with age for traditional POPs in the Texas children reduces the likelihood that diet is the main source of exposure to PBDEs because food items known to have a high concentration of PBDEs (e.g., fatty fish) also would be expected to contain traditional POPs. Nonetheless, this may be an oversimplification because the U.S. general population’s fish consumption is relatively low with a higher relative consumption of red meat and poultry that may also contain relatively high levels of PBDEs.2
Besides diet, a plausible explanation for the 3.0 to 7.9 times increase in serum concentrations of tetra- through hexa-PBDEs from birth to age >4 to 6 years in the Texas children is through exposure to PBDEs present in indoor dust.16,24 Hand-to-mouth behavior in young children is a well-established route of ingestion of residential dust and has been shown to be a major source of exposure to other contaminants, including heavy metals such as lead.25 Further, PBDEs originating from technical PentaBDE (tri- to hexa-BDEs) are present in residential dust at levels much higher in the United States than elsewhere in the world,16 further supporting dust ingestion as a major source of PBDE exposure in these children. For example, considering that PBDE-47 has been detected in residential dust in the United States at levels ranging from 430 to 644 ng/g16,26 and that children may ingest 100 mg of dust per day,18 the estimated maximum intake of PBDE-47 is 50 ng/day. On the other hand, the maximum dietary intake estimates of PBDE-47 derived from a food basket survey2 for fish (e.g., canned sardines) and meat and dairy products (e.g., bacon) and food consumption data for a 3 to <6 year old child are each 5 ng/day,18 10 times lower than the estimated daily intake from dust ingestion. Although these dietary estimates are likely associated with order of magnitude uncertainties for estimating the general population exposure to PBDE-47, the general trend suggests that dietary sources may not be the largest source of PBDE exposure for young children. However, for adults, the situation may be different with an overall lower dust ingestion rate per day and a larger amount of food consumed than for a young child.18 Further studies aimed at characterizing young children’s exposure to PBDEs are warranted, in particular, to determine the lifestyle factors that may contribute to such exposures.
Supplementary Material
Footnotes
ASSOCIATED CONTENT
Supporting Information
Detection frequency by available sample size <0.5 g of serum vs all samples by analyte. This material is available free of charge via the Internet at http://pubs.acs.org.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors declare no competing financial interest.
REFERENCES
- 1.Toxicological profile for Polybrominated Biphenyls and Polybrominated Diphenyl Ethers. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service, Agency for Toxic Substances and Disease Registry; 2004. http://www.atsdr.cdc.gov/toxprofiles/tp68.pdf. [PubMed] [Google Scholar]
- 2.Schecter A, Colacino J, Patel K, Kannan K, Yun SH, Haffner D, Harris TR, Birnbaum L. Polybrominated diphenyl ether levels in foodstuffs collected from three locations from the United States. Toxicol. Appl. Pharmacol. 2010;243(2):217–224. doi: 10.1016/j.taap.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Sjodin A, Wong LY, Jones RS, Park A, Zhang Y, Hodge C, Dipietro E, McClure C, Turner W, Needham LL, Patterson DG. Serum concentrations of polybrominated diphenyl ethers (PBDEs) and polyhrominated biphenyl (PBB) in the United States population: 2003–2004. Environ. Sci. Technol. 2008;42(4):1377–1384. doi: 10.1021/es702451p. [DOI] [PubMed] [Google Scholar]
- 4.Sjödin A, Jones RS, Caudill SP, Wong L-Y, Turner WE, Calafat AM. Polybrominated diphenyl ethers, polychlorinated biphenyls, and persistent pesticides in serum from the National Health and Nutrition Examination survey: 2003–2008. Environ. Sci. Technol. 2014;48(1):753–760. doi: 10.1021/es4037836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sjödin A, Jones RS, Caudill SP, Wong L-Y, Turner WE, Calafat AM. Polybrominated diphenyl ethers and other persistent organic pollutants in serum pools from the National Health and Nutrition Examination survey: 2001–2002. Environ. Sci. Technol. Lett. 2014;1(1):92–96. doi: 10.1021/ez400050w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polybrominated Diphenyl Ethers (PBDEs) Action Plan. Washington, DC: U.S. Environmental Protection Agency; 2009. http://www.epa.gov/oppt/existingchemicals/pubs/actionplans/pbdes_ap_2009_1230_final.pdf. [Google Scholar]
- 7.DecaBDE Phase-out Initiative. Washington, DC: U.S. Environmental Protection Agency; 2012. http://www.epa.gov/oppt/existingchemicals/pubs/actionplans/deccadbe.html. [Google Scholar]
- 8.WHO. Environmental Health Criteria 162. Brominated diphenyl ethers. Geneva, Switzerland: International Program on Chemical Safety, WHO; 1994. [Google Scholar]
- 9.Costa LG, de Laat R, Tagliaferri S, Pellacani C. A mechanistic view of polybrominated diphenyl ether (PBDE) developmental neurotoxicity. Toxicol. Lett. 2013 doi: 10.1016/j.toxlet.2013.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Darnerud PO. Brominated flame retardants as possible endocrine disrupters. International Journal of Andrology. 2008;31(2):152–160. doi: 10.1111/j.1365-2605.2008.00869.x. [DOI] [PubMed] [Google Scholar]
- 11.Driscoll L, Gibson AM, Hieb A. Chronic postnatal DE-71 exposure: Effects on learning, attention and thyroxine levels. Neurotoxicol. Teratol. 2009;31(2):76–84. doi: 10.1016/j.ntt.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Gee JR, Moser VC. Acute postnatal exposure to brominated diphenylether 47 delays neuromotor ontogeny and alters motor activity in mice. Neurotoxicol. Teratol. 2008;30(2):79–87. doi: 10.1016/j.ntt.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Viberg H, Fredriksson A, Eriksson P. Neonatal exposure to polybrominated diphenyl ether (PBDE 153) disrupts spontaneous behaviour, impairs learning and memory, and decreases hippocampal cholinergic receptors in adult mice. Toxicol. Appl. Pharmacol. 2003;192(2):95–106. doi: 10.1016/s0041-008x(03)00217-5. [DOI] [PubMed] [Google Scholar]
- 14.Kuriyama SN, Talsness CE, Grote K, Chahoud I. Developmental exposure to low-dose PBDE-99: Effects on male fertility and neurobehavior in rat offspring. Environ. Health Perspect. 2005;113(2):149–154. doi: 10.1289/ehp.7421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lilienthal H, Hack A, Roth-Harer A, Grande SW, Talsness CE. Effects of developmental exposure to 2,2′,4,4′,5-pentabromodiphenyl ether (PBDE-99) on sex steroids, sexual development, and sexually dimorphic behavior in rats. Environ. Health Perspect. 2006;114(2):194–201. doi: 10.1289/ehp.8391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sjödin A, Papke O, McGahee E, Focant JF, Jones RS, Pless-Mulloli T, Toms LML, Herrmann T, Muller J, Needham LL, Patterson DG. Concentration of polybrominated diphenyl ethers (PBDEs) in household dust from various countries. Chemosphere. 2008;73(1):S131–S136. doi: 10.1016/j.chemosphere.2007.08.075. [DOI] [PubMed] [Google Scholar]
- 17.Herbstman JB, Sjödin A, Kurzon M, Lederman SA, Jones RS, Rauh V, Needham LL, Tang D, Niedzwiecki M, Wang RY, Perera F. Prenatal exposure to PBDEs and neurodevelopment. Environ. Health Perspect. 2010;118(5):712–719. doi: 10.1289/ehp.0901340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Exposure Factors Handbook 2011 Edition. Washington, DC: U.S. Environmental Protection Agency; 2011. http://cfpub.epa.gov/ncea/risk/recordisplay.cfm?deid=236252. [Google Scholar]
- 19.Sjödin A, Jones RS, Lapeza CR, Focant JF, McGahee EE, Patterson DG. Semiautomated high-throughput extraction and cleanup method for the measurement of polybrominated diphenyl ethers, polybrominated biphenyls, and polychlorinated biphenyls in human serum. Anal. Chem. 2004;76(7):1921–1927. doi: 10.1021/ac030381+. [DOI] [PubMed] [Google Scholar]
- 20.Gillespie BW, Chen QX, Reichert H, Franzblau A, Hedgeman E, Lepkowski J, Adriaens P, Demond A, Luksemburg W, Garabrant DH. Estimating population distributions when some data are below a limit of detection by using a reverse Kaplan-Meier estimator. Epidemiology. 2010;21:S64–S70. doi: 10.1097/EDE.0b013e3181ce9f08. [DOI] [PubMed] [Google Scholar]
- 21.Thuresson K, Höglund P, Hagmar L, Sjödin A, Bergman Å, Jakobsson K. Apparent half-lives of hepta- to decabrominated diphenyl ethers in human serum as determined in occupationally exposed workers. Environ. Health Perspect. 2006;114:176–181. doi: 10.1289/ehp.8350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thuresson K, Hoglund P, Hagmar L, Sjödin A, Bergman A, Jakobsson K. Apparent half-lives of hepta- to decabrominated diphenyl ethers in human serum as determined in occupationally exposed workers. Environ. Health Perspect. 2006;114(2):176–181. doi: 10.1289/ehp.8350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schecter A, Johnson-Welch S, Tung KC, Harris TR, Papke O, Rosen R. Polybrominated diphenyl ether (PBDE) levels in livers of US human fetuses and newborns. J. Toxicol. Environ. Health, Part A. 2007;70(1):1–6. doi: 10.1080/15287390600748369. [DOI] [PubMed] [Google Scholar]
- 24.Watkins DJ, McClean MD, Fraser AJ, Weinberg J, Stapleton HM, Sjodin A, Webster TF. Impact of dust from multiple microenvironments and diet on PentaBDE body burden. Environ. Sci. Technol. 2012;46(2):1192–1200. doi: 10.1021/es203314e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Layton DW, Beamer PI. Migration of contaminated soil and airborne particulates to indoor dust. Environ. Sci. Technol. 2009;43(21):8199–8205. doi: 10.1021/es9003735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stapleton HM, Dodder NG, Offenberg JH, Schantz MM, Wise SA. Polybrominated diphenyl ethers in house dust and clothes dryer lint. Environ. Sci. Technol. 2005;39(4):925–931. doi: 10.1021/es0486824. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.