Abstract
We investigated the induction of interleukin-8 (IL-8) by bacterial lipopolysaccharide (LPS) and peptidoglycan (PGN) in the bladder cancer cell lines T24, 5637, UM-UC-3, and HT1197. T24 and 5637 cells strongly induced IL-8 after stimulation with LPS or PGN in a dose- and time-dependent manner, whereas UM-UC-3 and HT1197 cells did so very weakly. The expression of CD14 at the mRNA, total cellular protein, and cell surface protein levels differed among these cell lines, but the expression levels of Toll-like receptors 2 and 4 (TLR2 and TLR4) were not significantly different. The CD14 expression levels were found to correlate with the inducibility of IL-8 by LPS or PGN. Treatment of T24 and 5637 cells with phosphatidylinositol-specific phospholipase C to eliminate CD14 from the cell surface dramatically suppressed the induction of IL-8. On the other hand, UM-UC-3 cells transfected with CD14 cDNA expressed membrane-anchored CD14 and showed more efficent induction of IL-8 by LPS stimulation than untransfected controls. These results suggest that the presence of the membrane-anchored, but not the soluble, form of CD14 is a strong factor in IL-8 induction in bladder epithelial cells in response to bacterial components. The presence of the membrane-anchored form of CD14 may thus be a determinant for the inflammatory response of uroepithelial cells.
Like respiratory infections, urinary tract infections constitute a severe problem in the hospital environment. In particular, chronic infection of patients with indwelling urinary catheters by multidrug-resistant and weakly pathogenic bacteria such as Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus is currently a major problem. In these infections, bacteria initially contact bladder epithelial cells and provoke host defensive responses such as inflammatory reactions. For example, levels of the chemokine interleukin-8 (IL-8) in urine correlate highly with the infiltration of leukocytes into urine (27). Inflammatory responses are triggered by bacterial components, such as gram-negative bacterial lipopolysaccharides (LPS) and gram-positive bacterial peptidoglycans (PGN) (2, 7, 28).
Toll-like receptors (TLRs) have been shown to play important roles in the recognition of microbial components and in the cellular signal transduction pathway that results in inflammatory reactions (1, 7, 30). At least 10 members of the TLR family have been reported. Among these, TLR2 has been found to be involved in the recognition of various bacterial components such as PGN, lipoteichoic acids in gram-positive bacteria, and lipoproteins in mycoplasmas and mycobacteria. In some cases, TLR6 or TLR1 cooperates with TLR2 (18, 24). The LPS receptor TLR4 requires other molecules, including CD14 and MD-2, to recognize LPS and promote signal transduction (8, 22). It has been reported that TLR2 requires CD14 for signal transduction (16, 35), but this proposal is still controversial.
CD14 is expressed on the surfaces of monocytes and polymorphonuclear leukocytes as a glycophosphatidylinositol-anchored protein (3, 14), and it recognizes the LPS complex with a host serum glycoprotein, lipopolysaccharide-binding protein. CD14 is considered to efficiently present LPS to the TLR4-MD-2 complex (8, 31). On the other hand, CD14 also exists in a soluble form (sCD14) in serum. It had generally been thought that fibroblasts, epithelial cells, and endothelial cells do not express the membrane-anchored form (mCD14) and that complexes containing LPS and serum sCD14 interact with TLR4-MD-2 at the cell surface (4, 20, 26). However, recent reports suggest that mCD14 is indeed present in several fibroblast and endothelial cell lines (12, 21, 25).
In the case of uroepithelial cells, production of inflammatory cytokines by bladder and kidney cell lines has been reported (4, 5, 9, 11). However, these studies made use of single cell lines only, so they did not address the possibility that multiple cell lines of the same origin may exhibit diversity in this respect. In the present study, we examined IL-8 induction by LPS and PGN as a marker for the inflammatory response in four human bladder cancer cell lines. We found that the mCD14 molecule largely contributes to differences in inflammatory response among these cell lines.
MATERIALS AND METHODS
Cell lines.
The human uroepithelial cell lines T24, 5637, UM-UC-3, and HT1197 were obtained from the American Type Culture Collection (Manassas, Va.). The cells were cultured in Dulbecco's modified minimal essential medium supplemented with 10% (vol/vol) fetal bovine serum.
LPS and PGN.
LPS was isolated from P. aeruginosa IID1130 (serotype O11) according to the method of Westphal and Jann (32). For further purification, the preparation was subsequently treated with DNase and proteinase K, and the LPS was collected by ultracentrifugation (33). PGN derived from S. aureus was purchased from Fluka (Steinheim, Switzerland).
Determination of IL-8 by ELISA.
IL-8 concentrations in culture supernatants were determined with an enzyme-linked immunosorbent assay (ELISA) kit, Quantikine Colorimetric Sandwich ELISA Human IL-8 (R&D Systems, Minneapolis, Minn.). The threshold of detection of the ELISA system is <10 pg/ml.
RT-PCR.
Total RNA was prepared from cells cultured to subconfluency by using the RNeasy kit (QIAGEN, Hilden, Germany). One-step reverse transcription-PCR (RT-PCR) was carried out by using RT-PCR High-Plus (Toyobo, Osaka, Japan). PCR products were analyzed by electrophoresis on a 2% (wt/vol) agarose gel. The gel was stained with ethidium bromide. The quantitativity of the RT-PCR was confirmed by the linearity of determination curve with various amounts of RNA for each target. The following primer sets were used for the detection of each mRNA, as follows: for IL-8, the sense primer was 5′-ACTTAGATGTCAGTGCATAAAGAC-3′ and the antisense primer was 5′-TTATGAATTCTCAGCCCTCTTCAA-3′; for CD14, the sense primer was 5′-GGTGCCGCTGTGTAGGAAAGA-3′ and the antisense primer was 5′-GGTCCTCGAGCGTCAGTTCCT-3′; for TLR2, the sense primer was 5′-GCCAAAGTCTTGATTGATTGG-3′ and the antisense primer was 5′-TTGAAGTTCTCCAGCTCCTG-3′; for TLR4, the sense primer was 5′-AGATGGGGCATATCAGAGC-3′ and the antisense primer was 5′-CCAGAACCAAACGATGGAC-3′; and for glyceraldehyde-3-phosphate dehydrogenase (GAPDH), the sense primer was 5′-TCCACCACCCTGTTGCTGTA-3′ and the antisense primer was 5′-ACCACAGTCCATGCCATCAC-3′.
Western blotting.
Sodium dodecyl sulfate-polyacrylamide gel electrophoresis and Western blotting were carried out as described previously (34). A mouse anti-CD14 antibody (UCH-M1) and rabbit anti-TLR2 (H-175) and anti-TLR4 (H-80) antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, Calif.). Alkaline phosphatase-labeled goat anti-mouse or anti-rabbit immunoglobulin antibodies were purchased from BioSource International (Camarillo, Calif.) and used as secondary antibodies. Specific antibody binding was detected by using tetrazolium bromochloroindolylphosphate-Nitro Blue Tetrazolium as a substrate.
Flow cytometry.
Cultured cells on the tissue culture flask surface were removed with a cell scraper and harvested by centrifugation. Flow cytometry was carried out with a FACSCalibur (Becton Dickinson, San Jose, Calif.). Phycoerythrin-labeled mouse monoclonal antibodies against CD14 (61D3), TLR2 (TL2.1), and TLR4 (HTA125) and isotype controls, phycoerythrin-labeled mouse immunoglobulin G1 (IgG1) and mouse IgG2a, were purchased from eBioscience (San Diego, Calif.).
PI-PLC treatment.
Phosphatidylinositol-specific phospholipase C (PI-PLC) derived from Bacillus cereus was purchased from Sigma-Aldrich (St. Louis, Mo.). Cells were treated with 0.5 U of PI-PLC/ml for 2 h at 37°C, followed by the addition of 10 μg of LPS or PGN/ml, and were further cultured for 12 h. The concentration of IL-8 in the culture supernatant was determined by ELISA as described above.
Transient expression of mCD14 on mCD14-negative cells.
An expression plasmid carrying human CD14 cDNA (23) was provided by Brian Seed (Massachusetts General Hospital, Boston, Mass.). The CD14 expression plasmid or a control plasmid was transfected into cells by using SuperFect reagent (QIAGEN) according to the manufacturer's instruction manual. Twenty-four hours after transfection, the cells were treated with 1 or 10 μg of LPS or PGN/ml for 24 h. The culture supernatants were assayed for IL-8 concentrations by ELISA.
Effect of exogenous sCD14 on IL-8 induction.
Cultured cells were washed three times with Dulbecco's phosphate-buffered saline (PBS) and cultured in a serum-free medium containing 5% bovine serum albumin (BSA) for 6 h. Following culture in the medium in the presence of 5% heat-inactivated pooled normal human sera (NHS) (CosmoBio, Tokyo, Japan) or 5% BSA for 6 h, the cells were treated with 10 μg of LPS or PGN/ml for 24 h. Culture supernatants were assayed for IL-8 concentrations by ELISA. The heat-inactivated NHS contained sCD14 at a concentration of 1.45 μg/ml as determined by ELISA (R&D Systems). Furthermore, sCD14-depleted NHS was also used in the experiment. Depletion of sCD14 was carried out by an immunoadsorption method. NHS was treated with an anti-CD14 monoclonal antibody (UCH-M1; Chemicon, Temecula, Calif.) and protein G-Sepharose (Amersham Bioscience) at 4°C for 12 h, and then the resin which bound to the anti-CD14 antibody and sCD14 was removed by centrifugation. The treatment was repeated three times. The resulting depleted serum did not contain a detectable amount of sCD14 as determined by ELISA.
Immunohistochemistry.
Normal bladder tissues were obtained from surgical specimens derived from three patients with bladder cancer who were enrolled in this study at the Department of Urology, Sapporo Medical University Hospital. Informed consent was obtained from the patients. Nonneoplasic tissues were obtained after excision of the surgical specimens and were immediately frozen with liquid nitrogen. Tissue sections were prepared. After blocking of nonspecific protein binding, the sections were incubated with an anti-CD14, anti-cytokeratin, or anti-vimentin monoclonal antibody. Mouse antibodies against cytokeratin and vimentin were purchased from Progen Biotechnik (Heidelberg, Germany). The sections were stained with the ENVISION+ HRP kit (DAKO, Carpinteria, Calif.) according to the manufacturer's instruction manual. Development was carried out with 3,3′-diaminobenzidine tetrahydrochloride. Developed sections were counterstained with hematoxylin.
RESULTS
The inducibility of IL-8 by LPS or PGN differs among uroepithelial cell lines.
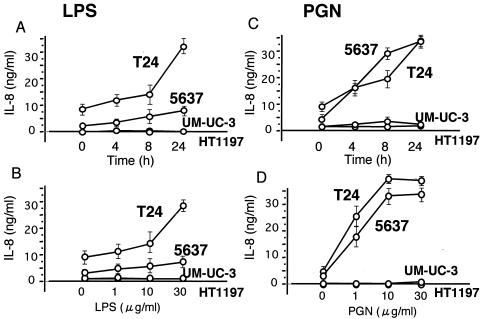
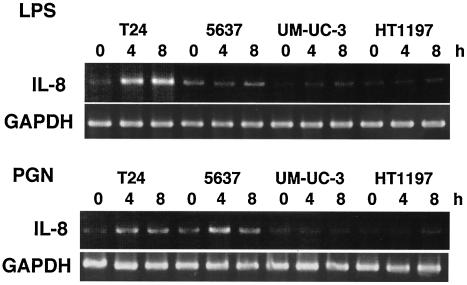
Four human uroepithelial cell lines were stimulated with P. aeruginosa LPS or S. aureus PGN, and the levels of IL-8 in the culture supernatants were determined by ELISA. The time courses and dose dependency of IL-8 induction are shown in Fig. 1. PGN was more a potent inducer of IL-8 in the uroepithelial cells than P. aruginosa LPS. The four cell lines could be divided into two groups: the high responders, T24 and 5637, and the low responders, UM-UC-3 and HT1197. The high responders produced significantly higher levels of IL-8 under nonstimulating conditions than the low responders, and IL-8 levels were dramatically increased by stimulation with the bacterial components. Similar results were observed for mRNA levels (Fig. 2). In response to LPS, IL-8 mRNA was upregulated strongly in T24 cells and weakly in 5637 cells. Induction of IL-8 mRNA by PGN was similar in T24 and 5637 cells, in agreement with results obtained by ELISA. The low levels of IL-8 mRNA in UM-UC-3 and HT1197 cells under nonstimulating conditions are indicated by very weak signals; these levels were only slightly increased in the presence of LPS or PGN.
FIG. 1.
Induction of IL-8 in human uroepithelial cells by stimulation with P. aeruginosa LPS (A and B) or S. aureus PGN (C and D) as determined by ELISA. (A and C) Time course of induction. Ten micrograms of LPS or PGN per milliliter was used for stimulation. (B and D) Cells were stimulated for 12 h. Each experiment was performed in triplicate.
FIG. 2.
Induction of IL-8 mRNA in human uroepithelial cells by stimulation with P. aeruginosa LPS or S. aureus PGN as determined by RT-PCR. Cells were stimulated with 10 μg of LPS or PGN/ml for various times as shown. GAPDH mRNA was used as a control.
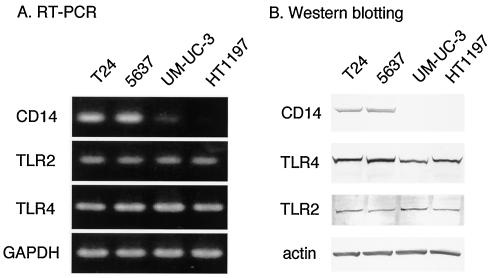
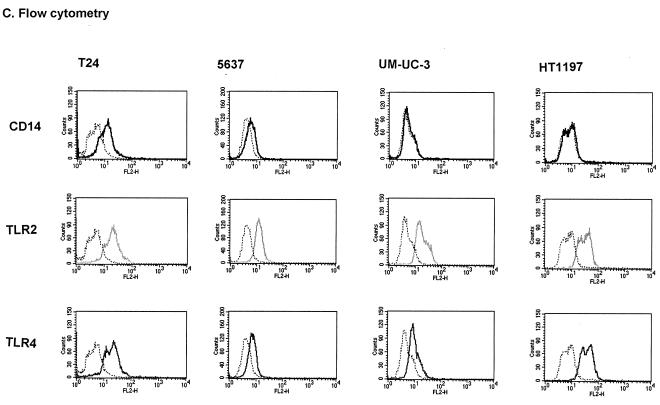
Expression of receptor components specific for LPS and PGN in uroepithelial cell lines.
In order to understand these differences in IL-8 induction, we examined the expression of receptor molecules in the uroepithelial cell lines. Levels of TLR2 and TLR4 expression, determined for the mRNAs by RT-PCR (Fig. 3A), for the proteins in total-cell lysates by Western blotting (Fig. 3B), or for the proteins at the cell surface by flow cytometry (Fig. 3C), were not significantly different in the four cell lines. On the other hand, CD14 mRNA was detected strongly in T24 and 5637 cells and only weakly in UM-UC-3 and HT1197 cells. CD14 proteins were detected on the surfaces of T24 and 5637 cells; in contrast, they were undetectable in UM-UC-3 and HT1197 cell lysates and on the cell surfaces. These results indicate that the expression levels of CD14 differ among uroepithelial cell lines. The difference in CD14 protein expression depended primarily on the transcriptional activity of the CD14 gene. However, the expression level of mCD14 in T24 cells was significantly higher than that in 5637 cells as determined by flow cytometry (Fig. 3C).
FIG. 3.
Expression of CD14, TLR2, and TLR4 in human uroepithelial cells. (A) mRNA levels estimated by RT-PCR. GAPDH mRNA was used as a control. (B) Total-protein levels determined by Western blotting. Actin was used as a control for protein loading. (C) Cell surface expression levels determined by flow cytometry. Dotted lines indicate staining with unrelated isotype-matched control antibodies.
Requirement of mCD14 for efficient induction of IL-8.
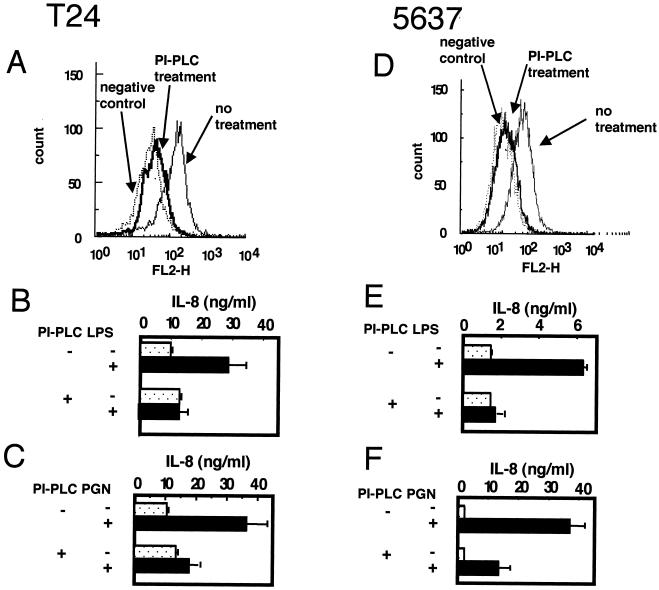
To determine the contribution of mCD14 to IL-8 induction, we tried to remove CD14 molecules from the cell surface. mCD14 is a glycosylphosphatidylinositol-anchored protein, and the protein portion of CD14 can easily be removed from the cell surface by PI-PLC treatment (23). Levels of mCD14 on the surfaces of T24 and 5637 cells were markedly decreased by PI-PLC treatment as determined by flow cytometry (Fig. 4A and D). PI-PLC-treated T24 cells showed dramatic reductions in the LPS- and PGN-stimulated induction of IL-8 (Fig. 4B and C). Similar results were observed for 5637 cells (Fig. 4E and F). These results suggest that mCD14 is necessary for the efficient induction of IL-8 by stimulation with bacterial components such as LPS and PGN. Our observations clearly show that mCD14 participates not only in TLR4 signal transduction but also in TLR2-mediated signaling. However, IL-8 remained inducible by PGN, but not by LPS, after PI-PLC treatment. This may be caused by the fact that both CD14-dependent and CD-14-independent pathways exist in TLR2 signaling.
FIG. 4.
Effects of PI-PLC treatment on IL-8 induction by P. aeruginosa LPS or S. aureus PGN in the uroepithelial cell lines T24 (A, B, and C) and 5637 (D, E, and F). (A and D) Cell surface expression of CD14 with or without PI-PLC treatment as determined by flow cytometry. Cells were treated with 0.5 U of PI-PLC/ml for 2 h and then analyzed by flow cytometry. Similar results were observed with treatment for as long as 14 h (data not shown). Dotted lines indicate staining with unrelated isotype-matched control antibodies. (B, C, E, and F) Induction of IL-8 after stimulation with LPS (B and E) or PGN (C and F) for 12 h in cells that were either left untreated or treated with PI-PLC. The concentration of IL-8 in the culture supernatant was determined by ELISA. Each experiment was performed in triplicate.
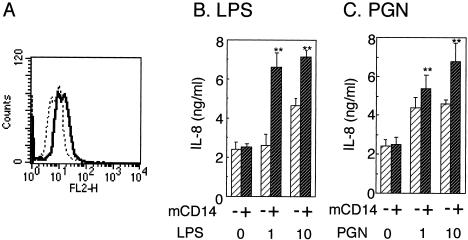
On the other hand, the lack of mCD14 expression is likely to explain the weak IL-8-induction in UM-UC-3 and HT1197 cells. We examined the transfection of a human CD14 expression plasmid into mCD14-negative cells. Figure 5 shows that UM-UC-3 cells transfected with human CD14 cDNA expressed mCD14 as determined by flow cytometry (Fig. 5A). UM-UC-3 cells expressing mCD14 showed more efficient induction of IL-8 production by stimulation with LPS or PGN (Fig. 5B and C). The absolute amount of induced IL-8 in UM-UC-3 cells was smaller than those in T24 and 5637 cells. However, the induction of IL-8 by LPS was about threefold (Fig. 5B); the level of the induction was comparable to those of the high responders, T24 and 5637 cells (Fig. 1A).
FIG. 5.
Effects of transfection with CD14 cDNA on LPS- or PGN-induced IL-8 production in the mCD14-negative cell line UM-UC-3. A human CD14 expression plasmid was transfected into UM-UC-3 cells. (A) Expression of mCD14 in UM-UC-3 cells after 24 h of transfection as determined by flow cytometry (solid line). Dashed line, cells transfected with a control plasmid. (B and C) After 24 h of transfection, cells transfected with a CD14 plasmid or a control plasmid were treated with 1 or 10 μg of LPS (B) or PGN (C)/ml for 24 h. IL-8 concentrations of the resulting culture supernatants were determined by ELISA. Significant differences between CD14 transfectants and control transfectants are indicated (**, P < 0.01).
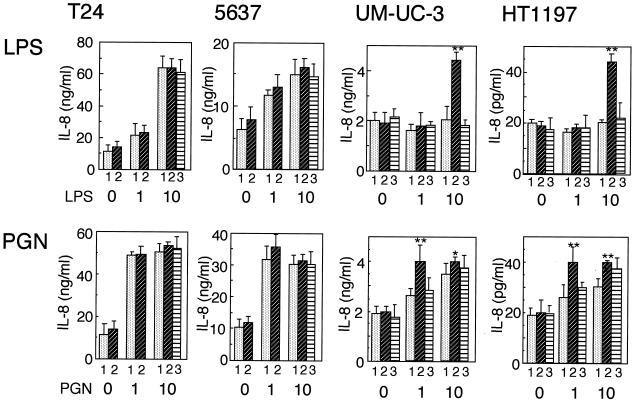
Requirement for sCD14 in the induction of IL-8 in uroepithelial cells.
The experiments described above were performed using cells cultured in a medium containing fetal bovine serum. Under these conditions, the serum is the likely source of sCD14. To clarify whether sCD14 is required for IL-8 induction in uroepithelial cells, we examined the effect of heat-inactivated NHS, which is a source of human sCD14, on the induction of IL-8 after cells had been cultured in a serum-free medium (Fig. 6). The NHS contained 1.45 mg of SCD14 per ml, as determined by ELISA (data not shown). The high-responder cell lines T24 and 5637 did not show significantly different responses in the presence and absence of NHS. In contrast, the low-responder UM-UC-3 and HT1197 cells showed significantly higher induction of IL-8 by LPS or PGN in the presence of NHS than in its absence. Furthermore, sCD14-depleted NHS did not show enhancement of IL-8 induction in UM-UC-3 and HT1197 cells. These results indicate that high responders, which express mCD14, do not need exogenous sCD14, because mCD14 is sufficient for IL-8 induction. In contrast, low-responder cells, in which mCD14 is not detectable, appear to require exogenous sCD14 for IL-8 induction by stimulation with LPS. However, UM-UC-3 and HT1197 cells showed significant induction of IL-8 by PGN stimulation in the absence of sCD14. This result suggests that TLR2 signal transduction by PGN occurs partly in a CD14-independent manner and partly in a CD14-dependent manner (as indicated by its enhancement by sCD14) in UM-UC-3 and HT1197 cells.
FIG. 6.
Effects of heat-inactivated NHS as a source of sCD14 on IL-8 induction in bladder epithelial cells by P. aeruginosa LPS (upper panels) or S. aureus PGN (lower panels). Cells were washed with PBS, cultured in a serum-free medium containing 5% BSA for 6 h, and then cultured in a medium with either 5% BSA (without NHS) (bars 1), 5% NHS (bars 2), or 5% CD14-depleted NHS (bars 3) for 6 h. The cultured cells were stimulated with 1 or 10 μg of P. aeruginosa LPS or S. aureus PGN/ml for 24 h. Concentrations of IL-8 in the culture supernatants were determined by ELISA. Significant differences (**, P < 0.01; *, P < 0.05) between the presence and absence of NHS are indicated. Each experiment was performed in triplicate.
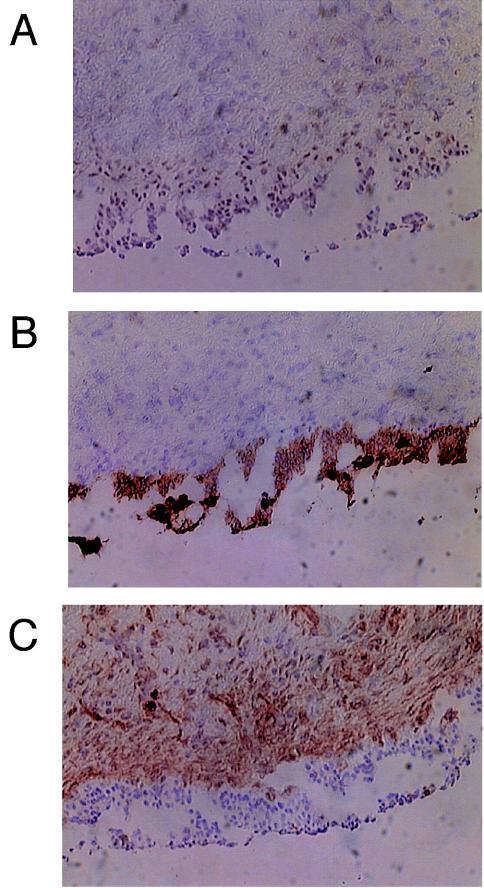
Expression of CD14 in the epithelium of normal human urinary tissues.
In order to reveal CD14 expression in normal human uroepithelial cells, we performed immunohistochemical experiments using normal bladder tissue from surgical specimens excised from bladder cancer patients. We stained with anti-cytokeratin (Fig. 7B) and anti-vimentin (Fig. 7C) antibodies as controls for the epithelium and mesenchyme, respectively. The anti-CD14 antibody (Fig. 7A) showed very weak but significantly positive staining at the epithelial region. These results suggested that CD14 protein is expressed in normal human bladder epithelial cells.
FIG. 7.
Immunochemical staining of CD14 (A), cytokeratin (B), and vimentin (C) in normal human bladder tissue. Binding of the specific antibody was detected by staining with a peroxidase-3,3′-diaminobenzidine system (brown). The specimen was counterstained with hematoxylin (blue). Staining of cytokeratin and vimentin was carried out as controls for the epithelium and mesenchyme, respectively.
DISCUSSION
In the present study, we showed that four uroepithelial cell lines could be subdivided into high responders and low responders with respect to their responses to bacterial components, such as LPS and PGN. High-responder cells produced relatively high levels of IL-8 under nonstimulating conditions and showed marked induction of IL-8 production after stimulation by either PGN or LPS. Low-responder cells produced low levels of IL-8 under both nonstimulating and stimulating conditions. We first showed that the difference in IL-8 induction among the cell lines should be primarily attributed to mRNA levels, i.e., that induction occurs at the level of transcriptional control. What factor(s) contributes to the induction of IL-8? To address this question, we examined the expression levels of cell surface receptors that recognize the bacterial components. TLR2 and TLR4, which are PGN and LPS receptors, respectively (1, 30), were expressed to similar extents in the different cell lines. On the other hand, CD14 mRNA was expressed at markedly higher levels in the two high responders. Low responders expressed extremely low levels of CD14 mRNA, and CD14 protein was undetectable in these cells. The lack of mCD14 expression in UM-UC-3 and HT1197 cells should depend on mRNA levels, but not on posttranscriptional control, such as the shedding or degradation of produced CD14 protein. CD14 is suggested to be present in a membrane-anchored form in high-responder cells. However, mCD14 expression levels were different in T24 versus 5637 cells. These cells had similar levels of CD14 mRNA as determined by RT-PCR and similar levels of total CD14 protein as determined by Western blotting. The expression level of mCD14 in T24 cells was significantly higher than that in 5637 cells. The difference in mCD14 levels could be caused by posttranslational modification. The differences in IL-8 induction were likely to correlate with the levels of mCD14 proteins. Furthermore, mCD14 levels should have a greater impact on responsiveness to LPS than on responsiveness to PGN (Fig. 4).
We propose that mCD14 is a major contributor to the inflammatory reaction, as seen in the induction of IL-8, which is promoted by bacterial components via a TLR2- or TLR4-dependent pathway. On the other hand, epithelial cells, as well as endothelial cells and fibroblasts, can induce IL-8 in the absence of mCD14. Exogenous sCD14 in serum forms a complex with LPS, and this complex interacts with cell surface receptors, namely, TLRs (4, 20, 26). We observed that induction of IL-8 in low-responder cells was significantly enhanced by the addition of human sera as a source of sCD14 (Fig. 6). However, high-responder cells, which express mCD14, did not require exogenous sCD14 for the induction of IL-8. Recent reports have described the presence of mCD14 in epithelial cells, endothelial cells, and fibroblasts (12, 21, 25). Recently, Bäckhed et al. (4) reported the induction of IL-8 by LPS in T24 cells, which we also used in this study. They suggested that T24 cells do not produce endogenous CD14 but efficiently induce IL-8 in the presence of sCD14 protein in the culture medium. Although the reason for this contradiction with our results is not known, we believe that T24 cells express mCD14 under our experimental conditions. We confirmed the expression of CD14 in T24 cells by different three methods: RT-PCR, Western blotting, and flow cytometry. Furthermore, CD14 protein on the cell surface, as detected by flow cytometry, was eliminated by treatment with PI-PLC, which cleaves the glycosylphosphatidylinositol anchor of mCD14 (Fig. 4A and D). Bäckhed et al. detected CD14 protein in T24 cells by Western blotting but not by RT-PCR. Therefore, they concluded that the CD14 protein detected originated from the serum in the culture medium, not from endogenous production. The conclusion that T24 cells lack CD14 mRNA was based on comparison with a positive control, the human monocytic cell line THP-1. We observed that the expression level of CD14 mRNA in T24 cells was much lower than that in THP-1 cells (data not shown). The detection limit for the RT-PCR experiment of Bäckhed et al. could have been too high to allow detection of CD14 mRNA in T24 cells.
The factor(s) that contributes to the variable expression level of mCD14 in bladder epithelial cell lines has not been identified. Transcription of the CD14 gene is controlled by the transcription factor Sp1 (15). There is a single-nucleotide polymorphism (−159C/T) in the promoter of the CD14 gene, and it alters the binding affinity of Sp1 for the promoter and thus the transcriptional activity of the gene (15). The CD14 allele carrying the −159T polymorphism produces CD14 more efficiently than the allele carrying the −159C polymorphism (6, 15). Furthermore, the levels of sCD14 in human sera are significantly different for individuals with the −159C versus the −159T allele, and these levels correlate with clinical features, such as serum IgE levels (6), risk for myocardial infarction (29), and clinical symptoms caused by Helicobacter pylori infection (13). We examined the polymorphism of the CD14 promoter in the four bladder epithelial cell lines by the bidirectional and allele-specific PCR method of Karhukorpi et al. (13) and found that four cell lines examined in this study were heterozygous for the polymorphism (data not shown). This result indicates that the variable levels of CD14 expression in the bladder cell lines are not due to the known promoter polymorphism.
Variation in mCD14 expression levels among individuals should correlate with variation in the ability to mount an inflammatory reaction. In the case of blood cells, there is some evidence for the contribution of mCD14 to the inflammatory response. High mCD14 expression levels are found in peripheral monocytes and intestinal macrophages derived from patients with Crohn's disease and inflammatory bowel disease (10), and mCD14-positive neutrophils accumulate in the lungs of patients with acute respiratory distress syndrome. In contrast, peripheral neutrophils exhibit low mCD14 expression levels, because the protein is shed from the cell surfaces of stimulated neutrophils from patients with acute respiratory distress syndrome (19). Glucocorticosteroids suppress the expression of both mCD14 and sCD14 (17), and the downregulation of CD14 is considered to be one of the mechanisms by which the anti-inflammatory effects of steroids are exerted.
In conclusion, mCD14 on the surfaces of bladder epithelial cells is a more potent contributor to induction of an inflammatory reaction than is sCD14. Urinary IL-8 levels are consistently elevated in patients with urinary tract infections. IL-8 in urine plays an important role in the infiltration of leukocytes, especially neutrophils, through the uroepithelium (27). Uroepithelial cells should be initial and major producers of IL-8 during the process of urinary tract infection. We found that CD14 proteins are expressed in the epithelium of normal human bladder tissue (Fig. 7), and we found by RT-PCR that CD14 mRNA is expressed in the bladder tissue (data not shown). However, at present there is negative evidence for the expression of mCD14 in normal bladder tissue (11). We have detected the expression of mCD14 in normal human bladder tissue by immunohistochemical staining; however, it is difficult to distinguish between mCD14 on the epithelial cells and sCD14, which originate from blood, associated with this tissue.
Acknowledgments
We thank Brian Seed for providing the human CD14 expression plasmid. We also thank Seiji Ohtani for technical support for the immunohistochemical experiments.
REFERENCES
- 1.Akira, S., K. Takeda, and T. Kaisho. 2001. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat. Immunol. 2:675-680. [DOI] [PubMed] [Google Scholar]
- 2.Alexander, C., and E. T. Rietschel. 2001. Bacterial lipopolysaccharides and innate immunity. J. Endotoxin Res. 7:167-202. [PubMed] [Google Scholar]
- 3.Antal-Szalmás, P. 2000. Evaluation of CD14 in host defense. Eur. J. Clin. Investig. 30:167-179. [DOI] [PubMed] [Google Scholar]
- 4.Bäckhed, F., L. Meijer, S. Normark, and A. Richter-Dahlfors. 2002. TLR4-dependent recognition of lipopolysaccharide by epithelial cells requires sCD14. Cell. Microbiol. 4:493-501. [DOI] [PubMed] [Google Scholar]
- 5.Bäckhed, F., M. Söderhäll, P. Ekman, S. Normark, and A. Richter-Dahlfors. 2001. Induction of innate immune responses by Escherichia coli and purified lipopolysaccharide correlate with organ- and cell-specific expression of Toll-like receptors within the human urinary tract. Cell. Microbiol. 3:153-158. [DOI] [PubMed] [Google Scholar]
- 6.Baldini, M., I. C. Lohman, M. Halonen. R. P. Erickson, P. G. Holt, and F. D. Martinez. 1999. A polymorphism in the 5′ flanking region of the CD14 gene is associated with circulating soluble CD14 levels and with total serum immunoglobulin E. Am. J. Respir. Cell Mol. Biol. 20:976-983. [DOI] [PubMed] [Google Scholar]
- 7.Barton, G. M., and R. Medzhitov. 2002. Toll-like receptors and their ligands. Curr. Top. Microbiol. Immunol. 270:81-92. [DOI] [PubMed] [Google Scholar]
- 8.da Silva Correia, J., K. Soldau, U. Christen, P. S. Tobias, and R. J. Ulevitch. 2001. Lipopolysaccharide is in close proximity to each of the proteins in its membrane receptor complex. Transfer from CD14 to TLR4 and MD-2. J. Biol. Chem. 276:21129-21135. [DOI] [PubMed] [Google Scholar]
- 9.Fünfstück, R., S. Franke, M. Hellberg, U. Ott, B. Knöfel, E. Staube, M. Sommer, and J. Hacker. 2001. Secretion of cytokines by uroepithelial cells stimulated by Escherichia coli and Citrobacter spp. Int. J. Antimicrob. Agents 17:253-258. [DOI] [PubMed] [Google Scholar]
- 10.Grimm, M. C., P. Pavli, E. van de Pol, and W. F. Doe. 1995. Evidence for a CD14+ population of monocytes in inflammatory bowel disease mucosa: implications for pathogenesis. Clin. Exp. Immunol. 100:291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hedlund, M., B. Fréndeus, C. Wachtler, L. Hang, H. Fischer, and C. Svanbirg. 2001. Type 1 fimbriae deliver an LPS- and TLR4-dependent activation signal to CD14-negative cells. Mol. Microbiol. 39:542-552. [DOI] [PubMed] [Google Scholar]
- 12.Jersmann, H. P. A., C. S. T. Hii, G. L. Hodge, and A. Ferrante. 2001. Synthesis and surface expression of CD14 by human endothelial cells. Infect. Immun. 69:479-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karhukorpi, J., Y. Yan, S. Niemelä, J. Valtonen, P. Koistinen, T. Joensuu, P. Saikku, and R. Karttunen. 2002. Effect of CD14 promoter polymorphism and H. pylori infection and its clinical outcomes on circulating CD14. Clin. Exp. Immunol. 128:326-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kielian, T. L., and F. Blecha. 1995. CD14 and other recognition molecules for lipopolysaccharide: a review. Immunopharmacology 29:187-205. [DOI] [PubMed] [Google Scholar]
- 15.LeVan, T. D., J. W. Bloom, T. J. Bailey, C. L. Karp, M. Halonen, F. D. Martinez, and D. Vercelli. 2001. A common single nucleotide polymorphism in the CD14 promoter decreases the affinity of Sp protein binding and enhances transcriptional activity. J. Immunol. 167:5838-5844. [DOI] [PubMed] [Google Scholar]
- 16.Muroi, M., T. Ohnishi, and K. Tanamoto. 2002. Regions of the mouse CD14 molecule required for toll-like receptor 2- and 4-mediated activation of NF-κB. J. Biol. Chem. 277:42372-42379. [DOI] [PubMed] [Google Scholar]
- 17.Nockher, W. A., and J. E. Scherberich. 1997. Expression and release of the monocyte lipopolysaccharide receptor antigen CD14 are suppressed by glucocorticoids in vivo and in vitro. J. Immunol. 158:1345-1352. [PubMed] [Google Scholar]
- 18.Ozinsky, A., D. M. Underhill, J. D. Fontenot, A. M. Hajjar, K. D. Smith, C. B. Wilson, L. Schroeder, and A. Aderem. 2000. The repertoire for pattern recognition of pathogens by the innate immune system is defined by cooperation between toll-like receptors. Proc. Natl. Acad. Sci. USA 97:13766-13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parsons, P. E., M. M. Gillespie, E. E. Moore, F. A. Moore, and G. S. Worthen. 1995. Neutrophil response to endotoxin in the adult respiratory distress syndrome: role of CD14. Am. J. Respir. Cell Mol. Biol. 13:152-160. [DOI] [PubMed] [Google Scholar]
- 20.Pugin, J., C.-C. Schürer-Maly, D. Leturcq, A. Moriarty, R. J. Ulevitch, and P. S. Tobias. 1993. Lipopolysaccharide activation of human endothelial and epithelial cells is mediated by lipopolysaccharide-binding protein and soluble CD14. Proc. Natl. Acad. Sci. USA 90:2744-2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Putnins, E. E., A.-R. Sanaie, Q. Wu, and J. D. Firth. 2002. Induction of keratinocyte growth factor 1 expression by lipopolysaccharide is regulated by CD14 and Toll-like receptors 2 and 4. Infect. Immun. 70:6541-6548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shimazu, R., S. Akashi, H. Ogata, Y. Nagai, K. Fukudome, K. Miyake, and M. Kimoto. 1999. MD-2, a molecule that confers lipopolysaccharide responsiveness on Toll-like receptor 4. J. Exp. Med. 189:1777-1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simmons, D. L., S. Tan, D. G. Tenen, A. Nicholson-Weller, and B. Seed. 1989. Monocyte antigen CD14 is a phospholipid anchored membrane protein. Blood 73:284-289. [PubMed] [Google Scholar]
- 24.Takeuchi, O., T. Kawai, P. F. Muhlradt, M. Morr, J. D. Radolf, A. Zychlinsky, K. Takeda, and S. Akira. 2001. Discrimination of bacterial lipoproteins by Toll-like receptor 6. Int. Immunol. 13:933-940. [DOI] [PubMed] [Google Scholar]
- 25.Tamai, R., T. Sakuta, K. Matsushita, M. Torii, O. Takeuchi, S. Akira, S. Akashi, T. Espevik, S. Sugawara, and H. Tanaka. 2002. Human gingival CD14+ fibroblasts primed with gamma interferon increase production of interleukin-8 in response to lipopolysaccharide through up-regulation of membrane CD14 and MyD88 mRNA expression. Infect. Immun. 70:1272-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uehara, A., S. Sugawara, R. Tamai, and H. Takada. 2001. Contrasting responses of human gingival and colonic epithelial cells to lipopolysaccharides, lipoteichoic acids and peptidoglycans in the presence of soluble CD14. Med. Microbiol. Immunol. 189:185-192. [DOI] [PubMed] [Google Scholar]
- 27.Uehling, D. T., D. B. Johnson, and W. J. Hopkins. 1999. The urinary tract response to entry of pathogens. World J. Urol. 17:351-358. [DOI] [PubMed] [Google Scholar]
- 28.Ulmer, A. J., E. T. Rietschel, U. Zähringer, and H. Heine. 2002. Lipopolysaccharide: structure, bioactivity, receptors, and signal transduction. Trends Glycosci. Glycotechnol. 14:53-68. [Google Scholar]
- 29.Unkelbach, K., A. Gardemann, M. Kostrzewa, M. Philipp, H. Tillmanns, and W. Haberbosch. 1999. A new promoter polymorphism in the gene of lipopolysaccharide receptor CD14 is associated with expired myocardial infarction in patients with low atherosclerotic risk profile. Arterioscler. Thromb. Vasc. Biol. 19:932-938. [DOI] [PubMed] [Google Scholar]
- 30.Vasselon, T., and P. A. Detmers. 2002. Toll receptors: a central element in innate immune responses. Infect. Immun. 70:1033-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Viriyakosol, S., P. S. Tobias, R. L. Kitchens, and T. N. Kirkland. 2001. MD-2 binds to bacterial lipopolysaccharide. J. Biol. Chem. 276:38044-38051. [DOI] [PubMed] [Google Scholar]
- 32.Westphal, O., and K. Jann. 1965. Bacterial lipopolysaccharides: extraction with phenol-water and further application of the procedure. Methods Carbohydr. Chem. 5:83-91. [Google Scholar]
- 33.Yokota, S., M. Terashima, J. Chiba, and H. Noguchi. 1992. Variable cross-reactivity of Pseudomonas aeruginosa lipopolysaccharide-core-specific monoclonal antibodies and its possible relationship with serotype. J. Gen. Microbiol. 138:289-296. [DOI] [PubMed] [Google Scholar]
- 34.Yokota, S., H. Yanagi, T. Yura, and H. Kubota. 1999. Cytosolic chaperonin is up-regulated during cell growth: preferential expression and binding to tubulin at G1/S transition though early S phase. J. Biol. Chem. 274:37070-37078. [DOI] [PubMed] [Google Scholar]
- 35.Yoshimura, A., E. Lien, R. R. Ingalls, E. Tuomanen, R. Dziarski, and D. Golenbock. 1999. Recognition of Gram-positive bacterial cell wall components by the innate immune system occurs via Toll-like receptor 2. J. Immunol. 163:1-5. [PubMed] [Google Scholar]