Complement anaphylatoxins (C3a, C5a) are potent inflammatory mediators, implicated in the exaggerated inflammatory response seen in chronic obstructive pulmonary disease (COPD) [1]. COPD patients have decreased levels of serum C3 and C4 [2, 3], and higher levels of sputum C3a and C5a, than healthy volunteers [4]. Both sputum and serum C5a levels climb during acute exacerbations [1, 5]. Serum C5a during COPD exacerbations has been positively correlated with C-reactive protein (CRP) and negatively correlated with percentage predicted forced expiratory volume in 1 s (FEV1 % pred) [5].
Short abstract
Rise in sputum complement (C3a, C5a) levels during COPD exacerbation is associated with recovery time http://ow.ly/ZaPj303xxPf
To the Editor:
Complement anaphylatoxins (C3a, C5a) are potent inflammatory mediators, implicated in the exaggerated inflammatory response seen in chronic obstructive pulmonary disease (COPD) [1]. COPD patients have decreased levels of serum C3 and C4 [2, 3], and higher levels of sputum C3a and C5a, than healthy volunteers [4]. Both sputum and serum C5a levels climb during acute exacerbations [1, 5]. Serum C5a during COPD exacerbations has been positively correlated with C-reactive protein (CRP) and negatively correlated with percentage predicted forced expiratory volume in 1 s (FEV1 % pred) [5].
We investigated complement activation in serum and sputum of a well-characterised COPD cohort, testing two hypotheses: 1) that baseline complement levels are related to markers of disease severity, and 2) that changes in degree of complement activation (C3a/C5a) during an exacerbation relate to severity of the episode and are associated with longer recovery times.
Subjects were patients enrolled in the London COPD cohort, with research ethics committee approval (REC 09/H0720/8). Recruitment and monitoring of these patients has been described previously [6]. Exacerbations and recovery were defined according to previously published criteria [6, 7]. Frequent and infrequent exacerbators were defined as patients having ≥2 or <2 diary card defined exacerbations per year, respectively [8].
Exacerbations were treated according to the prevailing guidelines and clinical judgement. Blood samples were taken and spirometry performed prior to commencing treatment. Bacterial presence and load in sputum was determined by quantitative PCR analysis [9].
Paired serum and sputum samples were obtained from 24 COPD patients, at baseline and at exacerbation onset. Serum and sputum samples were assayed for complement (C3a, C5a including C3a des Arg, C5a des Arg) and cytokines (interleukin (IL)-2, IL-4, IL-6, IL-10, tumour necrosis factor, interferon (IFN), IL-17a) using two commercial kits: BD Human Anaphylatoxin Kit for C3a/C5a and BD Human Th1/Th2/Th17 Kit for cytokines (BD Biosciences, San Jose, CA, USA), both employing a cytometric bead array method. Flow cytometry data were analysed using FCAP Array software (Soft Flow Hungary, Pecs, Hungary).
The 24 patients recruited (16 male, eight female) had a mean±sd age of 75.4±7.97 years. All had at least mild to moderate COPD with mean±sd FEV1 of 1.17±0.38 L, FEV1 % pred of 47.7±20.5% and FEV1/forced vital capacity ratio of 45.9±12.2%. Overall mean±sd smoking pack-years were 59.9±44.6 pack-years and seven out of 24 (29%) were current smokers. 20 out of 24 patients were on inhaled corticosteroids: 15 fluticasone, four budesonide and one beclomethasone. Four patients were on aspirin, eight patients on a statin and three patients on both. For both serum and sputum C3a and C5a there was no correlation between baseline levels and baseline markers of COPD severity, including absolute FEV1, FEV1 % pred, Global Initiative for Chronic Obstructive Lung Disease grade and COPD Assessment Test score. There was no correlation between levels of complement C3a/C5a at baseline and frequency of COPD exacerbations; furthermore, there was no difference in complement level between frequent versus infrequent exacerbators.
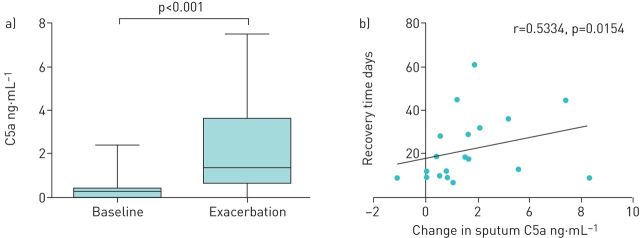
Sputum levels of both C3a and C5a were higher at exacerbation onset than during baseline: median (range) C3a 15.40 (1.471–30.78) versus 9.085 (0.4635–50.66) ng·mL−1, respectively, p=0.0428, and C5a 1.191 (0–7.544) versus 0.2985 (0–2.404) ng·mL−1, respectively, p<0.001 (figure 1a). Conversely, serum C3a was significantly lower compared with baseline levels: median (range) 113.9 (56.83–144.7) versus 153.7 (102.3–206.1) ng·mL−1, respectively, p<0.001; serum C5a levels were also significantly lower at exacerbation than baseline: median (range) 12.33 (5.402–34.48 ) versus 14.79 (8.332–32.43) ng·mL−1, respectively, p=0.0278.
FIGURE 1.
a) Median sputum C5a levels were higher during exacerbations than at baseline: 1.191 versus 0.2985 ng·mL−1, respectively (p<0.001). b) Recovery time from a chronic obstructive pulmonary disease exacerbation was associated with change in sputum C5a level between baseline and exacerbation.
A significant correlation was seen between the difference in sputum C5a level from baseline to exacerbation and time taken for clinical recovery: a greater increase in sputum C5a was associated with a longer clinical recovery (r=0.5334, p=0.0154) (figure 1b). The difference in sputum C3a from baseline to exacerbation was also correlated with clinical recovery (r=0.4488, p=0.0471).
Of the cytokines measured, only IL-6 and IL-10 showed any significant variation between baseline and exacerbation. Sputum C5a at exacerbation was positively correlated with sputum IL-10 level (r=0.5097, p=0.0110). There was no correlation between serum or sputum C3a or C5a and CRP at exacerbation. There was also no correlation between changes in C3a or C5a between baseline and exacerbation, or changes in FEV1 between baseline and exacerbation.
Bacteria was detected in the sputum of 11 out of 24 (46%) patients at exacerbation and in three out of 24 (13%) patients at baseline. However, we found no association between the presence of bacteria in sputum with either sputum C3a or C5a at exacerbation or baseline; there was no correlation between bacterial load and sputum complement levels, either at exacerbation or baseline.
This study demonstrated significant changes in markers of complement activation (C3a, C5a) between baseline and exacerbation in a well-characterised COPD cohort. Significant increases in both sputum C3a and C5a were found during COPD exacerbations compared with baseline; this was consistent with previous studies, two of which found sputum C5a elevated [1, 5] and another demonstrated C3a elevation at exacerbation [10]. The opposite was seen for serum C3a and C5a, in which we found significantly lower levels during exacerbations.
The increase in sputum C3a and C5a seen at exacerbation may relate to complement activation occurring locally in the lung or migration of activated complement components (including C3a and C5a) from the circulation into lung tissue. Although the liver is the major site of complement synthesis, it is known that complement proteins can be synthesised in lung epithelial cells and alveolar macrophages [11]; C5a generated in lung tissue has been shown to activate macrophages in the presence of immune complexes, leading to production of pro-inflammatory cytokines and chemokines [12]. In our study, IL-6 and IL-10 were the only cytokines found to have any variation between exacerbation and baseline. IL-10 has a predominantly anti-inflammatory role: the positive correlation between sputum C5a and IL-10 found in our study may indicate an inflammatory response secondary to complement activation occurring locally in the lung.
Exacerbation recovery is an important target for novel COPD treatments. The finding that a larger change in sputum complement levels (particularly C5a) between baseline and exacerbation is associated with longer recovery time raises the possibility that excessive complement activation has a harmful effect in this setting. Anaphylatoxins such as C5a have several potential harmful effects, including mediating chemotaxis (particularly neutrophil migration), inflammation and generation of cytotoxic oxygen radicals [13]. It would therefore not be surprising that excessive levels of these might have a negative impact on recovery.
Although our study has demonstrated an association between changes in complement levels in sputum at exacerbation and clinical recovery, we were not able to demonstrate any other association between complement and markers of disease severity, either at exacerbation or baseline. This was despite the fact that the majority of patients in this study (17 out of 24 (71%)) had a history of frequent exacerbations and thus were of a relatively severe COPD phenotype.
A limitation to the current study is the fact that given patient numbers were small, it is not possible to comment on the significance of our results to clinical practice. Further research, including the identification of subtypes of COPD patients that have particularly high complement levels at exacerbation, will enable this possible relationship to be further elucidated.
In conclusion, this study has shown significant changes in complement activation at COPD exacerbation. For the first time we have demonstrated a significant relationship between the rise in sputum C3a and C5a levels at exacerbation and recovery time. Excessive complement activation may impair local immune functioning and thus may prolong exacerbation length. Future studies should examine complement inhibition agents as potential novel acute exacerbation therapies.
Acknowledgements
Conception and design: J.-P. Westwood, A.J. Mackay, M. Scully; analysis and interpretation: J.-P. Westwood, A.J. Mackay, J.A. Wedzicha, S.J. Machin, G. Donaldson, M. Scully; drafting the manuscript for important intellectual content: J.-P. Westwood, A.J. Mackay, J.A. Wedzicha, M. Scully.
Footnotes
Conflict of interest: Disclosures can be found alongside this article at openres.ersjournals.com
References
- 1.Marc MM, Kristan SS, Rozman A, et al. Complement factor C5a in acute exacerbation of Chronic Obstructive Pulmonary Disease. Scand J Immunol 2010; 71: 386–391. [DOI] [PubMed] [Google Scholar]
- 2.Miller RD, Kueppers F, Offord KP. Serum concentrations of C3 and C4 of the complement system in patients with chronic obstructive pulmonary disease. J Lab Clin Med 1980; 95: 266–271. [PubMed] [Google Scholar]
- 3.Chauhan S, Gupta MK, Goyal A, et al. Alterations in immunoglobulin & complement levels in chronic obstructive pulmonary disease. Indian J Med Res 1990; 92: 241–245. [PubMed] [Google Scholar]
- 4.Marc MM, Korosec P, Kosnik M, et al. Complement factors C3a, C4a, and C5a in chronic obstructive pulmonary disease and asthma. Am J Respir Cell Mol Biol 2004; 31: 216–219. [DOI] [PubMed] [Google Scholar]
- 5.Zhang J, Yao WZ, Sun YC. [Changes of anaphylatoxin C5a in chronic obstructive pulmonary disease and the relationship with systemic and local inflammation]. Zhonghua Jie He He Hu Xi Za Zhi 2008; 31: 356–359. [PubMed] [Google Scholar]
- 6.Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 157: 1418–1422. [DOI] [PubMed] [Google Scholar]
- 7.Hurst JR, Donaldson GC, Quint JK, et al. Temporal clustering of exacerbations in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2009; 179: 369–374. [DOI] [PubMed] [Google Scholar]
- 8.Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363: 1128–1138. [DOI] [PubMed] [Google Scholar]
- 9.Garcha DS, Thurston SJ, Patel AR, et al. Changes in prevalence and load of airway bacteria using quantitative PCR in stable and exacerbated COPD. Thorax 2012; 67: 1075–1080. [DOI] [PubMed] [Google Scholar]
- 10.Zhang J, Yao WZ, Chen YH. [Change in airway anaphylatoxin-complement factors C3a of sputum in patients with chronic obstructive pulmonary disease]. Beijing Da Xue Xue Bao 2011; 43: 446–449. [PubMed] [Google Scholar]
- 11.Strunk RC, Eidlen DM, Mason RJ. Pulmonary alveolar type II epithelial cells synthesize and secrete proteins of the classical and alternative complement pathways. J Clin Invest 1988; 81: 1419–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sarma VJ, Huber-Lang M, Ward PA. Complement in lung disease. Autoimmunity 2006; 39: 387–394.16923538 [Google Scholar]
- 13.Ward PA. The harmful role of C5a on innate immunity in sepsis. J Innate Immun 2010; 2: 439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]